Conjunctivitis
(
conjunctivitis
) is an inflammation of the conjunctiva of predominantly infectious etiology, which is the most common eye disease with a favorable outcome.
The incidence of conjunctivitis is explained by the fact that the conjunctival sac, due to its anatomical position, is accessible to all kinds of external influences, and the conjunctiva itself (see) is highly reactive, easily responding to various influences of an endogenous and exogenous nature.
Classification
The most widespread etiological classification of Conjunctivitis is divided into:
1. Bacterial Conjunctivitis - acute bacterial, epidemic Koch-Wicks Conjunctivitis, Morax-Axenfeld blepharoconjunctivitis, blenorrhea of newborns and adults (see Blennorrhea), diphtheria Conjunctivitis.
2. Viral Conjunctivitis - adenoviral Conjunctivitis, epidemic keratoconjunctivitis, epidemic hemorrhagic Conjunctivitis with influenza, herpetic disease, Newcastle disease.
3. Conjunctivitis with inclusions - paratrachoma (see Trachoma).
4. Allergic, or toxic-allergic, conjunctivitis - phlyctenular keratoconjunctivitis, atonic (hay), medicinal, nutritional, spring catarrh (see).
5. Fungal Conjunctivitis.
6. Conjunctivitis that develops under the influence of various physical, chemical factors and radiation energy.
According to the nature of the inflammatory process, acute, subacute and chronic conjunctivitis is distinguished, and according to pathological features - catarrhal, purulent, membranous and follicular.
Allergic conjunctivitis in children and adults
Diagnosis of the disease is carried out on the basis of skin tests, various studies and allergy tests.
In this article
- Allergic conjunctivitis in children and adults
- Causes of allergic conjunctivitis in children and adults
- Development of allergic conjunctivitis
- What are the signs of infection with allergic conjunctivitis?
- Methods for diagnosing chronic allergic conjunctivitis
- Treatment of allergic conjunctivitis at home
- Precautions when using folk remedies
If a diagnosis of “allergic conjunctivitis” has been made, a variety of drugs are usually prescribed for treatment, which are taken orally and locally, eliminating allergy symptoms and suppressing the effects of the allergen.
According to statistics, about 15% of the population suffers from allergic conjunctivitis. It is quite a serious problem. Allergic conjunctivitis is equally common in both men and women.
In general, an allergic reaction that occurs in the eyes, in the vast majority of cases, is always accompanied by the appearance of conjunctivitis, eyelid dermatitis and other diseases of the visual organs. Often the disease occurs together with bronchial asthma and rhinitis. If left untreated, chronic conjunctivitis can lead to serious vision problems.
Etiology
Among the causes of conjunctivitis, the first place is taken by infectious agents, which often enter the eye exogenously and relatively rarely endogenously. Usually these are staphylococci and pneumococci. In seasonal epidemic outbreaks, a pathogen specific to the eye, such as the Koch-Wicks bacterium, is mainly important (see Koch-Wicks bacterium). Acute epidemic. Koch-Wicks conjunctivitis often affects children's groups, especially younger children (up to 2 years). The frequency of K. caused by the Morax-Axenfeld diplobacillus (see Morax-Axenfeld bacterium), streptococcus, Escherichia coli, and diphtheria coli is low. Gonorrheal K. (blennorrhea of newborns and adults), often leading to blindness in pre-revolutionary Russia, is extremely rare in modern practice thanks to active prevention in obstetric institutions.
The proportion of K. of viral etiology has increased significantly. Among them, the most common are K. caused by adenoviruses of types 3, 7a, less often 6, 10, 11, 17, 21, 22 (adenoviral K., or adenopharyngoconjunctival fever - the old name) or type 8 (epid, keratoconjunctivitis). Adenovirus K. are observed at different times of the year in the form of numerous sporadic cases and epidemics, outbreaks among all age groups of the population. The group of picornaviruses (enterovirus-70) includes the causative agent of K., first registered in Ghana in 1969 and called epidemic hemorrhagic K. In 1971-1973. This disease has become a pandemic that has spread to countries in Europe, Asia, Africa and the Middle East. In the USSR, outbreaks of epidemics and hemorrhagic K. were also noted.
The increase in the frequency of allergic reactions is associated with a constant increase in factors that contribute to changes in the body's reactivity (widespread use of vaccines, serums, chemotherapy drugs, insecticides, household chemicals, cosmetics, etc.). Allergens can be antibiotics, quinine, morphine, dionine, eserine, atropine and other drugs.
A significant role, especially in the occurrence of hron. K., play various physical games. and chem. factors in the chemical, textile, flour-grinding industries, sawmills, brick, lime factories, as well as light energy and ionizing radiation in the electrical industry, film production, during the operation of X-ray machines, etc. Chron. K. also develops with various hron, diseases of the body - inflammatory diseases of the paranasal sinuses, nasal pharynx, gastrointestinal tract. tract, with helminthic invasion, etc. The etiology of acute follicular K. is mainly infectious, while the etiology of hron, follicular K. does not differ from the etiology of hron, non-follicular K. In some cases, follicles are formed as a consequence of age-related hyperplasia of lymphoid tissue in children - folliculosis. Predisposing factors for the development of follicles may be disturbances in the activity of the gastrointestinal tract. tract, helminthic infestations, anemia, hypo- and avitaminosis, chronic intoxication, unsatisfactory sanitary hygiene. conditions.
Pathogenesis and pathological anatomy
The unique anatomical structure of the conjunctiva determines the peculiarities of the morphological picture and pathogenesis of conjunctivitis. Not only the pathogen plays a major role in their occurrence, but also the reactivity of the body, which determines the nature of the course of conjunctivitis of various etiologies.
An accessible and well-studied method of morphol, research for K. is the study of the cytological picture of conjunctival scrapings (see Cytological examination). With bacterial K., the scraping cytogram is characterized by the presence of a large number of neutrophils and the absence of changes in the epithelial cells. With K. of viral etiology, dystrophic changes in epithelial cells and a predominance of lymphomonocytic and histiocytic cells in the exudate are revealed. Exudate in allergic K. also contains eosinophils and basophils.
With fungal conjunctivitis, fungi are visible in the foamy discharge, often phagocytosed by neutrophils and histiocytic cells. Gistol, a study of K. in the conjunctival tissue itself shows hyperemia, edema and exudation, covering the entire conjunctiva or only part of it. Exudate in acute K. consists mainly of polynuclear cells that form accumulations around the vessels and in the subepithelial layer of the conjunctiva. In later periods, infiltration is characterized by an admixture of lymphocytes, eosinophils and plasma cells. For allergic K. local eosinophilia is especially characteristic, and for hron. K. lymphocytic and plasmacytic infiltration. In addition to infiltration, proliferative changes in the connective tissue elements are noted in the inflamed conjunctival tissue. In some cases, the formation of focal accumulations of cellular elements in the form of follicles is observed in the lymphoid tissue; their presence and development determines the special forms of follicular cells. With viral cells, the greatest changes are found in the epithelial cells of the conjunctiva, since viruses such as adenovirus are epitheliotropic. Destruction of epithelial cells, vacuolization of the cytoplasm and nuclei, fragmentation of nuclear chromatin, and accumulation of acid phosphatase occur.
Methods for diagnosing chronic allergic conjunctivitis
Diagnosis of the allergic form of inflammation of the conjunctiva can only be carried out by an ophthalmologist and an allergist-immunologist. This is especially important if the history clearly shows a connection between inflammation of the conjunctiva and exposure to an allergen. To confirm the diagnosis, specialists carry out:
- Ophthalmological examination: during it, changes in the conjunctiva are revealed (in particular, the presence or absence of edema, hyperemia and other signs). Examination of conjunctival scrapings using a microscope reveals eosinophils and an increase in IgE in the blood, which indicates infection with allergic conjunctivitis.
- Allergological examination: to establish the causes of the onset and development of the disease, a number of tests are taken: elimination (excludes contact with a possible allergen) and exposure (it consists of repeated exposure to the suspected allergen after all symptoms have subsided). When the acute manifestation of symptoms subsides, skin allergy tests are performed. With a temporary retreat of the disease, provocative tests are performed: conjunctival, nasal and sublingual.
- Examination in the laboratory. If allergic conjunctivitis is chronic, the eyelashes are examined for traces of demodex mites.
Typically, the prognosis for treatment of chronic allergic conjunctivitis is favorable. If you do not pay attention to the disease, various infections may occur, which can lead to serious problems, including a decrease in visual acuity. To prevent this, you can use preventative measures. These include no contact with known allergens. If allergic conjunctivitis is seasonal, preventive courses of desensitizing therapy should be used. At the first signs of the development of the disease, you should contact an allergist and ophthalmologist.
Clinical picture
Despite the variety of etiological factors in the occurrence of conjunctivitis, the clinical picture is characterized by a number of common signs - hyperemia, swelling of the conjunctiva of the eyelids and transitional folds, and the presence of discharge.
Rice. 8. Acute catarrhal conjunctivitis: hyperemia of the conjunctiva of the eyelids and eyeball.
Sharp K.
begins suddenly, without prodromal phenomena, first in one eye, then in the other eye. There is pain or pain in the eye, copious discharge and hyperemia of the conjunctiva (color. Fig. 8). The conjunctiva turns from pale pink to bright red, and hemorrhages often appear. A conjunctival injection of the eyeball develops, most pronounced at the fornix and gradually decreasing towards the cornea. Swelling of the conjunctiva leads to its thickening and blurring of the pattern of the glands of the cartilage of the eyelids (meibomian glands). In severe cases, due to swelling, the conjunctiva of the eyeball takes on a peculiar appearance, rising in the form of a shaft around the cornea (conjunctival chemosis). The discharge may be mucous, mucopurulent or purulent. Acute K. is often accompanied by general malaise, fever and headache. The duration of acute K. ranges from 5-6 days to 2-3 weeks. In severe complicated forms of K., the course may be delayed.
In children, membranous form K often occurs. It is characterized by moderate swelling of the eyelids, pronounced hyperemia of the conjunctiva of the eyelids with the presence of small hemorrhages and a mucopurulent film, which is easily removed with a cotton swab or spontaneously when the child cries. The most severe form of membranous K. develops with diphtheria K., which is extremely rare. It is characterized by the presence of grayish films on the conjunctiva, which are difficult to remove and leave a bleeding surface after removal.
Unlike acute, chronic
K. begins imperceptibly and is characterized by a persistent and long course. Patients complain of discomfort in the eye, a feeling of blockage. The conjunctiva of the eyelids and transitional folds is slightly hyperemic, loosened, its surface has an uneven, velvety appearance due to the increase in the height of the papillae. Chron. K. can drag on for years or in the form of catarrhal K., which is safe for the eye, or be accompanied by various complications from the cornea or eyelids, which is typical, for example, for trachoma.
Conjunctivitis can occur with the formation of transitional folds of follicles on the conjunctiva - small, pinhead-sized, translucent pale pink formations. Most often, follicular K. occurs in children, which is explained by the tendency of the lymphoid tissue of the conjunctiva of children to grow. Unlike trachoma, follicular K. does not leave behind scars and does not damage the cornea. With folliculosis in children, simultaneously with the follicles on the conjunctiva, similar follicles are found on the tonsils, the mucous membrane of the back wall of the pharynx, which disappear with age, leaving no trace.
Complications are rare; they can occur due to the transition of the inflammatory process to the cornea (see Keratitis). With trachoma, cicatricial changes in the eyelids occur—inversion of the eyelid (see), entropion of the eyelid (see), trichiasis (see Eyelids).
The diagnosis is usually not difficult. However, to establish the etiology of K., a number of labs are used. methods, among which the most widespread are the following. 1. Bacterioscopy and bacterial. examination of smears and conjunctival discharge with subsequent determination of the pathogenicity of isolated microorganisms and their sensitivity to antibiotics. 2. Tsitol, study of conjunctival scrapings for the purpose of differential diagnosis of type K. 3. Immunofluorescence study of scrapings of the patient’s conjunctiva to detect viral antigens (see Immunofluorescence). Carrying out these studies is especially important when studying the etiology of outbreaks of K. in children's groups, to lay down. and other institutions. A technique has been developed that allows simultaneous examination of a patient for antigens of adenoviruses, influenza viruses, parainfluenza, trachoma, inclusion body viruses, and rhinoviruses. 4. Immunol and serol methods. For the diagnosis of bacterial and allergic K., serological studies are indicated (see) in order to identify antibodies to bacterial or drug allergens. When deciphering outbreaks of viral K., studies to determine the titer of antibodies to adenovirus, influenza, and parainfluenza in reactions of neutralization or inhibition of hemagglutination are important. 5. Intradermal and focal tests. The most commonly used intradermal Mantoux and Pirquet tests with tuberculin (from the 8th to the 3rd dilution), tests with staphylococcal, streptococcal allergen (2-4 skin doses in 0.1 ml), pollen and other allergens.
Diagnostics
When contacting a doctor, the patient needs to describe his condition in detail: tell whether he is allergic to anything, when the first symptoms appeared and what they were, as well as at what time they intensified.
Basic diagnostic methods at the first visit to the doctor:
- ophthalmological examination,
- taking a smear from the mucous membrane of the eye.
After this, a general blood test is prescribed, as well as an immunoglobulin E test. Special skin tests are performed to identify allergens.
Which doctor should I contact?
If you have signs of conjunctivitis, you should consult an ophthalmologist. The main task of the doctor is to determine the type of conjunctivitis, since it can be viral, bacterial, or allergic.
After the ophthalmologist has carried out his diagnosis, you may need to consult an allergist: it is this specialist who conducts allergy tests.
Treatment
Treatment is etiopathogenetic and symptomatic. For acute bacterial infections, antibiotics and sulfonamide drugs are prescribed in the form of drops (20-30% sulfacyl sodium solution, 0.25% chloramphenicol solution, 10% norsulfazole sodium solution). In case of copious discharge, the conjunctival cavity is washed with potassium permanganate solution (1: 5000) or 2% boric acid solution. Bandaging is not recommended. Due to the increased resistance of microorganisms to antibiotics and the development of allergic complications when using them, it is advisable to more widely use long-acting sulfonamide drugs and combined forms of antibiotics. For this purpose, use 10% sodium sulfapyridazine solution in 10% polyvinyl alcohol solution and 1% polymer-based ditetracycline ointment once a day. Combined dosage form - tetracycline with oleandomycin - 1% oletethrin ointment is injected into the conjunctival sac 2-3 times a day for severe K. and 1 time for milder forms. To reduce the side effects of antibiotics, they are prescribed in combination with corticosteroids. When treating chronic For K., especially with allergic layers, a complex polymer-based preparation is effective - sulfadex, which includes 10% sulfapyridazine sodium solution and 0.1% dexamethasone solution.
A method has been developed for the treatment of bacterial K. using a new type of ophthalmic medicinal films (see). They do not irritate the eye tissue and help prolong the effect of medications. The active principle is sulfapyridazine sodium and the antibiotic neomycin.
For viral K., the most effective are interferon preparations, which have pronounced antiviral activity and a wide spectrum of action, as well as tebrofen, florenal and pyrogenal. Human leukocyte interferon is used in the form of instillations 6-8 times a day in the acute stage of the disease, tebrofen and florenal - in the form of 0.25% ointment 3 times a day. Corticosteroids (0.5% hydrocortisone ointment, 0.3% prednisolone solution) are prescribed only during the recovery stage. For epidemics and keratoconjunctivitis, injections of 5% vitamin B1 solution, 1 ml intramuscularly once a day, are additionally recommended for a course of treatment of 15 injections, and in the stage of eruption of subepithelial infiltrates - 0.01% citral solution, 1-2 drops into the conjunctival sac. If the general reaction of the body is severe, antibiotics or sulfonamides are prescribed orally.
For allergic K., topical corticosteroids are indicated, and oral antihistamines - diphenhydramine, suprastin, calcium gluconate, 1 tablet 1-3 times a day.
Prognosis and Prevention
The prognosis for mild forms of K. is favorable. If the cornea is damaged, visual function may decrease.
Prevention includes carrying out sanitary hygiene. measures that include observing personal hygiene rules, mandatory hand washing before eye procedures, the use of individual pipettes, sticks, etc. A set of measures is necessary in children's and medical settings. and other institutions aimed at stopping the spread of infection: wet cleaning of the room with 2% chloramine solution, air disinfection with ultraviolet rays, long-term sterilization of pipettes, sticks, instruments, control over the disinfection of water in public reservoirs and swimming pools. The complex of preventive measures includes improving working conditions and observing safety precautions, especially in enterprises using various harmful chemicals. substances. For epidemics and Koch-Wicks conjunctivitis in the autumn-summer period, chemoprophylaxis is carried out - the use of 1% ditetracycline ointment or ophthalmic medicinal films with sulfapyridazine once a day for 6 days. Chemoprophylaxis of neonatal blenorrhea is carried out in all obstetric institutions according to the Matveev-Crede method (see Blennorrhea). For adenoviral hemorrhagic K., it is recommended to apply 0.1% tebrofen ointment or instillation of interferon 1 - 2 times a day to all persons in contact with a patient with this form of K.
Certain forms of conjunctivitis
Individual forms of conjunctivitis are characterized by different features (Table).
Acute bacterial conjunctivitis.
The most common pathogens are pneumococcus and staphylococcus; less commonly, the disease is caused by streptococcus and Escherichia coli. K. develops acutely, the incubation period lasts 1-2 days. The most characteristic signs are severe photophobia and lacrimation. The conjunctiva of the eyelids and eyeball is infiltrated, hyperemic, and pinpoint hemorrhages appear in it. Grayish films often form on the conjunctiva of the eyelids, especially in children, which can be easily removed with a damp cotton swab. The cornea may be involved in the process. In its superficial layers at the border with the limbus, small infiltrates appear, which then erode, but do not leave behind persistent opacities. Microbes in the acute stage are found in the discharge and in the epithelial cells. In children's institutions, K. can be epidemic in nature.
Acute epidemic Koch-Wicks conjunctivitis
is a fairly common disease in hot countries. More often it occurs in the form of epidemics, outbreaks in children's groups in the summer-autumn period. It is highly contagious. The incubation period is short - from several hours to 1 - 2 days. Both eyes are affected: first one and then the other. A typical manifestation of K. is pronounced hyperemia and swelling of the conjunctiva with copious mucopurulent discharge. K. is often accompanied by general malaise, fever and headache, lasting on average 2-3 weeks. In severe cases, complications from the cornea are possible.
Morax-Axenfeld conjunctivitis
has a characteristic wedge, a picture in the form of the so-called. angular blepharoconjunctivitis involving the edges of the eyelids, especially in the corners of the palpebral fissure. In this case, there is moderate hyperemia of the conjunctiva, a slight mucous discharge and redness of the skin of the eyelids at the external and internal commissures. K. may have a subacute or more often chronic course.
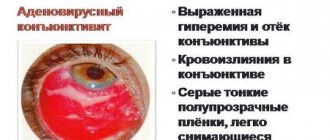
Adenoviral conjunctivitis.
The incubation period is 4-8 days. The onset of the disease is acute. It is preceded or accompanied by damage to the upper respiratory tract - rhinitis, pharyngitis, nasopharyngitis. Clinically, lacrimation, sometimes photophobia, hyperemia of the conjunctiva of the eyelids, lacrimal caruncle and transitional folds are noted. The conjunctiva is swollen, sometimes hemorrhages and film deposits occur, especially in children. The discharge is usually scanty and non-purulent. Rashes of small follicles are often found, which are located on the lower transitional fold. K. may be accompanied by general manifestations of the disease in the form of fever, headache and enlargement of the parotid lymph nodes. K. most often occurs in one eye, and after 1-3 days the second eye also becomes ill, and in a milder form.
Adenoviral epidemic keratoconjunctivitis.
Characteristically, in addition to K., frequent damage to the cornea in the form of small subepithelial infiltrates on the periphery of the cornea. Large coin- or disc-shaped infiltrates are less commonly observed. Fresh infiltrates usually appear within the first two days and then regress, leaving a long-term clouding of the cornea.
Epidemic hemorrhagic conjunctivitis.
A distinctive feature of this form of viral K. is the presence of hemorrhages of various sizes on the conjunctiva of the eyelids and eyeball - from small, pinpoint hemorrhages to extensive ones, occupying the entire surface of the conjunctiva.
Hemorrhages resolve in different periods depending on their size - pinpoint hemorrhages usually take 3-6 days, extensive hemorrhages take 2-3 weeks. Rice.
9. Phlyctenular conjunctivitis: at the limbus there are nodules (phlycten) of a round shape, with dilated vessels (indicated by arrows). Allergic (or toxic-allergic) conjunctivitis.
Its wedge, the picture is quite diverse depending on the nature of the allergic factor. Infectious-allergic K. includes phlyctenular keratoconjunctivitis, most often observed in children under 3 years of age (color. Fig. 9). Etiol, the factor is Ch. arr. sensitization to Mycobacterium tuberculosis. Toxins or decay products of mycobacteria from the focus of primary tuberculosis spread and become fixed on the conjunctiva, where antigenic contact with sensitized lymphocytes occurs. Along with hyperemia and infiltration of the mucous membrane, the appearance of one or several yellowish-grayish, rounded nodules surrounded by dilated vessels at the limbus is characteristic. Often keratoconjunctivitis in children is accompanied by eczematous skin changes at the wings of the nose and in the corners of the mouth. The cornea is often involved in the process, and superficial keratitis develops.
The most characteristic representative of atopic conjunctivitis
is K. for hay fever (see Hay fever). It differs in seasonality, exacerbations occur in spring and summer during the flowering period of grasses and trees. Both eyes become ill at the same time, and the patient complains of a burning sensation, lacrimation and photophobia. There is sharp pain, itching, hyperemia of the conjunctiva with swelling and copious serous discharge. K. is often accompanied by rhinitis.
Drug-induced conjunctivitis
occurs quite often. K. develops within 6 hours. after using the medicine and is characterized by rapidly increasing chemosis of the conjunctiva, severe itching, burning and copious mucous discharge. In some cases, after prolonged local use of a drug (allergen), papillary hypertrophy of the conjunctiva may occur, resembling spring catarrh. Follicular medicinal K. develops slowly, on average after 4 months, and gradually regresses after discontinuation of the drug, without leaving scars.
Allergic conjunctivitis usually manifests itself 6-24 hours after taking a sensitizing product - strawberries, citrus fruits, eggs, nuts, etc. Characteristics are a family predisposition, the presence of allergic dermatitis in childhood (see), concomitant skin lesions. Allergic Quincke's edema often occurs (see Quincke's edema). Allergic conjunctivitis also includes spring catarrh (see).
Development of allergic conjunctivitis
The main factor that provokes the onset of this type of conjunctivitis is the contact of the allergen with the mucous membrane of the eye. This leads to degranulation of mast cells and other processes, the result of which is an inflammatory-allergic reaction.
The severity of an allergic disease depends on the amount of allergen and the degree of vulnerability of the body. The speed at which the reaction develops varies: it can appear either almost immediately after contact with the allergen (within about half an hour) or after a fairly long period of time (about two days). This classification is of great importance for selecting a treatment regimen.
The classification of allergic conjunctivitis is as follows. This disease in an allergic form can manifest itself as hay fever, vernal or atopic keratoconjunctivitis, medicinal or chronic conjunctivitis. According to the nature of the course, the allergic form of the disease can be acute, subacute or chronic. There is also a division according to the time of occurrence - seasonal or year-round.