this is a psychological disorder, the symptoms of which boil down, first of all, to the patient’s obsessive and often unconscious tearing out of hair from his own head and other parts of the body with its subsequent ingestion (an associated complication diagnosed on average in every 10-15th patient).
Characteristic symptoms of deviation arise, as a rule, due to strong emotional experiences and stressful situations. In female patients, the disease is diagnosed on average twice as often as in males. Often the disease affects representatives of younger age groups.
After reviewing the information below, you will learn why symptoms of a disorder such as trichotillomania may occur, how this disease progresses and in what order it is treated.
General information about the disease
The disease under study was first described in 1889. This condition is classified as obsessive neurosis, because its main symptoms first arise consciously in the patient, but over time he almost completely ceases to control them.
The result is baldness of varying severity and quite serious skin damage. Most often, bald spots and bald spots are observed on the scalp, pubic area, limbs, as well as eyebrows, eyelashes and other places. Areas of localization of baldness are usually symmetrical. May be single or multiple.
There are 2 main types of the disease: childhood and adult. The second is characterized by a more complex course and its treatment requires serious efforts. In some cases, patients pull out their own hair even while sleeping.
The typical time of onset and progression of the childhood form of the disease is between 2 and 6 years. Adult trichotillomania primarily affects women and can occur at any stage of life.
Causes of mental deviation
Before starting treatment for a disease, you need to establish what caused its symptoms - this statement is true for any disease, and trichotillomania is no exception.
The main provoking factor is severe stress and constant psycho-emotional tension.
Patients often develop a parallel habit of biting their nails, this is especially true for children. Parents scold such children for such habits, trying in every possible way to wean them, not realizing that the culprit is not the child’s harmfulness, but a psychological disorder.
Otherwise, the reliable causes of this deviation remain unknown. Experts identify the following points as provoking factors:
- insufficient copper and iron content in the body;
- neurosis-like conditions, exposure to regular stress;
- depressive states;
- schizophrenia;
- head injuries;
- obsessive-compulsive disorders;
- conditions accompanied by instability and mental imbalance;
- childhood mental trauma;
- pathologies of organs and endocrine glands;
- various inflammations;
- allergies to medications;
- chronic tonsillitis.
In each case, nothing indicates impending trichotillomania - the disease is characterized by a sudden onset. At first, the patient develops minor bald spots, which become larger over time. The sizes of the lesions, however, are not subject to standardization and differ for each patient.
To prevent complete baldness, you need to start treatment as soon as possible. The characteristic signs and symptoms of trichotillomania will help you know if you need to see a doctor. More about them later.
Characteristic symptoms and signs of the disorder
The main sign of deviation is bald spots on different parts of the body.
The skin, if you do not take into account the damage caused by hair pulling, remains in normal condition, i.e. without itching, peeling and other adverse effects.
The behavior of patients in most cases is similar: the patient twirls the hair around his fingers, after which he begins to pull it until it is pulled out. Such pulling out allows you to get rid of the anxiety and nervous tension that accompany trichotillomania.
Such actions lead to hair thinning, but the situation reaches complete baldness extremely rarely - in most situations, patients see a doctor on time and receive appropriate treatment.
Hair pulling usually occurs mechanically, i.e. a sick person does not pay much attention to his actions. When stressful and exciting situations arise, the desire to pull out hair increases noticeably. In addition to their own fingers and nails, patients can use tweezers, tweezers and other aids to perform the described actions. It is very important to be able to distinguish the deviation under study from alopecia areata. The symptoms of the latter are complemented by complete baldness.
As noted, after pulling out hair, a person experiences relief and feels satisfaction. Such people, as a rule, do hair pulling alone. However, if a person is in a restless state or finds himself in a stressful situation, outside observers also interfere with him.
According to average statistical data, about 10-15% of patients eat plucked hair. As a result, such “food” accumulates in the stomach and clogs it.
Patients, at the same time, objectively evaluate their appearance and notice changes in the condition of their hair. As a rule, they try to hide their bald spots using scarves, hats and other similar accessories.
Types of disease
According to one version, trichotillomania is not genetically transmitted and is not congenital. This is an acquired illness.
There are three types of trichotillomania in children and adults:
- Transitional - pathological tendency is characterized by stress and strong feelings, based on recently suffered shocks.
- Chronic - observed in those suffering from personality disorder. Hair pulling also occurs during sleep.
- Episodic - attacks occur every time a stressful situation occurs.
Trichotillomania happens:
Concentrated - when the patient consciously prepares to pull out hairs, armed with tweezers.
Automatic - when the patient is not aware of his actions. The consequences may be evident later in the form of bald spots on the head and lack of hair in other areas.
Diagnostic methods
In the process of carrying out diagnostic measures, it is necessary, first of all, to exclude the possibility of syphilis, fungal infections and other diseases, the course of which is accompanied by baldness.
The essence of diagnosis comes down to interviewing the patient and assessing his appearance. The specialist will collect information regarding the following points:
- circumstances that give a person anxiety;
- diseases suffered previously;
- the presence of hereditary diseases in relatives;
- a list of medications taken recently;
- features of the daily routine, diet, physical activity.
After conducting the survey, the doctor will do the following:
- will assess the fat content of the patient’s head;
- will conduct a hair examination for the presence of split ends, fragility indicators, etc.;
- will examine the condition of the patient’s head for the presence of diseases of the dermatological group, i.e. check the skin for peeling, rashes, inflammation, etc.;
- assess the degree of hair damage;
- will find out whether the hair loss in a given patient is scarring or not.
How to treat trichotillomania?
The sooner treatment for trichotillomania is started, the higher the chances of recovery will be.
Along with this, the modern pharmaceutical industry does not have medications designed specifically to combat trichotillomania.
In view of this, treatment is based on the use of methods and means that exclude the possibility of the patient pulling out hair. For example, a person may be advised to shave his head. The method is effective in some situations, but not long-term.
Treatment may also be based on the use of the following techniques:
- wearing a zinc-gelatin cap - it is recommended to wear it at night;
- the use of antidepressants and sedatives, as well as vitamins;
- the use of medications that help restore the normal course of internal metabolic processes;
- use of hormonal ointments;
- undergoing hypnotic sessions, cryotherapy, paraffin therapy.
Among the effective physiotherapeutic methods of influence, one can note x-ray irradiation of the skin areas under which the spinal cord roots are localized. Such an effect is indirect and contributes to some regulation of the activity of the nervous system, calming the patient.
Medicinal effects on patients of younger age groups do not produce particularly positive results. First of all, for the reason that the desire to pull out hair in children in many situations is a reaction of a young patient to an unfavorable atmosphere in the family.
Thus, in order to provide effective treatment, it is necessary, first of all, to get rid of provoking and traumatic factors. The use of physical punishment methods will give strictly opposite results - remember this.
Home treatment for trichotillomania can be carried out using traditional medicine. Before using any of them, we advise you to consult a doctor - otherwise, responsibility for all possible consequences will lie solely with you.
A good example is garlic oil - it is sold in almost every pharmacy. If you wish, you can make this oil yourself. To do this, take a head of garlic, peel it and grind it to a pulp, then mix it with unrefined sunflower oil in the amount of one glass. Squeeze the juice of one lemon and add half of the resulting liquid to the previously prepared mixture. Take orally three times a day in the amount of one small spoon. The recommended course duration is 10-12 weeks.
The second popular folk recipe: finely chop the lemon without peeling it. Mix the resulting mass with the same amount of honey. Add 10-12 apricot kernels to the mixture. We take the product twice a day in the amount of one small spoon.
In some situations, trichotillomania goes away on its own over time and does not even require any treatment. Along with this, if the pathology continues to progress, in the absence of timely medical intervention, the situation can end quite badly - the patient will go bald.
In most cases, the prognosis is positive. Prevention comes down to eliminating the impact of stressful situations and other unfavorable factors on the patient.
Be healthy!
Trichotillomania is a mental disorder that occurs against a background of stress and is characterized by a person’s uncontrollable need to pull out their own hair, and sometimes by subsequently eating it. The risk group is women and children. Psychiatrists classify this disorder as obsessive-compulsive disorder.
Forms of trichotillomania:
- Children's room. It is observed in children aged two to six years.
- Heavy. It is observed in mature women, sometimes in men and adolescents.
Basically, a person pulls out hair from the head, less often from eyelashes and eyebrows, and extremely rarely from the pubic area, armpits and limbs.
The patient can pull out hair with his fingers or any available means. This habit leads to partial or complete pain, as well as associated adverse consequences. To eliminate it, you need to contact a specialist.
PsyAndNeuro.ru
Trichotillomania is a condition in which people experience an obsessive urge to pull out their hair, leading to thinning hair. This disorder affects approximately 0.5-2.0% of the population. In the DSM-5 (and the future ICD-11 - editor's note), trichotillomania is classified under obsessive-compulsive and related disorders.
Behavioral therapy has been successfully used in the treatment of trichotillomania, but not all patients are willing or able to comply with this treatment strategy, so there is a need for effective pharmacological treatment options. Historically, pharmacotherapy for the treatment of this disorder has been largely ineffective, but some findings have emerged in this regard. Fluoxetine, clomipramine, olanzapine, and naltrexone have been used in the treatment of trichotillomania, but evidence of their effectiveness has been varied and side effect profiles have limited practical application. Recent advances in understanding the pathophysiology of trichotillomania, as well as evidence of the effects observed with certain glutamate modulators such as N-acetylcysteine and dronabinol, have provided new potential pharmacotherapy options.
Criteria for trichotillomania in DSM-5:
- Repeated hair pulling leading to hair lossB. Repeated attempts to reduce or stop hair pulling
- Hair pulling causes significant distress or impairment in social, occupational, or other important areas of functioning
- This condition is not associated with other medical diseases (for example, dermatological)
- Hair pulling cannot be explained by the presence of another mental disorder (for example, attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder)
A recent study noted that the average age of onset of trichotillomania differed significantly between men and women. The overall mean age of illness was 17.7 years, the mean age in women was 14.8 years and 19.0 years in men.
The most common places where patients pull out hair are the scalp, eyebrows, pubic area, eyelashes and beard.
Dermoscopic features of trichotillomania include decreased hair density, brittle hairs of varying lengths, coiled or short vellus hair, trichoptilosis (split ends), occasional yellow spots, and absence of hair in the area as in alopecia areata.
Two different types of trichotillomania have been described, "automatic" and "focused", but most people show signs of both types. People with the automatic type are often unaware that they are pulling their hair, while people with the focused type often describe the experience of hair pulling as an integral part of their condition. Patients describe a feeling of pleasure or a decrease in negative emotions during hair pulling.
Three main additional variants of psychodermatological trichises that lead to hair loss have been described: trichotheiromania (rubbing/combing the affected area), trichotheomania (shaving/cutting) and trichodaganomania (hair biting).
Trichotheiromania is often treated with high doses of glucocorticoid creams, with varying effectiveness. A case report showed a good response to N-acetylcysteine treatment in a 47-year-old man who had partial improvement after eight weeks and full hair regrowth after 16 weeks after treatment with 1200 mg N-acetylcysteine per day.
Treatment includes both psychotherapeutic and pharmacological interventions. Treatment recommendations depending on the patient’s age:
- Preschool age. In this age group, trichotillomania is seen as a habit disorder similar to thumb sucking and goes away on its own. Parental support and education about the benign course of the disorder are most effective.
- School age. At school age, behavioral approaches were found to be more effective than pharmacotherapy. Because of the possibility of comorbid psychiatric disorders, psychiatric referral is warranted in this age group.
- Teenagers and adults. The most effective combination of psychopharmacotherapy, behavioral therapy and treatment of concomitant mental disorders
Cognitive behavioral therapy
Behavioral pattern replacement training is a type of CBT that is used as a 1st line of non-pharmacological intervention for trichotillomania. This therapy involves helping the patient become more aware of their hair-pulling behavior and its context, and then replacing that behavior with another behavior—such as making a fist that can be held until the pull subsides. hair pulling.
Stimulus control training
Stimulus control training involves changing a person's environment to make it less conducive to hair pulling. This may include removing things that make hair pulling easier or adding things that discourage the behavior. Examples include removing mirrors or adding an object that occupies the patient's hands, such as a stress ball or spinning object.
Acceptance and Commitment Therapy
Acceptance and Commitment Therapy attempts to help patients achieve hair-pulling behavior in terms of interfering with personal or life goals.
Although there are no FDA-approved medications for the treatment of trichotillomania, due to the condition's comorbidity with other psychiatric disorders, first-line pharmacotherapy usually consists of selective serotonin reuptake inhibitors (SSRIs) or the tricyclic antidepressant clomipramine.
Tricyclic antidepressants
In a placebo-controlled study, Ninan et al found that CBT was more effective than clomipramine and placebo. Clomipramine was found to reduce trichotillomania symptoms more than placebo, but the difference was not significant. However, there has been a case report of successful clomipramine monotherapy at a dose of 125 mg/day and clomipramine 50 mg/day therapy in combination with CBT.
SSRIs
SSRIs are widely used to treat trichotillomania in both adults and children, but evidence of benefit is weak. In animal models, SSRIs have been shown to reduce excessive grooming in mice, the genetic characteristics of which are associated with the pathogenesis of trichotillomania. In human studies, a meta-analysis by McGuire et al found a modest effect with SSRIs in the treatment of trichotillomania. However, a previous meta-analysis showed that clomipramine was more effective than placebo, but this pattern was not observed for SSRIs. A small, open-label, 16-week study showed the effectiveness of fluoxetine at doses up to 80 mg/day in reducing hair pulling, but the study did not include a control group. Placebo-controlled, double-blind studies did not show a significant benefit of fluoxetine compared to placebo. Since people with trichotillomania often have comorbid mental disorders such as depression and anxiety, there is every reason to include SSRIs in the treatment plan for such patients.
Antipsychotics
Antipsychotics have been considered as potential drugs for the treatment of trichotillomania due to their effectiveness in treating tics and the frequent comorbidity of trichotillomania and tic disorders. The most studied drug in the treatment of these patients was olanzapine, but there is evidence of the effectiveness of risperidone and haloperidol. However, we should not forget about the serious side effects that occur during antipsychotic therapy and weigh them against the potential benefits in the treatment of trichotillomania.
Opioid antagonists
The mechanism of action of these drugs in the treatment of trichotillomania is likely to be by reducing the chemical reward of hair pulling. Unfortunately, in a double-blind randomized controlled trial by Grant et al, naltrexone did not show a significant difference in reducing hair pulling compared with placebo in the treatment of trichotillomania, although it did significantly improve cognitive flexibility.
N-acetylcysteine
The mechanism of action of N-acetylcysteine in neurological and psychiatric disorders is not entirely clear, but may help protect against a number of pathological processes such as oxidative stress, neuroinflammation, glutamine and dopamine dysregulation. For impulse control disorders, including trichotillomania, N-acetylcysteine is thought to act primarily by regulating synaptic glutamate levels in the brain and reducing cytotoxicity. Evidence of the effectiveness of N-acetylcysteine in the treatment of trichotillomania varies from study to study. In the two main placebo-controlled studies conducted, one showed a significant benefit over placebo, while the other did not.
A 2009 double-blind, placebo-controlled study that examined N-acetylcysteine in 50 adults with trichotillomania found that N-acetylcysteine at a dosage of 1,200 mg twice daily showed significant benefit compared with placebo.
Because of its relative safety and tolerability compared to other treatments for trichotillomania, such as antidepressants or antipsychotics, and its low cost, N-acetylcysteine may become an important treatment option for those struggling with this disorder. However, further research is needed, including larger, long-term, randomized, placebo-controlled trials with more standardized outcome measures.
Milk thistle
Milk thistle has been shown to have antioxidant properties and is invaluable in the treatment of trichotillomania. A recent double-blind, placebo-controlled crossover study found that milk thistle had no significant benefit over placebo in reducing the severity of trichotillomania as assessed by the National Institute of Mental Health. However, a benefit was found in terms of Global Clinical Impression Scale score and reduction in time spent pulling hair per week. The study involved 20 people aged 12-65 years, 19 of whom were women.
Probiotics
The gut microbiota is thought to influence behavior in several ways. These include effects on vagus nerve signaling (possibly through serotonin synthesis by enterochromaffin cells), mineral metabolism, modulation of circulating cytokine levels, and changes in neurotransmitter turnover. In addition, changes in neurotrophic factor gene expression, SCFA-mediated modulation of G protein-coupled receptors, and changes in the hypothalamic-pituitary axis may also play a role.
Animal studies have shown that gut microbiota may also influence mammalian brain development, including the development of the striatum, which (among other brain regions) is structurally abnormal in individuals with trichotillomania.
Dronabinol
Dronabinol, a cannabinoid agonist, may provide potential benefit in the treatment of trichotillomania by reducing glutamate cytotoxicity in the striatum. In a small open-label study, dronabinol showed a significant benefit in reducing hair pulling in 9 of 12 patients.
Inositol
A proposed potential mechanism of action of inositol on psychiatric disorders is by attenuating serotonin-2 receptor desensitization, as the phosphatidylinositol second messenger system is used by these receptors. In a double-blind, placebo-controlled study, Leppink et al found that inositol had no significant benefit over placebo. The study lasted 10 weeks, and of the 38 participants, the majority were women. 19 patients received inositol, the remaining 19 received placebo.
Trichotillomania is a complex psychodermatological disorder that still requires much research regarding its pathogenesis and pharmacological treatment. Research into the comorbidity and genetics of this condition has shown potential for future research and new strategies for personalized treatment. In addition, some new pharmacotherapy options, including monotherapy or adjunctive therapy, show promise. Notably, N-acetylcysteine appears to be a well-tolerated and safe potential treatment for adults with trichotillomania. Another option includes complementary treatments such as probiotics and the cannabinoid agonist dronabinol, but more research is needed.
Author of the translation: Gadzhieva F.Sh.
Source: Everett GJ, Jafferany M, Skurya J. Recent advances in the treatment of trichotillomania (hair-pulling disorder). Dermatol Ther. 2020;e13818. doi:10.1111/dth.13818
Causes of trichotillomania
To this day, the obvious causes of trichotollomania have not been elucidated. This disease resembles obsessive-compulsive disorder, which manifests itself in the form of obsessive actions to get rid of disturbing thoughts.
Trichotillomania is also positioned as a way to distract from disturbing thoughts, but with a significant difference: a person gets a kind of pleasure from pulling out hair. According to research results, trichotillomania is hereditary.
Provoking factors may be:
- moving;
- change of place of work or study;
- death of a loved one;
- parental divorce;
- the beginning of independent life.
By pulling out hair, the patient attempts to get rid of unpleasant experiences and to gain pleasure.
In some patients, trichotillomania is one of the extreme manifestations of perfectionism. Such people look for “imperfect” hairs on themselves and pull them out. Over time, this becomes a habit and the hairline becomes much less frequent.
Therapy methods
Medical treatment for trichotillomania in children involves psychotherapy and antidepressants in combination with other methods to help improve well-being. A pediatric psychiatrist should take care of the child’s health.
The following methods of influence are also used:
To get rid of the effects of trichotillomania, special hormonal ointments and other means are used.
Symptoms of trichotillomania
The main symptom of the disease is baldness in specific areas of the head. In this case, symptoms such as itching, redness and peeling are not observed. The hair grows back, but the patient will get rid of it again. Soon the hair will thin out, but complete baldness will not occur. By performing this action, a person tries to cope with stress, inaction, anxiety or worry. Pulling out his hair, he gets relief.
There are several types of patients with trichotillomania:
- automatic – hair pulling occurs unconsciously. The process begins during times of extreme stress or exciting activity. It happens that a person does not even notice that he is pulling out his hair; those around him point this out to him and the consequences in the form of bald patches;
- focused. Hair pulling is a specific ritual that requires a lot of attention, preparation and privacy.
Symptoms
Hair pulling in trichotillomania can be conscious or unconscious. By causing pain and physical damage to oneself in this way, a person tries to displace more unpleasant sensations from the psyche - fear, nervous tension, anticipation, and so on.
Interestingly, pulling out hair during trichotillomania brings pleasure to patients - the pain provokes the release of hormones into the blood, which seem to “calm” the nervous system.
The following symptoms are typical for trichotillomania:
- Repetition of episodes of hair pulling in certain situations - for example, hair pulling occurs in moments of fear, nervous tension, or when performing boring, monotonous work.
- A combination of obsessive actions - hair pulling in babies can be accompanied by nail biting, finger sucking, and so on.
- Preliminary actions - before plucking, the hair can be curled around a finger, smoothed, ruffled, and so on.
More severe forms of trichotillomania may be accompanied by deliberate harm to one’s body - in these cases, hair is pulled out not only on the head, but also on the body, and auxiliary means - tweezers, forceps, and so on - can be used for this purpose.
Sometimes hair pulling turns into a ritual action - with its help, patients protect themselves from the evil eye, for good luck, or to protect themselves from something.
Most often, trichotillomania occurs in children who have suffered emotional trauma or are under stress. Hair pulling is unconscious; as a rule, children cannot control themselves and, being in uncomfortable conditions, cause themselves quite severe harm - they may develop bald patches, and then develop complications.
Older children, teenagers and women can become very worried about their “habits” and try to control their neurosis, further aggravating their condition.
Complications
Trichotillomania is dangerous not only in itself, but also because of its complications. Against the background of neurosis, patients may experience secondary consequences: depression, social phobias, anxiety, refusal of social life. Feeling ashamed of their behavior, especially if visible bald patches have appeared, adolescents and adult women refuse to communicate, and they often hide their disorder and stop communicating with others, which is why other behavioral and mental disorders arise.
In addition to psychological ones, somatic pathologies can also develop:
- In place of the torn hair on the head there is alopecia, skin irritation, inflammation and the formation of ulcers due to secondary infection.
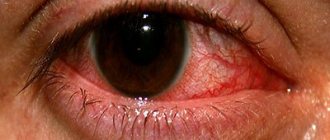
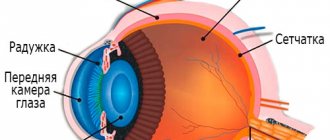
- More serious consequences of tearing out eyelashes are damage to the eyeball and even loss of vision.
- If hair is swallowed, intestinal obstruction may develop, which requires surgical intervention.
Possible complications
Baldness is just one of the complications of trichotillomania, which leads to adverse social consequences. In an effort to hide this habit, a person can become a recluse. Quite often, pathology leads to severe mental illnesses such as depression, attention deficit disorder, anorexia, etc.
The tendency to pull out eyelashes leads to various types of inflammation and infectious eye diseases, the treatment of which can be very difficult.
Another common complication is skin infections.
Various dental and intestinal diseases threaten patients who eat their own hair. Hair is very difficult to come out of the stomach and can form large clumps that can only be removed through surgery.
Treatment of trichotillomania
Before starting treatment, it is necessary to identify the true causes of the disease. Cognitive behavioral psychotherapy helps with this, helping to get rid of a bad habit, increasing the patient’s awareness and increasing his stress resistance.
Treatment of trichotillomania with medications is prescribed only after psychotherapeutic methods have failed.
If hair pulling occurs intensely, the patient is prescribed selective serotonin receptor inhibitors. To treat baldness, various hormonal ointments and other medications are prescribed.
At home, trichotillomania can be treated using folk remedies, the most effective of which is garlic oil. A mixture of lemon zest, honey and apricot kernels will help stabilize your psycho-emotional state and get rid of trichotillomania faster.
Effective treatment must be supported by preventive measures that are aimed at eliminating stress and stabilizing the mental state. Sports, an exciting hobby, and a balanced diet will be useful here.
Be sure to watch this interesting video about trichotillomania:
//www.youtube.com/watch?v=j2gNxaUKcbo
Trichotillomania is the compulsive pulling out of hair on different parts of the body, most often on the head, resulting in obvious patches of baldness. This disorder is quite widespread, especially common in childhood. According to American studies, trichotillomania affects 3.4% of girls and 1.2% of boys.
The most common hair loss experienced by people with trichotillomania is the scalp. Less commonly, eyebrows and eyelashes can become objects of a pathological habit. Cases of hair pulling out on the arms or legs, pubic area, or even in the perianal area are much less common. To remove hair, patients can use their own fingers, nails, or improvised means such as tweezers.
There are certain patterns both in situations in which trichotillomania appears and in the hair pulling procedure itself.
- Patients note a strong desire to pull out hair immediately before the act of pulling out.
- This condition disappears immediately after the hair is pulled out. Tension is replaced by pleasant relaxation and a feeling of pleasure.
- Episodes of trichotillomania usually occur in situations of boredom, loneliness, and routine, repeated actions - watching TV, driving a car, talking on the phone, reading. Also, episodes of trichotillomania can be a reaction to stress or nervous excitement, but often occur in a calm state.
- Hair pulling itself occurs unconsciously. Only in rare cases can this be a conscious action.
- Patients with trichotillomania are characterized by a special ritual of pulling out hair: if possible, they first twirl it around a finger, then pull it out, examine it, and eat the hair follicle. Less often, patients eat the entire hair.
- Patients try to hide areas of baldness that trichotillomania leads to. They wear wigs, false eyelashes, long sleeves, avoid doctor visits, and get eyebrow tattoos. With severe baldness, reclusiveness and avoidance of social contacts are possible.
There is a YouTube channel by Rebecca Brown from the UK, who suffered from trichotillomania. The doctors could not help her and in despair the girl began to record a video in which she talked about her illness and demonstrated areas of baldness. Her videos received several million views, and thanks to the support of the online community, the girl was able to cope with her illness.
Whatever the reason, don't ignore it
If you suspect stress is wreaking havoc on your hair, make an appointment with your doctor to rule out underlying causes (such as hormonal changes and anemia). And focus on methods of stress relief - a miracle will not happen overnight, but someday you need to take the first step. And the sooner the better.
Source: https://zdorovie.com/beauty/how-stress-ruins-your-hair/32616
Trichotillomania is a psychological disorder that directly affects hair health. With trichotillomania, there is an irresistible desire to pull out your own hair, which subsequently leads to baldness and damage to the scalp.
Pulling hair in this manner helps trichotillomania patients relieve tension and anxiety. However, such a habit can also appear during periods of inactivity and calm.
Such hair pulling leads to severe thinning of the hair on a certain area of the head. However, complete baldness is not usually observed. This disease should be distinguished from alopecia areata, in which we are dealing with a completely bald and smooth area of the scalp. Also, when diagnosing the disease, other ailments in which baldness is observed (syphilis and fungal infections) must be excluded.
A type of trichotillomania is the disease trichothemamania, in which the patient selectively pulls out only gray hair, claiming that pulling out helps relieve itching of the head.
So, as noted earlier, the main causes of the disease are various psychological disorders: neurotic conditions, schizophrenia, stress, severe anxiety, psychological trauma in childhood. According to patients, hair pulling provides some psychological relief and also helps hide unwanted emotions. However, many try to hide their habit from others, denying it completely, or indeed simply do not notice that they are actually pulling out hair unknowingly.
Recent studies also suggest that one of the causes of this disease is damage to a certain gene - SLITKR1. However, the genetic nature of the disease has not yet been fully confirmed.
Sometimes, in particularly difficult cases, additional medical treatment may be required, during which the patient is prescribed antidepressants or antipsychotics (however, in this case we are most likely dealing with a serious psychological disorder, in which trichotillomania is only one of its external manifestations).
https://www.healthyhair.ru/trihotillomania.html
Source: https://kst27.ru/index.php/dopinfo/560-2014-03-24-03-15-59
See also:
- Genotyping of human papillomaviruses HPV genotyping: what is it? Published: August 17, 2020, 1:43 pm The need to carry out HPV typing is due to the importance of determining the nature of the disease and making a prognosis for its course. HPV genotyping is an integral part of the diagnosis of the disease and is carried out […]
- How to remove a wart with prayer The magical subtleties of rituals to remove warts Modern people resort to the services of doctors to treat diseases, take medicine and go under a scalpel. In ancient times, when medicine as such did not exist, people rushed to healers for help. One of the purposes of visiting [...]
- Products with carbuncle Carbuncle - treatment, photos, causes What is it - a carbuncle is a purulent inflammation of the hair follicles, sebaceous glands, as well as the skin and subcutaneous tissue around them to a great depth. It has clear boundaries, a favorite localization, and has no tendency to be isolated [...]
- Breakfasts for psoriasis Proper nutrition and diet for psoriasis This is important to know! Exclusive interview with the main allergist-immunologist of Russia. how to properly treat eczema, psoriasis, dermatitis, itchy nose, runny nose and other types of allergies. Read more on this website. Psoriasis is a chronic disease [...]
- Gastritis atopic dermatitis Definition Food can provoke this disease. In most cases, allergies are caused by lemon, tangerine and other citrus fruits, brightly colored berries, fruits and vegetables. In some cases, the appearance of gastrointestinal allergies occurs after consuming [...]
- Conversations on the topic of pediculosis Abstracts on medicine State budgetary educational institution of secondary vocational education Tolyatti Medical College Contents Introduction 2.2 Treatment of pediculosis 2.3 Prevention of pediculosis Conclusion List of references Appendices Lice are small blood-sucking […]
- The wart turned black after super-cleaning. How to use super-cleaning correctly so as not to burn the skin and get rid of warts without a trace? Hello, guests of our site. Unfortunately, in our time there is hardly a person who has not encountered or heard about warts. This skin disease spares no one, it [...]
- Alopecia treatment of psoriasis Treatment of psoriasis with Coriodermina in Cuba at the Center for Placental Histotherapy Sample program of stay: !Important. It is recommended that you stop other treatments for psoriasis at least 45 days before your planned visit to your doctor. 1 day – arrival in Havana, hotel accommodation, free […]
Trichotillomania in children
The causes and prognosis of trichotillomania differ significantly in children under 3 years of age and in schoolchildren and adolescents. In young children, hair pulling is in the vast majority of cases an automatic action, preserved as a habit from the time when they played with their mother's hair during breastfeeding. Often they only play with their hair, twirling it around their fingers, and pulling it out happens accidentally.
In schoolchildren and adolescents, trichotillomania is a full-fledged mental disorder. Schoolchildren realize the inappropriateness of such behavior and try to get rid of it through a conscious volitional effort. In most cases, this does not bring any results or even worsens the habit. Therefore, by adolescence, trichotillomania becomes established as a stable pathological behavior and acquires features of obsession. It can also be a manifestation of auto-aggression due to low self-esteem and self-rejection.
In children who are completely deprived of maternal attention in early infancy, trichotillomania is a component of a general neurotic reaction. They refuse food, avoid people, and do not play with toys. Subsequently, this condition transforms into full-fledged depression. Rehabilitation of such children is long and requires significant effort.
Causes of trichotillomania
According to a number of signs, trichotillomania can also be classified as obsessive-compulsive disorder. Its causes are similar to those for OCD or tics. All reasons can be divided into several groups:
- Manifestations of mental disorders: inability to cope with anxiety and stress, obsessive-compulsive disorder. In the pathogenesis of the latter, a number of reasons are identified, in particular, unfavorable life circumstances, hereditary predisposition and impaired metabolism of biologically active substances in the neurons of the brain.
- Self-harm option. In this disorder, the patient purposefully injures himself for the sake of temporary relief from emotional problems. The pain of an injury triggers the release of endorphins, which give the patient a short-term feeling of satisfaction.
- Morphological changes in the brain. Some patients with trichotillomania have shown changes in brain structures, but their strict connection with the disease has not yet been proven.
- Genetic predisposition is now being actively studied; there are indications of a connection between the disease and the presence of a certain gene.
- Serotonin deficiency, as indicated by the effectiveness of selective serotonin receptor inhibitors in the treatment of trichotillomania.
- Changes at the hormonal level, which are supported by the high incidence of trichotillomania during hormonal changes in the body, in particular during puberty.
Psychotherapy
There is no special therapy for the treatment of such a disease, since the real origins of trichotillomania are not known. A successful outcome will require the help of a psychotherapist and the patient’s persistence.
Mental influences are aimed at training resistance to stress. Patients usually have low self-esteem. Accepting yourself as you are helps fight the manifestations of trichotillomania.
Types of therapy:
- Games. Treatment takes place in the form of a game, in which the patient is not limited by formalities and easily expresses his inner feelings. The patient is freed from internal tension, the child’s constant hysterics disappear along with the habit of tearing his hair. Play therapy is useful if it helps distract you from anxious thoughts.
- Hypnosis. The treatment is carried out by an experienced specialist. Its task is to introduce into the patient’s mind the idea of severe pain when pulling out hair. This establishes a ban on the bad habit.
- Behavioral therapy is about developing a new habit in the patient when he feels anxious and wants to pull his hair. The child should clench his hand into a fist, raise his forearm, and so on. The effectiveness of therapy is high, as confirmed by numerous reviews.
Differential diagnosis
Trichotillomania must be distinguished from other types of baldness.
With neurotrophic alopecia, areas of hairlessness are located evenly throughout the entire head, the surface of the baldness area looks polished-smooth, or is covered with evenly growing hair. In trichotillomania, the area of baldness is limited to an area convenient for plucking and looks poorly trimmed, as it is covered with hair in various stages of regrowth.
Dermatophytosis (fungal infection of the hair) is accompanied by itching and inflammation of the skin; the hair is not torn out, but broken off at the root.
Lichen planus on the scalp is characterized by complete loss of hair with scarring.
Telogen effluvium occurs after severe illnesses, childbirth, operations and is manifested by uniform hair loss, as a result of which hair density decreases without areas of baldness.
Diagnostics
Only a psychotherapist can make a correct diagnosis and find out the causes of trichotillomania. The basis of diagnostic measures are the following manipulations:
- studying the medical history of both the patient and his immediate relatives - this is necessary to find out what pathological factor influenced the development of such an illness;
- collection and analysis of life history - this should include information regarding the use of medications, nutrition, with which the human body often receives nutrients, as well as previous stress or nervous strain;
- a thorough examination of areas covered with hair - to determine the severity of the disease;
- a detailed interview of the patient, and if this is not possible, of the patient’s relatives - to obtain data from the clinician regarding when the characteristic symptoms first appeared and with what degree of severity they manifest themselves.
If after the measures described above it is not possible to establish the provoking etiological factor, then in addition the following general laboratory and instrumental procedures may be needed:
- general clinical and biochemical blood test;
- hormonal tests;
- genetic tests;
- radiography and ultrasound of the skull;
- CT and MRI.
Complications of trichotillomania
The most common are the social consequences of the disease - the patient avoids social contacts because he is afraid of being discovered. As a result, he may refuse treatment or examination, which leads to serious health consequences.
Skin and eye infections due to constant trauma to hair growth areas can become protracted and severe.
A number of patients eat their hair. First of all, this behavior leads to dental problems: enamel erosion and other damage to the teeth. The eaten hair cannot be removed from the stomach normally and accumulates there. This leads to the formation of trichobezoars in the stomach - “hair stones”, which can reach enormous sizes. Such trichobezoars require surgical treatment. Cases of removing hairballs weighing 1.5 and even 2 kilograms have been described.
Psychological problems also accompany trichotillomania. Among them are depression, anxiety disorders, various types of phobias, obsessive-compulsive disorders, attention deficit hyperactivity disorder, eating disorders (bulimia or anorexia).
Treatment of trichotillomania
Various psychotherapeutic techniques prevail in the treatment of a disorder such as trichotillomania. Treatment at home mainly involves shaving the hair, which gives temporary results. Psychologists and psychotherapists have developed many techniques for effectively treating trichotillomania.
Hypnosis
– an effective method that gives quick results and does not require numerous sessions and hard work on yourself. During a hypnosis session, the psychotherapist instills in the patient new, effective programs of behavior and response to stress. During hypnosis, deep suggestion is carried out, so new habits fall directly to the level of the unconscious and do not require training or habituation.
Cognitive behavioral psychotherapy.
The most effective CPT method for treating trichotillomania is habit retraining. At the same time, on the one hand, a person learns to identify situations in which undesirable behavior occurs. Most often, this is done by keeping a diary, recording the circumstances in which episodes of trichotillomania occur. On the other hand, the patient is taught substitute behavior that is not destructive and socially unacceptable. For example, instead of pulling out hair, he may massage the scalp or ear. Then there is a gradual replacement of one pattern of behavior by another. This method of treatment requires great consciousness on the part of the patient, a great desire to be cured and significant self-control.
Another effective method is to increase awareness of your actions. The patient learns a constructive attitude towards stress and discomfort. The patient gets the idea that the cause of the disease and other problems is not the stressful situation itself, but the attitude towards it. The situation is abstract and neutral, so the goal of treatment is to change attitudes. The patient learns a constructive attitude towards various uncomfortable situations, learns to live through them without the need to pull out hair.
Additionally, cognitive behavioral therapy may use techniques such as stimulus control and restructuring. The first uses special devices to eliminate the possibility of hair being pulled out. The second teaches the patient new patterns of thinking when the desire to pull out hair arises.
Individual psychotherapy
– use of the methods described above, psychoanalysis and Gestalt therapy, as well as their combinations to achieve maximum results for a particular patient.
Group psychotherapy
involves the active participation of patients themselves in treatment, which is corrected and directed by the psychotherapist. Not everywhere there are groups of patients with trichotillomania. Treatment is also possible in groups for patients with obsessive-compulsive disorder.
Pharmacotherapy.
If psychotherapy is insufficiently effective, selective serotonin reuptake inhibitors can be used to speed up its results or with a high intensity of hair pulling.
Treatment
With a disease such as trichotillomania, treatment begins with an accurate diagnosis, since sometimes somatic diseases are mistaken for psychopathology - lichen, baldness due to toxic substances, or severe disorders such as schizophrenia.
For treatment, drug therapy is used - antidepressants, sedatives, vitamin complexes and psychotherapy. Taking medications alone without psychotherapy is usually ineffective. Since it is important to understand the causes of the development of obsessive-compulsive disorder and act directly on them.
Treatment of trichotillomania at home begins with creating a comfortable psychological environment, improving the general physical condition of the patient, and eliminating factors that cause symptoms of the disease. It is also recommended to play sports, give up bad habits and overwork, special relaxation exercises and monitor the patient’s behavior. So, instead of pulling out hair, you can use an anti-stress toy, perform some physical exercises, or massage your fingers.
Trichotillomania is considered a fairly rare pathology, which is diagnosed in only 2% of the world's population. It is noteworthy that absolutely anyone can suffer from the disease, regardless of age and gender.
In the vast majority of situations, the illness is a consequence of psychological trauma. In addition, doctors identify several more predisposing factors that contribute to the development of the disease.
The main clinical sign is the very fact of hair pulling, which occurs against the background of a strong desire to do this. After such a process, there is calmness and a feeling of satisfaction. Nevertheless, the very fact of hair pulling remains unconscious.
Diagnosis is carried out by a psychotherapist, and the basis is taken from information obtained during a thorough physical examination of the head and other hairy parts of the body, as well as a detailed interview with the patient.
The disease can be cured both at home and through long-term work by a specialist with a sick person. In addition, eliminating the provoking factor plays an important role in therapy.