A foreign body in the lungs will cause pathological conditions caused by impaired respiratory function. Foreign objects enter the bronchial tree as a result of aspiration, and into the pulmonary parenchyma and pleura from wounds or as a result of medical interventions.
Symptoms depend on the size of the object, its properties and location. Diagnosis includes radiography, ultrasound, bronchoscopy, MRI or CT. Treatment involves removing the object, treating the wound, antibacterial and anti-inflammatory therapy.
Causes of venous stagnation
The lungs are a paired organ that is the main organ in the respiratory system. During breathing, they alternately increase and decrease, depending on the respiratory phase.
There may be several reasons for blood stagnation in them:
- Sedentary lifestyle of a person. This can lead to problems not only with the lungs, but also with other organs.
- Heart failure and heart disease. Because of this, blood is poorly pumped by the heart. Therefore, the blood leaving the left ventricles and atria penetrates into the lungs, where it can stagnate.
- Increased pressure in blood vessels. Because of it, an excessive amount of blood enters the alveoli. The breathing process is disrupted, gas exchange decreases. The person may experience shortness of breath.
Hypertension can be chronic due to vascular pathology, or it can occur due to taking certain medications and products.
- Chest injuries. They can lead to hemorrhage in the lungs and blood retention in them.
- Staying at high altitude. For example, frequent flights, skydiving. At altitude, the pressure is higher, so the organs begin to work in an unusual mode. This can cause various problems, including stagnation of blood in the lungs.
As a rule, for successful treatment it is necessary to eliminate the causes of the disease. Therefore, before selecting the optimal therapeutic regimen, the doctor studies possible factors in the development of the pathological process.
Complications
This disease requires timely and correct therapy to avoid possible negative health consequences.
In the absence of rational treatment, a person experiences the following complications:
- Emphysema gradually progresses , and therefore the severity of symptoms worsens.
- Loss of ability to work due to impaired breathing.
- Early disability, which is determined due to the development of cardiac and respiratory failure.
Attention! The pathology is dangerous due to irreversible processes in which organ tissue is deformed and breathing is impaired. Despite this, pulmonary syndrome can be alleviated by improving quality of life. For this purpose, doctors prescribe inhaled medications for continuous use.
In many cases, surgical treatment (lung removal and transplantation) is performed, which helps stabilize the chronic syndrome and prevent the frequent occurrence of suddenly recurring pneumothorax.
Signs of the disease
With weak immunity, the disease can make itself felt within 2-3 days. If the immune system is strong, then signs of pathology may not appear within a week. If a person has stagnant blood in the lungs, he may experience the following symptoms:
- The person begins to breathe quickly and complains of dull pain in the lungs.
- He speaks very slowly, sometimes stopping to catch his breath.
- Cold sweat appears during sleep and while awake.
- There may be a slight cough, and blood-streaked sputum is produced.
Sometimes bloody foam appears. In this case, the cough is very pronounced, the patient cannot clear his throat, something is blocking him in the lungs.
- Excessive weakness appears, the person quickly gets tired, even if he does not perform difficult activities.
- When lying down, shortness of breath begins. For it to pass, a person must take a sitting position. The pillow should also be high - a low one is uncomfortable for him, and shortness of breath also begins.
- The skin turns pale, a certain cyanosis appears above the lip, swelling appears on the legs, which makes it difficult for the patient to move.
- Pleurisy (inflammation of the pleural layers) may develop due to hypoxia. Accompanied by chest pain, dry cough, shallow breathing. During auscultation, the doctor may hear a pleural friction rub.
If any of the above symptoms occur, you should immediately consult a doctor.
. Otherwise, serious complications may develop, including the risk of death.
Lung diseases caused by smoking
Today, there are several types of diseases that can develop in the lungs when smoking. In this article we will look at the most common diseases:
Chronic obstructive disease
It should immediately be noted that such a disease develops in almost 90% of cases due to smoking. The disease can lead to difficulty breathing. In fact, such a disease is incurable. When this disease begins to develop, the body deteriorates in several ways. First of all, the inflammatory process occurs in the lungs of the smoker. That is, the gaps begin to gradually narrow, and the volume of mucus gradually increases. Smoking can also cause bronchitis. A smoker develops a cough that sounds very harsh and dry. If a person has chronic bronchitis, then it is not treated.
What happens to the lungs when smoking? If there are any symptoms, a person can only reduce them somewhat, but not get rid of them completely. Smoking can lead to emphysema in the lungs. Damage occurs to the alveoli, which can increase in size and also collapse. If a smoker has obstructive pulmonary disease, his gas exchange may be impaired. Symptoms of the disease include phlegm, heavy breathing, cough, colds and fatigue. Let us remind you that this disease cannot be completely cured. Treatment is aimed only at reducing possible exacerbation, as well as reducing symptoms;
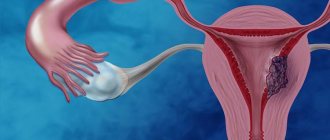
Lungs' cancer
The most common risk from smoking to the lungs is cancer. This disease is known to have a high mortality rate. Currently, the main cause of cancer is smoking. The highest likelihood of developing cancer is observed in smokers who smoke for a very long period of time and who do not quit smoking after diagnosis. If a person is able to quit smoking, then his risk of cancer decreases. Of course, there is a risk of lung cancer in a person who smoked but quit, but it is not as great as for someone who did not quit smoking.
Note that passive smoking can also cause the development of lung cancer. Symptoms of cancer development include: shortness of breath, cough, phlegm, shortness of breath, and chest pain. In the early stages of the disease, the patient may not experience any symptoms at all.
Diagnosis of the disease
Diagnosis of venous congestion in the lungs consists of a visual examination of the patient, listening to the lungs to detect noise, as well as palpation. During this, the doctor may detect abnormal heart and lung sounds, tachycardia, and rapid breathing. It is also possible to change the color of the skin - it may turn blue or pale.
Additionally, to confirm the diagnosis, the doctor may prescribe other diagnostic procedures. It is necessary to take a general and biochemical blood test, as well as an analysis of the oxygen content in it. Typically, with venous stagnation, its level increases significantly. The doctor may also recommend an X-ray of the cell, an ECG and an ultrasound of the heart.
How to treat venous congestion in the lungs
Treatment of congestion in the lungs is conservative. Doctors recommend following a certain motor regimen by performing special gymnastics. It is also necessary to give up bad habits - smoking has a negative effect on diseased lungs. And giving up alcohol and proper nutrition improves the condition of blood vessels, so blood from the lungs begins to dissolve.
To improve the rheological properties of blood, it is necessary to include fresh vegetables, fruits and herbs in the diet.
Drug therapy
Venous congestion in the lungs is a dangerous condition, and it must be treated in a hospital setting. The cause of the disease must be determined. If this happened due to a heart attack, it must be stopped.
The disease is treated with the use of venotonics. These drugs have a positive effect on the body:
- They increase the elasticity of blood vessels, thereby improving blood circulation through them.
- Relieves inflammatory processes and prevents their occurrence.
- Strengthen the immune system and improve the patient's condition.
Venotonics include the following drugs: Aescusan cream, Venen gel, Dr. Theiss with horse chestnut, Antistax gel and others. They are applied to the chest area.
It is also necessary to use anticoagulants. The universal remedy of this group is Heparin. It has a positive effect on thrombosis and reduces the severity of venous stagnation.
Diuretics are prescribed to remove excess fluid from the body. Medicines that strengthen the heart muscle are also needed.
If the patient cannot breathe on his own, oxygen is supplied to his lungs. For this, an oxygen mask or special plastic tubes are used that are brought to the nose. If the patient is connected to a ventilator, a tube is inserted into the trachea through which breathing is carried out.
The use of folk remedies
Venous congestion cannot be treated with folk remedies. They can only be used to strengthen the immune system, but only after returning home from a hospital setting. The following traditional medicine drugs can speed up the rehabilitation period:
- Peel the head of garlic and finely chop or grate it. Add honey so that there is as much as garlic. Stir well and leave for several hours. Take 1 tbsp. l. three times a day.
- Grate horseradish. Fill the glass ¾ full. Then fill it with vodka to the very top. Leave for a day, then strain the product and pour it into an enamel vessel. Add 200 g of beetroot and carrot juice, as well as 2 lemons, crushed together with the pulp. Boil for 10-15 minutes, and then pour liter jars into the floor. The drug increases hemoglobin and clears the lungs of accumulated blood and phlegm.
- Grind 50 g of red brush, pour in 500 ml of vodka. Leave for a month in a dark place. Take 1 tsp diluted with half a glass of water before each meal. The duration of one course is 3 months, then a break for 14 days. Repeat the courses three times.
But it will not be possible to cure venous stagnation only with the use of folk remedies. Self-medication can be dangerous to health.
The sooner you start treatment, the less likely there is to be a complication.
. Therefore, therapy should be started after the first symptoms of the pathological process appear.
Due to deterioration of vascular tone and thick blood against the background of a sedentary lifestyle, venous stagnation develops. The pathology is characterized by a violation of the outflow of blood from the extremities to the heart. High vein filling leads to the formation of edema and provokes additional stress on the lymphatic system. Slow circulation in the affected part of the body prevents the flow of oxygen and nutrients through the arterial blood. This condition leads to the formation of blood clots and other dangerous complications.
Clinical picture
Pulmonary tuberculosis with decay has a short course (from 2 weeks to 4 months). The clinical manifestations of the disease depend on what stage of development the pathological process is at.
Infiltration phase
During the period of infiltration of lung tissue, destructive changes do not yet develop in the organ. An inflammation process occurs, which is accompanied by exudation - the release of plasma and specific proteins from the bloodstream. Tuberculosis at this stage is manifested by the following symptoms:
- General weakness;
- Decreased performance, severe patient fatigue;
- Appetite disorders;
- The appearance of pain spreading throughout the chest;
- Dry cough without sputum production;
- Pyoderma is the appearance of pustules on the surface of the skin.
When listening (auscultating) the patient over the pulmonary fields in the area of the pathological focus, characteristic symptoms are detected - moist rales and pleural friction noise.
Decay phase
After completion of the infiltration stage, the decay stage begins. In this case, caseous necrosis develops in the lung tissue - the epithelium of the alveoli disintegrates. The rejected lung tissue is released through the bronchi, and the patient coughs it up along with sputum.
In tuberculosis, the collapse of the lungs leads to the formation of pneumopyogenic (pus-producing) cavities. Sometimes caseous masses come out not through the bronchi, but through formed fistulas - pathological purulent ducts.
At this stage, the patient’s symptoms worsen. The decay phase is characterized by:
- Severe cough with characteristic purulent sputum;
- Hemoptysis;
- The appearance of expiratory shortness of breath (difficulty in exhaling);
- Chest pain, feeling of pressure, fullness;
- Increased sweating;
- Sharp increases and decreases in body temperature;
- Insomnia;
- Cyanosis around the mouth;
- Decreased elasticity of the skin.
On auscultation, moist rales are detected. Sometimes they can be heard just like that, without a phonendoscope.
Seed phase
The last stage of lung decay in tuberculosis is contamination. At this stage, the pathological process spreads to surrounding organs from the primary tuberculosis focus. The spread of the disease occurs through sputum, which contains a large amount of the causative microorganism - Koch's bacillus.
The pathology first spreads to nearby organs, then can move further throughout the body. Pathological foci of irregular shape form in damaged tissues. At this stage, the symptoms of pulmonary tuberculosis are also accompanied by signs of damage to other organs into which the pathogenic microorganism has penetrated.
What is the reason?
Low physical activity provokes the development of diseases of the cardiovascular system. Due to physical inactivity, venous blood stagnates, primarily in the legs.
The deterioration of blood flow leads to:
- congenital or acquired disorder of the myocardium;
- thrombosis;
- improper functioning of the right heart ventricle;
- low elasticity of the lungs;
- prolonged stay of the patient in a supine position.
Risk group
The development of this condition is facilitated by pregnancy.
A genetic predisposition to varicose veins and venous congestion manifests itself if factors such as:
- the need to stand or sit for a long time;
- intense physical activity;
- frequent constipation;
- pregnancy.
Causes of emphysema
Smoking Causes Emphysema
The most common known cause or risk factor for emphysema and COPD is smoking. Approximately 90% of cases of emphysema and COPD are associated with cigarette smoking. However, COPD develops only in genetically predisposed smokers and does not always lead to this disease.
Other inhaled toxins also contribute to the development of emphysema and COPD, including those associated with occupational activities. In developing countries, smoke from cooking (indoors) and heating is also a significant cause of emphysema.
Although smoking is the most significant cause of emphysema, the following risk factors should not be discounted:
- low body weight
- childhood respiratory diseases
- passive smoking
- air pollution
- inhalation of industrial dust, for example, mineral dust, cotton dust, etc.
- inhalation of chemicals, such as coal, grain, isocyanates, cadmium, etc.
Your genes may also cause you to develop a rare form of COPD - emphysema, which can be caused by a deficiency of alpha-1 antitrypsin. The protein is necessary to protect the lungs from the destruction of neutrophil elastase in alveolar tissue. Alpha-1 antitrypsin deficiency is a congenital condition—that is, people are born with it.
The genetic disease affects nonsmokers, which explains some of the cases of COPD not related to smoking at an early age. Smoking, however, accelerates the development of the disease in genetically predisposed people.
Main symptoms
Manifestations of venous stagnation depend on the location of the pathological process:
Due to cervical osteochondrosis, the blood vessels of the brain may suffer.
- Brain. Osteochondrosis of the neck can impair blood circulation. In this case, bursting headaches occur. The pain intensifies when the patient turns his head or moves his eyes. There is noise in the ears, the lower eyelids swell, fainting and mental disorders are possible.
- Lungs. The patient's breathing becomes harsh and shortness of breath appears. Interpleural pressure increases. Blood is visible in the sputum.
- Legs and pelvis. Swelling of the extremities occurs, a venous pattern appears, and the skin turns blue. There is increasing pain in the legs, hips, and groin area. Possible swelling of the perineum and lower abdomen. On palpation the pain intensifies.
What is the danger of the disease?
Venous stasis provokes dangerous complications that threaten the health and life of the patient. There are several pathologies that arise against the background of venous stasis, which are divided depending on the affected area. If the disorder affects the lungs, the following is observed:
- compaction of lung tissue;
- development of sclerosis;
- stagnation of the pulmonary circulation.
In women, this condition can lead to infertility.
Stagnant processes are most dangerous for women, since the pathology provokes:
- infertility;
- miscarriages;
- premature birth.
When the legs are affected, the patient experiences pain and a feeling of heaviness. Venous insufficiency develops. The limbs swell, and blood clots may form, threatening thromboembolism. The most dangerous is stagnation of blood in the brain. Violation causes disability and death. Pathology provokes:
- cerebral edema;
- oxygen starvation;
- disruption of metabolic processes and neuron nutrition;
- ischemic processes.
Paraseptal
With this pathology, the pulmonary alveoli expand so much that the interalveolar septa are destroyed. Paraseptal emphysema leads to disruption of the functioning of the lung tissue, but the risk of death is extremely low. The body receives less oxygen than in a healthy state, but the shortage is not so critical as to lead to death.
- Korean cucumbers for the winter
- 5 delicious recipes for salting fish at home
- Heartburn - causes and treatment of the disease
Diagnostics
A timely examination is considered the best prevention of complications. The stagnant process, identified at the initial stage of development, can be eliminated with the help of therapeutic methods. To make a diagnosis:
Anamnesis is also important to make a diagnosis.
- general examination and medical history;
- blood pressure measurement;
- radiography;
- phlebography.
Ultrasound is used to determine the condition of the deep veins. MRI and CT scans make it possible to determine the area with the affected areas of the veins, the area where blood stagnation begins.
Treatment of venous stagnation
Drug therapy
Regardless of the characteristics of the pathology and the area of its localization, venous stasis requires an increase in vascular tone. For this purpose, venotonics are used, allowing:
- normalize the condition of vascular walls;
- increase the elasticity of veins;
- reduce swelling;
- eliminate vascular fragility;
- prevent the development of inflammation;
- increase the tone of the body as a whole.
If a person suffers from fluid retention, then he is prescribed diuretics.
If necessary, the patient is prescribed:
- Anticoagulants. Used to reduce blood clotting.
- Preparations with caffeine. Improves muscle tone.
- Diuretics. They remove excess fluid from the body and prevent the formation of edema.
Depending on the degree of damage and the area of localization, the doctor prescribes drugs that normalize the trophism of certain tissues and organs. The duration of treatment and dosage of medications cannot be changed independently. Unauthorized cancellation of therapy is dangerous. Congestion in the veins can be a manifestation of a serious illness, so at the first symptoms you should seek medical help.
If a person has insufficient ventilation in the lung tissues, this may be due to stagnation of blood in the pulmonary tract. This disease is extremely dangerous for health and life in general and is called “pulmonary congestion.”
The disease most often develops as a result of a person’s inactivity, the consequences of which can be chronic diseases of the cardiovascular and respiratory systems.
Pulmonary emphysema: classification
The ICD-10 code for emphysema is J43.9. This subgroup includes:
- McLeod syndrome (J43.0);
- panlobular (J 43.1);
- centrilobular (J 43.2) and
- another (J 43.8).
In addition, other categories of ICD-10 include the following types of pathology:
- compensatory (J98.3);
- caused by exposure to inhaled harmful substances (J68.4);
- interstitial (J98.2);
- newborn (P25.0);
- emphysematous obstructive bronchitis (J44).
In clinical practice, a classification is used based on taking into account the causes, anatomical changes and the X-ray picture of the pathology.
Depending on the causes, it can be congenital (primary) or acquired (secondary). According to the radiological type, homogeneous (total, diffuse, complete) and heterogeneous (partial, segmental) lesions are distinguished.
Types of emphysematous lesions
Depending on the structural changes, the following types of pulmonary emphysema are distinguished:
- panacinar (panlobular): the entire acinus is affected;
- centriacinar (centrilobular): only its central part is affected, that is, the branches of the terminal bronchiole (respiratory bronchioles);
- periacinar (perilobular): predominantly the alveolar ducts are damaged.
Centrilobular emphysema affects the upper lobes. A similar process develops with pneumoconiosis in miners, but in this case, areas of swelling alternate with areas of shrinkage (fibrosis) of the lungs.
Panacinar emphysema affects the alveoli, destroying the partitions between them. It is observed in the lower sections and has a more severe course.
Also, doctors sometimes talk about irregular emphysema. This condition is accompanied by varying degrees of enlargement and destruction of the alveoli in combination with cicatricial changes in the lung tissue. The cause of this condition is sarcoidosis, tuberculosis, pneumoconiosis, histoplasmosis, eosinophilic granuloma.
X-ray examination reveals the following types of pathology:
- diffuse, with the presence of multiple small cavities in the lungs;
- bullous, with the formation of hollow foci (bulls) with a diameter of more than 1 cm;
- combined, with the appearance of “bubbles” against the background of diffusely increased airiness of the tissue – bull.
Physiological forms that do not cause gas exchange disturbances include:
- senile, accompanied by expansion of the alveoli without damage to the bronchioles;
- vicarious (replacement) emphysema, which occurs after removal of part of the lung to normalize gas exchange.
Causes and symptoms
It is known that the lungs are a paired organ that is located in almost the entire chest cavity. They represent the main device of the respiratory system. Depending on the phase of breathing, the size and shape of the lungs change.
In addition to the above-mentioned inactivity, one of the causes of stagnation is also heart failure - blood is not pumped by the heart, resulting in stagnation of blood in the venous system of the lungs, which extends from the left side of the heart.
If the pressure invariably increases in the area of the blood vessels, then a large amount of blood penetrates into the alveoli. This causes a decrease in gas exchange, which subsequently results in shortness of breath, and in the worst case, the person begins to suffocate.
So, in addition to a decrease in physical activity, there are several reasons for stagnation:
- Heart diseases that weaken the heart muscle, as well as heart attacks.
- Shrinkage or insufficiency of the heart valves.
- A sharp increase in blood pressure, or hypertension.
- This condition is sometimes the result of taking medications.
- Kidney failure.
- Poisoning with poisonous gas.
- Serious injuries.
- Long stay at altitude.
At first, congestion in the lungs can be confused with pneumonia. There are many cases where it is difficult to diagnose the disease in the early stages.
The doctor's examination proceeds as follows:
- temperature is measured,
- breathing is heard,
- a blood test is performed;
- An x-ray of the lungs is prescribed.
Based on the above studies, appropriate treatment is prescribed. If a person has a weak immune system, then the disease can progress on the third day. The following symptoms are identified:
- usually a person’s temperature is normal and does not rise significantly;
- breathing quickens, tachycardia develops;
- the patient speaks slowly, stopping, and is characterized by cold sweat;
- A cough with the appearance of blood, in the worst case - bloody foam, is also characteristic;
- there are complaints of weakness and fatigue, it is difficult to lie down on a low pillow, while sitting, shortness of breath goes away over time;
- the skin has a pale tint, the area between the nose and lips is bluish, swelling appears in the legs;
- It is also possible that pleurisy may occur as a result of hypoxia or other pathologies.
Also characteristic are incessant wheezing, gurgling sounds in the chest area, which can be heard without even using a stethoscope. If a person experiences initial symptoms of congestion in the pulmonary tract, then it is necessary to immediately consult a doctor.
Complaints and symptoms of pulmonary emphysema
The difficulty in timely recognition and treatment of such an irreversible condition is that the pathology does not cause any complaints or symptoms for a long time. Only over time does respiratory failure develop, which subsequently becomes a cause of disability and mortality.
Emphysema usually accompanies COPD, and its symptoms are associated with this disease. The patient's main complaints are shortness of breath and cough with sputum. Less commonly heard is a whistling sound when breathing, heaviness in the chest, weight loss. Shortness of breath appears closer to 60 years of age and worsens with colds. There is a little sputum, it is light.
Appearance of a patient with emphysema: photo
The most typical objective symptoms that the doctor determines during examination are:
- usually have a thin build;
- the position of the chest frozen in the inhalation position;
- chest shape resembling a barrel (the distance between the sternum and the spine approaches the distance between the armpits) - emphysematous chest;
- reduction of noticeable movements during inhalation and exhalation;
- widening of the spaces between the ribs, and sometimes their bulging;
- bulging areas above the collarbones;
- boxed sound when percussing the lungs;
- drooping of the lower ribs, their inactivity when breathing;
- weakened breathing.
Blueness of the skin is not typical for patients; as shortness of breath increases, their skin turns pink. They often exhale through a half-open mouth, and during inhalation they close their lips tightly.
Primary pulmonary emphysema, which has a congenital cause and is associated with alpha-1-antitrypsin deficiency, has some features of the clinical course and symptoms:
- begins at 30–40 years of age with increasing shortness of breath without cough;
- often combined with liver cirrhosis at a young age;
- weight reduced;
- very low load tolerance;
- pulmonary hypertension and corresponding heart pathology appear only at a late stage of the disease;
- characterized by an increase in total lung capacity according to respiratory function;
- the form of the disease is panacinar.
Treatment and prevention
As noted earlier, it is imperative to treat pulmonary congestion immediately after diagnosis.
Regardless of the stage of the disease, it is best to use hospital treatment, and in case of any complications, resuscitation measures are used, in particular, using an artificial respiration apparatus and oxygen masks. The patient is obliged:
- undergo an ECG;
- take an x-ray of the lungs;
- undergo an ultrasound of the heart.
Inflammation is determined by biochemistry or a local blood test.
Before prescribing treatment, it is necessary to identify what causes the stagnation. If the underlying cause is heart failure, then it makes sense to use cardiotherapy.
Therapy
If the nature of the disease is infectious, then a complex of antibacterial therapy is used. It effectively reduces the influence of microbes on lung tissue, reducing inflammation and thereby relieving congestion.
In addition, drugs are prescribed to thin sputum clots (Bromhexine, ACC). Treatment of congestion in the lungs is carried out, in addition to the use of mucolytics, with the use of herbal extracts (plantain, coltsfoot, thyme), which ensure normalization of blood flow in the lungs and reduction of inflammation.
It is also necessary to include vitamins that increase immunity in the treatment regimen (Vitrum, Supradin). Therapy is often supplemented by the prescription of diuretics to relieve swelling and normalize fluid metabolism in the body. They ensure the removal of toxins and pathogenic organisms from the body that cause stagnation.
If a person suffers from congestion in the lungs, which results in weakening of the heart muscles, then it is imperative to follow all the doctor’s recommendations and undergo the full course of treatment prescribed by a cardiologist or pulmonologist. After all, the result of untreated congestion in the lungs can be cardiac arrest.
Warning
In addition to medicinal methods, dietary nutrition based on the exclusion of salt from the diet will help to reduce the risk of developing further complications. This will help reduce swelling and normalize the flow of blood and lymph in the lung tissue. It is very important to include foods with plenty of carbohydrates, vitamins and protein in your diet. This will provide the necessary vital energy to the cells.
During an exacerbation of congestion, if the patient is forced to adhere to bed rest, even while lying down, it is worth performing as many movements as possible - turns, lifting the torso, shoulders, arms.
This helps stop the development of stagnation processes. If a person does not have the strength to do the exercises himself, then he needs to turn to loved ones for help. The patient should not be in one position for a long time, because this will only complicate breathing and the functioning of the chest organs.
A specialist in physical therapy and breathing exercises can teach you basic exercises. It is very important to breathe correctly; to develop respiratory function, you can periodically inflate a balloon or breathe into a glass of liquid using a cocktail straw.
The listed exercises help enrich the respiratory system with the required amount of oxygen. Another benefit is the increased movement of the chest, which prevents congestion. The patient is recommended to be as active as possible to combat pulmonary congestion at any stage of the disease.
Venous stagnation of the brain is a pathology manifested by excessive accumulation of venous blood in the venous system of the brain. Stagnation is characterized by the accumulation of metabolic products in the brain substance and a decrease in oxygen in the cells.
Venous congestion is not an independent disease, but the result of an underlying disease, for example, heart failure.
The outflow of blood may be disrupted from internal cavities, such as the sinuses of the brain, and external veins. The first option is rarely diagnosed due to its latent course. Impaired outflow from the superficial veins manifests itself by external signs, so the doctor notes the disease at the first contact.
Stagnation of venous blood leads to cerebral edema and increased intracranial pressure.
Violation of the tone of the venous walls. Discirculatory stagnation appears due to narrowing of the veins, causing less blood to flow through them. Causes:
- cardiopsychoneurosis;
- autonomic nervous system disorders;
- intoxication with alcohol or drugs.
Congestion not directly related to the veins. Causes:
- heart failure, in which the heart muscle weakens, losing the ability to pump out blood;
- neoplasm compressing a vein;
- traumatic brain injury, developing swelling and preventing the outflow of venous blood.
Emphysema. New treatment methods.
Emphysema is a condition in which the air sacs in the lungs (alveoli) are partially destroyed, leading to a decrease in the total surface area of the lung tissue and resulting in progressive shortness of breath.
Causes of emphysema:
- smoking tobacco and/or smoking marijuana
- air pollution, including tobacco smoke (so-called “passive smoking”)
- occupational hazards (inhalation of dust and harmful substances at work: miners, grinders, welders, etc.)
- insufficiency of alpha-1-antitrypsin (this substance “protects” the alveoli from destruction). In this case, emphysema usually occurs before the age of 40.
Emphysema most often occurs in smokers as part of chronic obstructive pulmonary disease (COPD).
What happens with emphysema?
The lungs of a healthy person consist of air passages (trachea, bronchi and bronchioles) and air sacs (alveoli). The easiest way to imagine the structure of the lungs is in the form of a tree with large branches (trachea and bronchi), which continuously branch and turn into small branches (bronchioles). At the ends of the bronchioles there are hollow air sacs called alveoli (like bunches of grapes).
The alveoli have a very thin wall (0.5 micrometers) and are enveloped in a network of small vessels (capillaries). It is through the thin wall of the alveoli that oxygen enters the blood, and carbon dioxide enters the bronchioles and is removed from the body. The lungs can also be imagined as a very finely porous sponge. Thus, the total number of alveoli in both human lungs is 600-700 million. The diameter of one alveoli is 280 micrometers (for comparison, the thickness of a human hair is about 100 micrometers). The total surface area of the alveoli varies from 40 m² when exhaling to 120 m² when inhaling. This is a huge area! It is this feature that helps the lungs quite easily “extract” oxygen from the air and deliver it to the blood.
As emphysema progresses, the fine-porous sponge turns into a large-porous sponge. The walls of neighboring alveoli are destroyed, the alveolar sacs become larger. Thus, the diameter of one alveoli increases, but ultimately the total number of alveoli decreases, thereby reducing the total surface area of the lung tissue.
The lungs can no longer effectively “extract” oxygen from the air, so shortness of breath appears and progresses. No existing medications can restore normal alveolar structure or increase the total surface area of the lungs, which is why shortness of breath due to emphysema is so difficult to treat. One of the effective ways to reduce shortness of breath is to increase the concentration of oxygen in the inhaled air from 21% to 90%, then it will be easier for the lungs to “extract” it from the air.
Symptoms of emphysema.
The main symptom of emphysema is shortness of breath. The biggest challenge to making an early diagnosis is that shortness of breath develops gradually, very slowly. Even when you already have emphysema, you will not yet feel shortness of breath and will not consult a doctor in a timely manner. At first, shortness of breath worries only during severe physical exertion, and as the disease progresses, it occurs with minimal effort (talking, washing, dressing, etc.) or even at rest. Many patients unconsciously limit their physical activity, adapting to shortness of breath until it completely disrupts their lifestyle. Unfortunately, only then does the incentive arise to go to the doctor.
Later other signs may appear:
- weight loss
- change in the shape of the chest (“barrel chest”)
- cyanosis (bluish discoloration of the skin and mucous membranes)
- swelling in the lower extremities (not everyone experiences it)
Since emphysema most often occurs as part of a specific disease, symptoms of the underlying disease are observed in parallel with the progression of shortness of breath. For example, with COPD it is a cough.
Complications of emphysema.
In the presence of emphysema, the following often occur:
- giant bullae. Bullae are areas of the lung that are filled with air but do not participate in gas exchange. Essentially, these are large but useless air sacs in the lungs
- pneumothorax (collapse of the lung, most often due to ruptured bullae)
- chronic cor pulmonale (thickening of the wall and expansion of the cavity of the right half of the heart).
Diagnosis of emphysema.
If you experience shortness of breath, be sure to consult a doctor. No experienced and competent doctor will attribute your shortness of breath to age-related features or excess body weight until he conducts a full examination.
Minimum examination plan:
- patient examination
- complete blood count (to rule out anemia as a cause of shortness of breath)
- spirometry (pulmonary function test)
- electrocardiography (ECG, to exclude shortness of breath associated with heart disease)
- X-ray of the chest organs.
In many cases, additional examination is required to confirm the diagnosis:
- body plethysmography (a very accurate test of lung function)
- echocardiography (to exclude or confirm a complication of emphysema such as chronic cor pulmonale, or to exclude other heart diseases that cause shortness of breath)
- computed tomography of the lungs. Computed tomography of the lungs is the most accurate method for diagnosing emphysema. Because This study allows you to very accurately assess the structure of the lung tissue, measure its density and identify complications of emphysema (bullas).
- pulse oximetry (to determine blood oxygen saturation; with emphysema it may decrease)
- blood gas test (to detect hypoxemia - low oxygen content in the blood).
Treatment of emphysema.
Treatment of emphysema consists of two components - conservative and surgical.
Conservative treatment:
- Quitting smoking will help stop lung damage. This is the most effective method of treatment. If you are regularly treated with medications, but continue to smoke, the effect of treatment will be so insignificant that you will not even feel it. In the presence of occupational hazards, rational employment is very important to avoid contact with harmful vapors, gases, and dust.
- Treatment of the underlying disease. Emphysema is an essential component of COPD. Treatment of COPD is discussed in a separate article. In case of alpha-1-antitrypsin deficiency, injections of a drug containing this substance are prescribed (not registered in Russia).
- Long-term oxygen therapy. Many people with severe emphysema experience hypoxemia (low oxygen in the blood) due to ineffective lung function. The only way to eliminate it is long-term oxygen therapy using an oxygen concentrator. Treatment should be carried out indefinitely, daily for at least 15-18 hours a day. Long-term oxygen therapy for emphysema as part of COPD can reduce shortness of breath, increase physical activity, improve sleep, and most importantly, prolong life by 5-10 years or wait for a lung transplant.
Surgery:
- Lung volume reduction surgery. Most often it is performed when emphysema is predominantly localized in the upper lobes of the lungs. The essence of the operation is to remove altered areas of the lungs (parts of the upper lobes of the lungs), which allows relatively unchanged lung tissue to function normally. The operation reduces shortness of breath, but does not affect the prognosis and life expectancy of the patient.
- Bullectomy (removal of a giant bulla). After removing a bulla (or several bullae), space in the chest is “freed” for relatively unchanged areas of the lung, which allows them to function more efficiently.
- Lung transplantation.
A radical method of treating severe pulmonary emphysema, which has become available in Russia. Surgical treatment is performed only if conservative treatment is ineffective.
Call right now at 8 (495) 636-28-25 and get quality advice regarding the choice of equipment!
Symptoms
Minor venous congestion develops general cerebral symptoms and signs of inhibition of higher nervous activity:
- Headache, fatigue, dizziness.
- Vomiting with occasional nausea.
- Irritability, emotional lability, sleep disturbance.
- Depression of consciousness, lethargy, apathy, drowsiness. These symptoms may rapidly change into mental agitation, euphoria, and goofy behavior.
- External signs: blue complexion, bulging jugular veins, bulging superficial vessels of the head.
Severe venous congestion leads to cerebral edema. The pathology develops with impaired consciousness and the formation of negative neurological symptoms (loss of neurological functions). The first convulsions appear. A coma may develop.
There are three leading syndromes in the dynamics of cerebral edema:
General cerebral
It is formed due to increased intracranial pressure. Drowsiness and apathy develop - symptoms that have an unfavorable prognosis. The slow dynamics of increase in intracranial pressure is manifested by morning headaches, due to which the patient begins to vomit, after which the patient feels better. Mental changes gradually increase: fear of death, anxiety and agitation appear.
A rapid increase in intracranial pressure is characterized by severe and acute headaches, nausea and vomiting, which does not alleviate the patient’s condition. Motor reactions slow down, the heart beats slower. The psyche is inhibited: drowsiness, apathy, deterioration of attention and memory, thinking and reaction to stimuli slow down, contact with the patient becomes more difficult.
Diffuse rostrocaudal increase in neurological signs
The transition to this stage means that the subcortical and stem parts of the brain have begun to be involved in the pathological process. Generalized clonic convulsions appear (alternating muscle relaxation and contraction).
Mental arousal and anxiety develop, muscle tone increases, up to opisthotonus, in which the patient arches his back, taking an arched position. The muscles of the arms and legs are extended. Grasping and defensive reflexes are activated. The pupil reacts poorly to light.
If the swelling goes lower - to the diencephalon and midbrain - impaired consciousness develops. The patient falls into a comatose state, and important functions for life are disrupted: heartbeat and breathing.
With venous stagnation of the structures of the medulla oblongata, breathing is disrupted, developing according to the Biot type (periodic stops of breathing for up to one minute) and the cardiovascular system is upset: the pulse slows down, the pressure decreases.
Brain dislocation
When venous congestion develops to the limit, some brain structures are displaced and dislocation syndrome develops. Most often, the occipital and temporo-parietal lobes of the brain are displaced. The rhythm of breathing and heartbeat is upset. The oculomotor nerves are affected (the eyelids droop, the eyes diverge). Consciousness is depressed to a comatose state.
Diagnostics
Diagnostic criteria for venous stasis can be reliable and indirect.
Reliable signs are revealed using instrumental research methods:
- Nuclear magnetic resonance imaging.
Indirect symptoms are determined by the patient’s appearance (impaired consciousness, suppressed reflexes, interruptions in breathing and cardiac activity). They are also detected on:
- Electroencephalography.
- Fundus examination.
- Study of the state of cerebral vessels.
Emphysema: diagnosis
Laboratory methods for the symptoms of this pathology are of auxiliary value. The content of red blood cells and hematocrit in the blood increases, which reflects the body's adaptation to the lack of oxygen.
If concomitant COPD is moderate or severe, the patient undergoes pulse oximetry. If the level of blood oxygen saturation during this study is less than 92%, a study of its gas composition is indicated.
Bullous emphysema on CT scan
If symptoms of the disease occurred in a person under 45 years of age, or there were family cases, it is necessary to determine alpha-1-antitrypsin in the blood.
Instrumental diagnosis of pulmonary emphysema:
- a study of external respiration function reveals a decrease in vital capacity and expiratory flow rate, signs of mixed obstructive-restrictive breathing disorder and irreversible bronchial obstruction appear.
- X-ray of the lungs, which reveals emphysematous lungs - transparent, increased airiness, darker than normal;
- Computed tomography is the most accurate diagnostic method.
Treatment and exercises
Treatment of cerebral venous congestion is an emergency measure that is carried out in the intensive care unit.
When treating, doctors have several goals:
- Eliminate swelling.
- Normalize intracranial pressure.
- Ensure normal outflow of venous blood.
- Saturate tissues with oxygen.
- Eliminate pain and provide comfort to the patient.
- Maintain vital functions of breathing and heartbeat.
To prevent venous stagnation, you should exercise:
- Immediately after sleep, get out of bed and get on your knees. You need to touch your forehead to the floor while exhaling deeply. Inhale while returning to the starting position. Repeat 5 times.
- Standing position. Feet shoulder width apart. Make circular movements with your head for 30-60 seconds.
- Lying position on your back. Extend your arms along your body. Raise your legs at the pelvic joint without bending your knees. Repeat 10 times.
- Standing position. Stand with your back to the wall and press your head against it. Try to “move” the wall with your head, actively using your neck muscles. One approach takes 5 seconds. Repeat the exercise 5-7 times.
Venous stasis is a pathology characterized by obstructed outflow of venous blood, while arterial inflow is normal. This occurs due to poor elasticity of the vessel walls, as well as high blood viscosity.
In this case, tone is first lost, and then blood flow becomes difficult. The localization of the pathology is determined by the accumulation of venous vessels, so there are several places: the pelvis (legs), brain, lungs, kidneys, neck.
How to treat emphysema
No specific therapy for pulmonary emphysema has been developed at this time. First of all, it is necessary to completely eliminate those factors that lead to the development of this disease. That is, you definitely need to give up habitual intoxications. If severe emphysema is observed, it may even be necessary to change jobs if the patient is exposed to toxic effects that lead to the development of the disease.
Often this disease does not require hospitalization of the patient if he is in satisfactory condition. Treatment is carried out on an outpatient basis with mandatory supervision of the attending physician or pulmonologist. The patient is hospitalized in the pulmonology department of the hospital only if an infectious component has appeared or a complication has developed. Because these conditions require urgent measures, which should be carried out by a highly specialized specialist in a hospital setting.
Treatment of emphysema, like any other disease, should be carried out comprehensively. To achieve the best result, it should consist of the following components:
- Diet therapy. The patient's diet must be correct and balanced. It is advisable to follow a low-calorie diet high in raw fruits and vegetables. It is necessary to reduce the consumption of carbohydrates, since these elements can lead to a lack of oxygen in the patient’s body, which will further aggravate his condition.
- Medicines. Treatment is mainly symptomatic. In case of exacerbation of the process, the patient is prescribed therapy with broad-spectrum antibacterial agents. Also, if the patient suffers from a chronic form of the disease, then he must use bronchi dilating drugs on an ongoing basis. Such drugs include salbutamol, theophylline, which can be either in tablet form or in the form of inhalation. If there are problems with sputum discharge, patients should use a mucolytic agent.
- Oxygen therapy. Used to improve gas exchange in the lungs. The procedure involves the patient inhaling an air mixture with a reduced amount of oxygen, and then breathing air with a normal oxygen content. Such procedures should be carried out in cycles of 15-20 days. This therapy is especially indicated if emphysema occurs in children.
Causes
Thanks to heart contractions, which give an impulse for the movement of blood, the work of arterial vessels is facilitated. In the case of venous outflow, the situation is complicated by the fact that the only stimulators for it are contractions of the calf and abdominal muscles, as well as the arch of the sole. Breathing has a certain, albeit insignificant, effect on the flow of blood through the veins, even the heart has some effect on the return blood flow, yet the main responsibility lies with the muscle pump, which, figuratively speaking, squeezes blood out of the veins and activates the valves that are required to prevent the return flow blood.
But the functioning of the muscle pump may be impaired. The modern pace of life is characterized by rapid technological progress, which contributes to the emergence of an increasing number of benefits of civilization. Yes, the person began to move faster, but he began to move less. It is physical inactivity that is the provoking factor, due to which not only problems such as obesity, heart problems, and so on develop, but also venous stagnation (stasis, hyperemia - other names for the disease).
Since the basis of movement is the legs, physical inactivity causes the development of venous congestion in the legs in the first place. If this disease occurs in an acute form, there is a strong increase in pressure in the vessels, due to which their walls lose elasticity, the diameter becomes larger, and the speed of blood flow gradually decreases.
So, over time, a diagnosis appears in the patient’s card under the ominous name “venous insufficiency”.
Venous stagnation of blood in the pelvis is a common type of sluggish hyperemia. This poses a great danger to women. The fact is that stagnation in such an important organ as the uterus can lead to a woman being unable to have children at all, giving birth to premature babies, or experiencing a miscarriage. This disease is most common in people who, again, lead an inactive life, move little, sit a lot, and eat poorly. Various factors can provoke the development of the disease:
- the use of hormonal drugs that prevent conception;
- hereditary problems with vascular tone;
- temporary heavy stress of a psychological and physical nature;
- pregnancy;
- complications after childbirth.
Pregnancy can provoke the development of the disease.
Venous congestion in the head is most often the result of pathology inside and outside the skull. The disease is provoked by:
- heart problems;
- head injuries;
- dropsy of the brain;
- aneurysm;
- problems with the lungs and bronchi;
- vein thrombosis;
- tumors in the neck.
Venous congestion in the lungs manifests itself in poor blood flow through the veins of this organ. For this reason, blood accumulates in the lungs, so their tissue becomes denser, becoming brown in color. This situation leads to increased vascular permeability and stagnation in the pulmonary circulation. In addition, connective tissue grows in the vessels, that is, sclerosis occurs.
Regardless of where the pathology is localized, it is clear that a sedentary lifestyle, heavy lifting, bad habits, prolonged standing in an upright state, hereditary predisposition, the risk of manifestation of which increases in the presence of these factors - all this has a bad effect on the condition of the venous vessels . They lose their elasticity, and the blood in them begins to move poorly, which leads to its stagnation. In this case, it is necessary to identify the symptoms in time in order to begin treatment immediately. The emergence of more serious problems in the future depends on this.
What is bullous emphysema
With emphysema, the bronchi and alveoli lose their elasticity. Single or multiple bullae or blisters form within the tissues. They are what causes bullous emphysema. Air fills the bullae, but for various reasons does not come out of them. As a result, the walls of the blisters stretch, become thinner, and the size of the bullae increases. Sometimes the size of the bubbles exceeds 10 cm. The bubbles are very often located nearby, one above the other. They put pressure on healthy lung tissue, making breathing very difficult.
Bullous disease can be complicated by rupture of bullae and the occurrence of spontaneous pneumothorax. Burst of blisters can be caused by physical effort and severe coughing. The pathology develops gradually. Its beginning may be related to:
- unfavorable environment;
- smoking tobacco;
- hereditary reasons.
At their core, bullae are large, but useless air sacs for breathing. Bullous disease reduces the total area of healthy lung tissue. With timely diagnosis, it can be treated, like any emphysema; not only the patients themselves, but also their loved ones should know what it is and how to treat it.
Symptoms
The nature of the symptoms directly depends on the form of the disease:
- Venous stasis in the legs: low local temperature, sensations of overstrain and heaviness, the skin becomes bluish, small hemorrhages are observed in the area of the accumulation of veins, trophic ulcers appear, swelling in the evenings.
- Venous stagnation in the pelvis. A person complains of discomfort in the rectum. This is expressed in tingling, itching and pain after defecation. Bleeding and prolapse of hemorrhoids may even occur.
- Brain. Stasis in this area is manifested by pain with movement and strain. The veins located in the fundus are varicose. The pressure in them is 50-80 millimeters of mercury. Dizziness is observed, the person complains of hum and noise. With stasis in the brain, the face becomes cyanotic, the lower eyelids swell in the morning. Other symptoms of brain congestion: fainting, poor sensation in the legs, increased pain when drinking alcohol and emotional stress.
- Venous stagnation in the small circle. A person complains of shortness of breath, which may be systematic and constant, and cough. Moreover, when you cough, sputum is released, but this process is difficult. There may be blood streaks in it. There is swelling of the lower leg.
With stasis in the brain, dizziness is observed
Diagnostics
The doctor diagnoses the disease and makes an accurate diagnosis based on the symptoms listed and the results of additional studies. He questions the patient and examines the skin. If the diagnoses are confused, treatment will be ineffective and subsequently venous hyperemia will lead to dangerous consequences.
For example, if there are problems in the pelvis, an ultrasound scan of the organs located in it is performed. Brain congestion is diagnosed using phlebography, cubital vein pressure measurement, skull x-ray, MRI or CT scan. In the case of the lungs, auscultation is very important. When listening to the lungs, the doctor detects wheezing, especially in the back and lower parts.
Treatment
Treatment largely depends on the cause of venous hyperemia. First, doctors advise making your life more active, playing sports, training your body, if there are no contraindications to certain exercises.
If you stop smoking, drink large quantities of alcohol and establish proper nutrition, the condition of your blood vessels will improve. The rheological properties of blood will improve if you add more greens and vegetables to your diet.
Detralex belongs to the group of venotonics.
Venotonics help to cure venous stagnation. They have various actions: they increase the elasticity of the vein walls, normalize their properties, and prevent the development of inflammation. In addition, a well-known anticoagulant, heparin, is used. It is used for various diseases, including those that could be a consequence or cause of blood stagnation.
- If venous congestion occurs in the lungs, treatment for heart failure is given. Surgery is also possible. If the congestion of the lungs is persistent, disability may be assigned.
- Congestion in the brain is treated by reducing venous pressure, so aminophylline is often present in the prescription. In addition, therapy is prescribed to reduce congestion and the severity of edema. For stasis in the brain, laser-LED therapy, massage of the collar area, reflexology, and herbal medicine can be prescribed.
- Venous congestion in the pelvis is treated conservatively. This treatment is based on the use of drugs and suppositories for vaginal administration. Surgery may also be used.
- Hyperemia in the legs is treated with medications and folk remedies. Unfortunately, there are no effective drugs yet, but there are means aimed at preventing complications. Surgery may be used. To alleviate the course of the disease, it is important to engage in therapeutic walking, use ointments, and compression stockings.
Important facts about emphysema
Here are some key points regarding emphysema:
- In most cases, chronic obstructive pulmonary disease (COPD), and therefore emphysema, develops as a result of smoking.
- Emphysema is only rarely associated with a congenital condition called alpha-1 antitrypsin deficiency.
- Shortness of breath and cough are the main symptoms of emphysema.
- Doctors diagnose COPD and emphysema usually after a diagnostic procedure called a pulmonary function test to measure the vital capacity of the lungs.
- Spirometry is used in diagnostics to measure the volume of air exhaled in one second after a deep breath.
- Treatment cannot stop or reverse lung damage, but it can relieve symptoms and prevent flare-ups.
- Medicines and adjuvant therapies are the mainstay of treatment for emphysema.
- Treatment for emphysema includes inhaled bronchodilators, corticosteroids, and, when infection is present, antibiotics.
- Supportive care includes oxygen therapy, dietary modification, smoking cessation assistance, and other educational interventions.
- Surgery, including lung transplantation, is usually indicated for severe cases of emphysema.
- People with emphysema and COPD are recommended to get an annual flu shot and may also be recommended to get a pneumonia shot every 5 years.
Consequences
Venous hyperemia can have its unpleasant consequences. They consist in impaired nutrition of the pathological area. The degree of negative changes depends on the volume of pathology, time of stagnation, and recovery capabilities. The consequences are compactions, atrophy of tissues and organs. For example, specific brown myocardial atrophy may develop. If the stasis is prolonged, connective tissue elements grow, and the parenchyma accumulates carbonic acid.
Occlusion of the collar zone leads to the accumulation of a large volume of blood in the organs. Because of this, blood pressure drops, and organs experience oxygen starvation. Cerebral ischemia and respiratory paralysis may develop. The most terrible consequence is death.
But all this can be avoided in two ways. The first is prevention. It is based on an active lifestyle, quitting smoking and proper nutrition.
The second way is timely detection of the disease and effective treatment. Doing all this is not difficult and is very important to prolong life and make its course more pleasant.
What is emphysema
This disease increases the amount of air in the alveolar tissue of the lungs more than normal. Excess gas that accumulates in the organ can lead to a number of complications, for example, damage to bronchial tissue. The disease emphysema provokes excess gases not due to the addition of oxygen, but due to retention, accumulation of carbon dioxide and other impurities. This leads to disruption of the normal blood supply to the lung tissues and to their destruction. Pressure increases inside the organ, and compression of nearby organs and arteries occurs.
Kinds
This pathology is divided into several types and forms. Each of them has specific symptoms that can be detected during diagnosis and history. Emphysema can be acute or chronic (the latter is extremely rare in children). Moreover, each of the forms has an unfavorable prognosis without proper therapy. Types of emphysema:
- paraseptal;
- diffuse;
- panlobular;
- bullous
Why is emphysema dangerous?
The disease leads to irreversible changes in the structure of organ tissue, which manifests itself in the form of pulmonary failure. This is one of the reasons why emphysema is dangerous. Pulmonary hypertension leads to a significant increase in the load on the right myocardium. Because of this, some patients develop right ventricular heart failure, edema of the lower extremities, myocardial dystrophy, ascites, and hepatomegaly.
The timeliness of detection of the disease directly affects the further prognosis. Ignoring the problem and treatment measures leads to progression of the pathology, loss of the patient’s ability to work and further disability. In addition to the disease itself, complications of pulmonary emphysematosis pose a serious threat to human health.
- Ninth month of pregnancy
- How to freeze zucchini in the freezer
- Fitness classes at home for weight loss
Life forecast
Emphysematous lungs cannot be completely cured. Even with treatment, the pathology continues to progress. Timely visit to the hospital, compliance with all medical recommendations and therapeutic measures helps to slow down the disease, improve the standard of living, delay disability, and reduce mortality. The prognosis for life with pulmonary emphysema due to a congenital defect is usually unfavorable.