Diabetes mellitus is one of the diseases that is life-threatening with the rapid development of complications. The disease has a huge list of possible consequences affecting various organs and systems of the body.
After confirming the diagnosis, the patient is obliged to develop new eating and behavioral habits and direct all efforts to preventing complications.
- Complications of type 1 diabetes
- Complications of type 2 diabetes
- Late complications of diabetes
- Prevention of complications of diabetes mellitus
How does carbohydrate metabolism occur?
The process of carbohydrate absorption includes several stages:
- food containing polysaccharides of any composition is digested in the intestines. In this case, carbohydrate compounds are broken down into their simplest components - fructose and glucose molecules. They enter the blood and are delivered to all cells. At this moment, the concentration of glucose in the blood is at its highest;
- Some cells in the brain, for example, are able to metabolize glucose on their own. However, the cells of most tissues - liver, muscle, fat - cannot do this. The permeability of the cell membrane is too low to allow a fairly large sugar molecule to pass through. Insulin solves this problem;
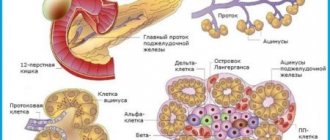
- the hormone is produced by beta cells of the pancreas - they thus respond to an increase in blood sugar. Insulin acts on receptors sensitive to it, the latter increase the permeability of the cell membrane, and glucose can penetrate inside;
- when the cell's need for such an energy source is satisfied, the receptors lose their sensitivity. As cells become saturated, blood glucose levels decrease;
- if some excess glucose remains, it is processed and stored as glycogen in the liver and muscles. If the glycogen depot in the liver is full, excess sugar is converted into fat by another enzyme and stored in adipocytes.
Violation at any stage of the chain leads to non-absorption of glucose, the appearance of hyperglycemia and the development of associated complications. However, only certain disorders of this mechanism are called diabetes.
2.What is insulin and why is it needed?
Typically, the hormone insulin is produced in small quantities in the pancreas. When you eat, the sugar (glucose) in the food stimulates the pancreas to produce insulin. Its amount is proportional to the amount of food taken. Insulin's main role is to help move certain nutrients, especially sugar, into the body's tissues and cells. Cells use sugar and other nutrients as an energy source to function.
The amount of sugar in the blood decreases when it enters the cells. This usually signals the beta cells to reduce the amount of insulin they secrete to avoid hypoglycemia (low blood sugar), and the amount of insulin they secrete also decreases. But the destruction of beta cells disrupts the functioning of the entire system.
Visit our Endocrinology page
Diabetes mellitus type 1
This disease accounts for about 5–10% of all cases of diabetes mellitus syndrome. It is associated with insufficient insulin secretion. The latter occurs for various reasons, but most are associated with genetic abnormalities.
Type 1 diabetes: what is it in simple terms.
Insulin is produced by the islets of Langerhans, special cells of the pancreas. This is the only source of the hormone. If the cells die for one reason or another, the pancreas does not produce insulin and type 1 diabetes develops. It is worth noting that the disorder manifests itself only after the death of at least half of the cells. Until this moment, the organ copes with the load.
In the absence of insulin, the cells of all insulin-dependent tissues do not allow glucose to enter. Accordingly, sugar accumulates in the blood very quickly. The conversion of sugar into glycogen and its deposition in the liver allows very little glucose to be utilized. Transformation into fat is impossible, since in the absence of insulin the enzyme that provides this binding method is not activated.
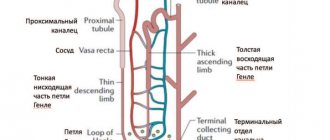
With hyperglycemia of 10 mmol/l, glucose enters the urine. The kidneys cannot reabsorb sugar and excrete it in the urine. This does not help in any way to cope with hyperglycemia; on the contrary, it contributes to the development of complications.
Cells starve without receiving glucose. The body tries to satisfy its energy needs by breaking down fats and proteins. This allows for the vital activity of cells, but this is completely insufficient for the growth of new cells, renewal, and tissue regeneration. This is why type 1 diabetes is so dangerous in childhood. During a period when the body is very actively developing, starvation leads to growth cessation and death.
If type 1 diabetes is left untreated, it progresses very quickly and leads to serious complications.
Causes
Unfortunately, today there is still no known reliable reason why type 1 diabetes mellitus occurs. There are only a number of hypotheses in this regard:
- stress factor - frequent stressful situations can lead to diabetes mellitus of the first degree;
- hereditary factor is one of the most reliable hypotheses existing today, however, the percentage of possible transmission of diabetes from parents to children is not so high and is about 5-10%;
- the possible development of diabetes mellitus is facilitated by past infectious or viral diseases;
- autoimmune process - for reasons unknown to science, a sudden malfunction occurs in the human body and beta cells are destroyed, which inevitably leads to diabetes.
How does type 1 diabetes develop?
The disease does not appear immediately and does not form instantly. Unfortunately, its signs also do not appear immediately, which makes diagnosis difficult in the early stages.
The development of the disease occurs in several stages.
- Type 1 diabetes mellitus is largely due to hereditary predisposition. The tendency to develop autoimmune disorders leading to the destruction of the islets of Langerhans is due to both recessive and dominant genes. Accordingly, the tendency to diabetes increases if there are already cases of the disease in the family. But, the disease may appear unexpectedly if it was transmitted with recessive genes.
- The trigger point is illness, injury, an unhealthy diet, too rich in carbohydrates and poor in proteins, causing autoimmune aggression. When any cytotoxic agents appear, autoantigens are produced. The latter ultimately lead to excessive synthesis of interleukin, which damages the beta cells of the pancreas. The latter become a target for macrophages. This moment acts as a trigger for the development of diabetes. At this moment, the pancreas produces a sufficient amount of insulin. Such a sign as high blood sugar has not yet appeared.
- Chronic autoimmune insulin - antibody titer increases, beta cells die. The speed of the process determines the timing of the disease manifestation.
As beta cells become damaged, insulin production decreases. On an empty stomach, hyperglycemia is not yet determined, but after a glucose load it becomes obvious that sugar is utilized too slowly. When 50% of the cells die, the first signs of type 1 diabetes appear.
- Clinical manifestation occurs when 80–90% of beta cells are dysfunctional. Insulin secretion decreases sharply. Hyperglycemia increases very quickly, and with it the main symptoms of the “sweet” disease appear.
- Absolute insulin deficiency occurs when all pancreatic cells die. Glucose is not absorbed, fats and proteins are actively broken down, so the patient suddenly loses weight.
Treatment for type 1 diabetes primarily involves insulin injections. Without artificial administration of the hormone, the patient risks dying.
Phases of the disease
Type 1 diabetes, like other chronic disorders, is characterized by remission and exacerbations. With the latter, the patient’s condition deteriorates greatly and the risk of death increases significantly, as it becomes impossible to control blood sugar.
- Phase compensation - remission. In this case, the glucose level does not exceed 8 mmol/l and changes little during the day. There are traces of glucose in the urine and nothing more. Complications that are possible with the disease manifest themselves weakly and do not develop. Blood sugar levels are maintained by normal doses of insulin and diet; additional injections are not needed.
- Subcompensation phase - glucose level increases to 14 mmol/l, no more than 50 g per day is excreted in the urine. However, ketosis is not observed, that is, the administered insulin is sufficient for the absorption of glucose. To correct the condition, additional doses of the hormone are required.
- The decompensation phase is an exacerbation of stage 1 diabetes mellitus. The sugar content can increase above 14 mmol/l and reach 30 mmol/l. There is more than 50 g of glucose in the urine. Acetone is detected in the urine and in the patient’s breath - ketosis occurs. The worst thing is that in this state, the sugar level changes greatly during the day, and it is not possible to correct it with insulin. In the decompensation phase, the risk of hyperglycemic coma increases sharply.
Diabetes mellitus type 1: causes
The mechanism of development of the disease is the same - only the triggering moments are different. Based on the nature of the “trigger”, the causes of the “sweet” disease are divided into categories: autoimmune and idiopathic.
Autoimmune causes are associated with the presence of a hereditary tendency to autoimmune aggression. It is caused by gene defects on chromosome 6. The tendency itself does not necessarily determine the formation of diabetes. Thus, identical twins raised in the same family suffer from type 1 diabetes in only 30–40% of cases. To provoke an endocrine disorder, an additional mechanism is required:
- childhood infectious diseases - measles, rubella, hepatitis often lead to damage to the pancreas. In normal cases, the cells of an organ gradually restore their functionality, but with a tendency to autoimmune aggression, the risk of self-destruction increases significantly. And if this happens, type 1 diabetes develops;
- some drugs - streptosacin, for example, damage the beta cells of the pancreas;
- Trauma to the pancreas also leads to the same result . By older age - 15-20 years, the cause of the disease can be acute or chronic pancreatitis. If you are prone to autoimmune diseases, it is not possible to completely cure inflammation, since the immune system in some way acts together with the disease;
- In an adult, type 1 diabetes mellitus may appear due to chemical poisoning . The disease develops without genetic prerequisites.
In the idiopathic form of the “sweet” disease, autoantibodies are not detected in the blood, so we can say that it is not associated with congenital anomalies. The reasons for its occurrence are unknown. However, it has been established that idiopathic diabetes is more common among representatives of the Mongoloid and Negroid races. In idiopathic diabetes, pancreatic functionality can be restored.
Prevention
- Avoid infectious and viral diseases. Get all preventive vaccinations in a timely manner.
- Try not to move to a new place of residence with a sudden change in climate.
- Take powerful medications with caution, especially antibiotics.
- For any problems with the pancreas, undergo examination and treatment.
- Strengthen your immune system using all known methods.
- Eat properly.
- Monitor your weight and prevent obesity.
- Avoid stress.
- Be active and try to maintain a healthy lifestyle.
Type 1 diabetes is not a death sentence. This diagnosis does not mean that from now on you will have to isolate yourself from society, constantly take injections and give up the joys of life. A favorable forecast for the future is in your hands. If you follow all clinical recommendations, you can avoid complications and enjoy every day of your existence.
Type 1 diabetes: symptoms and treatment
Determining type 1 diabetes in an adult or child is relatively easy. Symptoms of the disease develop very quickly and appear acutely, especially in childhood. Manifestation is possible even in the first half of a baby’s life. In most cases, the disease manifests itself before the age of 5 years.
The second dangerous period is puberty. Hormonal changes can cause autoimmune activity, which also provokes the formation of type 1 diabetes. In the future, pancreatitis and alcohol abuse are most often the provoking factors.
Clinical symptoms of type 1 diabetes are divided into primary and secondary.
Basic signs
The main clinical symptoms of type 1 diabetes occur when hyperglycemia has reached a certain level, glucose is excreted in the urine, and fats and proteins are actively broken down to replenish energy.
- Polyuria - glucose dissolved in urine increases the osmotic pressure of the fluid. As a result, the patient experiences frequent urges. And since more water is required to remove sugar, the daily volume of urine increases noticeably.
- Polydipsia is a constant thirst caused by both loss of water in the urine and increased sugar. The latter increases the osmotic pressure of the blood, and to compensate for this, you need to drink more or greatly increase your blood pressure.
- Polyphagia is another characteristic sign of diabetes. Fasting at the cellular level ensures a constant feeling of hunger, since in fact the lack of glucose only increases over time. In addition, in the absence of insulin, the corresponding part of the hypothalamus does not receive a signal of saturation. As a result, a diabetic feels hungry literally 1 hour after eating, or even does not feel full at all.
- Weight loss is a characteristic symptom of type 1 diabetes. Increased catabolism leads to rapid weight loss and exhaustion. In childhood, this symptom is especially dangerous.
Secondary clinical symptoms
There are some other signs that may indicate stage 1 diabetes. They develop more slowly and are less specific.
- Hyperglycemia causes malnutrition of the skin . It causes blood thickening, and at the same time capillary circulation is disrupted. The skin loses elasticity, becomes dry, changes color, but more importantly, its ability to regenerate decreases. Wounds and scratches on the skin take a very long time to heal and are prone to infection.
In addition, increased sugar irritates skin receptors. As a result, diabetics often suffer from severe, unquenchable itching. Soothing ointments do not work, since irritation occurs from the inside.
- Type 1 diabetes mellitus leads to a noticeable decrease in immunity . Lymphocytes use vitamin C when working. Its structure is similar to glucose. When the concentration of the latter is excessively high, lymphocytes use sugar instead of vitamin. As a result, the ability to resist infectious and inflammatory diseases decreases significantly.
Both general and local immunity decreases. This is partly responsible for poor wound healing and susceptibility to fungal diseases.
- The breakdown of fats is accompanied by the formation of ketone bodies - they are used as a source of energy. But ketone bodies are consumed quite slowly and at some point they begin to accumulate. The appearance of an acetone odor in urine and breath indicates ketosis. Ketosis is also the hardest on the kidneys, and kidney failure is the second leading cause of death for diabetics.
- Visual impairment in an adult is associated with both increased sugar and the formation and accumulation of sorbitol. Developing retinopathy can lead to complete blindness.
Only a laboratory examination can confirm or refute the suspicion of diabetes mellitus. If the tests reveal elevated blood sugar and liver failure is excluded, the diagnosis is confirmed.
Late complications of diabetes and health status
In both types of diabetes, late complications of diabetes cause significant health problems, being the most common cause of death from this pathology.
In type 1 diabetes, complications associated with damage to small vessels are more often detected, while in type 2 diabetes, complications associated with damage to large vessels are most common.
Diabetic macroangiopathy
Large vessels are most often affected by diabetes; this condition is called diabetic macroangiopathy. This is due to long-term hyperglycemia, which inevitably leads to atherosclerotic vascular damage - cholesterol plaques are deposited on the walls of blood vessels, the walls of blood vessels thicken and become rigid. The lumens of blood vessels narrow, which leads to hypoxia (oxygen starvation) of organs and tissues, strokes and heart attacks.
Clinically, macroangiopathy in diabetes is manifested by coronary heart disease, atherosclerosis of the vessels of the brain and limbs, and arterial hypertension. Moreover, the course of these diseases does not differ from those in people with normal blood glucose levels.
Only the incidence of cardiovascular pathology in people with diabetes is incredibly high. Thus, the risk of developing coronary heart disease in people with type 2 diabetes is 6 times higher than in people who do not have hyperglycemia.
High blood pressure is observed in 20% of patients with type 1 diabetes and 75% of patients with type 2 diabetes.
Heart attacks and strokes are the most common cause of death in type 2 diabetes. A feature of the course of a heart attack in diabetes mellitus is its painless form. This occurs in approximately 30% of cases and is likely due to concomitant nerve damage in diabetes.
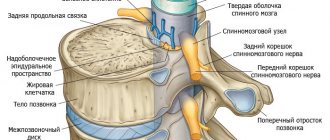
Diabetic neuropathy
The nervous system is affected in 30% of cases with type 1 and type 2 diabetes. The cause of damage to the nerves is hyperglycemia: microangiopathy in the vessels feeding the nerve trunks leads to disruption of their normal nutrition. High levels of glucose in the blood lead to the accumulation of free radicals, which have a damaging effect on nerve tissue.
Diabetic neuropathy has two forms:
- Sensory form.
Characterized by impaired sensitivity and motor function. Patients complain of unusual feelings appearing in the extremities: “crawling goosebumps”, “cotton legs”, loss of sensitivity like “gloves” and “stockings”, “alien legs”. There may be pain in the limbs that goes away after walking. More often, pain occurs at night, and even the touch of bed linen can cause it. Over time, the pain syndrome may disappear, which is associated with the death of small nerves.
- Vegetative form.
From the cardiovascular system: tachycardia at rest, fainting, heart attack without pain. From the gastrointestinal tract: impaired contractile function of the stomach with slow or too rapid evacuation of contents, reflux of gastric contents into the esophagus, diarrhea. From the genitourinary system: impaired bladder tone, which leads to frequent inflammatory diseases, erectile dysfunction in men.
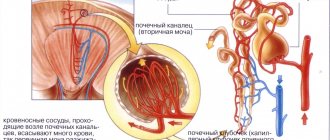
Diabetic nephropathy
It is characterized by an increase in pressure inside the vessels of the renal glomeruli and loss of protein in the urine due to impaired filtration function. And arterial hypertension, which is present in diabetes, aggravates the situation.
As diabetes mellitus progresses, the renal glomeruli die and the renal tissue is replaced by connective tissue (glomerulosclerosis). The outcome of diabetic nephropathy is chronic renal failure. This complication is more common in type 2 diabetes and is the cause of death in 15% of cases in this group of patients.
Treatment for type 1 diabetes
The disease is incurable, so we are talking about symptomatic treatment. With a stage 1 disease, a person cannot survive without treatment: the complete absence of insulin leads to the complete destruction of not only carbohydrate, but also fat and protein metabolism. Until insulin was obtained and used, the life of a diabetic was measured in months.
Treatment consists of a series of activities. All of them are mandatory.
- Compensation for carbohydrate metabolism consists of two parts. First of all, insulin is administered strictly according to the calculated scheme and in the precisely indicated dosage. The calculation is made taking into account the products consumed, for which a special system has been developed, and physical activity. Skipping even one injection is fatal.
- Diet for type 1 diabetes is the same element of treatment as insulin therapy. Without compliance with it, it is impossible to compensate for the disorder of carbohydrate metabolism. The daily diet should be organized so that the diabetic receives the same dose of carbohydrates with each meal. This ensures stable blood sugar levels.
- Prevention of complications and their treatment – diabetes causes many complications. Therefore, the patient has to constantly monitor his well-being and undergo examination. If a child is sick, this responsibility is performed by the parents.
- Normalization of weight – with type 1 diabetes, the vast majority of patients lose a lot of weight. It is necessary to maintain at least a minimum body weight.
- Patient education - the patient must monitor sugar levels independently, since this must be done several times a day and with any change in well-being. Adults and adolescents, as well as parents of younger children, are taught how to use a glucometer and evaluate for signs of hyperglycemia or hypoglycemia.
In critical cases, type 1 diabetes is treated with surgery. Pancreas transplantation or islet transplantation of Langerhans can permanently cure the disease.
Type 1 diabetes mellitus is a very serious incurable endocrine disease. The patient requires lifelong insulin therapy. Only strict adherence to diet and insulin regimen ensures a sufficiently long life span.
See also:
Treatment of type 1 diabetes: insulin therapy, diet and prevention of complications
Diet for type 1 diabetes: allowed foods, principles of organization and significance
Diabetes mellitus type 1: conditions for assigning disability group 1, 2 and 3
Type 2 diabetes: causes of the disease, mechanism of formation and main symptoms