Published: 10/10/2016
Crohn's disease is a nonspecific inflammatory relapsing disease characterized primarily by granulomatous, necrotic-ulcerative and cicatricial-stenotic processes in the wall of the digestive tract, usually affecting a limited segmental nature.
The etiology and pathogenesis of Crohn's disease remain unknown. Apparently, the most likely cause of the disease is viral, as well as secondary bacterial damage to the intestine against the background of immunological sensitization of the body.
Etiology
The following etiological factors can lead to the development of an inflammatory process in the ileum:
- intoxication of the body with toxic substances, medications, poisons;
- consequences of intestinal surgery;
- exposure to rotavirus and enterovirus infections;
- damage to the intestine by opportunistic or pathogenic microflora.
Predisposing factors for the development of intestinal ileitis include:
- unhealthy diet - the diet is dominated by fatty, fried, spicy foods;
- excessive consumption of alcoholic beverages and surrogates;
- smoking;
- the presence of gastroenterological pathologies of a chronic nature;
- long-term use of certain medications.
In addition, ileitis may not be a separate disease, but a symptom of ulcerative colitis, typhoid fever and tuberculosis.
Symptoms of terminal intestinal ileitis
Many patients with diagnosed nonspecific pathologies of the digestive organs often have a question: how to recognize this inflammatory disease of the ileum? This question is quite complex, because the symptoms of terminal ileitis are very similar to other diseases, and accurate research is necessary to determine the diagnosis.
In addition, this pathology of the digestive organs is almost always accompanied by manifestations that seem foreign at first glance: joint or kidney pain, inflammatory processes developing on the skin and mucous membranes, and eye pathologies. But, despite the fact that such symptoms are very difficult to attribute to the development of terminal ileitis in the body, some of them should alert the patient and set him up to visit a specialist to clarify the diagnosis. The main signs that usually accompany the development of this disease and their intensity roughly indicate its stage are the following:
- Unreasonable loss of appetite and severe weight loss;
- Attacks of nausea, always turning into vomiting;
- Pain in the ileum, reminiscent of colic;
- An increase in temperature to 39-40 degrees and a feverish state that occurs for no apparent reason;
- Cramping pain reminiscent of an attack of acute appendicitis.
All these alarming symptoms correspond to the development of catarrhal inflammation in the ileum. Moreover, one should remember the fact that the more clearly these manifestations of the development of the pathological process are expressed, the more severe the form of ileitis.
Chronic ileitis is always characterized by its gradual onset and fairly moderate severity of symptoms. Complaints of patients with developing terminal ileitis usually boil down to the presence of moderate pain localized in the right iliac region, bloating accompanied by sound effects, yellowish watery stool with inclusions of undigested food.
Consequences of reflux ileitis
If, despite the alarming symptoms, the patient does not consult a specialist to clarify the diagnosis and begin appropriate treatment, ileitis will take a chronic form and will torment the person for the rest of his life. With insufficient treatment of the disease, the destruction of the intestinal mucosa becomes progressive, and this is fraught for the patient with the development of very severe symptoms that always accompany terminal reflux ileitis. Among them, the most common are the following:
- Bloody diarrhea with mucus;
- Acute attacks of pain;
- Fever.
In addition, if appropriate therapy is not used for the development of this pathology, the inflammatory process will spread to other organs of the digestive tract, provoking the formation of numerous erosions and ulcers and the occurrence of intestinal obstruction. In addition, ignoring the development of terminal ileitis leads to the formation of such a terrible defect in the body as fistulas. They penetrate into neighboring organs and cause large amounts of protein deposits to accumulate in them, which disrupts metabolic processes. With such development of ileitis, urgent surgical intervention cannot be avoided.
Treatment and diet for terminal ileitis
Despite the fact that it is quite difficult to interpret all the conflicting information about the immunological status of such a type of Crohn's disease as terminal ileitis, which develops in the ileum and is accompanied by catarrhal inflammation, it is thanks to immunomorphological studies that the opportunity has arisen to substantiate active therapies. And this allows for adequate treatment of this pathology of the ileum.
It places a special emphasis on patients taking medications such as corticosteroids and antibacterial drugs, and, for certain indications, other immunosuppressants. In addition, this disease also uses a large arsenal of various symptomatic drugs necessary for the treatment of ileitis: psychotropic, blood substitutes, anti-inflammatory and others.
Very important in the adequate treatment of this disease is given to an optimal diet, as well as an appropriate diet, because all specialists know very well that this pathology cannot be completely cured and you can only freeze the pathological process for some time.
Proper dietary nutrition for such a type of Crohn's disease as ileitis is of great importance. It is thanks to it that it becomes possible to facilitate the work of the digestive organs, as well as eliminate the possibility of additional injury to the intestinal mucosa.
This is the only way to stop the formation of new erosive lesions and scars on its walls. This is facilitated by the fact that all dishes included in the patient’s diet are very easily digestible, high in calories, and contain large amounts of vitamins and fluids necessary for the damaged digestive organ.
Classification
Due to the formation of the disease, the following forms of this pathological process are distinguished:
- parasitic;
- infectious;
- drug;
- toxic;
- enzymatic;
- nutritional;
- postoperative.
According to the criterion of localization of the lesion, the following forms of this disease are distinguished:
- isolated;
- with damage to the colon and stomach;
- with damage to the entire intestine.
Ileitis is also distinguished between primary and secondary (arising against the background of existing gastroenterological pathologies) type.
Based on enzymatic activity, this intestinal disease can be atrophic or non-atrophic.
According to the nature of the intensity of the lesion, the disease can occur in the following forms:
- light;
- medium-heavy;
- heavy;
- with complications.
Forms of ileitis
If chronic ileitis is diagnosed, then a distinction is made between the stages of exacerbation, complete and incomplete remission.
Causes
The causes of Crohn's disease have not yet been established, which makes the patient's condition incurable. You can stop the disease and its symptoms. However, there are other factors that provoke the development of ileitis of the ileal mucosa:
- Secondary infection due to weakened immunity;
- Poor nutrition;
- Penetration of viruses and bacteria;
- Poisoning with poisons, toxins, heavy metals;
- Sedentary (passive) lifestyle;
- Genetic predisposition;
- Improper functioning of the valve between the small and large intestines;
- Metabolism problems;
- Drug abuse;
- Pathologies in the structure of the digestive system.
The chronic form develops due to the lack of proper treatment. Neglecting one’s own health leads to the development, rather than extinction, of the disease. In this case, the chronic form is observed in people with a genetic predisposition. Doctors do not discount the influence of bad habits - alcoholism and smoking. These factors affect the general condition.
Symptoms
At the initial stage of development, the disease may be asymptomatic. The patient may occasionally be bothered by minor disturbances in the gastrointestinal tract, which are usually attributed to poor nutrition.
The acute form of this disease manifests itself in the form of the following symptoms:
- bloating, rumbling;
- diarrhea – frequency of bowel movements up to 10 times a day;
- nausea, which is often accompanied by vomiting;
- increased body temperature;
- weakness;
- headaches for no apparent reason.
It should be noted that a similar clinical picture can be observed with other intestinal diseases, so you cannot take treatment on your own. Unauthorized treatment measures without an accurate diagnosis can lead to the development of serious complications.
The chronic form of this gastroenterological disease has a less pronounced clinical picture and manifests itself as follows:
- attacks of moderate pain in the iliac region, often localized around the navel;
- watery stools that often contain particles of undigested food. Unlike the acute form of the disease, it does not appear so often;
- weight loss, which is caused by metabolic disorders, impaired absorption of vitamins and minerals;
- symptoms of hypovitaminosis.
A similar clinical picture in adults can also be a manifestation of ulcerative colitis or Crohn's disease, so you should urgently seek medical help and not self-medicate or ignore these symptoms. Prolonged bouts of diarrhea can lead to complete dehydration of the body, which is also fraught with the development of serious complications.
Crohn's disease - symptoms
The clinical manifestations of the presented pathology correspond to its degree, localization and duration of the inflammatory process, the frequency of relapses and other factors. There are some nonspecific signs that accompany terminal ileitis - general symptoms:
- fever or wave-like increase in temperature;
- weakness;
- constant fatigue;
- weight loss;
- stomach ache;
- lack of appetite;
- diarrhea lasting more than 6 weeks.
Terminal catarrhal ileitis
This type of disease is characterized by inflammation only of the mucous membranes of the gastrointestinal tract. Catarrhal Crohn's disease may be accompanied by intestinal and extraintestinal symptoms. The first group of clinical manifestations includes:
- pain simulating acute appendicitis;
- nausea;
- anorexia;
- vomiting;
- bloating;
- chronic diarrhea.
Extraintestinal signs of Crohn's disease:
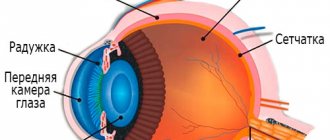
- conjunctivitis, uveitis or keratitis;
- aphthous stomatitis;
- sclerosing cholangitis;
- cirrhosis;
- pyelonephritis;
- fatty liver;
- cholelithiasis;
- cystitis;
- hydronephrosis;
- cholangiocarcinoma;
- kidney amyloidosis;
- nephrolithiasis.
Terminal follicular ileitis
A large number of Peyer's patches are located in the submucosal layer of the small intestine and ileum. These are special lymphoid follicles designed to produce immunoglobulins. Terminal ileitis often affects such structures, resulting in the already listed symptoms and additional clinical manifestations:
- exposure to frequent infections, especially viral ones;
- ankylosing spondylitis;
- erythema nodosum;
- pyoderma gangrenosum;
- angiitis;
- adhesions;
- monoarthritis;
- peritonitis;
- fistula tracts;
- intra-abdominal abscesses;
- narrowing of the lumen and intestinal obstruction;
- sustained increase in body temperature.
Erosive terminal ileitis
The Crohn's disease in question is characterized by the formation of deep ulcerations on the mucous membranes of the gastrointestinal tract. Inflammation in combination with erosive processes is considered one of the most dangerous forms of terminal ileitis, leading to dangerous and life-threatening consequences. Peptic ulcer Crohn's disease - manifestations:
- perforation of the intestinal walls;
- internal bleeding;
- toxic megacolon;
- abscesses as a result of secondary infection.
Diagnostics
If you have the above-described clinical picture, you should contact a gastroenterologist. After clarification of complaints, medical history and physical examination, a diagnosis is carried out, which includes the following laboratory methods:
- general and biochemical blood test;
- stool occult blood test;
- virological and bacteriological examination of stool.
To make an accurate diagnosis, the most informative instrumental method will be contrast radiography with barium, which can determine impaired intestinal motility, as well as intestinal obstruction.
To exclude other gastrointestinal ailments, the following are carried out:
- Ultrasound of the abdominal organs;
- FEGDS;
- MSCT;
- endoscopy.
Carrying out FEGDS
Based on the results of the examination, a final diagnosis is made and the most appropriate treatment tactics are selected.
Ileitis - what is it?
Ileitis is an inflammation localized mainly in the final part of the small intestine and covering adjacent tissues.
Leads to the formation of polypoid or scar-ulcerative formations. It affects not only the thermal part of the small intestine, but also the duodenum, jejunum, and colon. Mostly, ileitis is diagnosed in people aged 20 to 40 years, more often in men. It occurs two times less often in rural populations than in residents of large cities. According to scientific data, in 70% of cases, pain in the right iliac region is a symptom of chronic ileitis. In general, the described pathology accounts for 6% of all intestinal inflammation.
Classification of ileitis
According to the criterion of damage to the small intestine, the following are distinguished:
- isolated ileitis;
- ileitis, combined with inflammatory processes in the stomach and colon;
- ileitis affecting the entire intestine.
Due to the occurrence of ileitis, it happens:
- parasitic;
- medicinal;
- infectious;
- enzymatic;
- nutritional;
- postoperative;
- toxic.
It can also be primary or secondary (resulting from another gastrointestinal disease).
Taking into account enzymatic activity, doctors distinguish:
- atrophic ileitis;
- non-atrophic ileitis.
According to the characteristics of the course, inflammation can occur with or without complications in three forms:
- light;
- moderate;
- heavy.
Types of ileitis
Depending on the location of inflammation, ileitis is divided into two types:
- First type. These include: damage to only one area of the small intestine;
- damage only to the ileocecal region (the zone of transition of the small intestine to the large intestine);
- damage to only one segment of the colon.
- damage to several parts of the small and large intestine at once;
Forms of ileitis
Taking into account the characteristics of the course of ileitis, gastroenterologists classify it into three forms:
- Primary attack (acute symptoms dominate).
- Chronic intestinal ileitis - there are no acute symptoms, the disease lasts more than six months.
- Recurrent ileitis - symptoms often recur, exacerbations alternate with remission for more than six months.
Depending on the characteristics of the clinical picture, it happens:
- acute ileitis (inflammation of the ileum);
- chronic jejunoileitis, accompanied by impaired absorption of nutrients;
- jejunoileitis, complicated by small intestinal obstruction syndrome (the jejunum and ileum become inflamed, the process of passing feces through the intestines is disrupted);
- granulomatous proctitis (multiple small tumor-like formations form on the wall of the rectum),
- granulomatous colitis (small tumor-like granulomas form on the wall of the large intestine).
Treatment
Treatment of this gastroenterological pathology is only complex - drug therapy is combined with diet. In the acute form of the disease, hospitalization of the patient is implied.
Drug therapy may include taking the following medications:
- means for normalizing intestinal motility;
- astringents;
- probiotics;
- antibiotics.
If the patient experiences severe vomiting and diarrhea, infusion therapy is prescribed to prevent dehydration.
As for nutrition, in most cases, patients are prescribed dietary table No. 4 according to Pevzner. The following are excluded from the diet:
- chicken eggs in any form;
- fatty fish and meats;
- smoked meats;
- dairy products;
- grape;
- White cabbage;
- hot and fatty sauces;
- carbonated drinks.
The patient’s diet does not prohibit the consumption of the following foods:
- yesterday's bread;
- pasta;
- broths from lean meats;
- porridge with water;
- low-fat varieties of fish and meat;
- vegetable soups;
- weak tea, dried fruit compotes without sugar.
This type of nutrition for the patient can relieve acute symptoms and reduce the load on the intestines. In the chronic form of the disease, the diet must be followed constantly. During periods of stable remission, it is possible to expand the menu, but in agreement with the attending physician.
Prevention
Ileitis can be prevented. To do this, it is enough to lead a healthy lifestyle and play sports. At the first, even minor, symptoms, it is better to immediately consult a doctor. Detection of the disease at an early stage is the key to successful treatment.
Ileitis is an acute or chronic disease of inflammatory pathogenesis that affects the tissues of the distal small intestine, also called the ileum. There are isolated and combined forms of ileitis, which is accompanied by lesions in other parts of the intestine. Despite the intense clinical signs expressed in the manifestation of dyspeptic disorders, it is often difficult to differentiate the disease from other pathologies, which leads to the use of incorrect treatment tactics and chronic inflammation.