Estrogens are the flagships of hormonal levels in women
Estrogens are steroidal female sex hormones that are synthesized primarily in the ovaries of women and are produced in small quantities by the adrenal cortex, bone and adipose tissue, hair follicles, skin and even the brain. By the way, in men, a certain amount of estrogen is produced by the testicles.
Without exaggeration, the role of estrogens in the female body can be called global. They conduct the entire orchestra of physiological functions. Not only the reproductive system, but also the central nervous, cardiovascular, bronchopulmonary, bone, urinary and other systems depend on the activity of estrogen.
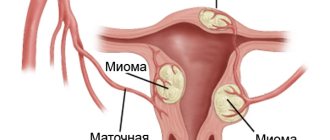
We can say that they create an invisible dome that protects the fair sex from many ailments: atherosclerosis, thromboembolism, heart attacks and strokes, hypothyroidism, uterine fibroids, endometriosis, cystitis, osteoporosis, obesity, depression and other disorders. And of course, pregnancy is impossible without estrogens. The cessation of menstruation and the onset of menopause are associated precisely with a drop in estrogen levels.
Estrogens include estradiol (the most active and significant hormone for women), estrone and estriol . Interestingly, they are all formed from male sex hormones - androgens. In particular, estradiol is produced by the action of aromatase on testosterone, so testosterone is also a very important hormone for women, although it is considered a male hormone.
The female genital organs are divided into internal and external.
- sex gland - ovary,
- uterus,
- the fallopian tubes,
- vagina.
The external genitalia include formations of the so-called pudendal region:
- large private lips,
- small pudendal lips,
- clitoris.
The ovary is a paired gland that is located in the small pelvis on the posterior surface of the broad ligaments of the uterus. On the outside, the ovary is covered with a connective tissue membrane, under which there is a cortex, and deeper - the medulla. The ovarian cortex contains vesicles of different sizes, or follicles, each of which develops a female reproductive cell (ovum), and the medulla contains blood vessels and nerves. The formation of follicles is completed at the time of birth. 200-300 thousand of them are laid, by the age of 10 there are 3-4 times fewer of them, by the beginning of puberty there are about 15 thousand left, of which only 300-400 mature.
Unlike the male gonads, the ovaries do not have ducts. A mature egg is released from the follicle when its wall ruptures. Together with the flowing clear liquid, the egg ends up on the surface of the ovary, in the peritoneal cavity, from where it is drawn into the lumen of the fallopian tube. In place of the burst follicle, a corpus luteum is formed - an endocrine gland. When the egg is not fertilized, the corpus luteum is called false and undergoes reverse development. When the egg is fertilized and pregnancy occurs, the corpus luteum is called true; it grows and remains throughout pregnancy.
The uterus lies in the pelvis between the bladder and rectum. In the uterus there are:
- bottom (top),
- body,
- neck (bottom).
The slit-like cavity of the uterus from the bottom communicates with the right and left fallopian tubes, and from the cervix it continues into the cervical canal, which ends with an opening in the vagina. On the uterus, the vesical and intestinal surfaces, right and left edges are distinguished.
The wall of the uterus has:
- mucous membrane (endometrium),
- muscular (myometrium),
- serous (perimeter) membrane.
The mucous membrane contains glands that secrete mucous fluid and blood vessels into the uterine cavity. The fertilized egg is immersed here. Outside of pregnancy, the surface layer of the mucous membrane regularly, after 24-28 days, peels off and is rejected along with the egg entering the uterine cavity. The ruptured vessels of the mucous membrane bleed. This uterine bleeding is called menstruation and lasts 3-4 days. The time from the beginning of one menstruation to the beginning of the next is called the menstrual cycle. At this time, complex structural and functional changes occur in the woman’s body.
The fallopian tube is a paired formation 10–12 cm long, through which the egg moves into the uterus. Each tube lies at the top of the broad ligament of the uterus and has two openings: one opens into the uterus, the other opens into the peritoneal cavity near the ovary. The wall of the tube consists of a mucous membrane covered with ciliated epithelium, a muscular and serous membrane. Fluctuations of the cilia of the epithelium and contractions of the muscular layer contribute to the movement of the egg through the tube.
The vagina is a tube about 8 cm long, the front and back walls of which are flattened. At the top the tube communicates with the cervix, and at the bottom it opens into the pudendal area. Before entering this area, the vagina, like the urethra, pierces the thickness of the urogenital diaphragm. The rectum lies behind the vagina and the urethra lies in front. The inner surface of the vagina is covered with a mucous membrane, which forms a fold in the pudendal area, called the hymen, then there is a muscular layer and then connective tissue, in which there are many elastic fibers.
Male genitalia are divided into internal and external. Internal ones include:
- sex gland - testicle,
- epididymis,
- seminal vesicle,
- prostate,
- bulbo-urethral glands.
The external genitalia include:
- penis,
- scrotum.
The testicle is a paired gland that originates in the abdominal cavity and then descends into the scrotum through the inguinal canal. The testicle has several membranes: serous, has two layers: parietal and visceral, between which a serous testicular cavity is formed with a small amount of serous fluid. The visceral layer covers the tunica albuginea, adjacent to the substance of the testicle, and forms septa inside this substance that divide it into lobules. There are 150–250 lobules in the testicle. Each lobule contains tubules, in the initial part of which the formation of male germ cells - sperm
The epididymis is located along the superior posterior edge of the testicle and has:
- head,
- body,
- tail.
The efferent tubules of the testicle in the epididymis, connecting, form the epididymal duct, which serves to conduct sperm into the vas deferens. The vas deferens enters the spermatic cord, where in addition to it there are arteries, veins, lymphatic vessels and nerves surrounded by membranes. The spermatic cord, in the form of a cord on which the testicle and epididymis are suspended, rises up and passes through the inguinal canal. The vas deferens, having separated from the cord, runs along the side wall of the pelvis to the bottom of the bladder, where it connects with the excretory duct of the seminal vesicles.
The seminal vesicle is adjacent to the end of the vas deferens. The excretory duct of the vesicle converges at an acute angle with the vas deferens. The seminal vesicle contains a fluid that is secreted by the mucous membrane and affects sperm motility.
The prostate gland (unpaired organ) is located under the bottom of the bladder in such a way that it covers the beginning of the urethra. The prostate gland contains glandular elements and smooth muscle fibers. The secretion of the gland flows through small ducts into the urethra and joins the seed, which enters here through the ejaculatory ducts. The smooth muscle tissue of the gland helps to squeeze secretions out of the gland and narrow the urethra, i.e., retain urine in the bladder while semen passes through the urethra.
The penis consists of:
- root,
- bodies,
- heads.
The skin covering the head is called the foreskin. Two cavernous bodies and one spongy body lie longitudinally, passing into the head of the penis. The spongy part of the urethra passes through the corpus spongiosum. The three parts of the male urethra (prostatic, membranous and spongy) serve to remove urine and semen.
The scrotum is a skin-muscular sac where the testicles are located. The skin of the scrotum is thin, folded, with a large number of sweat and sebaceous glands. Under the skin is a fleshy membrane containing bundles of smooth muscle tissue. The scrotum is divided by a septum into two sections, each of which contains a testicle.
The sex glands are classified as mixed secretion glands. The male reproductive gland is the testis (testicle). It has the shape of a somewhat compressed ellipsoid. The testes are the place where the process of spermatogenesis occurs, which results in the formation of sperm. Male sex hormones are synthesized in the testes. The wall of the convoluted tubule consists of two types of cells: those that form sperm and those that participate in the nutrition of sperm. Sperm enter the epididymis through the efferent tubules and then into the vas deferens. Both vas deferens pass into the ejaculatory ducts, which enter this gland, pierce it and open into the urethra.
In the female gonads - the ovaries - the process of egg formation occurs - oogenesis (ovogenesis).
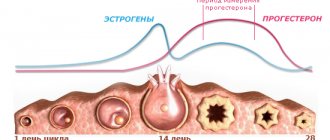
In women, the sexual cycle manifests itself in menstruation. The first menstruation appears after the maturation of the first egg, the bursting of the Graafian vesicle and the development of the corpus luteum. The sexual cycle lasts on average 28 days. It is divided into 4 periods:
- restoration of the uterine mucosa within 7–8 days, a period of rest;
- proliferation of the uterine mucosa and its enlargement for 7–8 days, preovulation, caused by increased secretion of folliculotropic hormone of the pituitary gland and estrogens;
- secretory - release of a secretion rich in mucus and glycogen in the uterine mucosa, corresponding to the maturation and rupture of the Graafian vesicle, ovulation;
- rejection, or post-ovulation, lasting an average of 3–5 days, during which the uterus contracts tonically, its mucous membrane is torn off in small pieces and 50–150 ml of blood is released.
The last period occurs in the absence of fertilization.
Male and female sex hormones are produced in approximately equal quantities in girls and boys. By the time they reach puberty, girls produce several times more sex hormones than boys. In young men, the secretion of male sex hormones increases. Precocious puberty is inhibited by the thymus gland, which functions as an endocrine gland until puberty.
Male sex hormones - androgens (testosterone, androstenediol, etc.) are formed in Leydig cells located in the interstitial tissue of the testes and in the spermatogenic epithelium. Thanks to testosterone and its derivative androsterone, the following occurs:
- development of the reproductive apparatus and growth of the genital organs;
- development of secondary sexual characteristics: deepening of the voice, changes in physique, appearance of hair on the face and body;
- affect the level of protein and carbohydrate metabolism, for example, they reduce the synthesis of glycogen in the liver.
Female sex hormones - estrogens (estrol, estriol and estradiol) are regulators of the ovarian-menstrual cycle, and when pregnancy occurs, regulators of its normal course. Estrogens influence:
- development of genital organs;
- egg production;
- determine the preparation of eggs for fertilization, the uterus for pregnancy, and the mammary glands for feeding a child;
- ensure intrauterine development at all stages.
Estrogens increase glycogen synthesis in the liver and fat deposition in the body. Androgens and estrogens affect bone growth, practically stopping it.
Why can female sex hormones estrogens be called hormones of youth?
- Estrogens control both the formation of the entire female reproductive system and its basic functions. They are the ones who make a woman reproductive , and with a decrease in their number, the ability to conceive and bear fruit disappears.
- Regulate lipid metabolism , reducing the level of bad cholesterol (low-density lipoproteins) in the blood and increasing the level of good cholesterol (high-density lipoproteins). Thanks to this, they prevent the development of atherosclerosis, maintain blood vessels in good condition , which ensures good conductivity of nutrients to all organs and tissues.
- Participate in protein metabolism : stimulate the production of globulin, protein, fibrinogen, etc.
- Prevents increased blood clotting (thickening) and the formation of blood clots.
- Maintain normal water-salt balance.
- Thanks to the above, they maintain the beauty and health of skin, hair and nails .
- Estrogens maintain normal bone density : they inhibit the activity of osteoclast bone cells, which are responsible for the resorption (destruction) of bone tissue and stimulate the growth of bone tissue. That is why one of the pronounced negative consequences of menopause is the development of osteoporosis.
Progestins – pregnancy hormones
Progestins are steroidal female sex hormones, the main role of which is to ensure conception and pregnancy. They are also called gestagens or progestogens . The corpus luteum of the ovaries, partly the adrenal cortex and the placenta during pregnancy, are responsible for their production. In men, progesterone is produced by testicular tissue and the adrenal cortex in small but constantly maintained quantities. In women, progestin levels depend on the period of the menstrual cycle or pregnancy.
It is gestagens that prepare the uterus to accept and secure a fertilized egg. Then they stabilize the metabolism, creating comfortable conditions for the fetus; strengthen the muscles that will be involved in childbirth; provide lactation.
They also participate in the formation of the mammary gland and contribute to the transformation of the breast from a conical shape in girls to a round shape in women. So if your breasts are your special pride, you should thank gestagens.
Progestins reduce estrogen activity , which sometimes poses a number of threats to the female body. So, if estrogens can contribute to the dangerous growth of the endometrium and mammary glands, including oncology, then gestagens prevent these processes. Normal levels of progestins reduce the risks of cystic fibrosis of the breast, mastopathy, endometrial hyperplasia and cancer, and breast cancer. In addition, they normalize blood sugar levels.
A lack of gestagens can be felt in the form of painful periods, chronic inflammation of the reproductive organs, non-menstrual uterine bleeding, miscarriage or post-term pregnancy, and fetal underdevelopment. An increase in their level is also dangerous: it is fraught with cycle disorders, bleeding, corpus luteum cyst, deterioration of kidney function, and improper development of the placenta.
Production of female and male hormones by the sex glands
The gonads produce special components that ensure the development and functional characteristics of biological sex characteristics of the female or male type.
The signaling biologically active chemicals are called hormones, and the organs that produce these secretions in humans are the gonads.
They produce sex gametes, which in the female body are represented by the ovaries, and in the male body by the testes.
Women's
The basic female hormones of the sex glands are estrogen, oxytocin, estradiol, progesterone and prolactin. They affect the functioning of the organs and systems of the woman’s body.
Progesterone and estrogen are the main ones and take part in many processes, from conception to bearing a child. The condition of the skin, hair and overall well-being will also depend on hormonal levels.
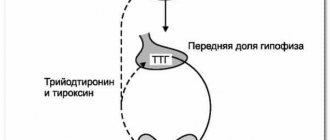
The pituitary gland, which regulates the activity of the sex glands, is the central organ of the human endocrine system.
Estrogens and progestins
Estrogens and progestins are the most important for a woman’s body. This is a separate group of substances produced in the gonads - ovaries. They are responsible for the formation of the figure, roundness and are able to influence the character.
Estrogens actively participate in the processes of renewal of the cellular structures of a woman’s body, allowing her to keep her skin elastic and healthy for a long time, and maintain the shine and thickness of her hair. In addition, estrogens actively participate in the protective barrier of vessel walls to prevent increased cholesterol deposition.
Insufficient production of the hormone estrogen can provoke increased hair growth on the face, hands and entire body. In addition, the skin fades much faster, and fatty deposits accumulate.
https://www.youtube.com/watch?v=7sd61TJTpXo
Estrogens are found not only in the gonads, but also in other organs - muscle fibers, kidney and liver structures. They are able to stimulate the tone of the uterus during childbirth, and after the birth process they allow you to accelerate the return of the organ to physiological size and the separation of the placenta.
Under the influence of estrogens in the bloodstream, the total number of red blood cells and the content of iron-containing protein significantly increases, accelerating blood clotting and significantly reducing the likelihood of large blood loss during childbirth.
The regulation and formation of estrogens is carried out by gonadotropic hormones of the pituitary body - follicle-stimulating hormone (FSH) and luteinizing hormone (LH), as well as prolactin and special substances secreted by the hypothalamus.
Progesterone
This type belongs to gestagens. This is the next group of sex hormones inherent in the female body. It includes an important element - progesterone, formed by the corpus luteum of the ovary.
The concentration of progesterone in the bloodstream begins to increase 2-3 days after the release of the egg from the ovary, as soon as the corpus luteum becomes active, and reaches its maximum concentration on the 14th day of the cycle. In the absence of fertilization, the corpus luteum succumbs to involution, and hormonal activity comes to naught.
Gestagens have various effects, inhibiting the functional centers of the brain responsible for the release of lutropin and the onset of ovulation.
Under the influence of progesterone, the base and muscle layers of the uterus loosen, weakening the contractile function. This allows the embryo to attach to the wall of the organ for further maturation. Progesterone begins to suppress the effect of estrogen, enhancing the formation of glandular cells of the uterus, increasing their secretory characteristics.
In addition, progesterone is actively involved in the development of the alveoli of the mammary glands. After a successful birth, its level in the bloodstream decreases, which allows the concentration of prolactin, which is responsible for milk production, to increase.
Estradiol
One of the important female sex hormones, related to estrogens. Estradiol is normally responsible for the reproductive ability of the female body.
Estradiol is produced in the follicles, corpus luteum of the ovaries, and also in the adrenal cortex. During the process of bearing a child, this substance is formed in the placenta. The production of the hormone is due to the work of FSH and LH (pituitary hormones).
Its concentration in blood serum increases during the follicular stage of the menstrual cycle. As ovulation ends, estradiol levels begin to decrease and then increase again as a new corpus luteum forms.
Estradiol deficiency can provoke the following changes in women:
- absence of a menstrual cycle for more than 6 months.
- reduction in the size of the mammary glands and uterus.
- dry skin.
- problems conceiving a child.
Prolactin
Prolactin is a lactotropic biologically active substance, sometimes called mammotropin. This is one of the hormones secreted by the acidophilic cells of the anterior pituitary gland.
Prolactin is needed, first of all, for lactation. It stimulates the release of colostrum, its maturation and transformation into mature breast milk.
In addition, prolactin is involved in stimulating the growth of mammary glands.
Note! An increase in the level of prolactin concentration that is not associated with pregnancy and lactation requires contacting a specialist. Excess prolactin has a negative effect on the human body.
Oxytocin
Belongs to the group of peptides. It is formed in the posterior part of the pituitary gland, accumulates to the required amount, and then is released into the bloodstream. The production of oxytocin increases the stimulation of the smooth muscles of the uterus, increasing the activity of contractions and the tone of the myometrium.
Under the influence of oxytocin, milk produced by prolactin begins to be released. The hormone entering the mammary glands with blood helps fluid pass through the subalveolar ducts. After the end of feeding, oxytocin enters the hypothalamus through the spinal nerves.
High levels of oxytocin during the final weeks of pregnancy are a signal for the onset of labor. During the research, it became known that the hormone contributes to the formation of maternal instinct.
In men who are close to the child immediately after birth, oxytocin levels also increase, which is responsible for emotional attachment. In addition, it reduces stress levels when a child is born.
Note! Stimulation of oxytocin production occurs through nerve receptors in the skin. It is called the hug hormone.
Men's
Male sex hormones are responsible for the formation of sexual characteristics and reproductive function. Androgens can also be found in the female body, but their concentration is extremely low.
They have two functions:
- Androgenic.
- Anabolic.
Anabolic is responsible for the development of the muscle and bone skeleton, androgens are responsible for sexual desire.
Androgens
This type is necessary for the normal development and maturation of sperm, their motor activity and the identification of sexual behavioral characteristics.
Androgens affect metabolic processes, having an anabolic effect, increasing protein formation in various tissue structures, especially in muscle fibers.
But androgens can also reduce fat content in internal organs, increasing metabolic processes.
The male gonads produce hormones:
- Testosterone.
- Androstenidone.
- Androsterone.
- Dehydroepiadrosterone.
The most active and important is testosterone.
Testosterone
Testosterone is a steroid type androgen. It is sometimes called an anabolic steroid. The hormone is produced in the testes, and the process is controlled by the pituitary gland and hypothalamus.
The basic role of androgen is that it takes part in the development of the reproductive organs in men and is responsible for reproductive function, as well as male characteristics, such as the timbre of the voice, the size of the genitals, and the growth of hair on the face and trunk during puberty.
Source: https://endometriy.com/sekret/vyrabotka-zhelezy
Other female sex hormones
Ovarian hormones inhibins are not steroidal, but peptide in nature. Their normal level is important for maintaining the viability of eggs and their ability to fertilize. A decrease in the amount of inhibins can lead to miscarriage, polycystic ovary syndrome, and with the onset of menopause - to the development of tumors. The cause of inhibin deficiency can be following strict diets and anorexia. These are not specifically female hormones; in men they play an important role in spermatogenesis.
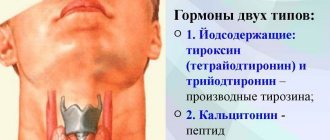
Sex hormones also include hormones that are not produced by the reproductive system, but are involved in the regulation of its functions. This:
- Gonadorelin (GnRH) produced by the hypothalamus. It enhances the pituitary gland's synthesis of so-called gonadotropic hormones - luteinizing and follicle-stimulating.
- themselves are luteinizing and follicle-stimulating hormones , produced by the pituitary gland, as well as human chorionic gonadotropin , produced by the placenta. The function of the first two hormones is to regulate the activity of the gonads in both women and men. And human chorionic gonadotropin (hCG) is normally produced only in pregnant women from the beginning of conception, reaching its peak around the end of the second month of pregnancy. After week 11, hCG levels drop. Detection of hCG in men or non-pregnant women may indicate a tumor.
- Prolactin is produced by the pituitary gland and acts primarily on the mammary glands: it participates in their growth and formation, and ensures lactation. Interestingly, receptors for this hormone are scattered throughout the body. They are found in the heart, lungs, liver, uterus, kidneys, skin, skeletal muscles, pancreas, skin, central nervous system, etc. However, their role there is not entirely clear to modern science.
When a newborn is first applied to the mother's breast, it is prolactin that enters the blood in large quantities and gives the order for milk production. Interestingly, babies can also secrete droplets of colostrum from their papillae, which are popularly dubbed “witches’ milk.” This is a consequence of the fact that the mother’s body shared its prolactin with the fetus. Men also have prolactin in their bodies. It helps representatives of both sexes achieve orgasm.
We looked at the main female sex hormones. With a stretch, this group can also include melatonin , somatostatin , insulin, glucocorticoids, thyroid and other hormones that indirectly affect the functioning of the reproductive system. However, their main functions are not related to reproduction, so they will remain outside the scope of this article.
Structure and functions of the female reproductive glands
primary follicles. During puberty and puberty (from 10-12 to 45-55 years), some primary follicles begin to increase in size and produce hormones. Such follicles are called secondary or maturing.
During the generative period in women, only 400 - 500 follicles mature. The frequency of follicle maturation is on average one follicle every 28 days (from 21 to 35 days), this is the duration of the menstrual cycle.
The mature follicle is called the Graafian vesicle. On the 14th day of the menstrual cycle, Graafian vesicle ruptures - ovulation, in which a mature egg is released into the peritoneal cavity. At the site of the follicle that ruptured after ovulation, the so-called corpus luteum develops - a temporary additional endocrine gland that produces gestagens (progesterone) - the hormone for maintaining pregnancy. It creates conditions for the fertilization of the egg, its implantation (introduction into the wall of the uterus) and the subsequent development of the fetus.
If fertilization does not occur, then such a corpus luteum releases gestagens into the blood before the start of the next menstrual cycle and is usually called the menstrual corpus luteum, which functions until the start of the next menstrual cycle.
In the case of fertilization of the egg, the corpus luteum of pregnancy is formed, which performs an endocrine function throughout the entire period of pregnancy. The most significant role of the corpus luteum is until 12-16 weeks of pregnancy, then the placenta is formed and the main role in the production of this hormone passes to this provisional organ.
After the cessation of endocrine function, the corpus luteum undergoes involution (reverse development) and a scar remains in its place - a whitish body.
Estrogens are produced by maturing follicles. They ensure the development of the genital organs and the formation of secondary sexual characteristics according to the female type.
Mixed glands also include the sex glands. The testis (testicle) has the shape of a somewhat compressed ellipsoid. In an adult, its weight at an average age is 20-30 g. In children, the weight of the testicle (g) at 8-10 years is 0.8; 12–14 years—1.5; 15 years old - 7.
The testicles grow rapidly up to 1 year and from 10 to 15 years.
The period of puberty for boys is from 15-16 to 19-20 years. It fluctuates individually. The outside of the testicle is covered with a fibrous membrane, from the inner surface of which a growth of connective tissue wedges into it along the posterior edge. From this growth thin connective tissue crossbars diverge, which divide the gland into 200-300 lobules.
The lobules are divided into: 1) seminiferous tubules and 2) intermediate connective tissue. The wall of the convoluted tubule consists of two types of cells: those that form sperm and those that participate in the nutrition of developing sperm.
In addition, the loose connective tissue connecting the tubules contains interstitial cells. Spermatozoa enter the epididymis through the straight and efferent tubules, and from it into the vas deferens. Above the prostate gland, both vas deferens become the ejaculatory ducts, which enter this gland, pierce it and open into the urethra.
The prostate gland (prostate) finally develops around age 17. Weight for an adult is 17-28 g.
Rice. 96. Male genital organs: 1 - testicle, 2 - epididymis, 3 - vas deferens, 4 - seminal vesicle, 5 - bladder, 6 - prostate gland, 7 - opening of the ejaculatory duct, 8 - urethra, 9 - Cooper's glands, 10 - cavernous bodies of the penis, 11 - cavernous body of the urethra, 12 - glans penis Spermatozoa are highly differentiated cells 50-60 microns long, which are formed at the beginning of puberty from the primary germ cells of spermatogonia.
The sperm has a head, neck and tail.
How to normalize a woman's hormonal levels?
Hormonal disruptions due to overload, illness, and menopause can put a woman’s health under serious threat. Fortunately, not only do hormones affect us, but we can also influence them. The main thing is not to make a mistake when choosing a method for correcting hormonal levels, since not all of them are safe.
Modern medicine boldly interferes with natural endocrine mechanisms thanks to the fact that science has learned to synthesize artificial hormones. Hormone replacement therapy (HRT) promises to equalize the balance of hormones, prolong youth, restore bone strength, etc. However, HRT has two significant disadvantages:
- the introduction of ready-made hormones disables the mechanisms of their own production, therefore, if hormone replacement is abandoned, the situation worsens and all diseases attack with even greater force;
- negative side effects of HRT include oncological diseases of the reproductive organs, cardiovascular pathologies, increased thrombus formation, etc. (for more information about HRT, see here).
How, if necessary, can you increase the level and balance female sex hormones in a safe way? An alternative method to hormone replacement was proposed by Russian scientists. It turns out that there already exists a natural substance rich in hormonal precursors, from which the human body itself draws exactly as much material to create its own hormones as it needs. This is a drone brood used in the East for centuries - a donor of entomological estradiol (up to 847.9 nmol/100 g), prolactin (up to 475.4 nmol), progesterone (up to 60 nmol) and testosterone (up to 0.322 nmol).
As you can see, this bee product is extremely rich in material for creating female estrogens. It also increases testosterone, which was established in a study described in the dissertation of L. A. Burmistrova. Note that it is testosterone, as an anabolic hormone, that plays a decisive role in restoring bone formation in osteoporosis, a typical manifestation of menopause.
Drone brood not only supplies the body with prohormones, but also acts on the pituitary gland, stimulating its own hormone production. This is a fundamentally different mechanism of action than hormone replacement. There is no talk of withdrawal syndrome or dangerous “side effects” here. This is a gentle correction of the endocrine system, and not a gross invasion with accompanying disruption of natural hormonal mechanisms.
While biochemists are struggling to reinvent the bicycle that nature has already created (that is, safe hormone substitutes), you can normalize your hormonal levels today with the help of unique preparations based on drone homogenate. Osteomed , Osteomed Forte and Osteo-Vit D3 will help you not only improve endocrine functions, but also strengthen bones, teeth, hair and nails, and generally improve the health of the body and prevent the approach of old age.
USEFUL TO KNOW:
ABOUT JOINT DISEASES
How to avoid joint pain?
JOINTS Author: admin625.12.2018Leave a comment
No one thinks about how to avoid pain in the joints - the thunder hasn’t struck, why install a lightning rod. Meanwhile, arthralgia - the name of this type of pain - affects half of people over forty and 90% of those over seventy. So preventing joint pain is something worth considering, even if you...
Read more
ABOUT HORMONE THERAPY
The power of hormones. What active substances regulate cartilage restoration?
HORMONES Author: admin1110.12.2018 Leave a comment
A person’s condition and the coherence of the organs of his body are largely determined by hormonal balance. Cartilage restoration is also subject to the influence of ubiquitous life regulators. Without normalizing hormonal levels, complete regeneration of the joint is impossible. What strings does the invisible puppeteer, the endocrine system, pull, influencing cartilage tissue? Testosterone This hormone is produced by the gonads and the adrenal cortex, as in...
Read more
ABOUT BONE DISEASES
Fracture of the leg: symptoms and treatment. How to recover in a short time?
BONES Author: admin1112.08.2020
Fractures of the lower leg are a fairly common injury in the practice of a surgeon. It accounts for 10% of all other fractures. How quickly the bones heal and what treatment methods the doctor chooses depends on the complexity of the fracture, its location and the general health of the patient. It usually takes three to four months to restore bone integrity. However, modern science can significantly speed up this process.
Read more
ABOUT CONNECTIVE TISSUE DISEASES
ABOUT VITAMINS FOR BONES
May there always be sunshine! What is vitamin D for?
VITAMINSAuthor: admin311.12.2018Leave a comment
Sunlight for a person is not only a source of good mood, joy and happiness. When it comes into contact with the retina and skin, a large number of physiological processes are triggered in the body, for example, the synthesis of calciferol. What is vitamin D for, besides improving calcium absorption? How to compensate for its deficiency if exposure to ultraviolet rays of the sun is undesirable for a person? For…
Read more
DIAGNOSIS OF OSTEOPOROSIS
Sex hormones in a broad sense [edit | edit code]
In a slightly broader sense, sex hormones are generally all hormones produced by the sex glands, not only sex steroids, but also, for example, ovarian inhibin.
In the broadest sense, the concept of sex hormones includes all hormones that are directly related to the physiological regulation of reproductive function, both hormones produced by the gonads and gonadotropin-releasing hormone, gonadotropic hormones, prolactin. Here, with some degree of convention, one can include the pineal gland hormone melatonin, which is a kind of “gonadostatin”, functionally similar to somatostatin in the somatotropic axis, for the gonadotropic axis.
Despite the fact that almost all hormones influence certain aspects of reproductive function (for example, insulin increases steroidogenesis in the ovaries, glucocorticoids reduce the sensitivity of tissues to sex steroids, thyroid hormones increase it, etc.), they are not classified as sexual even with the broadest interpretation of the term, since the regulation of reproductive function is not the only or even the main physiological role of these hormones.
A significant factor that affects the internal processes and condition of each representative of the fairer sex is hormonal levels.
Female hormones are a priority component that can affect physiological characteristics, reactions, emotions, hair/eye color, and growth.
In addition, these active components regulate a woman’s behavioral habits, her thinking and character.