The expectant mother should always take care of her health, since during pregnancy the baby should receive a minimum amount of medication and optimal conditions for development. That is why candidiasis during pregnancy is not only undesirable, but can also pose a serious danger to the unborn baby. This disease does not simply cause fungal infection of both the mother and the developing child. Thrush is the cause of all kinds of inflammatory processes, in particular, the fungus causes adhesions, which provoke painful sensations that are especially strong in the 3rd trimester of gestation. The place where adhesions form can be anywhere, and if they form in the genitals, this can be fatal for the unborn baby, as they provoke miscarriage or termination of pregnancy.
Signs of the disease
Thrush develops not only against the background of reduced immunity: an increase in the acidity of the vaginal environment (for example, in the presence of dysbiosis, chronic inflammatory process) creates a favorable environment for fungi.
Signs of thrush: curdled discharge
Hormonal imbalance and changes are another reason for the activity of fungal infection. At this time, a woman is most sensitive to the slightest changes in the bacterial flora.
The development of infection can be provoked by a lack of vitamins and microelements - the expectant mother’s body especially needs them. Therefore, it is important to eat right from the first days of pregnancy, and also, if possible, treat chronic inflammation in advance.
If thrush has already begun, you should definitely consult a doctor.
Symptoms of candidiasis in pregnant women:
- Copious white cheesy discharge with a pronounced sour odor.
- Swelling and swelling of the vulva.
- Itching and burning that gets worse at night.
- Irritation and redness of the mucous membrane.
When these symptoms are pronounced and constantly bother a woman, she becomes irritable. In this case, hoping that it will go away on its own is wrong: before childbirth and during breastfeeding, the woman’s immunity will remain reduced and will not be able to overcome the infection on her own .
The mechanism of fungal spread
Pregnancy is a special state of a woman’s body, when all systems work in increased mode , there is a decrease in general and local immunity, which in turn weakens the protective function and makes the expectant mother “easy prey.”
Studies have shown that fungi of the albicans type can attach to vaginal cells, and in relation to white blood cells (protective) cause disruptions in their functioning - therefore the body cannot quickly respond to the “invasion” .
Currently reading: Hidden pregnancy
It is very important to note that a low level of lactobacilli in a woman’s vagina is a favorable environment for the proliferation of pathogenic flora , because it is these microorganisms that produce hydroperide, which inhibits the growth of fungi.
Frequent use of antibiotics reduces the number of these bacteria in a woman's vagina and provokes the development of candidiasis , which can subsequently become resistant to antibiotic therapy. This list also includes local antibiotics; they can also cause thrush.
If we talk about transmission routes, it can be noted that the sexual route is one of the factors of infection and can provoke candidiasis, however, the percentage of transmission of the fungus through sexual contact is not so high.
Danger of disease during pregnancy
To treat or not to treat candidiasis in pregnant women? Doctors do not have a clear opinion on this matter.
Some believe that it is better not to subject the expectant mother’s body to medicinal stress once again, especially if the disease does not cause concern.
Others are sure that it is better to choose the safest possible drug and undergo treatment so as not to infect the baby during childbirth.
Danger for women
Weakened local immunity of the vagina and the presence of fungi can provoke the addition of another, more severe infection that will spread to the uterus. This can lead to various complications and miscarriage .
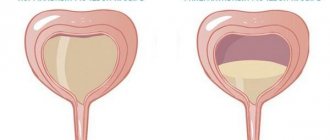
Hypertonicity of the uterus
Inflammation of the genital tract often causes hypertonicity of the uterus, and this is the cause of a lack of oxygen and the risk of premature birth.
Cervical erosion
Inflammation reduces muscle elasticity, so a woman with candidiasis is at higher risk of tearing during childbirth. The fungus also increases the risk of cervical erosion.
Chronic candidiasis
In addition, the long-term presence of untreated candidiasis can lead to a woman developing a chronic form of the disease. Even after childbirth, it will be difficult to cure it.
Danger to the fetus
While the baby is in the womb, he cannot become infected. Infection occurs in rare cases when thrush rapidly develops in the mother - the child is at risk of intrauterine infection.
Premature birth
The biggest risk at this time is premature birth, when the baby’s body does not have time to fully form and prepare for life outside the mother’s body.
Fungal diseases of the newborn
But most often, infection occurs during childbirth. From the very first days, such a baby develops candidal stomatitis, redness and inflammation of the skin, and dermatitis. But this is not the worst thing.
If the infection enters the internal organs through the bloodstream, the newborn may die.
What is the danger?
Thrush must be treated before the baby is born.
Thrush does not have a negative effect on the course of pregnancy. There is no evidence that it can cause premature birth or spontaneous miscarriage. And it does not cause the development of endometritis after childbirth. Why does it need to be treated? Why is thrush dangerous during pregnancy? The answer is obvious. Any change in the body is fraught with disruptions in the functioning of this well-coordinated mechanism. But what other dangers does thrush pose? You will find the answer to this question in this article.
The development of candidiasis entails a further change in the microflora; a favorable environment may form in the vagina for the development of other pathogenic microorganisms that are not as harmless as thrush.
Approved medicinal products
You should not buy the first drug you come across, or try to get rid of the disease on your own with the ones prescribed to you before pregnancy: most antifungal drugs can cause serious problems in the fetus.
The doctor must prescribe the medicine, taking into account the general condition of both the woman and the baby, as well as all the risks that the treatment may cause.
Typically, for the treatment of candidiasis, local treatment is supported by tablets. During pregnancy, only local treatment is used .
It may not give a 100% effect and get rid of thrush for life, but it will alleviate the symptoms and reduce the risks for mother and baby.
Pimafucin
Pimafucin.
Vaginal suppositories The active ingredient is natamycin, one of the safest, yet effective local remedies. But provided that the woman tolerates it well (alas, in many this drug causes a local allergic reaction).
Therefore, you should not buy this drug on your own in the hope that it will relieve symptoms - neither during pregnancy nor at any other time.
Pimafucin is used in the form of suppositories. The average price in pharmacies is from 500 rubles (for 6 candles).
If the doctor prescribed Pimafucin, but the nearest pharmacy did not have it, you can take Ecofucin or Primafungin - these are analogue drugs.
Clotrimazole
Clotrimazole. Ointment
An effective fungicidal agent, available in the form of cream and suppositories. Suppositories are used once at night for a week. The cream is not used on its own - only in addition to suppositories to speed up recovery.
Clotrimazole rarely causes side effects or allergies. But it is not advisable to use it in the first trimester.
An important point: if the burning and itching does not stop after two days of use, it is advisable to change the drug to a more effective one - again, on the recommendation of a doctor.
Clotrimazole is inexpensive - from 40-50 rubles and above, depending on the type of drug and dosage. Its analogues are: Amyclone, Antifungol, Kandizol, Triakutan .
Terzhinan
Terzhinan. Vaginal tablets
This is a French drug that is effective against Candida fungi and some other bacteria that cause inflammation of the vagina.
Available in the form of tablets, which must be soaked before administration. The course of treatment ranges from 10 days to 2 weeks.
The drug reduces local immunity, so you need to stop having sex during treatment.
Terzhinan is prescribed from the second trimester. But in rare cases, it can be prescribed in the first weeks of pregnancy.
In the first days, unpleasant symptoms may intensify - immediately after administration of the tablet. But soon they will begin to subside.
The price of the drug starts at 380-400 rubles per package. There are no complete analogues (with identical composition) of Terzhinan; conventional ones can be called Meratin Combi and Neotrizol.
Livarol
Livarol. Vaginal suppositories
It is prescribed for only 3-5 days, and relieves symptoms almost instantly. But it is allowed only from the second trimester.
This is a local drug that is not absorbed into the blood at all, therefore it is not toxic to the fetus. Some doctors note that Livarol is more effective and better tolerated than Pimafucin.
The cost of the drug is approximately 340 rubles for a package of 5 suppositories. Analogues of Livarol are Mycoquet, Oronazole and Clotrimazole.
If candidiasis is not treated during pregnancy
Candidiasis (thrush) is a very unpleasant, and in some cases even dangerous, disease. So, pregnant women often suffer from this disease. The danger of developing a yeast-like infection in the body is that a woman may experience problems associated with bearing a fetus and the course of pregnancy. Also, a fungal infection can be transmitted to the fetus while still in the womb or while passing through the birth canal. What to do if a pregnant woman has thrush and is it necessary to treat this disease, or is this a common occurrence for women expecting the birth of a baby?
What will the article tell you?
Many women before pregnancy did not even know what thrush was, but during pregnancy they develop this disease. Why are pregnant women susceptible to it? What is the cause of persistent thrush during pregnancy? The appearance of a fungal infection during pregnancy is associated with changes in the hormonal levels of the expectant mother. At this time, the number of lactobacilli decreases, as a result of which the microflora changes, from a normal state to a pathological one. This is facilitated by the penetration of Candida fungi into the mucous membrane and further proliferation in it.
In addition, very often factors that contribute to a decrease in the body’s defenses and changes in the vaginal microflora include:
- stress;
- chronic diseases;
- bad ecology;
- insufficient consumption of vitamins, fresh vegetables and fruits;
- lack of sleep, rest.
This disease is already dangerous in itself, but during the period of bearing a child it can greatly harm both - the expectant mother and the baby:
- Spontaneous miscarriage is possible in the first trimester.
- A fungal infection can even cause oxygen starvation, as a result of which the child is born with various abnormalities.
- Fetal growth may be delayed and the child may be born with a critically low birth weight.
- A pregnant woman may lose amniotic fluid prematurely, as a result of which the birth will be difficult, and doctors will have to literally save the baby.
- After childbirth, a woman often experiences an inflammatory process in the uterus, called endometritis, against the background of thrush.
- The child may experience candidiasis of the skin, oral mucosa and genital organs.
That is why it is so important to detect the disease in a timely manner and begin surgical treatment. Don't know what to do if you have thrush during pregnancy? Your task is to seek help from the gynecologist who is managing your pregnancy, take the necessary tests, and undergo inpatient or outpatient treatment.
Trying to cope with an illness on your own is not only stupid, but also dangerous, because we are talking not only about the health of the mother, but also the unborn baby. Even if before conception you suffered from candidiasis, you know how to treat it and with what medications, then when you are pregnant, you should forget about the old treatment. After all, the treatment of thrush in patients in an interesting situation is completely different. It is absolutely impossible to undergo treatment without the help of a doctor and his advice. Therapy for candidiasis should be carried out comprehensively and only under the supervision of a specialist.
To successfully treat yeast-like fungi you need:
- resort to medication;
- Healthy food;
- observe the rules of personal hygiene.
Let's look at what women should do during pregnancy to deal with thrush, and what medications can be used to quickly destroy the Candida fungus? After all, most drugs for this problem cannot be used by this category of patients. The main thing that a woman should remember is that the medicine must be safe, and if the instructions say that the medicine is contraindicated while pregnant, then you should not risk being treated with this medicine.
When treating thrush in pregnant women, doctors often prescribe therapy with local medications - vaginal tablets, suppositories. The most common of them are:
- Polygynax - vaginal capsules containing nystatin, neomycin. These components have antifungal and antibacterial effects. It is not recommended to use the drug for a long time. It cannot be used by women in the first trimester, but it can be used in the second and third.
- Nystatin is a vaginal suppository that causes a weakening of the protective membrane of fungal cells, leading to its death. The peculiarity of these suppositories is that they act selectively: they purposefully destroy the Candida fungus and do not cause the destruction of beneficial microorganisms.
- Betadine - these suppositories are recommended for the treatment of thrush in the first trimester. If a woman is not allergic to iodine or has problems with the thyroid gland, then she can safely use these suppositories. The duration of treatment should be no more than one week. But from the second trimester, treating vaginal candidiasis with Betadine suppositories is not recommended, because the substances contained in the drug can penetrate the placental barrier and cause disruptions in the functioning of the thyroid gland.
Very often, the symptoms of this fungal infection depend on the patient’s diet. Therefore, the patient’s first priority is to review her diet, temporarily remove sweets, caffeine, sweet fruits, spicy, fatty, spicy foods from it. Such food not only feeds the fungus, giving it a chance to further flourish, but also has a bad effect on the well-being of the pregnant woman and the development of the fetus.
The diet of a patient expecting a baby should be rich in vegetables. Cabbage, carrots, cucumbers, beets, tomatoes, eggplants, greens - all these fresh vegetables must be included in the patient’s diet. The following products are also recommended for her:
- fruits – green apples, plums, cherries;
- dairy products - kefir, fermented baked milk, sour cream with a low fat content;
- cereals – buckwheat, barley, rice porridge;
- Drinks: rosehip, fruit compote.
Personal hygiene of a pregnant woman is a very important issue in getting rid of a fungal infection as quickly as possible. If a patient’s thrush does not go away during pregnancy, she may underestimate the role of intimate hygiene in the treatment and prevention of fungal infection. When the disease appears, the patient must adhere to the following recommendations:
- Wash twice a day using warm running water. You cannot use regular or liquid soap - it dries out the vaginal mucosa very much. You should give preference to special liquid or gel based products. It is very good if the patient uses Lactacid or its analogues. This drug not only helps keep the genitals clean, but also removes pathogenic fungi on the surface of the skin.
- When washing, the water stream should be directed forward, the patient should wash from front to back. Otherwise, bacteria from the anus can get onto the labia, further into the vagina, and then there will be even more problems.
- You can't get carried away with douching. You can use herbal remedies or special medicinal liquids only as recommended by a doctor. It is imperative to observe the frequency of such procedures and the duration of their use.
- Use your own towel. For the genital area, you need to choose a soft towel so that it does not cause irritation. The towel needs to be washed regularly and must be ironed.
- It is better not to wear panty liners, especially in summer, since these hygiene products create a greenhouse effect and contribute to the active growth of fungus. But if the patient cannot live without such pads, then she should take care of changing them regularly (every three hours).
- Wear cotton panties. Natural fabric perfectly absorbs sweat, does not steam the skin, and does not impede oxygen access to the genitals. The patient should change her panties daily.
- During treatment for thrush, you should abstain from sexual activity.
Many women do not know what to do when thrush does not go away during pregnancy. It seems that the treatment was carried out in accordance with the instructions and recommendations of the doctor, but the disease still does not lag behind and returns.
The reason for this phenomenon, the return of candidiasis like a boomerang, may be that:
- A woman’s body has a more serious infection that is sexually transmitted, for example, chladydia or ureaplasmosis.
- The woman is not treating a fungal infection of the Candida genus, but another type of fungus. After all, there are about 200 species. And if a woman has not been tested, does not know exactly what pathogen is in her body, and carries out treatment according to the usual regimen, then there may be no effect from such therapy.
- The patient's immune defense is severely weakened. In pregnant women, due to hormonal changes, immunity drops significantly. If the patient does not take immunostimulants in parallel with antifungal drugs, the fungus may continue to return. After all, bacteria and fungi are present in the body only in a certain concentration.
- The patient has intestinal dysbiosis. If a woman is treating vaginal thrush, but has problems with her intestines, then she should definitely reconsider her diet and start leading a healthy lifestyle.
Based on materials from medicsina-blog.ru
According to statistics, candidiasis occurs in 9 out of 10 women during pregnancy. Most often, this disease manifests itself in the last trimester. But, despite the “harmless” symptoms, the infection can lead to serious consequences for both the expectant mother and the child.
Candidiasis or thrush develops due to excessive proliferation of the yeast-like fungus Candida albicans. In small quantities, its strains are present in the normal microflora of the vagina.
Candidiasis during pregnancy is becoming more common, despite the development of diagnostic and therapeutic trends in medicine. The main reasons are the adverse effects of external factors in combination with reduced immunity.
While expecting a child, a woman's body undergoes a restructuring. The intestinal microflora changes, and a deficiency of vitamins and minerals appears.
Dysbacteriosis leads to increased proliferation of pathogenic microorganisms, including Candida fungi. From the intestines they can spread to the vaginal mucosa.
Hormonal levels change. This factor acts in several directions at once.
Firstly, increased levels of progesterone inhibit the activity of the immune system, so adverse external influences such as hypothermia, overwork, and unbalanced nutrition can easily lead to the development of candidiasis.
Secondly, the action of hormones changes the vaginal mucosa, making it more susceptible to infections.
Thirdly, changes in hormonal levels lead to emotional disturbances, reduce resistance to stress, which provokes a decrease in the body’s protective functions and the development of thrush.
In addition to these specific features, candidiasis in pregnant women can develop for reasons common to all women:
- chronic infectious diseases, including genital diseases;
- the presence of thyroid pathology, diabetes mellitus, obesity;
- chronic diseases of the intestines (colpitis, dysbacteriosis), liver or kidneys;
- taking antibiotics or hormonal drugs;
- unbalanced diet with a predominance of sweet foods.
Candidiasis is a sign of trouble in the female body, a decrease in general immunity. Therefore, treatment of the disease should be aimed not only at destroying the fungus, but also at strengthening the immune system.
Vaginal candidiasis during pregnancy does not have symptoms that are different from those at any other time in a woman’s life. As a rule, patients complain of itching, white cheesy (flaky) discharge with a sour, unpleasant odor.
Itching and pain intensify during sexual intercourse and disappear for a while after hygiene procedures. On examination, irritation and redness of the external genitalia are noted.
But all these symptoms can indicate not only candidiasis, but also a number of other diseases (including STDs).
To clarify the diagnosis, the doctor writes out directions for diagnostic examinations:
- Microflora smear. During the procedure, a tampon is inserted into the vagina and the contents (mucus, discharge) are collected on it. The material is then dried on a viewing glass and examined under a microscope. The laboratory technician counts the number of bacteria, fungi and leukocytes. With vaginal candidiasis, the smear reveals fungi, a large number of leukocytes, characteristic of inflammatory reactions, and a predominance of pathogenic bacteria over beneficial ones. Read more: what a gynecological smear shows→
- Bacterial culture. It is not always carried out; it allows us to identify exactly which bacteria and fungi inhabit the vagina, as well as determine effective drugs for treatment.
Since it usually takes several days to obtain diagnostic data, the doctor prescribes therapy after the first examination and then, if necessary, supplements and adjusts it.
Candidiasis is a fungal disease associated with decreased activity of the immune system. Therefore, its treatment includes the use of antifungal and immunostimulating agents.
Antifungal drugs, in turn, are divided into systemic (tablets, capsules for oral administration) and local (creams, suppositories, etc.).
Treatment of candidiasis during pregnancy should be comprehensive. Tablets and capsules destroy the fungus in the intestines, where its main focus is located, and local preparations act on the surface of the vaginal mucosa, quickly eliminating unpleasant symptoms.
Most often, the following are prescribed for the treatment of thrush in pregnant women:
- Systemic antifungal drugs: Nystatin, Pimafucin. They are allowed both during pregnancy and during breastfeeding, they are effective and non-toxic. More popular antifungal agents, for example, Diflucan and Fluconazole, are contraindicated in pregnant women.
- Local preparations: “Epigen Intim” (spray), “Pimafucin” (cream, suppositories), “Nystatin” (suppositories). The spray is used in combination with Nystatin or Pimafucin, quickly relieves inflammation and restores normal vaginal microflora. The selection of drugs in each specific case should be done by a gynecologist, since there are drugs that are contraindicated in the first trimester, but acceptable in the later stages.
- Local anti-inflammatory and antiseptic drugs. During pregnancy, the use of a solution of borax in glycerin (sodium tetraborate in glycerin) and brilliant green (brilliant green) is allowed. These products are applied to a gauze swab and mechanically clean the vaginal walls of fungus. This prevents its growth and relieves inflammation. In addition, the drugs are approved for use in the first three months of pregnancy, when other drugs are contraindicated.
- Immunomodulatory and restorative drugs. Excessive proliferation of pathogenic microflora in the intestines and vagina begins with a decrease in immunity, or in the presence of a chronic disease. To treat thrush during pregnancy, it is possible to prescribe multivitamins, Viferon suppositories, as well as probiotics with bifidobacteria (Bifidin, Bifidumbacterin).
When deciding how to treat candidiasis during pregnancy, you should first consult with a gynecologist.
All groups of drugs must be prescribed by a specialist, as they have their own contraindications. It is necessary to take into account the woman’s general health, tendency to allergies and other factors.
It is important to undergo therapy together with your sexual partner. Otherwise, the infection will manifest itself again. Men can use any antimycotic drug: Fluconazole, Nystatin, Diflucan, Nizoral, etc.
In combination with medications, candidiasis during pregnancy can be treated with traditional methods:
- Baths with iodine and soda. For the first procedure, you need to dissolve 1 tsp in a liter of boiled warm water. soda and sit in the basin for about half an hour. For the second and subsequent procedures, add 1 tsp to the soda solution. Yoda. Do baths once a day until complete recovery.
- Douching with salt, soda and iodine. In one liter of boiling water you need to stir 2 tbsp. l. salt, boil the solution, cool until warm. Then, add 1 tbsp. l. soda and 0.5 tsp. Yoda. The douching procedure is carried out twice a day for 5 days.
- Irrigation with herbal infusion. To prepare the infusion, you need to mix 3 tbsp. l. chamomile, yarrow, calendula and sage. 2 tbsp. l. pour the resulting mixture with a liter of boiling water, leave for several hours, strain. Irrigation is carried out using a syringe bulb. The procedure is repeated twice a day for two weeks.
You cannot rely only on folk remedies; they are all local and do not completely eliminate the infection.
During the treatment of thrush during pregnancy, most antifungal drugs are contraindicated. They can lead to various developmental disorders of the fetus, including heart defects and pathologies of skull formation.
The drug Betadine, which is often used outside of pregnancy, should not be used; it affects the development and functioning of the thyroid gland of the unborn child.
Sometimes, having heard that taking probiotics is recommended for candidiasis, women begin to use drugs with lactobacilli, which create a favorable environment for the development of a fungal infection. It is important to remember that for thrush it is bifidobacteria that are needed.
With properly organized treatment, improvements become noticeable already on the second or third day. In some cases, by this time the symptoms have completely disappeared, creating the appearance of recovery.
In fact, a significant amount of fungus is still present in the body, and the positive effect is due to local elimination of the causative agent.
It is necessary to continue the course of treatment until the end, regardless of how you feel. This will help avoid relapses and the transition of candidiasis to a chronic form.
Treating thrush during pregnancy is not an easy task, so you need to try to prevent the fungus from spreading.
To prevent candidiasis, you must adhere to the following recommendations:
- Wear clothes, and especially underwear, made from natural fabrics that allow air to pass through and prevent the creation of a damp and warm environment.
- Choose the right intimate hygiene products. They should not be aggressive and disturb the natural acidic environment of the vagina (the best option is with a neutral pH level).
- Avoid constipation and dysbiosis by consuming enough fresh fruits, vegetables, and, if necessary, preparations with bifidobacteria. If you find problems with the intestines, consult a doctor immediately.
- If you are prone to fungal infections, regularly carry out tests to determine the pH and, in case of deviations, contact a specialist.
- Maintain immunity: eat a balanced diet, take multivitamins, regularly walk in the fresh air, engage in physical activity (gymnastics, swimming, walking), if there are no contraindications.
Thrush is a disease that, in the absence of timely treatment, leads to unpleasant consequences for the expectant mother and baby.
Some women, especially those with a chronic form of the disease, have a question: is it possible to get pregnant with candidiasis? Of course, this is physically possible. But by treating the disease in advance, a woman will avoid many complications.
A fungal infection makes the vagina less elastic, which causes cracks and external and internal tears to form during childbirth.
For this reason, at the end of pregnancy, the gynecologist conducts a thorough examination of the woman in the chair and, having detected signs of microflora disturbance, prescribes treatment.
Thrush complicates the healing process of sutures after childbirth: suppuration and inflammation often occur, requiring antibiotics.
The consequences for the child are more serious. The fungus penetrates the internal organs of the newborn, affecting the eyes, nose, mouth, skin and mucous membranes of the respiratory system. This leads to health problems and, in rare cases, death.
Due to the characteristics of the female body, thrush is a common problem during pregnancy. Natural changes in hormonal levels and decreased immunity in the expectant mother lead to the development of infection.
Treatment is complicated by the fact that many drugs are contraindicated during pregnancy, so from the first trimester it is worth paying special attention to preventive measures.
Author: Olga Khanova, doctor, especially for Mama66.ru
Based on materials from mama66.ru
During the intrauterine development of a child, a woman’s body’s defenses are significantly reduced. Patients become defenseless against many diseases controlled by the body's immune system. Thrush during pregnancy is a pathology that occurs when immunity declines.
The main cause of pathology in the first trimester is a hormonal surge in the body. The fungus of the albicans variety, which provokes dysbacteriosis in the perineum, is contained in the microbiota of the genital organs even before conception, but does not bring significant discomfort to the girl.
When ovulation occurs and fertilization of the egg with sperm occurs, a hormonal surge occurs in the body, affecting the intimal microbiota. Rising progesterone plays a key role by changing the acidity of the environment.
When the imbalance is disturbed and acidity increases, the most fertile time comes - their active reproduction begins and their number increases in relation to opportunistic microorganisms. Outwardly, this manifests itself as symptoms of a vaginal infection.
Thrush during pregnancy manifests itself with typical markers, but sometimes the symptoms of the pathology even intensify. The main symptom is the appearance of white discharge with a curd or creamy consistency, as well as itching, a burning sensation in the genital area, irritation at the vestibule of the vagina and labia minora. The discharge is characterized by an unpleasant sour odor.
A severe form of the pathology worsens general well-being, lethargy and fatigue appear. Signs of vaginal dysbiosis appear in any period, but in the latter period the disease is especially dangerous - complications during childbirth can also appear in the baby.
The main problem for doctors is that not all medications prescribed for therapy can treat thrush during pregnancy.
The basic principle of treating a mycotic infection in a “specific” population is the choice of medication that is most gentle for the health of the mother and child.
If systemic assistance is needed, if a severe stage is diagnosed, the use of tablets is indicated. Gynecologists mainly prescribe Terzhinan vaginal tablets. The instructions indicate that they can be taken during pregnancy, they do not have a teratogenic effect, and are well tolerated by expectant mothers. Terzhinan contains the active component ternidazole, as well as neomycin sulfate, nystatin and prednisolone.
Thanks to its unique composition, Terzhinan has a strong antimycotic effect and helps restore the surface of the mucous membrane. It is noteworthy that Terzhinan can also cure gardnerellosis, which often worsens due to hormonal imbalance.
Using Terzhinan is not difficult - one tablet of the drug needs to be moistened in water and inserted into the vagina, then it is recommended to lie down for about 15 minutes until the tablet dissolves. The duration of taking Terzhinan will be determined by the doctor, observing the dynamics of the situation, but on average it is 10 days.
It is also sometimes recommended to take the following tablets - Nystatin, Pimafucin.
For mild cases, doctors prescribe Clotrimazole 500 mg suppositories once - in most cases, the medication at this dosage successfully copes with entire albicans colonies.
Pimafucin is effective. The active chemical compound is natamycin. Pimafucin has a pronounced antifungal effect; the drug is capable of damaging the cell walls of pathogens, which leads to their death. It is noteworthy that to date, albicans have not yet developed resistance to Pimafucin, and it is relevant for helping patients expecting a new addition to the family. Treat with suppositories for 3 to 6 days (1 at night).
Experts also recommend Livarol. The active substance of the drug is ketoconazole. Livarol actively changes the lipid structure of the albicans cell membrane, after which death occurs. Suppositories are used for both acute and recurrent forms. Use one piece at night; it is recommended to use Livarol for three to five days. If the infection is in advanced form, the suppositories are extended for five days. Zalain has a similar effect, so it is also prescribed to eliminate discomfort on the surface of the mucosa.
After the disease has been cured with antifungal medications, Hexicon suppositories are recommended for prevention. They do not affect the causative agents of dysbacteriosis, but are able to ensure the cleanliness of the genital mucosa for a long time, right up to the birth of the baby.
Cream-like forms for candidiasis are very popular - these inexpensive analogues give no less positive effect, and they are much more convenient to use.
Manufacturers of many brands produce the medicine not in one form, but in several - in the form of an ointment or gel. Before purchasing a prescribed medication, you can ask the pharmacy if it is available in a creamy form. The drug Miramistin, for example, is available in the form of an ointment and a spray - the choice is up to the patient.
The following names are actively purchased in the pharmacy - Pimafucin, Dalatsin-cream, Polygynax, Neo-Penotran, Ketoconazole, Clotrimazole, Nystatin and other antimycotic suppositories and ointments.
Medicine is sensitive to the treatment of pregnant women, and the most useful and effective folk remedies are selected for this contingent.
A good way to get rid of the cause of dysbiosis in any period is tampons with honey. For preparation, you need to purchase real fresh honey, not candied. A small tampon is rolled out of gauze, but you can also use hygienic tampons of the smallest size. The tampon is dipped in honey and inserted into the vagina in a supine position, but not deeply. You need to soak with honey for several hours. The procedure is repeated the next day and so on for 5-7 days, depending on the severity of the disease. Severe thrush goes away in 10 days.
Good reviews are left after using sodium bicarbonate. Soda will not harm the fetus at all, so it is approved as a solution for local treatment of the genitals. It’s easy to prepare a soda solution - you need to add 20 g of soda per liter of warm boiled water, and to soften the liquid you can also dissolve a little sea salt in the water. The resulting medicine is recommended to be used as baths. This is possible in the first 6 months of the “interesting situation”, when the stomach is not yet large. Stay in the baths - up to 20-25 minutes, course - no more than 7-10 days.
At the end of the second and third period, when it is difficult for a woman to take baths, washing with soda will be useful.
Treatment of thrush during pregnancy largely depends on how far along the woman is. We will analyze the methods and specifics of therapy by trimester.
Thrush during pregnancy in the 1st trimester is treated with a limited number of medications, since not all medications are allowed to be taken during this period. Doctors prefer to treat with the safest drug Pimafucin.
It does not have a teratogenic effect on the fetus. During the period of using Pimafucin, vitamin preparations are prescribed to help boost immunity so that the problem does not return in the future.
If an infection is detected in the first 3 months, help should not be delayed. You need to be treated for a week, maximum ten days. During this period, itching and discomfort can be eliminated and the baby can be protected from the spread of the disease. After complete recovery, partners are allowed to have sex.
The infection activates in the second trimester much less frequently than in the first, because hormones have already stabilized, although immunity is still not high enough.
The developing fetus ceases to dictate conditions to doctors - in case of vaginal dysbiosis, a prescription is given even for medications prohibited in the first three months. Thrush during pregnancy in the 2nd trimester is treated with the drugs Nystatin, Terzhinan, Betadine, Clotrimazole, Livarol, Pimafucin remains popular.
The 3rd trimester of pregnancy is special for both mother and baby. The fungus in the last week carries a high risk of giving birth to a fetus affected by the infection. Patients in the third trimester risk being left with ruptures after childbirth, since the areas of the birth canal affected by infection do not stretch during the passage of the fetus, and it is in those places that women in labor experience damage to the intimate area.
Stitching up tears is not a pleasant sensation, so it is better to protect yourself in every possible way from such a nuisance. The disease can be treated, as before, at home - Clotrimazole, Pimafucin or Ketoconazole ointment are used to get rid of unpleasant symptoms.
If the fungal pathology does not go away during this time, gynecologists prefer to preserve the manifestations during childbirth and breastfeeding.
In the future, when a woman is allowed to take all medications, doctors insist on using stronger drugs, and in some cases they use hardware methods to treat the disease. Women should not do this while expecting a baby, but after giving birth, all methods of combating pathology will become available.
For the purpose of prevention, doctors conduct conversations with women, placing special emphasis on the health of both sexual partners. Dysbacteriosis of the mucous membrane will no longer appear if you normalize your diet, increase your immunity, and take vitamins.
In order for thrush to be cured during pregnancy, treatment must be carried out completely and completely, without stopping medications on your own. It is very important to eliminate all diseases at the initial stage so that you do not have to use antibiotics - it is after them that the disease worsens than ever.
If you treat vaginal dysbiosis correctly, it will go away quickly. However, the fungus candida albicans continues to live in the patient’s body, and this threatens a new exacerbation. The most important thing in this case is careful prevention of fungal infections.
Based on materials from lechenie-molochnicy.info
Traditional treatment
In addition to choosing the drug, the doctor must also prescribe the period for its use. For some, 3-5 days will be enough, while others will need at least two weeks.
The doctor prescribes the dosage and duration of treatment after an examination (examination + smear for flora): the more severely a woman is infected, the longer it will take to be treated.
If the prescribed drug is not suitable - the symptoms intensify, the burning and itching increases - there is no need to torment the body. You need to contact your doctor again so that he can select another remedy, taking into account the patient’s individual intolerance to certain components.
Treatment of thrush in early pregnancy
The first 12 weeks are the most risky.
If possible, it is better to postpone treatment of candidiasis for a month or two, so as not to provoke a miscarriage. Only if a woman experiences a strong burning sensation should the doctor choose the most non-toxic drug possible. Most often in this case, Pimafucin is chosen - in the form of suppositories or cream.
At this time, it is better for a woman to abstain from sexual intercourse to prevent re-infection. And diversify your diet with vegetables and fruits, excluding sweets and baked goods. This will help keep the infection under control, and at the same time improve your general condition, replenish the lack of vitamins, and prevent rapid weight gain.
If there are no contraindications, you can increase the amount of fluid. Just give up tea, coffee, sweet juices in favor of plain water.
Features of therapy in the 2nd and 3rd trimesters
At this time, the restrictions are not so strict, and you can use all drugs allowed for pregnant women.
At this time, you can use drugs to normalize the vaginal microflora to prevent the recurrence of the disease before childbirth.
A course of treatment does not guarantee that the infection will not return before the end of pregnancy. Therefore, it is important to adhere to hygiene standards, proper nutrition, and strengthen the immune system.
Recurrence of thrush is a direct path to the chronic form. Repeated use of the same drug leads to the formation of resistance in the pathogen, so with each exacerbation it will be more difficult to treat.
Often, doctors advise women to undergo treatment for thrush in the last weeks before giving birth to prevent the baby from becoming infected.
Babies and candidiasis
On average, candidiasis accounts for 15-30% of the total number of all infectious diseases of newborns . And in more than half of such cases, it is detected in the later stages, and this significantly complicates the treatment of the expectant mother.
Currently reading: Fetal hypotrophy during pregnancy. Causes, signs, treatment
There can be several causes of candidiasis . First of all, the mother’s infection in the last two trimesters of pregnancy and during childbirth, as well as elevated blood sugar levels in the expectant mother.
An important role is played by the fact that if the baby was born prematurely , this increases the risk of infection with a fungus of the genus Candida, especially if he undergoes such manipulations as resuscitation or ventilation. Babies born prematurely, as a rule, have reduced immunity, which leaves them defenseless against this disease.
Candidiasis in infants is classified into several types:
- Congenital. It appears in the first 3 days of life, and the cause of which was intrauterine infection.
- Acquired. A consequence of certain manipulations or possible damage to the skin, mucous membranes, etc. It usually appears 8-10 days after birth.
People's Councils
The first thing you should pay attention to is nutrition and drinking regimen: you should exclude sweet and spicy foods, consume more fiber and clean water.
Herbal baths
Warm (not hot) local baths with herbs and antibacterial mixtures - chamomile, nettle, oak bark, sage, yarrow - help. 1-2 tablespoons of herbs are poured into a liter of water, brought to a boil, infused and filtered.
Baking soda
Since the fungus multiplies in an acidic environment, it is necessary to create conditions unsuitable for life - to increase the alkaline level. For this, soda baths are used - ordinary baking soda is dissolved in warm boiled water.
Douching during pregnancy (especially without a doctor’s recommendation) is not advisable. Even before using methods that helped your mothers and grandmothers, it is better to consult a specialist.
Tea tree oil
Tampons soaked in tea tree oil, a powerful antiseptic, are also used. Although essential oils are contraindicated for pregnant women, they are the only ones that do not cause allergies or side effects.
Prevention
To prevent illness, a woman, even before planning a pregnancy, needs to be screened for infections, treated for them, and also choose her own strategy for supporting the immune system.
To prevent exacerbation of the disease in pregnant women, it is necessary:
- Follow a diet.
- Follow the rules of personal hygiene for pregnant women.
- Get more rest and avoid any stress.
- The sexual partner must use condoms!
Do not try to cure thrush on your own : if any symptom appears, rush to the gynecologist. Full compliance with the doctor’s recommendations will guarantee the mother’s successful recovery and the birth of a healthy child.