Scarlet fever in adults: etiology
The incubation period for scarlet fever is on average 1-3 days, although it can appear after 12 days. The beginning is always sharp. General weakness develops quickly and appetite decreases.
When swallowing, a sore throat and headaches appear. Within a few hours, a high temperature develops up to 39 degrees, although cases of the disease with a low-grade fever, that is, within 37 degrees, have been recorded.
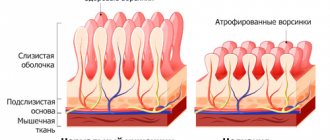
As the disease progresses, the symptoms of general intoxication of the body begin to increase and acute tonsillitis develops. Hyperemia develops on the mucous membrane of the oropharynx, the tonsils become larger and more painful. Lymphoid cells swell and accumulate in the area of the soft palate, which looks like tubercles with a diameter of 1-1.5 cm of a bright red hue.
Within 6-12 hours, rashes form on the skin in the form of red bumps, which merge with each other as they grow on the hyperpigmented surfaces of the skin and mucous membranes. This manifestation is called exanthema.
The rash is primarily localized in the upper torso, neck and proximal extremities. The nasolabial triangle is usually not affected by the rash. It manifests itself to the greatest extent as a Pastia symptom, that is, in the area of the elbow fossa, inner thighs, armpits and lower abdomen. If scarlet fever is severe, then the rashes are more pronounced.
On days 2-3, the rash with itching reaches its maximum severity, and then gradually begins to disappear. At the site of former rashes, the skin peels off and pityriasis-like scales separate on the body, and lamellar scales on the feet and palms. If scarlet fever acquires a measles-like character, then papular rashes with clear secretion develop. The skin also shows signs of white dermophagism, in which white streaks appear due to spasm of small blood vessels.
This disease is manifested by severe pain in the throat, which causes difficulty swallowing. The patient may even unconsciously make a characteristic movement with his head and grimace. There is hyperemia and swelling of the affected tissues of the oropharynx. In this case, the redness has clear boundaries. Serous exudate often accumulates on the tonsils. Scarlet fever usually has a catarrhal course of the disease, but in some cases the pathology may also occur with purulent-necrotic manifestations.
On the 3-4th day, the tongue disease gradually clears of serous plaque, exposing the granular surface. This condition lasts about 10 days. The symptom is called “raspberry tongue.”
Features and causes of scarlet fever in adults:
Causes of the disease in adults
The source of infection can be a person who is a carrier of pathogenic microflora. Scarlet fever develops when streptococci penetrate the mucous membrane of the nasopharynx.
A person can become infected by inhaling air saturated with bacteria. Rarely, the pathogen is transmitted through personal belongings. For the symptoms of scarlet fever in adults to make themselves felt, 5 minutes of communication with an infected child is enough.
In the area of infection penetration, a local focus of the inflammatory process is formed. In it, pathogenic microflora actively multiply and release toxins into the blood, which lead to intoxication of the body. This phenomenon provokes the development of a rash on the skin. If bacteria have entered the blood, there is a high probability of damage to tissues and internal organs.
Causes
The causes of the pathology can generally be divided into two categories. In the first, it is the pathogen itself. The second category includes third-party factors that increase the chances of contracting an infection.
Pathogens
The causative agent is streptococcal infection. The main pathogens are group A beta-hemolytic streptococci.
They tolerate freezing well and do not lose their viability when heated to 70 degrees for an hour. The pathogen persists in dried organic substrates for a long period.
Accordingly, the source of infection is the virus carrier, that is, contaminated surfaces and secretions secreted by a person - saliva and other liquids, as well as the person himself. Accordingly, we can conclude that the pathogen is capable of being transmitted by airborne droplets, household contact and droplets.
Scarlet fever is a toxic-mediated infection in which the pathogen produces Dick's toxin, which can cause pathological changes at the cellular level and a febrile response. Endotoxin increases the permeability of the cell membrane, which consequently contributes to the suppression of the functions of the reticuloendothelial system, causing acute inflammation in the upper dermal layers. Such exposure can lead to necrosis.
Provoking factors
Provoking factors are:
- Contact with contaminated surfaces in the presence of wound defects on the skin;
- Transmission also occurs through milk and dairy products;
- Contact with a patient if general or local immunity in the oropharynx is reduced (primary focus is tonsillitis);
- The presence of other inflammatory processes in the oropharynx, wound surfaces;
- The presence of autoimmune processes;
- Allergy.
In general, reduced immunity, untreated infectious diseases such as ARVI, influenza, tonsillitis and wound surfaces on the skin and mucous membranes play a large role in infection. An additional risk factor is abnormal functioning of the immune system.
Symptoms
Main symptoms:
- Intoxication of the body in the form of weakness, loss of appetite, lethargy;
- A sore throat;
- Headache;
- A sharp increase in temperature;
- Skin rashes (in rare cases they may be absent);
- White stripes on the skin;
- Raspberry tongue.
At the end of the course of the disease, the pathology causes peeling. In some cases, peeling was observed on the skin of the face, as well as on the feet and hands. On the fingers, the skin can completely peel off without any discomfort, revealing young skin.
In moderate and severe cases, tachycardia, purulent or catarrhal tonsillitis may be observed. Temperatures can reach 41 degrees. There is significant loss of body weight. Meningeal symptoms, decreased blood pressure, and infectious-toxic shock may develop.
The most rare cases occur in the fulminant course of scarlet fever, also called the hypertoxic form, in which symptoms increase rapidly, delirium, blackouts, convulsions, total cyanosis, and repeated vomiting appear. Without emergency assistance, this course most often ends in coma and death. Such an acute course often does not give specific symptoms of scarlet fever, which is why the pathology remains unrecognized.
Hemorrhagic scarlet fever manifests itself as a hemorrhagic rash in the form of hemorrhages under the skin. It also refers to severe forms and is considered a type of hypertoxic type of disease. This pathology is considered the most dangerous, as it most often ends in death.
When necrotizing tonsillitis occurs, the lymph nodes and adjacent tissue are involved in the process. In this case, a severe septic form of scarlet fever is diagnosed.
If infection occurs through a wound on the skin, then the extrabuccal form develops. Such a patient is less contagious to others. It is not capable of spreading the pathogen by airborne droplets. The incubation period is shortened, there are no typical symptoms of angina
If the form of sore throat is erased, the rash may not appear. Scarlet fever or rudimentary scarlet fever may develop. These patients are the most dangerous in an epidemiological sense, since they are not isolated and continue to spread the infection.
The photo shows the symptoms and manifestations of scarlet fever
Scarlet fever symptoms in adults photo rash
Scarlet fever is an infectious disease characterized by acute development of symptoms. The causative agent of the disease is considered to be a pathological microorganism from the streptococcus family, which releases dangerous toxins in the human body that lead to deterioration of health.
Currently, scarlet fever is considered a childhood disease. However, it is not. It can also affect adults who did not have scarlet fever in childhood and have weakened immunity.
This is especially true for people under 30 years of age, as well as the elderly and those suffering from chronic diseases, although cases of scarlet fever in adults are now quite rare.
Scarlet fever in adults photos
We recommend that you familiarize yourself with what scarlet fever looks like in the photo.
Classification
Depending on the route of infection, two forms of scarlet fever are distinguished in adults:
- Pharyngeal - bacteria enter the body through the mucous membrane of the oropharynx;
- Extrapharyngeal - the pathogen can enter the blood through the wound surface of the skin, after which it spreads throughout the body.
The disease can occur in a standard or atypical form. The latter form includes scarlet fever with an erased or rudimentary course.
It is worth highlighting the following three forms of scarlet fever:
- Extrabuccal form. It occurs extremely rarely, as it is characterized by penetration of the pathogen through wounds. The disease has an extremely short incubation period, after which a rash begins on the skin from the site of infection and beyond. The pharynx has a healthy appearance, which distinguishes this disease from other forms.
- Erased form. Adults are more likely to experience this form of the disease. Although the main symptoms of scarlet fever are present, intoxication is mild, and skin rashes quickly disappear.
- Septic form. Unlike children, adults are more likely to have severe scarlet fever. The disease occurs abruptly and is accompanied by multiple complications. Skin rashes look like petechial hemorrhages. Kidney diseases, blood poisoning and other pathologies may develop if not treated in a timely manner.
Symptoms
The incubation period for scarlet fever in adults (see photo) can range from 1 to 10 days.
The disease most often begins with “acute” symptoms: a sudden sharp rise in body temperature (up to 40–41 C), the appearance of a pronounced intoxication syndrome (weakness, headache, nausea, vomiting).
Severe tachycardia also occurs (as the body’s response to an increase in body temperature), and abdominal pain may occur. Sometimes, at the onset of the disease, low-grade fever and slight malaise may occur.
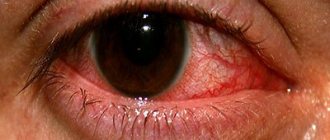
A characteristic symptom of scarlet fever is the appearance of a sore throat when swallowing. Upon examination, pronounced hyperemia (redness) of the pharynx, tonsils, soft palate, and pharynx is detected. White-gray plaques may appear on the tonsils.
In the first days of the disease, the tongue is covered with a grayish coating; on the 4th–5th day it clears, it acquires a bright crimson color, the papillae look hypertrophied - this is one of the symptoms that allows one to diagnose scarlet fever in adults.
The appearance of the symptoms described above is often regarded by adults as a severe cold or sore throat, but with scarlet fever a number of characteristic symptoms appear that allow one to suspect the disease. With scarlet fever, simultaneously with the appearance of hyperemia of the pharynx, regional lymphadenitis develops, and hardening and tenderness of the anterior cervical lymph nodes are noted.
1–2 days after the onset of the disease, skin rashes typical of scarlet fever appear; this symptom also often helps to establish the correct diagnosis in adults.
With the erased form of the disease in adults, the rash may be pale, not abundant or practically absent, or may disappear a few hours after its appearance.
On days 3–5, the symptoms of scarlet fever begin to subside, the temperature drops, the rash resolves, the hyperemia of the pharynx decreases, but pain during swallowing movements still persists. After about a week, the skin begins to peel in places where there were skin rashes.
Diagnostics
The diagnosis is made taking into account clinical indicators, supplemented by laboratory tests.
When conducting a physical examination, the doctor first of all pays attention to the patient’s symptoms of acute intoxication, catarrhal phenomena, exanthematous rashes, thickening in the natural folds of the skin and pronounced white dermographism, gradually giving way to peeling (fine-scaly on the body and large-plate on the soles and palms).
Laboratory diagnostics include clinical and biochemical blood tests (cardiac-specific enzymes are taken into account), a general urinalysis, microbiological examination (bacteria culture from the source of infection) and a serological retrospective study of antistreptolysin (ASLO antibodies) to streptolysin (antigen of β-hemolytic streptococcus).
Both in the hospital and on an outpatient basis, scarlet fever needs to be differentiated from other diseases; in 28% of cases, the diagnosis is incorrect and scarlet fever in adults is mistaken for:
- Rubella - 20% of all misdiagnoses
- Measles (see symptoms of measles in adults) - 19%
- Infectious mononucleosis - 14%
- Pseudotuberculosis - 13%
- Lacunar tonsillitis - 12%
- Drug dermatitis, toxicoderma -9%
- ARVI - 5%
- Food poisoning - 5%
- Adenoviral infection - 2%
- Meningitis - 1%
Until now, in our country, not everywhere there are accessible and effective 100% early diagnostic methods, laboratory tests for the determination of scarlet fever (rapid tests for streptococcus (strips).
And doctors have to be guided only by the clinical manifestations of the disease, which is why so many erroneous diagnoses are made.
When a person needs urgent treatment, and the diagnosis is not correct, sometimes doctors prescribe inadequate therapy.
Complications
Most often they occur due to untimely treatment or an erased form of scarlet fever. The following consequences are possible:
- purulent sore throat;
- otitis;
- sinusitis;
- pneumonia;
- foci of necrosis on the tonsils;
- glomerulonephritis, renal failure;
- hemorrhagic vasculitis;
- myocarditis, endocarditis, heart failure;
- toxic shock;
- joint damage, including arthritis;
- sepsis;
- hemorrhage in the adrenal cortex or brain.
In case of severe manifestations, you must immediately go to the hospital, otherwise death is possible.
Medicines
Drug treatment for scarlet fever is the most important. It involves taking etiotropic drugs (antibiotics), as well as symptomatic ones (painkillers, antipyretics).
The following medications are indicated for patients:
- Antibiotics of the penicillin group (Penicillin, Amoxicillin). If you are allergic to Penicillin, the doctor can replace it with macrolides, cephalosporins (Azithromycin, Clarithromycin, cephalosporin). Antibiotics are taken strictly according to the course, without ending treatment prematurely even with significant relief.
- Antipyretic drugs. Prescribed at elevated temperatures. As a rule, they take Aspirin, Ibuprofen, Paracetamol.
- Antihistamines. Used to combat itching in severe skin rashes. The most popular are Tavegil, Zirtek, Cetrin.
- Probiotics. The drugs are taken to eliminate the negative effects of antibiotics on the microflora of the oral cavity and stomach. Linex, Bifiform, Hilak forte are prescribed.
- Vitamins. Since the immune system is weakened, doctors usually prescribe vitamin complexes or immunomodulatory drugs to prevent the occurrence of new infections.
Bed rest
Maintaining rest is the first measure of help for a sick body. It is necessary to rest for at least 7 days, but no less than for the entire period of illness and 2 days after recovery. The need for such a gentle regimen is due to the fact that the disease can hit the heart.
Severe forms of scarlet fever are treated in a hospital. Bed rest involves providing the patient with his own room. Avoid going to work and visiting crowded places. It is better to wait for a doctor than to expose yourself to additional risk.
Rinsing and irrigation
Furacilin solution is most often used as local therapy. Rinse your mouth and throat with an antibacterial agent every hour. To do this, you can purchase a ready-made solution at the pharmacy or buy tablets that are dissolved at the rate of 2 pieces per glass of water.
You can use other equally effective means to gargle:
- Chlorophyllipt,
- propolis,
- Rotokan,
- various herbal infusions,
- salt compounds.
As for sprays, Miramistin, Ingalipt and Hexoral are usually used to combat the effects of scarlet fever.
Physiotherapy
In order for the patient to recover faster, he may be prescribed a number of physiotherapy procedures that will help quickly cure a sore throat and clear the tonsils of streptococcal plaque. Therapy should include the following procedures:
- Treatment of tonsils with UV rays, which have a destructive effect on proteins in bacteria and thus destroy them.
- SVM therapy of the tonsils is carried out.
- Magnetic laser therapy is indicated to activate the immune system.
- UHF therapy to accelerate the healing of ulcers and relieve inflammation from soft tissues.
- FUF procedures cleanse the tonsils of pathogenic microorganisms.
Physiotherapy procedures are performed only if there are no general health contraindications.
Diagnostics
When diagnosing scarlet fever, it is made after examining the patient. Laboratory tests are also carried out, suggesting:
- donating blood, urine;
- microbiological examination of a smear from the source of infection;
- A retrospective study of the anti-streptolysin antibody ASLO (anti-streptolysin).
ECG and ECHO-CG are also considered necessary. It is necessary to differentiate the pathology from rubella, allergies, and the scarlet-like form of pseudotuberculosis.
Treatment
Treatment of scarlet fever in adults involves the use of a number of therapeutic, physiotherapeutic and medicinal methods. The patient must be isolated, but treatment can take place at home. In particularly severe cases, hospitalization is necessary.
General recommendations
The patient needs:
- isolate in a separate room (10 days if the patient is recovering);
- carry out regular wet cleaning and ventilation of the room;
- follow the prescribed diet (gentle nutrition with a liquid or semi-liquid diet);
- taking large amounts of fluid;
- Bed rest is mandatory.
Adults who live with preschoolers or schoolchildren who have not had scarlet fever are subject to hospitalization.
Medication
Drug treatment involves:
- use of penicillin antibacterial drugs (10 days, 6 million units per day);
- macrolides, alternatives to penicillin drugs, if there is intolerance to this type of drug - cephalosporins, erythromycin, lincosamides, semi-synthetic penicillin.
- Gargling with furatsilin or herbal infusions;
- Spraying the throat with antiseptics such as Miramistin.
If the patient has a severe form of scarlet fever, then it is necessary to use antitoxic scarlet fever serum in the first 48 hours. It is not used for the septic form of the disease.
Reviews about the treatment of scarlet fever:
Physiotherapy
Physiotherapy involves the use of ultraviolet irradiation of the affected areas. But this method of treatment is practiced at the discretion of the doctor. In some cases it simply makes no sense to use it.
Symptoms of the disease and photos
The main distinguishing sign of this infection is exanthema (see photo). This is the name of a characteristic red rash that quickly spreads throughout the body. The phenomenon is accompanied by severe itching of the skin. The remaining symptoms are typical for sore throat and other infectious diseases:
- Acute sore throat with redness of the tonsils and dry cough . Enlargement of the cervical lymph nodes is often noted.
- A general deterioration in health, fever, nausea and severe headache are a consequence of intoxication of the body. During its life, streptococcus releases toxic substances that, if left untreated, can cause vomiting and dyspepsia.
- Scarlet fever in adults causes changes in the tonsils : in addition to redness, their swelling, friability and a specific white coating are noted. Less commonly, ulcers may appear.
Symptoms of the disease with proper timely treatment weaken already on the 3rd day. The exanthema goes away within a week, and by the end of the ten-day period the patient’s condition improves significantly.
Complications
The main complications from the pathology:
- Otitis;
- Sinusitis;
- Nephritis;
- Myocarditis of infectious-allergic type.
In pregnant women in the first trimester, infection causes spontaneous abortion. Later dates have favorable prognoses. Antibacterial therapy is prescribed only after 12 weeks. The rest of the treatment does not differ from the classical one.
It is worth noting that with a weakened immune system (HIV or after treatment for cancer), mastoiditis, streptococcal sepsis or adenophlegmon can develop.
Prevention
Prevention is
- Isolation of the patient;
- Wearing protective equipment when in contact with a sick child (face mask);
- Increasing the functionality of the immune system with vitamin preparations and other means;
- Complete treatment of infectious pathologies of the oropharynx and other areas;
- Treating wound surfaces with an antiseptic and covering them with protective agents - bandages or plaster;
- Maintaining oral and skin hygiene;
- Normalization of lifestyle, nutrition, work and rest;
- Avoid contact with infected people.
Why scarlet fever is dangerous, watch in our video:
Forecast
The prognosis depends on the course and form of the disease, as well as on the speed of seeking treatment from a doctor. Severe forms without providing appropriate assistance in the first two days often end in complications at best, and death at worst.
For mild forms with adequate treatment, the prognosis is presumably good. Complications rarely develop. In case of pregnancy, positive prognosis is possible for the woman. For the fetus, the disease is not dangerous only if the period is more than 4 months. Early pregnancy usually ends in spontaneous abortion, which doctors are most often unable to prevent.
Physiotherapy
If a doctor diagnoses scarlet fever in adults, symptoms and treatment require a comprehensive approach. Therefore, along with medications, physiotherapy may be recommended. Such measures will help get rid of the sore throat that accompanies scarlet fever and clear the tonsils of streptococci. Therapy includes the following procedures:
- Irradiation of the tonsils with UV rays, which destroy proteins in bacteria and destroy them.
- SMV therapy for tonsils.
- Magnetic laser therapy to improve blood circulation and activate the immune system.
- UHF therapy to eliminate inflammation and heal ulcers.
- FUF therapy destroys bacteria and cleanses the tonsils.