Thus, in acute appendicitis it is often possible to distinguish between the initial and final localization of pain (V.I. Kolesov).
For a typical attack of acute appendicitis, the final localization of pain in the right iliac region is the most common and characteristic symptom.
Localization of initial pain in the epigastric region, regardless of the location of the appendix, is characteristic mainly of destructive forms of acute appendicitis.
| Classification of acute appendicitis By the nature of morphological changes | According to the prevalence of the pathological process | According to the clinical picture | According to the clinical course | ||
| 1. Simple (over | 1. Uncomplicated | 1. | From a typical wedge | 1. | Fast regression |
| catarrhal, catarrhal | chesk picture | raging | |||
| ny) appendicitis | |||||
| 2. Phlegmonous | 2. Complicated: | 2. | From an atypical wedge | 2. | Non-progress |
| appendicitis | - appendicular | chesk picture: | raging | ||
| infiltration | - with dizurnic | ||||
| - appendicular | disorders | ||||
| 3. Gangrenous | abscess | - with symptoms for | 3. | Slow progress | |
| appendicitis | - local peritonitis | biliary diseases | sibling | ||
| - spilled perito | exit paths | ||||
| nit | - with diarrhea | Rapidly progress | |||
| 4. Perforated | - others are more difficult | - with signs of cha | 4. | ||
| appendicitis | niyami (retroperitoneal | yellow purulent | raging | ||
| phlegmon, interintestinal | intoxication | ||||
| abscesses, etc.) | - with hyperpyrexia | ||||
Causes and pathogenesis of appendicitis
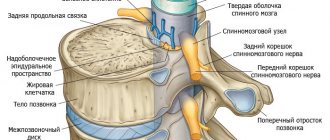
The development of appendicitis is traditionally associated with the activation of microorganisms in the intestine against the background of blockage of the lumen of the appendix by a tumor, fecal stone, intestinal parasite or hyperplastic lymphoid follicle. Obturation of the appendix naturally leads to increased accumulation of intestinal mucus in it, containing a number of opportunistic bacteria. Their active growth causes inflammation, which can result in ischemia of the walls of the appendix, their necrosis or suppuration with the formation of an abscess, and then phlegmon. In addition, increasing mucus pressure in the appendix can contribute to its perforation with the occurrence of diffuse peritonitis.
The cause of gangrenous appendicitis may be thrombosis of the appendicular artery, which is more common in patients with diabetes mellitus, as well as in the elderly.
Etiology
Acute catarrhal appendicitis is provoked by various pathogenic factors and mechanisms. Clinicians have identified the following main causes of the disease:
- pathogenic microorganisms present in the organ;
- intestinal infections;
- problems with appendix contraction;
- stones and undigested parts of food;
- transfer of inflammation from other organs and peritoneum.
While determining the possible factors provoking the formation of the disease, doctors identified several theories. If we consider the disease from the allergic side, then inflammation can form under the influence of an allergic reaction of types 3 and 4. For this reason, the permeability of the walls of the process increases, which leads to the penetration of opportunistic flora into the middle.
According to the nutritional theory, the appendix can be affected due to a lack of fiber and dietary fiber in the diet, as well as from a large amount of meat. Due to this factor, the movement of food masses in the intestines is disrupted, and the evacuation of contents from the colon worsens.
Often the risk group consists of people with the following parameters and ailments:
- young age – from 12 to 17 years;
- the presence of infectious diseases in the intestines;
- inflammation in the pelvis;
- weakened immune system;
- impaired bowel function;
- fecal stones;
- helminthiases.
In medicine, secondary catarrhal appendicitis is also diagnosed. It is formed under the influence of the inflammatory process in other organs, which progressed to the appendix. It is quite difficult to diagnose, and such a pathology can only be truly established during surgery.
The following diseases can provoke inflammation in the appendix:
- peritonitis;
- intestinal diverticulum;
- Crohn's disease;
- adnexitis;
- destructive cholecystitis;
- stomach and duodenal ulcers;
- enterocolitis;
- enteritis.
Clinical medicine specialists identify several reasons that provoke the development of pathology:
- pathogenic microorganisms existing in the body;
- intestinal bacteria;
- improper functioning of the appendix during contractile movements;
- ingestion of particles, undigested food and stones;
- inflammatory processes in other organs, which eventually spread to the appendix.
Morphological picture of acute appendicitis
Today, experts distinguish two main forms of acute appendicitis - simple and destructive. Destructive, in turn, is divided into phlegmonous, gangrenous and perforated appendicitis.
1. Simple catarrhal appendicitis is characterized by thickening of the appendix and its infiltration with leukocytes. The patient's blood shows typical laboratory signs of an inflammatory process, such as leukocytosis, an increase in erythrocyte sedimentation time, and a shift in the leukocyte formula to the left.
2. The phlegmonous form of appendicitis is characterized by the presence of purulent discharge in the intestinal lumen, as well as more pronounced local changes, signs of ulcerative defects on the surface of the appendix.
3. Appendicitis is considered to be gangrenous, in which the appendix is subject to oxygen starvation and the appearance of areas of necrotic tissue. Externally, necrosis appears as dirty green or brown areas on the surface of the appendix.
Read also Colon cancer - complications, treatment, surgery
4. Perforated appendicitis occurs when there is increased pressure inside the blocked appendix, when the necrotic area is simply squeezed into the abdominal cavity. Its infected contents are poured there, causing severe purulent peritonitis.
Under certain conditions, sometimes delimitation of the inflamed appendix occurs with the formation of an infiltrate of the iliac region. This is the so-called “chronic appendicitis”, which is treated conservatively at the initial stage.
Treatment and rehabilitation
Surgery is the only possible treatment option today.
The only possible treatment, unfortunately, is appendectomy - surgical removal of the inflamed appendage. Surgical procedures last about half an hour. If there are any complications, time drags on. Traditional appendectomy is used more often. In this surgery, an incision is made in the abdomen at the site of pain, and then the appendix is pulled out and removed. Next, a surgical suture and bandage are applied. The disadvantage of this manipulation is a very noticeable scar.
In addition, there is laparoscopic appendectomy. This is a modern type of surgery. Removal of the inflamed appendix is carried out through barely noticeable punctures in the abdomen. After this manipulation, the scar on the body is almost invisible. Drug treatment does not solve this health problem. After the operation, the patient receives the necessary medications (tablets, droppers with solution, dressings). After some time (7-10 days), if necessary, the stitches are removed. Both methods have their advantages and disadvantages. However, laparoscopic appendectomy makes surgery safer, because there is less blood loss. As a result, the risks from the surgical and rehabilitation period become minimal. A significant disadvantage of this method is the insufficient supply of medical institutions in provincial cities.
The post-rehabilitation period includes physical recovery (minimal exercise) and diet. You can’t immediately include familiar dishes into your diet. First, the food should be liquid: soups, broths with second water, purees, as well as low-fat fermented milk products. Eliminate solid foods, smoked foods, salty, sour, fatty foods, soda and coffee. You need to approach the diet responsibly, because if it is not followed, the internal sutures on the appendix may come apart. From a month to six months the patient monitors his diet. By following the doctors' recommendations, the patient will recover faster.
Symptoms of appendicitis
The symptoms of acute appendicitis depend on each specific form of the disease, but the onset of the inflammatory process is usually similar. Patients note moderate pain in the upper abdomen (epigastric region), which gradually descends, localizing in the right iliac region - the so-called “pain transfer” symptom, or Kocher-Volkovich symptom. This symptom is observed in approximately half of the cases.
Often, pain with appendicitis may initially bother you in the navel area or immediately in the right iliac region. In this case, the pain, as a rule, does not radiate, intensifying as the disease progresses. At the final stages of necrotizing appendicitis, the pain syndrome decreases while all other clinical and laboratory signs are preserved. This only means that the ischemic zone also included areas with nerve endings.
Somewhat later nausea and vomiting follow. In some cases, diarrhea or constipation is noted, the temperature may be low-grade or rise to extremely high levels. There are phenomena of general intoxication.
An objective examination reveals local tension in the muscles of the anterior abdominal wall.
Positive symptoms of appendicitis are revealed:
|
|
|
|
|
|
|
Read also Acute cholecystitis - causes, symptoms, treatment, surgery
With an atypical location of the appendix, the clinical picture changes, making it difficult to diagnose acute appendicitis. The appendix can be located subhepatically, retrocecally, laterally, medially. With the pelvic location of the appendix, appendicitis simulates diseases of the genitourinary system and requires consultation with a gynecologist or urologist with additional research methods.
An even rarer case is an anomaly such as transposition of internal organs. In this case, the vermiform appendix, and therefore all the symptoms, are shifted to the left iliac region.
Stages of the disease
When performing late or incorrect surgical intervention, the patient may develop the following consequences:
- adhesions;
- hernia;
- peritonitis;
- suppuration and perforation of the organ;
- bleeding;
- infiltrate;
- pylephlebitis.
The vermiform appendix becomes inflamed due to the action of bacteria. In a normal state, they do not have a negative effect - the mucous membrane protects. An etiopathogenetic factor can weaken the protective function. For example:
- Blockage of the lumen of the process. There is a constant formation of mucus in it. When the lumen of the appendix closes, the fluid does not go away, but accumulates. The process is stretched and therefore the mucous membrane is damaged.
- Changes in blood flow. When arteries become clogged, the process lacks nutrition and its protective function is reduced.
- Unhealthy food. In order for the intestinal walls to contract, vegetables and fruits are needed. If there is a shortage, feces stagnate, which takes on a stone appearance and clogs the lumen.
- Allergy.
- Increased tendency to change bowel habits. Frequent constipation does not move stool; it ends up in the appendix.
Mechanism of development of appendicitis:
- The tissues of the appendix swell and increase its size;
- Toxic substances irritate the peritoneal area;
- Intestinal function is disrupted;
- Toxic substances penetrate the bloodstream, the temperature increases.
Possible complications due to untimely treatment:
- Appendiceal infiltrate. If the operation is not performed on time, pain and fever up to 37 degrees appear.
- Pus in the abdominal cavity. The person suffers from severe pain and elevated body temperature. Surgically treated by opening.
- Peritonitis. The severe stage is when pus enters the stomach. Without proper treatment, death is possible. It is treated by prescribing antibacterial agents and surgery.
- Pylephlebitis. A rare form, but dangerous. Associated with pus entering the veins, blood clots form. For treatment, medications with antibacterial action are prescribed.
There is still no consensus on the reasons for the development of acute appendicitis. Among the etiological theories of acute appendicitis, mechanical, infectious, angioneurotic, allergic, immunological, etc. are discussed. It is believed that the leading factor in inflammation of the appendix (appendicitis) is mechanical blockade of the lumen of the appendix caused by fecal stone, foreign body, parasites, hyperplasia of lymphoid tissue. This leads to the accumulation of mucus in the appendix, activation of the bacterial flora, inflammation of the walls of the appendix, and vascular thrombosis.
According to the infectious theory, the development of acute appendicitis can be initiated by various infectious diseases - amoebiasis, parasitic infections, tuberculosis, yersiniosis, typhoid fever, etc. Proponents of the angioneurotic theory are of the opinion that trophic disorders in the wall of the appendix, associated with a violation of its innervation, are of primary importance.
To a certain extent, a nutritional factor can contribute to the development of acute appendicitis. It is known that eating predominantly meat foods contributes to disruption of intestinal motor-evacuation function and a tendency to constipation, which, in turn, predisposes to the development of acute appendicitis. Also, unfavorable background factors include intestinal dysbiosis, decreased body resistance, and some types of location of the appendix in relation to the cecum.
Acute appendicitis is caused by nonspecific microbial flora: anaerobic non-spore-forming microorganisms (bacteroides and anaerobic cocci - in 90% of cases), aerobic pathogens (Escherichia coli, enterococci, Klebsiella, etc. - 6-8%), less often - viruses, protozoa present in the appendix . The main mechanism of infection of the appendix is enterogenous; lymphogenous and hematogenous routes of infection do not play a leading role in the pathogenesis of acute appendicitis.
There are four stages of the disease, depending on the severity of the disease:
- Catarrhal form of appendicitis or the first stage. Symptoms appear in the evening or at night. A lingering pain appears in the stomach area, and later vomiting begins. It may seem to the patient that gastritis has begun, the stomach is soft, and the pain gradually moves to the right side. The stage lasts about 12 hours, and this is the most favorable period for the operation, but at this stage rarely does anyone seek help.
- The next stage is catarrhal phlegmonous appendicitis. This stage lasts about a day. The pain becomes throbbing, the heart beats faster, the body temperature rises, but not higher than 38 degrees. On palpation, hardening is observed on the right side of the lower abdomen.
- The gangrenous form begins already on the second or third day after the appearance of the first symptoms. The process of death of the nerve endings of the organ develops, so the pain subsides. Body temperature drops to 36 degrees. Increased pain is typical only for the palpation procedure.
- At the last perforative stage, through holes appear in the organ. The pain is constant and severe. Abdominal bloating and tachycardia are observed. A dark brown coating appears on the tongue.
Despite the prevalence and fame of the disease, its etiology is unclear. A large number of theories have been put forward, each of which is inextricably linked with the others. However, in each of the versions of the occurrence of pathology, the following prerequisites appear:
- Impaired motility of the appendix due to its obstruction or bending.
- Poor circulation as a result of vasospasm.
- Activation of bacterial activity.
- Decreased protective function of the appendix.
One of the determining factors in the development of the disease is the nutritional factor, which activates putrefactive processes in the appendix and upsets the balance between bacteria and the barrier function of the organ.
The causative agents of inflammation are microorganisms that are located in the appendix. In preschool children, the main cause is helminthic infestation.
If you do not go to the hospital in a timely manner or undergo late surgical treatment, complications may occur:
- appendicular infiltrate;
- abscesses: periappendicular and pelvic;
- peritonitis;
- perforation of the appendix.
Infiltrate
Appendiceal infiltrate is a set of tissues connected by adhesions around the appendix. This is the body's attempt to prevent inflammation from spreading. A characteristic sign of the formation of an infiltrate is the cessation of abdominal pain and improvement in the patient’s well-being. Objectively, the surgeon notes the disappearance of muscle tension.
The infiltrate develops on the 3rd–5th day from the onset of the disease. Upon palpation, a dense formation is detected at the site of the appendix.
Treatment measures include:
- compliance with bed rest;
- cold to the location of the inflamed organ;
- taking antibiotics;
- a diet of easily digestible foods.
When the infiltrate resolves, to eliminate the risk of recurrence of appendicitis, a planned appendectomy is performed 3–4 months after discharge from the hospital.
Abscess
If the patient again notices pain at the site of the appendix and the surgeon notes an increase in the size of the infiltrate upon palpation, then a periappendiceal abscess is suspected.
Treatment for the development of a periappendiceal abscess in a patient is only surgical. However, during an operation to open the abscess that has formed, the inflamed appendix is not removed. Because the surgeon, when searching for the affected organ among the pus, may unintentionally injure the thin intestinal loops, which will lead to bleeding.
Ways to get rid of catarrhal appendicitis
Once the diagnosis is made, the patient should receive proper treatment.
The success of the operation depends on the amount of time that has passed since the onset of symptoms. Ideally, it should be carried out no later than 1 hour after the surgeon determines the disease. The main stage of the operation is appendectomy. It involves removing the appendix. There are several types:
- Open intervention. Simple and fast method. No special equipment required.
- Laparoscopic method.
Any type is performed using general anesthesia.
Laparoscopy for appendicitis - it is possible to use the technique to diagnose and treat the disease. The surgeon introduces equipment equipped with a camera. The advantage of this method is that the specialist can examine the entire affected organ. The operation is performed in cases where:
- The person is seen by a specialist for a long time, the presence of appendicitis is unclear;
- Symptoms are similar to gynecological diseases;
- A patient with diabetes mellitus. The person cannot be observed; complications develop quickly;
- Overweight person. If another method is used, the suture takes a long time to heal, and this can lead to suppuration;
- The patient requests this procedure.
Complete treatment of the acute form with medications without surgery is impossible. Medicines are used as an additional measure to surgical treatment.
Medicines:
- Cefuroxime.
- Clindamycin.
- Metronidazole.
- Trichopolum.
Attention! Antibiotics are dispensed with a prescription form from a doctor.
The use of treatment methods with folk remedies is unacceptable. Appendicitis requires emergency surgery.
Differential diagnosis
In most cases, differential diagnosis is required to clearly establish the diagnosis. Indeed, at any stage of catarrhal appendicitis, the symptoms may be too similar to the signs of other diseases:
- cholecystitis;
- pancreatitis;
- ulcer;
- gastroenteritis and others.
That is, in order not to confuse inflamed appendicitis with other diseases in the abdominal cavity, differential diagnosis is carried out.
Why does it happen?
Among surgical diseases in the abdominal cavity, acute appendicitis is the leader - in 90 cases out of 100, and it is the most common cause of peritonitis. If we talk about the prevalence of the disease, then there are approximately 4-5 cases per 1000 people. It is known that there are many more women among the patients, children are also susceptible to the disease, the most dangerous age is 20-40 years.
An inflammatory process in the appendix can occur due to:
- its contractions are incorrect and, as a result, feces will appear in its cavity;
- undigested pieces of food (for example, nuts, seeds) blocking the passage;
- pathogenic microorganisms that have entered the vermiform appendix;
- intestinal infections - bacterial and viral;
- inflammation that has passed from another organ;
- abdominal injuries.
Chronic form
Diagnosis of chronic appendicitis is much less common. Making an accurate diagnosis is complicated by the unclear and vague clinical picture of the disease.
The symptoms of the disease are not bright, the pain syndrome is distorted, there are no changes in the cavity of the appendix.
The following signs are noted:
- In the chronic form of the disease, the lumen of the appendix narrows. This leads to the accumulation of gas, pus and swelling fluid.
- The nature of the pain syndrome is insignificant.
- The pain can intensify after eating or even the slightest physical activity.
- Abnormal bowel habits such as diarrhea or constipation are noted.
We recommend reading: Is it painful to do a colonoscopy without anesthesia: reviews and feelings of patients, consequences
When palpating the abdominal cavity, the patient feels a pain effect on the right. There is a feeling of discomfort when trying to raise the right leg.
The tone of the muscle tissue in the right area of the peritoneum is significantly reduced. While walking, the right leg gets tired faster than the left.
If you turn to medical statistics, you can get quite disappointing data.