What is dysbiosis
Dysbiosis is an imbalance of bacteria living in the intestines under the influence of various factors (taking antibiotics, poor nutrition). Recently, pathology is often observed in very young children.
The intestines are the habitat of beneficial and neutral bacteria
Features of the disease in newborns and infants
The risk group includes the following categories of children:
- premature;
- those who are bottle-fed;
- children whose mothers received antibiotics during pregnancy or breastfeeding;
- late applied to the breast.
Breastfeeding is a reliable prevention of dysbiosis
In babies who receive breast milk, dysbiosis develops much less frequently. Their intestinal microflora consists of 90% lactobacilli and bifidobacteria.
Signs of impaired intestinal microflora in newborns and infants are as follows:
- bloated stomach;
- bad breath;
- stomach ache;
- formation of gases in the intestines;
- secretion of a large amount of saliva;
- dry and tight skin;
- the appearance of allergic rashes on the skin;
- inflammation of the oral mucosa;
- signs of thrush in the mouth;
- difficult stool;
- diarrhea for three or more days;
- vomiting after eating;
- problems gaining weight;
- greenish foamy stool, possibly blood.
According to the World Health Organization, imbalance of intestinal microflora is not a disease. Some foreign experts suggest not interfering with this condition and allowing the body to independently regulate this process. However, most doctors are of the opinion that therapy is still necessary.
To fully evaluate bowel function in a newborn or breastfed infant, the following tests must be performed:
- coprogram (reveals the digestive activity of the intestine, inflammatory processes);
- sowing stool for opportunistic flora (shows how many neutral bacteria are in the intestines);
- tank. stool culture for dysbacteriosis (reveals the percentage of normal and opportunistic intestinal microflora).
According to some experts, it is incorrect to talk about dysbiosis in newborn babies. Children are born with a sterile intestine, which is gradually colonized by bacteria, so it is difficult to judge their normal ratio and quantity.
Causes of imbalance of intestinal microflora in adults and children
Dysbacteriosis can develop in children of preschool and school age, as well as in adults. Most often, the following reasons lead to this condition:
- taking antibiotics;
- eating disorder;
- the presence of a large amount of sweets in food, lack of coarse plant fiber;
- changing your usual food and water when moving to another area;
- infectious intestinal diseases (shigellosis, salmonellosis);
- general decrease in immune system activity;
- operations on the stomach and intestines;
- inflammatory diseases of the stomach and intestines (gastroenterocolitis).
Dysbacteriosis in men and women usually has the same causes. However, the following factors can also contribute to the development of pathology in the fairer sex:
- women's passion for strict diets;
- frequent bowel cleansing using enemas;
- addiction to laxatives for the purpose of losing weight;
- more active treatment with antibiotics.
What signs may indicate the presence of pathology?
Symptoms of dysbiosis in adults and children of preschool and school age:
- bloating and abdominal pain;
- decreased appetite;
- nausea and vomiting;
- undigested pieces of food in stool;
- the appearance of a white coating on the tongue;
- bad breath;
- decreased vitality, fatigue;
- periodic acute abdominal pain;
- dry and brittle hair;
- the appearance of bleeding gums and dark plaque on the teeth.
Microbiological examination of stool will show the ratio of microorganisms in the intestine
To confirm objective signs of dysbiosis, it is necessary to do a microbiological examination of stool. This analysis will show the concentration and ratio of beneficial microorganisms (bifidobacteria, lactobacilli, bacteroides) and opportunistic ones, as well as the presence of pathogenic bacteria (shigella, salmonella).
Doctor Komarovsky about dysbiosis - video
Is special training needed?
If the test is prescribed for an infant who has started feeding, then three days before the test the introduction of new products is excluded. Also, for several days before donating stool, you should stop giving your baby any medications, including activated charcoal and anti-colic medications.
It is very important not only to correctly collect stool for analysis for dysbacteriosis, but also to deliver the sample on time, and also to observe all the details of preparation.
Let's start in order:
- If you have been treated with antibiotics, keep in mind that it makes sense to take a stool test to determine imbalances in the intestinal microflora no earlier than two weeks after the end of therapy;
- Three days before the examination, it is necessary to stop using laxatives, antidiarrheals and anthelmintics, NSAIDs, pro- and prebiotics, castor and petroleum jelly, barium and bismuth preparations;
- You need to purchase in advance at the pharmacy or get from the laboratory a sterile plastic container with a spoon and a tight-fitting lid, specially designed for collecting and transporting stool for analysis;
- Defecation should occur naturally, without the use of an enema or any other aid;
- You cannot collect a sample for analysis from a toilet bowl. For these purposes, you need to prepare any convenient container, which should be thoroughly washed, doused with boiling water, dried, and defecated into;
- Before starting the process, you must urinate, then wash and dry yourself. Under no circumstances should urine or secretions from the genital tract enter the sample collected. If a woman is menstruating, she should use a tampon;
- When defecation has taken place, you need to open the prepared container, take a spoon and collect a little material from different parts of the stool: from the middle, from the surface. If you see a suspicious area containing mucus or blood that differs in consistency or color from the surrounding feces, be sure to place it in a container! In total, 6-8 spoons of stool will be needed for analysis;
- Close the container tightly and deliver the sample to the laboratory no later than 2 hours after collection.
Most of the bacteria that make up the intestinal microflora are anaerobic, therefore, when exposed to open air, they gradually die. This is why it is so important to take a stool test for dysbacteriosis on time - only then will the interpretation of the results be reliable.
If you are undergoing a biochemical test, the urgency is less urgent - you can even freeze the sample and bring it to the laboratory the next day. This is especially convenient for parents of infants and small children, because it is unknown whether they will be able to collect feces from the child for analysis early in the morning - perhaps he simply does not want to go to the toilet.
There are various factors that can cause unfavorable changes in the composition of the intestinal microflora:
- taking certain medications;
- infectious diseases of various origins;
- poor nutrition;
- the presence of diseases of the digestive system;
- congenital defects or postoperative disorders;
- prolonged psycho-emotional stress;
- allergic diseases;
- immunodeficiency;
- excessive physical activity;
- environmental factors;
- a sharp change in climatic and geographical conditions.
The state of microflora imbalance does not have characteristic symptoms. Its manifestations are similar to the clinical picture of many gastrointestinal diseases. A change in the qualitative and/or quantitative composition of the microflora can be suspected if the following symptoms are present:
- bowel dysfunction (both constipation and loose stools);
- flatulence;
- intolerance to certain foods;
- allergy;
- decreased appetite;
- severe weakness;
- skin rash;
- stomach ache;
- nausea.
There are many methods aimed at detecting dysbiosis - coprogram, bacteriological examination of stool, PCR diagnostics, gas chromatography-mass spectrometry and biochemical study of microbial metabolites. Tests for dysbacteriosis are prescribed by a doctor in accordance with the patient’s health condition.
With a coprogram, the study of the stool of a patient with suspected dysbiosis occurs according to the following scheme: the result of the analysis for dysbiosis is studied, the color of the stool, consistency, and the presence or absence of any unnatural impurities in the stool, such as blood, mucus or undigested food particles, are taken into account.
We suggest you read: Caring for a newborn in the first month of life
The gas chromatography-mass spectrometry method is performed using a spectrograph. Such a study makes it possible to determine the ratio of the mass of biological material to the charge of ions. The results obtained can be saved in the information base.
PCR diagnostics (polymerase chain reaction) is a highly informative method that helps identify the presence of hereditary pathologies, acute or chronic infections in the intestines. The causative agent of dysbacteriosis is determined by its DNA material.
Biochemical analysis is a method for studying metabolites (volatile fatty acids) released by microbes during their life processes. The analysis is simple and allows you to get results within a few hours, to diagnose not only dysbiosis, but also gastrointestinal diseases.
The most common is bacteriological testing, which involves testing stool in the laboratory for dysbacteriosis. Determine what types of microbes inhabit the intestines and their number.
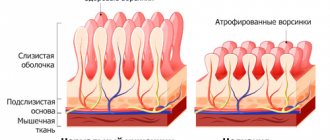
When examining stool for dysbacteriosis, it is necessary to take into account the presence of cavity and mucosal microflora in the intestine. Cavitary flora are microorganisms that are free in the intestinal lumen. Mucosal flora are bacteria that are fixed on the surface of the mucous membrane. In the stool, only cavity flora is available for analysis for dysbacteriosis.
This fact means that the result of the analysis will give only a partial picture of what biocenosis is present in the intestines. The majority of microorganisms on the surface of the mucosa will not be taken into account.
For 3 days, avoid eating foods containing substances that will affect the accuracy of the result:
- fish;
- meat;
- beet;
- alcohol.
For two weeks, avoid the use of medications that may affect the intestinal microflora:
- laxatives;
- antibiotics;
- antidiarrheal drugs;
- anthelmintics;
- rectal suppositories with probiotics;
- barium and bismuth preparations;
- NSAIDs (non-steroidal anti-inflammatory drugs);
- Castor oil;
- Vaseline oil;
- enema.
Stool analysis for dysbiosis: feasibility and reliability of such diagnosis
According to foreign and Russian pediatricians, there is no point in taking a stool test for dysbiosis in children who are breastfed, since mother's milk protects the child from this problem. If the baby is receiving artificial feeding or has already switched to regular food, and he has signs of dysbiosis, a visit to the pediatrician is first necessary.
After the examination, the following tests will be prescribed:
- general clinical analysis of urine and blood;
- coprogram (analysis of intestinal digestive activity);
- stool analysis for the presence of helminthic infestation and enterobiasis (pinworms);
- Ultrasound of the intestines.
And only as a last resort, if other diseases have not been detected, a stool test will be required to study the intestinal microflora, the results of which will be ready in 4-7 days.
To date, the question of the reliability of such a study remains open. In order for the results to be as accurate as possible, you need to collect the material correctly.
When is it not necessary to treat Klebsiella in the stool of an adult?
Klebsiella in stool. Changes in the normal composition of intestinal microflora can cause significant digestive disturbances and often require treatment. At the same time, the intestinal flora has great regenerative potential and in some situations is able to independently restore itself to a normal state without any treatment.
Thus, if deviations are detected in the bacteriological composition of the feces of an adult or child, treatment is not always necessary. The main argument in favor of refusing treatment for dysbiosis is the absence of any symptoms of dysbiosis.
Treatment of dysbiosis does not need to be carried out in the following situations:
- an increase in the amount of Escherichia coli with normal enzymatic activity of more than 3-4 x 106 /g;
- reduction in the amount of E. coli to 10 6/g in children under one year of age and to 2 x 106 million/g in older children and adults;
- an increase in the number of enterococci by more than 25%;
- the presence of epidermal or saprophytic staphylococcus, streptococci up to 25%;
- the presence of hemolyzing Escherichia coli, Proteus, Klebsiella, lactose-negative enterobacteria, Staphylococcus aureus in an amount of no more than 10% (103);
- the presence of Candida mushrooms in the amount of 104;
- any increase in the number of bifidobacteria and lactobacilli or a decrease in the number of bifidobacteria and lactobacilli to 106.
When not to get tested
It is not recommended to be tested for dysbacteriosis when taking the following medications:
- antibiotics;
- anti-inflammatory non-steroidal drugs;
- other groups of antibacterial drugs;
- vitamins;
- drugs that reduce gas formation in the intestines (Plantex, Espumisan);
- enterosorbents (Smecta, Enterosgel);
- laxatives.
The study should not be performed if the patient is receiving rectal suppositories or enemas.
Bacterial composition of intestinal microflora
For convenience, doctors classify all microorganisms that inhabit the intestinal cavity according to whether they can pose any danger to their carrier under certain conditions.
- healthy bacteria that function in the intestines and do not cause harm to the carrier: lactobacilli, bifidobacteria, Escherichia;
- opportunistic microorganisms that can provoke the development of certain pathological processes under certain conditions: clostridia, staphylococci, candida, enterococci;
- pathogenic, which are causative agents of dangerous diseases: salmonella, shigella.
How to properly collect stool: preparing for the test
You need to collect morning stool for analysis; it is advisable to bring it to the laboratory within an hour . Be sure to place the material in a sterile glass container (not one that contains canned meat or fish or mayonnaise). The best container in this situation is a special plastic container for such analyzes. It is necessary to ensure that the urine of a child or adult does not get into the feces. You need to collect it not from a diaper, but from a diaper.
A sterile container is the best container for collecting stool for analysis
If it is not possible to take the material in the morning, the evening feces will have to be placed on the bottom shelf of the refrigerator until the morning.
Indications and contraindications for stool culture
Stool examination is prescribed in certain cases when the doctor needs specific information about the patient’s health status. Indications for prescribing bacteriological examination of stool are:
- the need to prescribe antibiotics;
- preparation for conceiving a child;
- presence of digestive problems: constipation, diarrhea, heartburn, nausea and vomiting, heaviness in the stomach:
- stomach ache;
- increased gas formation;
- completed course of antibiotic treatment;
- manifestations of allergic reactions;
- frequent infectious diseases, suspicion of helminths;
- diagnosed cancer;
- immunodeficiency.
As for possible contraindications, this procedure does not have any - bacteriological examination of stool can be carried out at any age and in any condition of the patient.
Norms for stool analysis for microbiological culture - table
| Microflora | Children under one year old | Older children | Adults |
| Bifidobacteria | 1010-1011 | 109-1010 | 108-1010 |
| Lactobacilli | 106-107 | 107-108 | 106-108 |
| Escherichia | 106-107 | 107-108 | 106-108 |
| Bacteroides | 107-108 | 107-108 | 107-108 |
| Peptostreptococci | 103-105 | 105-106 | 105-106 |
| Enterococci | 105-107 | 108 | 105-108 |
| Saprophytic staphylococci | <104 | <104 | <104 |
| Pathogenic staphylococci | — | — | — |
| Clostridia | <103 | <105 | <105 |
| Mushrooms of the genus Candida | <103 | <104 | <104 |
| Salmonella | — | — | — |
| Shigella | — | — | — |
Interpretation of research results: Escherichia, Staphylococcus aureus, Clostridia and other microorganisms in feces
- Bifidobacteria and lactobacilli synthesize substances necessary for the normal digestive process and for the fight against “bad” bacteria, and take part in the formation of immunity.
- Escherichia appears in the intestines from birth and remains there throughout life. They take part in the formation of B vitamins, vitamin K, and the transformation of sugars. They produce substances that fight infectious agents like antibiotics.
- Bacteroides break down fats.
- Peptostreptococci process carbohydrates and milk proteins. If they increase, the doctor can diagnose intestinal inflammation.
- Enterococci process carbohydrates and provide intestinal immunity. An increase in their quantity can cause digestive upset.
- Staphylococcus should not normally be in the intestines.
Staphylococcus aureus is especially dangerous, causing foodborne illnesses. These microorganisms usually enter the intestines due to unwashed hands or foods. Staphylococcus aureus causes foodborne illnesses - Clostridia process proteins in the intestines. An increase in their quantity leads to the formation of toxic substances, which stimulates the development of putrefactive processes.
- An increase in fungi of the genus Candida leads to increased fermentation processes and fungal diseases of the intestines.
- The presence of salmonella or shigella in the material indicates a pathological condition. These microorganisms should not be present in a normal stool sample.
What does the color of stool, mucus or blood in it indicate?
The color of stool in newborns and infants is usually bright yellow; the appearance of a greenish tint indicates an imbalance of microflora or a disease. In adults, the biomaterial should be brown.
The appearance of mucus indicates inflammatory bowel disease. Blood in a child’s stool is a sign of an intestinal infection; in adults, such a symptom may be a manifestation of an oncological process in the intestines or hemorrhoids.
How to pass a biochemical analysis: explanation
These techniques are also called biochemical stool analysis. Its essence lies in the following: all microorganisms produce a certain range of fatty acids during their life activity. Some of them are specific to only one type of microorganism, while others can be produced by all bacteria. By determining the spectrum of these fatty acids, we can assume which microorganisms predominate in the gastrointestinal tract and which part of it is affected.
The advantages of this express method are the speed of obtaining results (they are available in almost an hour), the determination of not only those microorganisms that are in the intestinal lumen, but also located near its walls (these microorganisms cannot always be obtained by examining the patient’s stool), the delay of the study material (stool examination can be carried out even one day after receiving the material).
Pathogenic microorganisms
Pathogenic (disease-causing) bacteria and fungi are not found in the body of a healthy person. Their presence immediately indicates an intestinal infection, which can only be determined by the treating specialist after taking stool for bacteriological examination.
Bacteriological analysis of feces is a laboratory procedure in which a specialist takes human feces and places biological material in a nutrient medium to determine the content of pathogenic, opportunistic and beneficial microorganisms in it. The patient is prescribed stool sampling for bacteriological culture if he has characteristic symptoms of dysbiosis and intestinal infections.