Aspergillosis is a group of infectious diseases caused by mold fungi of the genus Aspergillus.
These diseases usually affect the human respiratory system.
The mold that causes aspergillosis is very common both outdoors and indoors. Most strains are harmless to humans, but some can cause serious infection, especially if their spores are inhaled by someone with a weakened immune system, lung disease, or asthma.
Aspergillus spores cause allergic reactions in some people. Others have severe lung infections. The most dangerous form of aspergillosis occurs when the infection enters the bloodstream and spreads throughout the body - a systemic fungal infection. Depending on the type of aspergillosis, treatment may be limited to observation or include medications and even surgical methods (in rare cases).
General information about the disease
Despite the fact that aspergillosis is a rare pathology among diseases of the lung tissue, it is diagnosed in 75% of cases. There are several forms and stages of the disease.
Often the pathology develops asymptomatically or is disguised as concomitant diseases, asthma or cystic fibrosis. Only through examination can problems in the lungs be identified.
If diagnosis has not been carried out previously, a person learns about the disease already in advanced situations. However, sometimes fungal infection occurs rapidly and causes severe symptoms.
Pathogenesis
Once in the lungs, the fungi begin to quickly colonize. They are able to reproduce at temperatures close to the temperature of the human body, and foci of inflammation appear quickly. Sometimes they accumulate in existing cavities of the lung tissue and can grow into blood vessels.
The fungus itself is not dangerous for a healthy body: immune cells block microorganisms and destroy them. However, the toxin that is released from mushrooms does not disappear anywhere. And it harms a weakened body.
Forms and types of aspergillosis
Asperigillosis in the lungs is divided into primary (invasive) and secondary (non-invasive). In the first case, microorganisms that enter the lungs of a healthy person begin to parasitize, creating infiltrates in undisturbed lung tissue. This form of the disease develops aggressively.
In the second case, aspergillus develops against the background of an existing disease, when the lung tissue is damaged, due to tuberculosis, lung abscess or chronic lung disease. A so-called aspergilloma may form - a ball-shaped accumulation of microorganisms in cavities. This accumulation can move through the lung tissue, causing new foci of inflammation.
An allergic type of disease is distinguished. Sensitivity to fungi appears in asthma or a similar disease. In this case, the symptoms of the original pathology worsen.
This disease is divided into forms:
- Chronic.
- I'll sharpen it up.
- Spicy.
Symptoms are increasing in severity.
Main symptoms
Symptoms of aspergillosis are determined by its location. The respiratory system is most often affected: the lungs and bronchi. Mushrooms of this species live both in the soil and in the air, as well as in water.
Their greatest distribution in the air determines the highest frequency of damage to the respiratory tract. From the lungs, fungi can spread with the flow of lymph throughout all organs and tissues, causing massive damage to all organs and systems, provoking generalized forms up to sepsis.
When the process is generalized, the fatality rate is up to 80 percent.
Symptoms
Symptoms vary depending on the form and type of disease. With non-invasive aspergillosis, the patient complains of the following symptoms:
- hemoptysis;
- thick discharge;
- frequent coughing attacks;
- temperature increase;
- general malaise.
With the invasive type of pathology, the following main symptoms are distinguished:
- shortness of breath with minimal exertion;
- fever;
- wheezing when listening;
- chest pain;
- severe coughing attacks;
- dizziness;
- decreased appetite and body weight;
- blood in sputum.
Often the patient's skin takes on a blue tint.
Clinical picture of aspergillosis in humans
From the moment the microbe enters until the first clinical signs appear, it can take from 3 hours to 3 days .
If the fungus enters the respiratory tract, the disease begins acutely. There is a feeling of soreness in the throat, the heartbeat quickens, and an asthmatic component in the form of expiratory shortness of breath (difficulty exhaling) is added. The intoxication syndrome is pronounced: severe headache, febrile body temperature up to 39 degrees, pain in joints and muscles.
On auscultation, dry rales are heard in the lungs. On the second day of the disease, the cough becomes wet, gray sputum is released, with a small amount of blood streaks, fine rales are heard in the lungs, and bronchospasm is present. In general, this form of the disease is very similar to tracheitis and tracheobronchitis; in some cases, lung tissue is affected and pneumonia occurs.
There are chronic forms of aspergillosis, they are layered on existing lung diseases, most often bronchiectasis, tuberculosis, chronic obstructive pulmonary disease. In these cases, there is a constant low-grade fever, night sweats, and weight loss. As the disease progresses, destruction of lung tissue and severe septic shock may develop. This form is especially dangerous for HIV-infected patients.
Aspergillosis of the skin is characterized by the presence of an ulcerative defect on the skin , most often on the palms. The defect is painful, with discharge of purulent contents. Body temperature may rise to 38 degrees.
Risk group
Before identifying groups of people who are at risk, it is important to recall that pulmonary aspergillosis is a pathology caused by fungi. Microorganisms enter the lungs when their spores are inhaled by humans.
Therefore, everyone who comes into contact with the ground and grain crops is at risk. But with a normal level of immunity, the body copes with fungi without harm to health. Microorganisms have a detrimental effect on those who have immunodeficiency. It may be due to:
- Long course of radiation and chemotherapy.
- Numerous surgical interventions in the respiratory system.
- Taking corticosteroids.
HIV in the AIDS stage causes pulmonary aspergillosis in 90% of cases. The risk group includes patients suffering from chronic diseases of the respiratory system (asthma, chronic pulmonary failure).
Pulmonary aspergillosis: what is it?
Aspergillosis is an infection or allergic reaction caused by various types of mold (a type of fungus). Mold is often found outdoors on plants, soil, or rotting plant matter. Mold can also grow indoors on household dust, food products such as ground spices and building materials. Aspergillus fumigatus is a type of fungus that most commonly causes aspergillosis in some people when they inhale its spores.
Exposure to Aspergillus is unlikely to cause problems for most people whose immune systems are healthy. However, people with chronic lung problems or people with weak immune systems (immunosuppression) may be at greater risk of developing an infection. People with weakened immune systems include those undergoing chemotherapy or having an organ transplant.
How common is aspergillosis?
Aspergillus is extremely common in the environment and is found everywhere. Aspergilli have been isolated from ventilation and air conditioning systems; they are found in baths, showers and bathrooms, in household and personal hygiene items. If the fungus “lives” in the house, then it can be easily activated by, for example, renovating an apartment or moving old furniture. Aspergillus lives in grass, fallen leaves, and pots of indoor plants, and food rots under its influence.
Up to 10% of people with cystic fibrosis or asthma experience an allergic reaction to Aspergillus fungi. Allergic bronchopulmonary aspergillosis is estimated to occur in approximately 2% of all asthmatics and 2-15% of patients with cystic fibrosis.
Possible complications
Without treatment, the patient's situation worsens. Chronic necrotizing pneumonia may develop. The process is slow, but irreversible. Against the background of parasitic microorganisms, destruction and then death of lung tissue begins.
Without proper therapy, patients experience pulmonary insufficiency, cerebral circulatory disorders, and cardiovascular failure. Pulmonary hemorrhage may develop.
In 50% of cases, if the body does not respond to the proposed treatment, pulmonary aspergillosis leads to death. In the remaining 50% of cases, remission can be achieved, but relapses are frequent.
Prognosis and prevention
The most favorable course is observed with aspergillosis of the skin and mucous membranes. The mortality rate from pulmonary forms of mycosis is 20-35%, and in people with immunodeficiency - up to 50%. The septic form of aspergillosis has a poor prognosis.
Measures to prevent infection with aspergillosis include measures to improve sanitary and hygienic conditions: combating dust in production, wearing personal protective equipment (respirators) by workers in mills, granaries, vegetable stores, weaving enterprises, improving ventilation of workshops and warehouses, regular mycological examination of persons from risk groups.
Diagnosis of pathology
When visiting a doctor, it is important to tell them the symptoms so that he or she has a detailed picture of the illness. Diagnosis begins with a complete examination and interview of the patient. Because the symptoms are similar to bacterial pneumonia or bronchitis, it is important to rule out these diseases.
Differential diagnosis is carried out with other fungal diseases of the lungs, as well as with the following ailments:
- alveolitis;
- bronchial asthma;
- lung abscess;
- malignant neoplasms;
- tuberculosis.
For this purpose, laboratory and instrumental examinations are carried out.
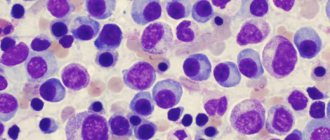
A general and biochemical blood test is taken. It is important to identify and confirm a strong inflammatory process. Then they take sputum for analysis (cytology, microscopy and biopsy). At this stage, the content of microorganisms in the lungs is determined.
Then they move on to instrumental diagnostics:
- Radiography.
- CT scan.
- Bronchoscopy.
The photographs show infiltrates, disruption of tissue structure and deformation of the bronchial tree.
When making a diagnosis, not only pulmonologists, but also TB specialists, oncologists, immunologists and other doctors are involved. It is important not only to establish a diagnosis, but to clarify the degree of influence of the disease on the body. Complications cannot be allowed to happen.
Treatment
The therapy program is developed collectively. They call a council of doctors, where they offer effective treatment options for pulmonary aspergillosis.
Depending on the degree and form of the disease, conservative therapy or surgical intervention is chosen.
If the disease is detected on time, it is possible to get rid of it with 1-2 courses of taking antifungal medications orally. In more severe cases, intravenous and intramuscular administration of antifungal agents is prescribed, as well as:
- Corticosteroids.
- Antibiotics.
- Angioprotectors.
This reduces painful symptoms and restores metabolism.
The patient is also shown:
- Physiotherapy. Usually, immediately after the main symptoms are removed, they move on to strengthening the body. Electrophoresis, magnetic therapy, and massages are used. Sometimes applications with herbal ingredients that make breathing easier have a good effect on the body.
- Physiotherapy. They switch to it at the final stage of treatment in order to normalize metabolic processes and restore respiratory function.
- Diet. The body was able to resist pathology itself; it is important to strengthen the immune system. Therefore, patients are advised to eat only healthy foods, without overusing smoked, salted and starchy foods.
In situations where the pathology is advanced, radical measures are taken. The affected areas of the lung tissue are removed, the cavities are cleaned of microorganisms and they are sutured to eliminate the possibility of relapse.
In some cases, an embolism is performed on one of the bronchial branches to prevent the development of aspergillosis in other parts of the respiratory system.
Then they prescribe antifungal drugs, antibiotics and glucocorticosteroids.
How many days does it take to treat aspergillosis?
Antifungal therapy is continued until the clinical signs of the disease disappear, the pathogen is eradicated from the source of infection, radiological signs stop or stabilize, and the period of neutropenia ends. The average duration of treatment until the patient's condition is stabilized is 20 days, and complete remission is achieved - 60 days. Typically, antifungal therapy is continued for at least three months. However, in patients with persistent immunosuppression, longer treatment is required.
Elimination or reduction of the severity of risk factors is achieved by successful treatment of the underlying disease, correction of neutropenia, as well as the abolition or reduction of the dose of steroids or immunosuppressants, etc. The effectiveness of various “immunomodulators” in randomized clinical trials (RCTs) has not been established.