Types of Herpes
What kind of disease is this? It is caused by herpes viruses type 1 (HSV-1, or herpes labialis) and type 2 (HSV-2, or genital herpes).
- Type 1 herpes causes sores around the mouth and lips (blisters, popularly known as cold sores);
- Herpes type 2 - ulcers in the genital area or rectum, sometimes in other places, but always below the waist.
These blisters burst over time, leaving behind painful ulcers that heal from 2 to 4 weeks (they take the longest to heal in people who have the virus for the first time). Even after the blisters and sores have passed, the virus still remains in the body and can manifest itself at any time - the same bubbles will appear in the same places.
Herpes of the lips can be transmitted by kissing, through airborne droplets and through household contact.
Genital is transmitted through unprotected sex and is less common, but still every 5th adult is infected with genital herpes, and most people do not even know about it - this type is often asymptomatic or its symptoms can be mistaken for manifestations of any another disease.
Diagnosis of herpes
A reliable method for diagnosing herpes virus types 2 and 1 is ELISA (enzyme-linked immunosorbent assay). Using this method, protective antibodies are detected - immunoglobulins of class G and M, which circulate in the blood of a sick person. After a pregnant woman becomes infected, Ig M appears in her blood, and a little later, after a few weeks, Ig G (after relapse of the disease or primary infection). The ELISA reaction can be qualitative and quantitative. In this case, a qualitative reaction is determined by the presence of Ig G or Ig M antibodies to the herpes virus, and a quantitative reaction reveals its immunoglobulin titer (their number).
A qualitative reaction reliably establishes the type of virus (HSV 1 or 2), and also determines whether the patient has immunity to herpes infection. Using a quantitative reaction, the state of a woman’s immunity to the herpes virus is assessed. If there is a high titer of antibodies in the blood, this indicates a relapse of the disease.
There are other methods for diagnosing herpes: virological culture (material - the contents of vesicular rashes), PCR (polymerase chain reaction) - detection of viral DNA. Herpes zoster is diagnosed based on symptoms and clinical manifestations, which, as a rule, do not raise doubts. Laboratory diagnostic methods include: microscopy, immunofluorescence method, cultural and serological diagnostics.
Herpes during pregnancy
Herpes often manifests itself during pregnancy, when a woman’s immunity is significantly reduced. By the way, this happens not because the body “weakens,” but to preserve and bear the fetus, which is essentially a foreign object for the mother’s body and, if the mother’s immune system were working at full strength, it would simply be rejected.
A decrease in immunity during pregnancy is simply necessary, but from the point of view of exacerbation, this is a very favorable moment.
If a woman has noticed rashes on her lips, nose, facial skin or mucous membrane of the genital organs, the doctor will definitely prescribe an additional examination to identify what type of virus has entered her body.
Simple herpes is not so terrible, while genital herpes during pregnancy can cause serious complications, which will be discussed later.
A test for herpes during pregnancy is either a tissue sample taken from the affected area or, more commonly, a blood test.
Genital
One of the most dangerous types of virus during pregnancy.
Causes:
- domestic infection;
- infection through unprotected sexual contact;
- infection during childbirth (from mother to child).
Herpes is often accompanied by other infectious diseases of the genital tract: mycoplasmosis, chlamydia, trichomoniasis, gonorrhea, syphilis, therefore, if a genital-type virus is detected in the body, it is necessary to undergo examination to identify sexually transmitted infections.
Symptoms of herpes infection during pregnancy:
- Vaginal discharge is slight, watery, lasting 5–7 days (sometimes in pregnant women this is the only symptom of this pathology).
- Rashes on the skin of the external genitalia, as well as on the walls of the vagina and the lining of the cervix. These rashes resemble small blisters filled with clear liquid, which burst after 2–3 days, leaving behind ulcers that do not heal for 7–10 days, and sometimes this period reaches 2 weeks;
- Itching, burning sensation - often appear before the rash itself and serve as its harbingers.
- Muscle pain, headache, general malaise and weakness, increased body temperature to 38–39 °C.
Simple
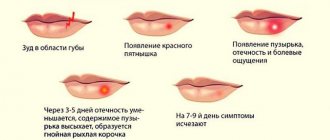
Labial, or herpes simplex, goes through 4 stages of development. At first, itching or discomfort appears in the area of the lips, nose or other parts of the face, and possibly general malaise and even fever.
The second stage is inflammation, characterized by slight swelling and soreness of the lips, which expands over time and occupies a larger surface.
At the third stage, the bubbles burst, a clear liquid flows out of them, containing many viral embryos, and therefore dangerous in terms of infection. In place of the burst bubbles, wounds form.
The fourth stage is characterized by the formation of scabs (crusts) at the site of the wounds. If you touch them with your finger, they cause pain and sometimes slight bleeding.
Herpes zoster
Herpes zoster is especially dangerous during pregnancy (synonym: herpes zoster - causes). This is also a disease of viral etiology, which is characterized by unilateral skin rashes that mimic herpes. As the rash progresses, severe pain is noted, due to the fact that the virus lives in nerve cells. Herpes zoster is caused by the chickenpox virus; it can live in the body for a long time without causing any symptoms, and then suddenly become active when the immune system is weakened. (see signs of chickenpox in adults, herpes zoster - symptoms, treatment)
Herpes zoster can have different forms: ophthalmological, Ramsay-Hunt syndrome, motor. There are also atypical forms of the disease: cystic, abortive, gangrenous, hemorrhagic.
Depending on the form of the disease, its symptoms may be different, but in all cases rashes appear, which are located along large nerve trunks and nerves (intercostal nerves, trigeminal nerve, etc.) and have a unilateral (asymmetrical) nature of the lesion. In the area of the rash there is severe itching of the skin. General symptoms also appear - malaise, increased body temperature. Later, neuralgic pain appears in the areas where the rashes are located. (see herpes on the body, treatment, symptoms)
Initially, pink spots are visible on the skin, against which, after a few days, erythematous papules and blisters with serous contents appear. As the nature of the rash changes, nearby lymph nodes enlarge and pain along the nerves increases sharply. After about a week, the burst blisters dry out and crusts form in their place, which fall off over time, leaving behind pigmented areas of skin. After the patient's rash and other manifestations of the disease have disappeared, he may still have pain along the nerves (postherpetic neuralgia), which is difficult to treat.
Is herpes dangerous during pregnancy?
If a woman had herpes before pregnancy or was a carrier, then the child can be said to be lucky: he is protected by maternal antibodies, so the pregnancy prognosis is quite favorable - the probability of infection of the fetus is only 5–7%.
The situation is worse if the expectant mother became infected during pregnancy. The likelihood of the baby becoming infected in this case increases to 50–60%. Will the fetus become infected? Here it’s like in Russian roulette: maybe yes, maybe not.
If the virus nevertheless enters the baby’s body through the placenta, this can negatively affect his health and the course of pregnancy.
If herpes enters the child's body in the early stages of pregnancy, the risk of miscarriage increases.
But even in the case of successful gestation, this insidious virus can manifest itself in another area, causing a wide variety of malformations and defects in fetal development:
- visual and hearing impairments,
- congenital brain defects,
- damage to the central nervous system,
- deviations in the physical development of the baby.
Therefore, herpes in the early stages of pregnancy becomes an indication for its termination. It makes sense to continue the pregnancy only if the infection occurs after the sixth month, but not everything is smooth here either. If infection with the virus occurs in the third trimester of pregnancy, this can cause the birth of a stillborn baby or a baby with brain damage.
Genital herpes during pregnancy is much more dangerous - it is what leads to the most serious complications. However, this is not a death sentence: if shortly before giving birth there is an exacerbation of genital herpes, doctors, in order to avoid infecting the child when passing through the birth canal (and this risk is very high), will most likely suggest a cesarean section.
Some gynecologists and obstetricians still practice delivery without cesarean section, naturally - for this, emergency treatment is used with the help of special medications. These are powerful medications, but if your doctor has prescribed them, don't worry—the prospect of contracting a virus will do much more harm to your baby than taking “harmful” medications.
Possible consequences of herpes contracted during pregnancy:
- For the fetus - miscarriages, frozen pregnancy, brain damage (microcephaly), congenital developmental anomalies, heart defects, congenital viral pneumonia, premature birth.
- For a newborn baby - sudden death of a child after birth, epilepsy, cerebral palsy, deafness, blindness.
Cases of such terrible consequences are rare, but the doctor will definitely prescribe a course of treatment for you to eliminate the slightest possibility of any complications.
Ways of transmission of herpes
Infection with labial herpes HSV-1 is carried out through household contact or airborne droplets (kissing with a sick person, contact with infected areas of skin, through the personal belongings of a sick person - dishes, towels, washcloths, toothbrushes, cosmetics).
A pregnant woman can become infected with genital herpes (HSV-2) through sexual intercourse. In 50% of cases, infection occurs when the virus is in an asymptomatic active phase, and the sick person has minor unpleasant sensations - burning, pain, small rashes. When a pregnant woman is initially infected with genital herpes, the risk of infection of the fetus is about 50–60%.
The HSV-2 virus can also be transmitted vertically from a pregnant mother to her fetus through the placenta or during childbirth through contact with the mother's birth canal infected with herpes.
Infection of the population with the herpes simplex virus is very high. Therefore, the problem of the influence of herpes on pregnancy is primarily a problem that directly depends on the state of immunity of the expectant mother
Treatment
If you noticed blistering rashes before pregnancy, be sure to tell your obstetrician-gynecologist about it. If during pregnancy you notice a relapse or an exacerbation of the disease, consult a doctor as soon as possible - the sooner medical measures are taken, the greater the chances of successfully maintaining the pregnancy.
There is no universal medicine that could get rid of this disease once and for all. Therefore, doctors can take measures to suppress the activity of the virus or boost immunity.
If the diagnosis shows immune deficiency, immunoglobulins are used as treatment, which are not contraindicated for pregnant women - ginseng, eleutherococcus, echinacea, B vitamins.
Treatment of herpes in a pregnant woman is complicated by the fact that many of the known effective drugs cannot be used during this period. Most likely, the doctor will prescribe you one of the many ointments, which will need to be applied to the affected surface 5 times a day for 7-10 days. It is also sometimes recommended to lubricate rashes with an interferon solution or vitamin E (sold in capsules) - they help speed up the healing of painful ulcers.
Medications
Treatment of herpes during pregnancy should be carried out only under the supervision of a doctor. Using medications on your own is dangerous. The specialist prescribes such medications based on the benefits and risks for both the baby and the mother herself.
The most common medications for treating the herpes virus include a group of antiviral drugs. Immunomodulators may also be indicated for complex therapy and prevention of disease relapse.
Antiviral agents
Antiviral drugs are used only as prescribed by a doctor and, most often, in external form. This form is the safest and is not capable of affecting the fetus. These drugs include medications that contain acyclovir.
Valaciclovir or famciclovir may also be indicated. However, the effectiveness and safety of the latter two drugs in the treatment of herpes in pregnant women has not been fully studied.
Widely used purpose:
- Acyclovir.
- Panavira.
- Herpevira.
- Zovirax.
- Fenistil pencivir 1%.
Acyclovir, Gerpevir, Zovirax
Drugs that contain acyclovir are produced in different dosage forms under different trade names. The mechanism of action is based on the direct effect of the drug on the DNA of viral particles.
Thus, the virus is unable to reproduce itself and dies. A special feature of the drug is that the cell affected by the virus practically does not suffer after the action of the drug.
The main indications for the use of acyclovir during pregnancy are:
- herpes on the lips;
- herpetic sore throat;
- stomatitis;
- dermatitis;
- herpes of the genital organs (the drug for this diagnosis is indicated only in the second or third trimester);
- chickenpox.
As a rule, the prescription of medication is justified only in moderate or severe cases, when the virus causes inconvenience to a pregnant woman or poses a threat to the baby in the womb.
Effects after taking Acyclovir:
- Reducing the spread of rash throughout the body.
- Fast crust formation.
- Healing damaged skin.
- Reducing the risk of spreading the virus both to the baby in the womb and to others.
The main contraindication is hypersensitivity to the drug, as well as kidney or liver pathology.
Side effects include:
- nausea, vomiting;
- allergic dermatitis, skin itching, allergic rash;
- abdominal pain, headaches, drowsiness, dizziness.
Panavir
An effective and safe medicine with antiviral action. The drug contains herbal components, the complex effect of which can strengthen the immune system and help quickly cope with opportunistic microflora.
The composition includes extract of potato tops shoots. This component is found in all forms of release of Panavir.
Panavir, regardless of its release form, is capable of providing:
- anti-inflammatory;
- wound healing;
- pain reliever;
- immunomodulatory and antipyretic effects.
In the early stages, the drug is safest in injection form. With its help, it is possible to treat various types of herpes virus, as well as the virus in the fetus. In addition, indications include papilloma virus, viral dermatosis, influenza, tick-borne encephalitis and others.
Contraindications:
- serious kidney pathologies;
- hypersensitivity.
As a rule, the medicine does not cause side effects and is well tolerated. In some cases, allergic reactions may develop.
Fenistil pencivir 1%
Fenistil is a medicine whose main ability is to suppress allergic reactions in the patient. At the same time, the medicine copes well with various skin rashes, relieves itching, swelling and redness. However, for the treatment of herpes during pregnancy, it is Fenistil Pencivir, which contains the antiviral component penciclovir, that is used.
The action of this substance is aimed at destroying and blocking the development of viruses of types 1 and 2. With its help, it is possible to prevent or eliminate the acute course of the disease and reduce the risk of transmission of herpes infection.
Fenistil pencivir is used only externally to treat various types of herpes on the lips.
Side effects can be observed in the form of burning, tingling at the site of application. There were no cases of overdose.
Immunomodulators
This group of drugs is used for complex treatment. Preference is given to herbal components, which are recommended to be consumed with vitamin complexes.
Such means include:
- Eleutherococcus extract;
- ginseng extract;
- rosea radiola extract;
- echinacea extract.
You can take herbal ingredients only after your doctor's permission. The danger of self-medication is that during pregnancy a woman’s sensitivity to various plant components increases. Therefore, it is better to take extracts after consulting your doctor.
Folk remedies
Traditional medicine recommends lubricating the affected area with fir, sea buckthorn or rosehip oil (this therapy lasts 2-3 weeks), chamomile cream, calendula ointment, and also drinking plenty of hot drinks that boost immunity - for example, tea with honey and viburnum.
This is not to say that these remedies are useless, but on their own they are ineffective, since they only affect the symptoms of the disease, and not the virus itself. It is better to use them in combination with medications prescribed by a doctor.
Effect on the child’s body
Herpes is an unpredictable disease, no one can tell you exactly when it will occur, why and what consequences it will bring, but even herpes on the lips in early pregnancy can be fatal for the child. More details about this disease can be found here. Depending on the type of disease, the mother’s immunity and the age of the fetus, herpes during pregnancy can lead to the following consequences:
- Heart defect in a child;
- Delayed physical and emotional development;
- Jaundice for a long time and consequences after it;
- Possibility of external or internal bleeding;
- Lack of hearing, vision;
- Dumbness;
- Frequent seizures of epilepsy, etc.
As you can see, the options for diseases in a child are quite high, not to mention the death of the baby. Remember that preparation for childbirth should include not only the purchase of everything necessary for the child, but also constant monitoring of your condition. Remember that during gestation the body will react to everything that could interfere with the child’s normal development, and therefore this will not cause you much difficulty. If you know that you are prone to herpes, be careful and listen to your body.
Prevention of herpes during pregnancy
There are a number of measures that allow you, although not with a 100% guarantee, to protect yourself from infection with the herpes virus, but, if possible, to prevent it:
- strengthening the body’s immune forces is not only taking immunostimulants, but also a healthy lifestyle, proper physical activity, balanced nutrition, and hardening;
- giving up all bad habits;
- a blood test for the virus before pregnancy, during the planning period of conception.
All these measures are aimed only at strengthening the body’s immune defense and have an indirect, preventive value.
If rashes torment you quite often, it is recommended to take a course of multivitamins or immunomodulatory drugs before conceiving a child. There is also a special procedure - intravascular irradiation of blood using a laser. True, even this is not capable of killing the virus completely, but its activity will still be suppressed. This procedure is now offered by many clinics.
If you are not infected with the virus, be especially careful about sanitary precautions: direct prevention of herpes infection is avoiding contact with infected people.
Pregnancy after herpes
Many mothers are wondering what to do during pregnancy and how to react if they are pregnant after having herpes. This question remains relevant today, since no one knows the exact answer.
The variants differ from each other depending on the time of infection. So, if at the time of conception one of the parents had herpes, there is a high probability that the child would be infected with this virus. Especially when it comes to genital manifestations. Subsequently, this can be considered as full-fledged herpes during pregnancy, although in fact it appeared earlier. Even if at the time of conception the herpes has practically disappeared, you should still be extremely careful, because even the absence of an external manifestation does not guarantee the fact that the virus has disappeared from the body. If the last rash occurred long before conception, parents should not worry that it could somehow be passed on to the child. The main thing is to protect yourself in the future so that there are no manifestations during pregnancy. Remember that the attending physician must know about your disease in order to pay attention to it during examinations and take appropriate measures at the first manifestations.
What is the danger of infecting a child with genital herpes during childbirth?
The presence of this form of pathology in the mother leads to an increased risk of infection of the unborn baby during childbirth. Penetration of pathogenic microorganisms occurs in different ways: through the cervical canal from the vagina, the placenta, and through the fallopian tubes. There is a chance of infecting the baby during childbirth, when it passes through the vagina and comes into close contact with the diseased areas of the mucous membranes. The main consequences of infection during childbirth appear after 13-16 days.
The mildest form of manifestation will be the appearance of painful blisters on the skin and mucous membranes. Occurs in 20-40% of cases. Visually, the bubbles are about 2 m in diameter, filled with translucent liquid, and can appear on any part of the body without signs of an inflammatory reaction. Over time, they burst and heal completely within 2 weeks. Against the background of these symptoms, the baby may develop ophthalmological diseases:
- uveitis;
- herpetic keratoconjunctivitis;
- iridocyclitis;
- chorioretinitis;
- corneal erosion.
Prevention
To eliminate the likelihood of premature birth and deformity as a result of the influence of the virus on the development of the fetus, it is necessary to carry out all preventive actions before pregnancy. According to doctors, these simple rules help to significantly reduce the risk of transmission of the virus from mother to fetus during pregnancy and childbirth:
- give up bad habits;
- strengthen your immune system: exercise, a healthy lifestyle, hardening, proper nutrition;
- undergo a timely HSV test before planning a pregnancy, and not after conception.
If the expectant mother is diagnosed with a recurrent type of pathology, then before conception she should undergo therapy with immunomodulators and multivitamins. A course of laser treatment will be required to reduce the activity of the virus as much as possible. It is necessary to limit contact as much as possible with people who often suffer from exacerbation of herpes infection.
What is herpes and how is it transmitted?
Herpes is an extremely common viral infection.
The herpes virus rarely causes serious illness in adults, and the infection is most dangerous for pregnant women. Having entered the fetal body during pregnancy or during childbirth, the herpes simplex virus can cause serious consequences in newborns. There are 2 types of herpes simplex virus:
- Herpes simplex virus type 1 (HSV 1, HSV 1) typically causes painful blistering rashes on the lips (cold sores). Infection with herpes type 1 usually occurs in childhood and adolescence, through contact with the saliva of an infected person (for example, when sharing dishes, kissing, etc.)
- Herpes simplex virus type 2 (HSV 2, HSV 2) most often causes painful rashes on the genitals (genital or genital herpes). Infection with herpes type 2 occurs through sexual contact. This is one of the most common sexually transmitted infections.
Both types of herpes simplex virus can pose a threat to an unborn baby. However, type 2 herpes during pregnancy is more dangerous: it causes severe consequences 3 times more often than type 1 herpes.
Why is herpes dangerous during pregnancy?
The herpes virus during pregnancy can cause serious consequences for the unborn child: for example, herpes in the early stages of pregnancy can lead to frozen pregnancy and miscarriage. If the fetus survives, intrauterine infection with this virus can cause the following consequences:
- Skin rashes in a newborn
- Eye damage
- Brain underdevelopment
- Convulsions
- Delayed physical and mental development
If a herpes infection occurs during childbirth, the following complications may occur:
- The appearance of rashes on the skin or mouth, damage to the eyes
- Inflammation of the brain (encephalitis)
- Disseminated herpes infection, which leads to the death of the child in 80% of cases.
Herpes and pregnancy planning
If you are just planning a pregnancy, your doctor may recommend testing for herpes. Tests for herpes are included in the complex of examinations for TORCH infections: these are the four most dangerous infections during pregnancy (toxoplasmosis, cytomegalovirus, rubella and herpes). Knowing in advance whether you are immune to these diseases, your doctor will make recommendations that can protect you and your unborn child from serious consequences. It is recommended that you, as well as the future father of the child, be tested for the herpes simplex virus.
Diagnosis of herpes infection at the stage of pregnancy planning includes blood tests for antibodies to herpes simplex viruses type 1 and 2. Only a doctor can decipher the test results, but we will try to give basic clues to deciphering the results obtained:
- IgG antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - negative
- IgM antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - negative
You are currently healthy and there is no herpes simplex virus in your body. This infection does not threaten future pregnancies, but you should take every precaution to avoid contracting herpes during pregnancy. See recommendations for preventing herpes during pregnancy at the end of this article.
- IgG antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - positive
- IgM antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - negative
There is a herpes virus in your body and you are immune to this infection. You can start planning your pregnancy. There is a risk that you will infect your unborn child with herpes during pregnancy or childbirth, but it is very small and amounts to no more than 3%.
- IgG antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - negative
- IgM antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - positive
A positive IgM for herpes means that you have recently become infected and have not yet developed strong immunity to this infection. You should postpone planning a pregnancy for a while and consult an infectious disease doctor. Your doctor may prescribe antiviral treatment.
- IgG antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - positive
- IgM antibodies to herpes simplex virus types 1 and 2 (HSV 1/2 or HSV 1/2) - positive
Either you became infected with herpes recently, or the infection occurred a long time ago, but at the moment the virus is activated. You should postpone planning a pregnancy for a while and consult an infectious disease doctor. Your doctor may prescribe antiviral treatment.
Herpes during pregnancy
Experiencing herpes symptoms during pregnancy can be a warning sign, so you should always tell your doctor. The herpes simplex virus can cause the following symptoms:
- Herpes on the lips during pregnancy
Herpes of the lips during pregnancy is most often caused by the herpes virus type 1, which rarely causes consequences for the unborn child.
The risk of developing complications will be extremely small if you have developed herpes on the lips not for the first time, and episodes of rashes on the lips were observed before pregnancy. This means that you already have immunity to this type of virus and it most likely will not enter the bloodstream or cross the placenta to your unborn baby.
If you have developed lip herpes for the first time during pregnancy, and you have never experienced rashes before pregnancy, then the risk of complications for the fetus will be slightly higher. In this case, you should visit a doctor and take a blood test for antibodies to herpes simplex viruses type 1 and 2. To make sure that the virus has not harmed the fetus, your doctor may order a series of repeat ultrasound examinations.
- Genital herpes during pregnancy
Genital (genital) herpes during pregnancy is manifested by the following symptoms: painful rashes in the form of blisters in the perineum, on the labia or on the mucous membranes of the vagina and cervix, pain during sex and during urination, vaginal discharge, fever, headaches etc. Genital herpes is usually caused by the herpes virus type 2, which is more likely to cause dangerous complications during pregnancy.
If you are pregnant and experience symptoms of genital herpes, you should visit your gynecologist as soon as possible. The doctor will examine you and prescribe the necessary tests to determine the risk of consequences for the unborn child.
I contracted herpes during pregnancy. What is the risk that I will pass this infection on to my unborn child?
The risk of transmission of the virus from a pregnant woman to her unborn child depends on at what stage of pregnancy the infection occurred:
- If a pregnant woman becomes infected with the herpes virus before 20 weeks of pregnancy, the risk of infection of the fetus is quite small. However, if infection does occur, the consequences can be very severe (frozen pregnancy and miscarriage).
- Infection with herpes in the 3rd trimester of pregnancy poses the greatest threat to the unborn child, since the risk of transmission of infection at this stage ranges from 30 to 50%
Infection of a child with herpes can occur in utero (during pregnancy), during childbirth, and also after childbirth. In 85-90% of cases, infection occurs during childbirth, if at this moment the woman has a rash on the genitals.
What should I do if I get herpes during pregnancy?
If you are pregnant and have symptoms of herpes, you need to visit the gynecologist who is caring for your pregnancy as soon as possible.
Possible actions of the doctor in this situation:
- If you have never been tested for antibodies to the herpes virus, your doctor will recommend this examination. With the help of an analysis, the doctor will determine whether you have immunity to the herpes virus, which means what is the risk of transmitting this infection to your unborn child.
- If you have been tested for antibodies to the herpes virus before, your doctor will review the results again and determine whether further testing is necessary or whether the risk to the unborn baby is negligible.
Treatment of herpes during pregnancy
Antiviral medications can be used to treat herpes during pregnancy:
- Acyclovir
- Valaciclovir
It should be noted that the safety of these drugs during pregnancy has not yet been adequately proven, but animal studies have shown no adverse effects on the fetus.
The dosage of the medicine and the duration of treatment are determined by the attending physician. Don't self-medicate!
Childbirth with genital herpes
Genital herpes during pregnancy poses the greatest threat to the unborn child if its symptoms first appear or worsen shortly before birth. To reduce the risk of complications, your healthcare provider may recommend prophylactic treatment with antiviral medications (such as Acyclovir) from 36 weeks of pregnancy until delivery.
If by the time labor begins you have herpetic eruptions on the genitals, then natural delivery can be extremely dangerous for the unborn child. In this case, doctors may insist on a cesarean section.
Prevention of herpes during pregnancy
If your herpes tests show that you are not immune to the virus, follow these guidelines to avoid getting herpes during pregnancy:
- Do not share your food and drinks with other people.
- Do not finish eating or drinking other people's food or drinks.
- Use separate containers from which only you will eat or drink. This is especially important if someone in your household has symptoms of herpes on the lips.
- Avoid close contact with people who have symptoms of herpes on the lips: do not kiss them or share utensils.
- If your partner (husband) has ever had symptoms of genital herpes, or if his herpes tests showed that he is infected with HSV type 1 or 2, refuse sex for the entire duration of pregnancy, or use condoms during sex. This is especially important if the partner’s genital herpes is in the acute stage.
- If your partner has ever had herpes on the lips, then avoid oral sex (cunnilingus) in the third trimester of pregnancy.
Types of herpes
There are different types of this pathogen, which provoke diseases with different symptoms. A person currently has a risk of becoming infected with one of 8 types of pathology:
- Simple type 1 - manifests itself, as a rule, in the form of blisters on the lips.
- Simple type 2 – causes a genital form of pathology during pregnancy.
- The chickenpox virus causes herpes zoster and chickenpox.
- Virus type 4 or Epstein-Barr. Becomes the cause of the development of infectious mononucleosis.
- Cytomegalovirus becomes a consequence of infection with the 5th type of HSV.
- When type 6 penetrates the body, tumor processes and lymphoproliferative diseases can begin.
- Chronic fatigue syndrome develops when infected with type 7 of the virus.
- In the presence of AIDS, type 8 can cause Kaposi's sarcoma.
Symptoms
Chronic pathology, primary genital herpes in pregnant women have similar manifestations. The main external symptoms of this type of pathology include the following:
- pain, swelling in the intimate area;
- blistering rashes on the outer genitalia;
- if the vagina is affected, painful sensations appear in the lower abdomen;
- light, copious vaginal discharge;
- frequent and painful urination;
- body temperature rises to 38 degrees;
- general health worsens.
Increasingly, in medical practice, cases of an erased (atypical) course of genital HSV are noted. The main and only symptoms of the disease are burning, itching in the labia majora and minora, light discharge, and a slight increase in body temperature. The acute period usually lasts about 10-12 days. After the rash, erosions remain, which gradually crust over and heal.