Causes and course of the disease
The causes of inflammation of the auricle are various infections, among which the most common is Pseudomonas aeruginosa, which penetrates the perichondrium in the following cases:
- In case of mechanical trauma, as well as as a result of surgical trauma, which can occur during plastic surgery of the external auditory canal and after radical surgery on the ear;
- For burns and frostbite;
- With a boil of the ear;
- For influenza or tuberculosis.
Purulent perichondritis of the outer ear is diagnosed more often than serous perichondritis, which occurs as a result of insect bites.
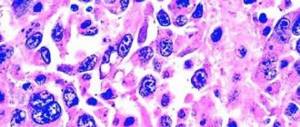
First, pain appears in the ear canal or ear area. Then a swelling appears, which gradually spreads over almost the entire area of the shell, with the exception of the lobe. At the beginning of the disease, changes in the skin are almost invisible, but then a lumpy swelling appears. In such places, fluctuation (wave-like fluctuations when touched) is observed, which occurs due to the formation of purulent exudate between the cartilage and perichondrium. If treatment is not started on time, melting of the cartilage will occur, followed by wrinkling and cicatricial deformation of the auricle. The clinical picture of serous perichondritis is much calmer than that of purulent perichondritis.
Diagnostics
If the above symptoms appear, you should seek qualified help from a therapist or otolaryngologist. Regardless of the form of the disease, instrumental examinations are required to confirm the diagnosis. However, first of all, the clinician must:
- get acquainted with the patient’s medical history - to identify the underlying ailment that could serve as a source of perichondritis;
- collect and analyze the patient’s life history to establish the primary or secondary nature of the origin of the pathology;
- Conduct a thorough physical examination of the problem area, aimed primarily at assessing the condition of the skin and identifying deformations. If the costosternal joints are affected, palpation of the anterior wall of the abdominal cavity will be required;
- interview the person in detail to establish the degree of intensity of symptoms.
Instrumental and laboratory diagnostic measures may include:
- general clinical and biochemical blood test;
- fistulography;
- CT and MRI;
- radiograph of the ribs;
- cartilage biopsy;
- laryngoscopy;
- diaphanoscopy;
- rhinoscopy;
- puncture of the inflammatory focus for subsequent laboratory studies.
Rhinoscopy photo.
Clinical picture
The main symptom of this disease is pain, which quite often precedes reactive infiltration of the skin of the outer ear. The swelling quickly spreads to the entire surface of the ear. The exception is the lobe, because it lacks cartilage. Initially, the swelling has an uneven, even rather lumpy surface. Exudate then forms between the cartilage and the perichondrium. If the patient does not receive urgent (emergency) help, and the pus is not evacuated (removed), the cartilage will melt and turn into a bag of pus, and the process will develop into chondritis (inflammation).
Friends! Timely and correct treatment will ensure you a speedy recovery!
Perichondritis of the costal arch code ICD
Perichondritis is inflammation of the perichondrium. It is observed quite rarely. Perichondritis of the costal cartilages usually develops after injury. Damage to the auricle can occur due to injuries and purulent processes in the outer and middle ear. Perichondritis of the laryngeal cartilages is usually a complication of intubation or radiation therapy for laryngeal cancer. In addition, cartilage damage can develop as a result of a general infectious disease (malaria, influenza). Specific tuberculous and syphilitic perichondritis occur very rarely. There are two main forms of perichondritis: aseptic and purulent. With aseptic perichondritis, as a rule, there is a gradual regression of symptoms, with purulent perichondritis - destruction of cartilage and the formation of fistulas. For aseptic perichondritis, conservative therapy is carried out; for purulent perichondritis, surgical operations are performed. Treatment of perichondritis, depending on the etiology and location, can be carried out by traumatologists, otolaryngologists or oncologists.
Features of the perichondrium.
In its functions, the perichondrium is similar to the periosteum. However, pathological processes in the periosteum and perichondrium occur differently and have different consequences, which is due to differences in the structure and nutrition of bone and cartilage. The bone is equipped with its own blood vessels; it receives nutrition not only from the outside (from the periosteum), but also from the inside (from the bone marrow). Cartilage does not have blood vessels, and the perichondrium is its only source of nutrients. Therefore, with periostitis, bone necrosis does not always occur, while destruction or detachment of the perichondrium inevitably entails necrosis of the entire layer of underlying cartilage. The periosteum has pronounced proliferative and plastic properties, which allows it to participate in the formation of callus in the fracture zone. The same property of the periosteum explains the proliferation of bone tissue in chronic (ossifying) periostitis. Unlike the periosteum, the perichondrium has insignificant proliferative properties, so excess cartilage is not formed as a result of inflammation, and the only clinically significant forms of perichondritis are aseptic and purulent.
Purulent perichondritis of the ribs.
Purulent perichondritis of the ribs usually occurs as a result of an open injury with damage to the costal cartilages and/or crushing of the surrounding soft tissues or due to contact spread of infection (with mediastinitis, pleural empyema, osteomyelitis of the sternum and ribs). Less commonly, perichondritis is caused by complications after chest surgery. The causative agents, as a rule, are streptococci or staphylococci, less often - Escherichia coli, Proteus, Pseudomonas aeruginosa and other bacteria. Costal perichondritis is manifested by pain along the ribs, aggravated by movements and deep breathing. The general condition in the absence of other purulent processes usually remains satisfactory. An infiltrate forms in the affected area. After some time, the area of compaction softens and fluctuation appears. If the costal arch is involved in the process, inflammation can spread to the entire lower part of the chest and the upper part of the anterior abdominal wall. The formed abscess breaks through the skin or through the posterior perichondrium. In the first case, a fistula is formed, in the second - swelling in the soft tissues. The period of acute inflammation with perichondritis of the ribs can last up to 3 months. At this time, foci of destruction form in the area of the perichondrium, from which microbes penetrate into the central zone of the cartilage. Chondritis develops, spreading beyond the primary purulent focus. From the central areas of the cartilage, the infection spreads to the unchanged perichondrium. The peculiarities of the spread of the purulent process cause damage to the cartilage over a significant extent. After 3 months, the phenomena of perichondritis subside, while regenerative processes are combined with ongoing necrosis of cartilage tissue. Usually, the destroyed cartilage is gradually replaced by scar tissue, less often by bone tissue. Cartilage restoration is very rare. The diagnosis of perichondritis is based on the clinical picture, CT and MRI data. For fistulas, fistulography is performed. The most effective treatment is complete removal of the affected cartilage. When the process spreads to the bone (osteomyelitis of the ribs), an additional 2-3 cm of bone tissue is removed. In the postoperative period, antibiotics and painkillers are prescribed. The outcome of rib perichondritis is usually favorable.
Tietze syndrome.
Tietze syndrome is aseptic perichondritis in the area of attachment of the costal cartilages to the sternum. The etiology is not fully understood; there are theories about the connection of the disease with previous injuries, metabolic disorders and decreased immunity. The patient complains of pain on the side of the sternum (usually on one side, more often on the left). The pain intensifies with sneezing, coughing, movements and turns of the body. Upon palpation, a tumor-like formation measuring 2-5 td is determined. The skin over it is usually not changed, in 10% of patients there is slight swelling, local hyperthermia and hyperemia. In the early stages, the diagnosis of perichondritis is clarified using CT scan or cartilage biopsy. After 2-3 months, corresponding changes appear on radiographs of the ribs: calcification of the cartilage, narrowing of the intercostal space and thickening of the anterior part of the bony rib. Conservative therapy includes taking NSAIDs (ibuprofen, diclofenac, voltaren) and gentle manual manipulation. For severe pain, blockades with hydrocortisone are performed. Surgical treatment consists of resection of the affected cartilage.
Perichondritis of the larynx.
The cause of the development of laryngeal perichondritis is most often measles necrosis, radiation therapy for laryngeal cancer, and bedsores caused by intubation. Less commonly, the cartilage of the larynx is affected by tuberculosis and syphilis. Inflammation is always purulent in nature due to contamination of the affected area with pathogens penetrating from the upper respiratory tract. As a rule, perichondritis begins in the deep layers of the perichondrium. Pus exfoliates the perichondrium from the cartilage, and the corresponding area of cartilaginous tissue becomes necrotic and gradually melts. After some time, the abscess opens into the larynx, esophagus or pharynx, less often - out through the skin. The diagnosis of perichondritis is made based on clinical signs and laryngoscopy data. The course of the disease is long, the prognosis is unfavorable. Due to the weak restorative ability of cartilage, the resulting defect is poorly filled, granulations form weakly and sluggishly. Many patients with laryngeal perichondritis die from pneumonia or sepsis. Even with a favorable outcome, a deforming scar is formed in the affected area, which affects the voice, makes breathing difficult, or (in the case of large scar formations in the area of the entrance to the larynx) causes frequent entry of food into the respiratory tract.
Treatment
For this disease, antibacterial therapy is prescribed. Damaged areas are lubricated with 5% tincture of iodine or 10% silver nitrate (lapis). The following physiotherapeutic procedures must be prescribed: ultraviolet irradiation, UHF, microwave, laser therapy sessions, magnetic therapy sessions, ultrasound sessions. If fluctuation is observed, then drainage is performed, which involves a wide incision and curettage of the abscess, which is necessary to remove necrotic tissue. Tampons with antibiotic solutions are placed into the cavity. Dressings are done daily, and in severe cases - twice a day.
Treatment of perichondritis
The treatment plan for eliminating perichondritis is prescribed by the attending physician individually for each patient, since treatment tactics may differ depending on the location of the inflamed cartilage.
Thus, treatment for perichondritis may include:
- surgical intervention aimed at removing the affected cartilage is indicated for damage to the ribs. After surgery you will need to take antibiotics and painkillers. A similar treatment option is necessary for Tietze syndrome;
- opening of the abscess and physiotherapeutic procedures for damage to the outer ear. The most effective in the treatment of perichondritis of the auricle are UHF and microwave. The use of local agents, for example, Tizin or Nazivin, is also indicated;
- resection of the cartilage of the larynx - however, even after this, a deforming scar is formed, affecting the voice and making breathing difficult;
- drainage of an abscess in the nasal cavity - in order to partially preserve the nasal septum.
Treatment with lotions and compresses based on decoctions of medicinal herbs or plants, as well as a solution of boric acid, can be effective only if the outer ear or nasal septum is affected. In any case, such therapy should be agreed upon with the attending physician.
Perichondritis
Perichondritis
- This is an inflammation of the perichondrium. It can be primary (for acute or chronic cartilage injuries) or secondary (for general infectious diseases and direct microbial damage). Most often it occurs in the area of the costal cartilages, cartilages of the larynx and auricle. Manifested by pain and swelling of the affected area. When suppuration occurs, the tissue may melt and form a fistula. The diagnosis is made on the basis of clinical symptoms, ultrasound and fistulography (for purulent processes). Treatment of perichondritis can be conservative or surgical.