Massive hemoptysis - the release of more than 400 ml of blood in 3 hours. Its most common causes are bronchiectasis, bronchial carcinoma, infectious diseases (for example, tuberculosis, lung abscess or aspergillosis) and trauma.
Often the reason becomes clear after clarifying the anamnesis. In patients with pulmonary hemorrhage, its location can be determined by a characteristic “gurgling” sound heard on auscultation. Find out whether the patient smokes and takes any medications.
The patient is examined to identify the disease causing the bleeding and to assess the hemodynamic and respiratory response to the bleeding.
It should be remembered that the source of bleeding can be not only the lungs, but also the upper respiratory tract, nasopharynx, and gastrointestinal tract.
Hemoptysis is the release of blood with sputum from the respiratory tract. The criterion for massive hemoptysis is the release of >600 ml of blood during the day.
Most of the blood (95%) reaches the lungs through low-pressure vessels (pulmonary arteries). About 5% of the blood circulates through high-pressure vessels (bronchial arteries), which supply the main airways and supporting structures. When hemoptysis occurs, blood comes from the bronchial arteries.
Causes of hemoptysis
Most often, hemoptysis syndrome is observed in bronchiectasis, tuberculosis, bronchitis, pneumonia, and abscess. The causes of hemoptysis can be bronchial adenoma, lung carcinoma, thromboembolism of the pulmonary artery, mitral valve stenosis. Hemoptysis is one of the main symptoms of pulmonary hypertension, pulmonary angiitis, idiopathic progressive pulmonary induration, amyloid dystrophy and hemorrhagic hemostasiopathy.
The syndrome of hemoptysis and pulmonary hemorrhage can develop when an aortic aneurysm ruptures and subsequently enters the bronchus.
With pulmonary tuberculosis, the syndrome of hemoptysis and pulmonary hemorrhage also often develops. In this case, bleeding is accompanied by pain in the chest associated with inflammation of the pleura, a prolonged dry cough of varying intensity and an increase in body temperature.
Regular and prolonged hemoptysis in smokers may indicate the presence of a tumor in the lungs.
Determining causes by symptoms
Lungs
The manifestations of different diseases can vary significantly. Lung pathologies are manifested by the following symptoms:
Symptoms of pathologies of the bronchi and trachea are:
- Tumor processes. In these cases, the first signs include increased night sweats, fatigue, weight loss, constant weakness and desire to sleep, and coughing attacks.
- In acute bronchitis, there is first a dry and then a wet cough, which may contain streaks or traces of blood. Chronic bronchitis in the acute stage is practically no different in symptoms from the acute form of the disease.
- Bronchiectasis. The patient has a prolonged cough with sputum, and calcified lymph nodes are also detected.
- The entry of foreign objects into the bronchi is manifested by difficulty breathing, lack of air, shortness of breath and bouts of severe coughing, often with blood.
Vessels
When blood vessels are damaged, the following symptoms may occur:
- Thromboembolism of the pulmonary artery. Manifestations: severe sharp pain at the beginning, decreased breathing rhythm and slow heart rate, shortness of breath.
- Venous pulmonary hypertension. Signs of this disease are: severe shortness of breath when lying down, symptoms of volume overload, and moist rales.
- Rupture of the pulmonary artery: weakening and sometimes complete absence of respiratory movements on the affected side, rapid increase in symptoms of anemia, severe chest pain, weakness.
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
Hemoptysis refers to both the coughing up of sputum mixed with blood and large volumes of blood.
Diagnosis of hemoptysis
Regular hemoptysis in patients under thirty years of age without signs of another disease indicates a bronchial adenoma. In bronchiectasis, recurrent hemoptysis is accompanied by regular discharge of purulent sputum. Severe pleural pain with hemoptysis indicates a possible myocardial infarction. A physical examination helps to establish the true cause of hemoptysis: friction noise of the serous membrane of the lungs indicates the presence of any pathology associated with damage to the membrane of the lungs (abscess pneumonia, coccidioidosis, angiitis); Local crackles indicate possible lung carcinoma. The initial examination necessarily includes a chest x-ray. But even with normal X-ray results, there remains the possibility of bronchiectasis or a neoplasm as a bleeding factor. An X-ray of the chest allows you to monitor fluid levels, which indicate an accumulation of pus or a distal tumor blocking the bronchus. Some patients are prescribed computed tomography of the chest and tracheobronchoscopy. Examination with a rigid endoscope is especially necessary in case of profuse hemoptysis.
Diagnostics
If such a symptom appears, you should contact a general practitioner, who will refer the patient to a pulmonologist, rheumatologist, gastroenterologist or other specialized specialists, depending on the suspected disease.
Carrying out bronchoscopy
After collecting complaints, questioning, and examining the patient, the doctor prescribes the following studies:
- general blood test with determination of platelet count, as well as coagulogram;
- blood biochemistry with determination of liver and kidney function indicators (bilirubin, ALT, AST, alkaline phosphatase, urea, creatinine);
- microbiological examination of sputum to identify pathogens of pneumonia, tuberculosis and other infectious diseases;
- cytological analysis of sputum to detect malignant (atypical) cells in smoking patients over 40 years of age;
- X-ray of the chest organs (diagnosis of lung cancer, effusion in the pleural cavity, pulmonary congestion, etc.);
- computed tomography (detailed image of the structures of the chest, especially useful for bronchiectasis, small tumors, fungal infections);
- tomography with contrast to identify the source of bleeding;
- bronchoscopy (examination of the respiratory tract using a flexible optical fiber).
Pulse oximetry and arterial blood gas analysis are used to determine the severity of oxygen deficiency resulting from bleeding.
Other research methods can be used:
- ECG and echocardiography for suspected heart disease or pulmonary embolism;
- angiography;
- FGDS.
Help with hemoptysis and pulmonary hemorrhage
Pulmonary hemoptysis is the release of large amounts of blood through the respiratory tract without coughing or during coughing. Without coughing, blood flows into the oral cavity from the respiratory tract in a stream. The most common causes of pulmonary hemoptysis are lung cancer and tuberculosis.
The blood released during pulmonary hemoptysis is scarlet in color, foams and does not clot. For pulmonary hemoptysis, emergency hospitalization to a medical facility is indicated.
First aid for hemoptysis is to give the person a “half-sitting” position, an elevated position, calm him down, and prohibit him from talking and moving. It is strictly forbidden to place cups on the chest, apply mustard plasters, heating pads and hot compresses. An ice pack should be placed on the affected area of the chest and the patient should be allowed to swallow small pieces of ice. The reflex spasm upon swallowing will reduce the blood supply to the blood vessels of the lungs.
What does the doctor do?
Diagnostics
Whatever the location and causes of bleeding in the respiratory system, it is very important that the attending physician initially questions
patient about the circumstances of hemoptysis:
- When did this first happen?
- How long did it last?
- How much blood was coughed up and what did it look like?
- Are there any predisposing conditions?
These and other questions help narrow down the possible causes. However, patient statements, especially regarding blood quantity, are often unreliable because the quantity is subjectively perceived to be greater than it actually is.
The doctor will draw blood to obtain important laboratory data (blood test, coagulation values, blood oxygen levels, etc.).
When it comes to locating the source of bleeding, diagnostic procedures such as radiography, bronchoscopy and HRCT (high-resolution computed tomography) are used.
Therapy
Treatment depends on the specific cause. In acute bleeding, it is important to determine the cause and stop the bleeding as soon as possible, which is often possible with the help of bronchoscopy. If not, then either surgery or targeted blockage of the vessels, called x-ray embolization, is performed.
Depending on the cause of hemoptysis, various medications are used, such as antibiotics, immunosuppressants, chemotherapy, or even surgery.
Emergency measures
If the bleeding is severe and the source of the bleeding is in the lower bronchi or lungs, it is advisable to place the patient on the side of the bleeding lung so that the uninjured lung can function freely. Transfusions may also be required, replacing lost blood volume with saline solutions or similar medications.
Anyone who sees a doctor early and is treated properly can prevent recurrence of hemoptysis.
Treatment of hemoptysis
The main goal of treating hemoptysis is to ensure normal functioning of the lungs and heart and prevent asphyxia. Treatment of hemoptysis consists of bed rest and taking medications that suppress cough - opiates (dihydroxycodeinone 5 mg four to six times a day, codeine 10-30 mg).
At the very beginning of treatment, a rigid bronchoscope is used to identify the source of bleeding, and then isolate the unaffected lung and provide its ventilation. In case of respiratory failure and massive hemoptysis (excretion of about 0.6 liters of blood over two days), resulting from blood entering the respiratory tract, aspiration is required. To isolate the damaged area of the lung, a special tube with an inflated balloon is inserted to carry out the lung incubation procedure. Taking into account the location of the source of bleeding and the state of the patient’s respiratory function, a classic or surgical method of treating hemoptysis is chosen. Resection of the affected area of the lung cannot be performed in case of inoperable cancer and expected severe impairment of external respiratory function. In cases of significant impairment of pulmonary function, catheterization and embolization of the bronchial artery are performed. In this case, before the procedure, the bleeding area is tamponed with a balloon catheter, lavage is performed with fibrinogen solution or saline, and vasopressin is administered intravenously.
For massive and submassive hemoptysis, angiography is used, which includes selective embolization of the bronchial artery. The angiography method allows you to save a significant amount of lung tissue. This method is used for chronic lung diseases in patients.
Video from YouTube on the topic of the article:
Causes of hemoptysis
Sputum streaked with blood occurs in many respiratory diseases, for example, ARVI and viral bronchitis.
Differential diagnosis includes a large number of nosologies.
In adults, the causes of hemoptysis in 70-90% of cases are:
- Bronchitis.
- Bronchiectasis.
- Tuberculosis.
- Necrotizing pneumonia.
Primary lung cancer is the leading cause in smokers >40 years of age, but metastases rarely cause hemoptysis. The cause of hemoptysis is increasingly becoming an aspergillus infection with the formation of cavities, but less often than lung cancer.
In children, the main causes of hemoptysis are:
- Lower respiratory tract infections.
- Foreign body aspiration.
Massive hemoptysis. Main reasons:
- Bronchogenic carcinoma.
- Bronchiectasis.
- Tuberculosis and other types of pneumonia.
Common causes of hemoptysis
- Bronchostatic disease (with or without infection).
- Bronchial carcinoma.
- Infectious diseases.
- Tuberculosis.
- Pneumonia.
- Lung abscess.
- Aspergilloma.
- Bronchitis.
- Injury.
- Arteriovenous malformation.
- Pulmonary embolism.
- Mitral stenosis.
- Congenital heart defect.
- Aortic aneurysm.
- Microscopic polyangiitis.
Causes of hemoptysis, Source - trachea and bronchi
| Cause | Manifestations | Diagnostic algorithm |
| Tumor (bronchogenic, bronchial metastatic, Kaposi's sarcoma) | Night sweats. Weight loss, Intensive smoking. Risk factors for Kaposi's sarcoma (HIV infection) | X-ray of the chest organs. CT. Bronchoscopy |
| Bronchitis (acute or chronic) | Acute: productive or non-productive cough. Chronic: productive cough most days of the month or 3 months of the year for 2 years in a patient with COPD or a smoker | Acute: clinical examination. Chronic: chest x-ray |
| Bronchiectasis | Chronic cough and sputum production in patients with recurrent infections | High resolution CT. Bronchoscopy |
| Bronchodilators | Calcified lymph nodes in patients with a history of granulomatous disease | CT scan of the chest. Bronchoscopy |
| Foreign body (usually chronic and undiagnosed) | Chronic cough (usually in young children) in the absence of ARVI symptoms. In some cases, fever | X-ray of the chest organs. In some cases, bronchoscopy |
Causes of hemoptysis, Source - lung parenchyma
| Causes | Manifestations | Diagnostic algorithm |
| Lung abscess | Subacute fever. Cough. Night sweats. Anorexia. Weight loss | X-ray or CT scan of the chest can reveal an irregularly shaped cavity filled with air and fluid |
| Pneumonia | Fever, productive cough, shortness of breath, pleuritic pain. Decreased breathing or egophony. Leukocytosis in peripheral blood | X-ray of the chest organs. In hospitalized patients, blood and sputum cultures |
| Active tranulomatous disease (tuberculosis, fungal, parasitic infection, syphilis) or mycetoma | Fever, cough, night sweats, weight loss in patients who have had contact with infectious patients. History of immunosuppression | X-ray, CT. |
| Goodpasture's syndrome | Fatigue. Loss of body weight. Often - hematuria. Sometimes - swelling | Analysis of urine. Creatinine level. Kidney biopsy. Antibodies to the basement membrane. ANCA |
| Wegener's granulomatosis | Chronic bloody discharge from the nose, ulcers in the nasal cavity. Joint pain, skin manifestations (nodules, purpura). Thickening of the gums, granulomatous gingivitis. Saddle nose, perforation of the nasal septum. In some cases, kidney failure | Biopsy of the affected organ (kidney, skin), testing for ANCA, detection of vasculitis in small and medium-sized arteries, bronchoscopy |
| Lupus pneumonitis | Fever, cough, shortness of breath, pleuritic pain in patients with SLE | CT scan of the chest (alveolitis). In some cases, a study of bronchial lavage (lymphocytosis or granulocytosis) |
Causes of hemoptysis, Primary source in the blood vessel
| Cause | Manifestations | Diagnostic algorithm |
| Arteriovenous malformations | The presence of telangiectasia on the skin and mucous membranes or peripheral cyanosis | CT angiography. Angiopulmonography |
| Pulmonary embolism | Acute onset: acute chest pain, tachypnea, tachycardia, especially in patients with risk factors for pulmonary embolism | CT angiography or ventilation-perfusion scintigraphy. Duplex scanning of the veins of the lower extremities |
| Venous pulmonary hypertension (especially with mitral stenosis, left ventricular heart failure) | Wet wheezing. Symptoms of central and peripheral volume overload. Orthopnea or paroxysmal nocturnal dyspnea | ECG. MNE. Echocardiography |
| Aortic aneurysm with bleeding into the lung parenchyma | Back pain | X-ray of the chest organs (mediastinal widening). CT angiography |
| Pulmonary artery rupture | Recent pulmonary artery catheter insertion | Emergency CT angiography or pulmonary angiography |
Various causes of hemoptysis
| Cause | Manifestations | Diagnostic algorithm |
| Pulmonary endometriosis (hemoptysis during menstruation) | Recurrent hemoptysis during menstruation | Clinical examination In some cases, a trial of oral contraceptives |
| Systemic coagulopathy or use of anticoagulants or thrombolytics | Patients receiving systemic anticoagulants for pulmonary embolism, deep vein thrombosis, or atrial fibrillation Patients receiving thrombolytics for stroke or myocardial infarction In some cases, family history | Prothrombin time, partial activated thromboplastin time or antifactor Xa level Stopping hemoptysis when correcting coagulation disorders |
Urgent Care
First aid is necessary for massive hemoptysis (pulmonary hemorrhage). First of all, you should call an ambulance. What to do, how to provide first aid for hemoptysis before hospitalization:
- Calm the patient, give him a sitting position or lay him down so that the diseased lung is below. A person should not be laid down if the affected area is in doubt. You must remain in a sitting position until the doctors arrive.
- To reduce bleeding in the lungs, you can give the patient a piece of ice to swallow and drink cold water - this helps to narrow the blood vessels and reduce bleeding. You can repeat taking ice every 15 minutes until the doctors arrive.
- In order to reduce pain and the force of bleeding, it is very important to persuade the patient to breathe deeply, try to restrain the cough, if possible, not to speak.
Emergency medical care for hemoptysis consists of reducing the intensity of the cough, eliminating chest pain, and stopping the release of blood. As a pain reliever, you can give a solution of analgin with pipolfen. If the pain cannot be reduced and its intensity increases, narcotic drugs are administered against the pain syndrome. It is imperative to administer a drug to suppress cough (codeine, dionine), but not to completely stop it, otherwise blood will not be removed from the lungs. To reduce a strong cough reflex, promedol is usually used, but in very rare cases.
Calcium chloride is used to stop bleeding. In the absence of thromboembolism, a gelatin solution is injected into the thigh. In patients with low blood pressure, therapy with vasoconstrictor drugs is contraindicated. If this algorithm for stopping pulmonary bleeding does not help, a blood transfusion is performed after checking compatibility. Other procedures that are used to treat massive hemoptysis:
- Embolization of bronchial vessels. The procedure is otherwise called catheterization. To perform embolization using angiography, it is necessary to determine which artery is causing the bleeding. After this, a special material is injected through the catheter to block it.
- Ventilation of the lungs. Bleeding can lead to asphyxia (suffocation), so patients often require a special apparatus to support breathing. It is important to insert a special tube into the canal of the unaffected bronchus.
- Packing the site of massive hemoptysis. This reduces blood aspiration to a minimum.
The treatment of large amounts of blood pouring into the lungs due to myocardial infarction has some features. Fibrinolysin, sodium chloride, and heparin are administered. In case of circulatory failure, strophanthin, korglykon, and glucose solution are used. Painkillers and antibiotics are used. Oxygen therapy and diuretics are administered in case of left ventricular failure.
In cases where embolization is not possible and massive hemoptysis threatens shock and respiratory failure, it can be stopped through surgery. Resection of the respiratory organ is performed. In this way, it is impossible to stop hemoptysis in lung cancer and serious diffuse pathology, since removal of even a small part of the lung is contraindicated. The shock state of the pulmonary organ is difficult for resuscitation - ventilation, blood transfusion, and administration of heparin and contrical are necessary. After the critical condition has been alleviated, the patient remains in the hospital, the doctor determines the category of nursing intervention, prescribes medications for recovery, and monitors the patient.
Classification of the disease
The classification of hemoptysis makes the clinical picture of the disease more complete and helps prescribe the correct treatment to the patient. The disease is distinguished by the mechanism of development, the degree of blood loss and other characteristics. Based on the amount of blood released per day from the lungs, the disease is:
- First degree – up to 50 ml per day.
- Second degree – 50-200 ml per day.
- Third degree – 200-500 ml per day.
At the same time, pulmonary hemorrhage is measured by the number of milliliters of blood fluid poured out per hour, so coughing up blood should be differentiated from it. According to the mechanism of development, hemoptysis occurs due to: mechanical injuries, defects in the vascular wall due to various pathologies (erosion), and decreased permeability of the vascular walls.
According to the degree of blood loss, hemoptysis is mild, when blood in the form of streaks or liquid appears in the sputum, but the condition is stable and not life-threatening, and also massive. The second type is another name for pulmonary hemorrhage. Depending on the number of repetitions, hemoptysis can be: single, episodic, recurrent.
Entering data according to the classification into the chart of a patient who is coughing with blood from the lungs allows you to prescribe the most appropriate therapy, as well as continue treatment with other specialists without repeated examinations and collecting a complete history.
Treatment
Treatment tactics differ depending on what disease led to hemoptysis. It is the doctor who determines how to treat pathologies of the respiratory system or heart in order to eliminate the appearance of blood with cough. Under no circumstances should you self-medicate. Conservative therapy with medications (injections, tablets) and other non-surgical methods may be prescribed, and sometimes surgical treatment of the damaged area of the lung is performed.
In some cases, it is permissible to use traditional methods. As a result of therapy, relief of the underlying disease leads to a stop or reduction in hemoptysis from the lungs. Symptomatic treatment involves the administration of tranexamic acid.
Excerpt describing hemoptysis
“I’ll give them a military command... I’ll fight them,” Nikolai said senselessly, suffocating from unreasonable animal anger and the need to vent this anger. Not realizing what he would do, unconsciously, with a quick, decisive step, he moved towards the crowd. And the closer he moved to her, the more Alpatych felt that his unreasonable act could produce good results. The men of the crowd felt the same, looking at his fast and firm gait and decisive, frowning face. After the hussars entered the village and Rostov went to the princess, there was confusion and discord in the crowd. Some men began to say that these newcomers were Russians and how they would not be offended by the fact that they did not let the young lady out. Drone was of the same opinion; but as soon as he expressed it, Karp and other men attacked the former headman. – How many years have you been eating the world? - Karp shouted at him. - It’s all the same to you! You dig up the little jar, take it away, do you want to destroy our houses or not? - It was said that there should be order, no one should leave the houses, so as not to take out any blue gunpowder - that’s all it is! - shouted another. “There was a line for your son, and you probably regretted your hunger,” the little old man suddenly spoke quickly, attacking Dron, “and you shaved my Vanka.” Oh, we're going to die! - Then we’ll die! “I am not a refuser from the world,” said Dron. - He’s not a refusenik, he’s grown a belly!.. Two long men had their say. As soon as Rostov, accompanied by Ilyin, Lavrushka and Alpatych, approached the crowd, Karp, putting his fingers behind his sash, slightly smiling, came forward. The drone, on the contrary, entered the back rows, and the crowd moved closer together. - Hey! Who is your headman here? - Rostov shouted, quickly approaching the crowd. - The headman then? What do you need?.. – asked Karp. But before he could finish speaking, his hat flew off and his head snapped to the side from a strong blow. - Hats off, traitors! - Rostov’s full-blooded voice shouted. -Where is the headman? – he shouted in a frantic voice. “The headman, the headman is calling... Dron Zakharych, you,” submissive voices were heard here and there, and hats began to be taken off their heads. “We can’t rebel, we keep order,” said Karp, and several voices from behind at the same moment suddenly spoke:
Text of the book “Hemoptysis”
Differential diagnosis of hemoptysis
In general, diseases and pathological conditions that can potentially be complicated by the development of hemoptysis and pulmonary hemorrhage can be presented in the form of a table (Table 1).
Table 1
Diseases and pathological conditions that can potentially be complicated by the development of hemoptysis and pulmonary hemorrhage
The admixture of blood in sputum, as the main complaint that patients may present, does not always serve as a manifestation of diseases of the bronchopulmonary system. Clinical situations requiring exclusion in patients with suspected hemoptysis are:
● vomiting blood;
● nosebleeds;
● bleeding from the mouth and larynx.
In these cases we are talking about the so-called false hemoptysis. The differential differences between false and true hemoptysis are presented in Table. 2.
table 2
Differential diagnosis for hemoptysis
As can be seen from the table, the principal factors that require consideration when carrying out differential diagnosis between false and true hemoptysis are: anamnesis, conditions of bleeding, as well as the nature of the blood released, the presence of impurities and the duration of bleeding.
Thus, in the presence of anamnestic data for diseases of the gastrointestinal tract (erosive and ulcerative lesions, liver diseases, including against the background of chronic alcoholism, etc.), it is necessary to exclude gastrointestinal bleeding. In addition, it should be taken into account that with gastrointestinal tract vomiting there is vomiting of blood, which has a dark color, taking on the appearance of “coffee grounds,” as well as the development of melena. Nosebleeds or bleeding from the mouth can be suspected if there is a history of diseases of the oral cavity, nasopharynx, including malignant neoplasms. In this case, scanty spit of sputum is coughed up in the morning with blood clots on their surface.
In situations where there is a history of diseases of the bronchopulmonary system, as well as cardiovascular pathology, accompanied by symptoms of pulmonary hypertension, the presence of “true” hemoptysis can be assumed. In these cases, there is a discharge of sputum mixed with blood, mostly independent of the time of day and lasting from several hours to several days.
Main causes of hemoptysis
“When working on a problem, it is always useful to know the answer.” This seemingly contradictory formulation actually justifies itself, especially when it comes to medical issues. Any diagnostic search makes sense only when its possible outcomes are initially known.
If we talk about the etiology of hemoptysis, there are many different classifications of its main causes.
Based on the pathophysiological mechanisms, the following causes of hemoptysis can be identified:
1) pathology of the respiratory system itself;
2) hemoptysis as a consequence of pathological conditions accompanied by pulmonary hypertension;
3) blood clotting disorder;
4) systemic pathology of connective tissue (immune inflammation);
5) “false CC” – coughing up latently aspirated blood.
Attempts to systematize the etiological factors in the development of hemoptysis were made earlier, including by outstanding clinicians over the years. One of them, Eugene Braunwald, the great American cardiologist of the early 20th century, classified the main causes of hemoptysis into the following etiological groups (Table 3).
Table 3
Classification of causes of hemoptysis (E. Braunwald)
Despite some shortcomings of this classification, in particular, the unification of many different nosologies into a single group “others” without their clear differentiation, the general principles of separation do not lose their relevance today.
However, today it is more convenient to classify all possible causes of hemoptysis according to the following headings (Table 4):
Table 4
Classification of causes of hemoptysis
End of table. 4
If we consider the frequency of occurrence of various causes of hemoptysis, then this indicator will differ depending on the patient population.
Thus, in 2005, foreign researchers Sinha S. et al. reported on 429 patients with CC who underwent fiberoptic bronchoscopy. As a result, lung cancer was diagnosed in 45.7% of cases, pulmonary tuberculosis - 9.8%, pneumonia - 9.1%, bronchiectasis - 2.8%, aspergiloma - 2.6%, sarcoidosis - 3.9%, extrapulmonary pathology – in 4.7% of cases. These data differ significantly from the results of a ten-year study conducted by domestic scientists led by A.O. Ledin. (2005) in a general clinic (Fig. 5). Among the main causes of CC, various therapeutic pathologies were in first place (41.9%), lung cancer in second (28.2%), and nonspecific lung diseases in third (22.8%). These results are confirmed by world literature data, according to which currently the most common cause of chronic bronchitis in the pulmonology clinic is chronic bronchitis.
Rice.
5. Frequency of occurrence of various causes of hemoptysis
Naturally, the frequency of registration of the above reasons depends on the institution in which the patients are located, and on what signs are used to judge the presence of bleeding: a large amount of blood or its streaks in the sputum. Taking both features into account, the most common cause is bronchitis and bronchiectasis (approximately 60–70% of cases). In surgical hospitals, extensive lung lesions and diseases requiring surgical intervention are more common: carcinoma (20%), localized, segmental or lobar bronchiectasis (30%). In TB hospitals, the most common cause of hemoptysis is, naturally, tuberculosis (2–40% of cases). In reports of hemoptysis, which include both medical and surgical patients, the range is very wide: carcinoma (20%), bronchiectasis (30%), bronchitis (15%), other inflammatory diseases, including tuberculosis (10–20%) , other diseases, including vascular, traumatic and hemorrhagic (10%). However, even with the most thorough examination, in 5–15% of cases of massive hemoptysis, its exact cause cannot be established (Fig. 6).
Rice.
6. Frequency of occurrence of the main causes of hemoptysis
Diagnostics
Some axioms of diagnosis for hemoptysis
Before talking about the directions of diagnostic search for hemoptysis, I would like to mention a well-known statement among doctors: “Common diseases are common, rare diseases are rare.” Indeed, any diagnostic concept should be built around diseases most often accompanied by a symptom that is the main one in the clinical picture. As for hemoptysis, if the patient has it, the following should be remembered:
● Hemoptysis is rare in metastatic lung carcinoma;
● With viral or pneumococcal pneumonia, scanty hemoptysis may sometimes appear, but in each such case it is necessary to exclude a more serious concomitant disease;
Besides:
● In young patients with hemoptysis, the initial task is to exclude pulmonary tuberculosis, in elderly patients - to exclude lung cancer;
● In every case of repeated hemoptysis in a patient without signs of pulmonary tuberculosis, bronchiectasis should be assumed.
Before discussing possible diagnostic concepts for hemoptysis, let us remember about propaedeutics, because it is knowledge of the basics of medicine that determines the high level of clinical thinking of a doctor.
The diagnostic search in any clinical situation can generally be schematically represented as follows (Fig. 7):
Rice.
7. Structure of the diagnostic search
Naturally, making a diagnosis is impossible without a correct assessment of complaints, anamnesis, objective data, and the competent use of laboratory and instrumental research methods. Only a cumulative assessment of the above components can ensure the development of a specific diagnostic opinion.
Patients with hemoptysis are no exception.
Features of the anamnesis in patients with hemoptysis
When collecting an anamnesis, the following main points must be taken into account:
● Onset of the disease (acute, long-term course), possible provoking factors, symptoms;
● History of chronic lung diseases (COPD, bronchiectasis);
● Diseases of the cardiovascular system (coronary artery disease, heart defects, arrhythmias);
● Diseases of the blood and connective tissue;
● Smoking and occupational hazards;
● Social status (alcoholism, drug addiction, working and living conditions, education).
One of the luminaries of Russian propaedeutics, Professor M.V. Chernorutsky repeatedly pointed out that the main factor is the constitution as a set of functional and morphological characteristics of the organism, arising on the basis of hereditary and acquired properties and determined by the social environment. It is the social environment that is everything that surrounds a person in his daily life and that which largely affects his primarily physical condition.
The social status of the patient today is becoming one of the leading diagnostic criteria. In addition, in some controversial cases, it is the correct assessment of social status that allows for a correct differential diagnosis. We are talking primarily about socially disadvantaged segments of the population (persons without a fixed place of residence, abusing alcohol, narcotic substances). In some cases, indirect criteria allow judging social status, namely living conditions, education, presence or absence of a workplace, etc., not to mention the objective clinical signs of chronic alcoholic polyvisceropathy.
Chronic alcoholic polyvisceropathy is currently acquiring the status of an independent nosology. Being a background for many diseases of internal organs, it complicates their course and also reduces the effectiveness of the therapy, increasing the frequency of adverse outcomes.
In this regard, the following clinical example is typical:
Patient K., 42 years old, called an ambulance team due to severe weakness, shortness of breath, and hemoptysis. At the prehospital stage, a decrease in blood pressure to 90/60 mm Hg was recorded. Art. The ECG revealed atrial fibrillation. The patient was given a saline infusion; delivered to the emergency department with a diagnosis of “paroxysm of atrial fibrillation of unknown duration.” However, when collecting anamnesis, the emergency department therapist found out that the patient does not work, lives in a rented apartment with a partner, abuses alcohol (the last alcoholic excess occurred within 5 days before hospitalization), smokes about 1 pack of cigarettes per day. Based on chest x-ray data, a lung abscess cannot be ruled out. Due to the severity of the condition, the patient was hospitalized in the general intensive care unit with a diagnosis of “Alcoholic cardiopathy. Atrial fibrillation, constant form, tachysystole. Chronic alcoholic polyvisceropathy. Lung abscess. Intoxication".
In this case, the social environment is a rented apartment, a cohabitant, who keeps company for the constant consumption of alcohol and its surrogates.
Typical for this social environment are unsanitary conditions, constant hypothermia and, as a consequence, socially determined alcohol-associated conditions (Table 5), which must be detected during examination.
Table 5
Alcohol-associated conditions
Inherent features upon local examination are a beard and mustache, missing teeth, a broken nose, a median scar on the stomach after a perforated ulcer, etc.
Here's another example:
Patient B., 58 years old, an illegal migrant from Uzbekistan, was hospitalized on “03” in the emergency hospital with complaints of cough with sputum streaked with blood.
From the anamnesis it is known that the deterioration of the condition developed gradually. I have not asked for help before. He smokes 1.5 packs of cigarettes a day and abuses alcohol.
Epid. medical history: has been living illegally in Russia for 3 years, working as a construction worker as a laborer, living in a dormitory with five colleagues.
On examination: the condition is serious due to respiratory failure and low nutrition. Multiple abrasions on the skin of the back, arms, legs. Intelligence is reduced. There is harsh breathing in the lungs, scattered dry and wet rales on both sides. NPV – 28 per minute. Heart sounds are muffled, no murmurs are heard. Heart rate is 100 per minute, the rhythm is correct. Blood pressure – 100/70 mm Hg. Art. The abdomen is soft and painless. Liver +4 cm below the costal arch. Stool and urination without any peculiarities. According to the results of laboratory examination, the following were revealed: Hb - 110 g/l, MCV - 83.6, WBC - 18.6 × 10 9/l, total bilirubin - 46 µmol/l, AST - 78 IU, AlAt - 64 IU, total protein – 54 g/l.
ECG: sinus tachycardia. EOS deviation to the right. NBPNPG. X-ray infiltrative changes in the lungs on both sides (Fig. 8).
CT scan of the chest – disseminated tuberculosis. Emphysema, bullous transformation of the right lung.
Rice.
8. Radiographs of patient B.
Fig.
9. Research data from patient B
There are 9.2 million migrants on the territory of the Russian Federation (according to the Federal Migration Service of the Russian Federation), who are characterized by their own social environment: cramped living conditions - “corner” - bed space, overcrowding, spending leisure time in public places (shopping malls). centers). This contingent is characterized by its own pathology and, above all, the spread of infection (tuberculosis, HIV), which must be taken into account during the examination.
There is a third social environment. It is characterized by the following example.
The patient was hospitalized for emergency reasons due to complaints of fever up to 39 °C, unproductive cough, and suspected pneumonia. It is known that he has been using intravenous drugs for more than 15 years, the last time he used it was a week ago.
Understanding that for such patients, socially determined diseases are hepatitis C, B, HIV infection and infective endocarditis, an appropriate examination was carried out, which is fully consistent with their social status.
When examining in this situation, you should pay attention to traces of IV injections, tattoos, changes in complexion (pallor, maybe redness, circles under the eyes, dry or painful oily skin (“greasy plaque”), excessively constricted or dilated pupils, a border of irritation around the lips and especially in the corners of the mouth, redness and swelling of the face, difficulty in nasal breathing, a mask-like, hypomimic, puffy face or, conversely, animation of facial expressions. Drug addicts' teeth turn yellow, become covered with an indelible coating; the tongue loses its natural color, becomes thick, deep longitudinal cracks appear, a state of intoxication without the smell of alcohol, weight loss, pantomime changes, reflecting the “gestural contour” of the entire personality.
Unfortunately, the described variants of socially determined diseases are of particular importance today in view of their increasing prevalence and high negotiability. These conditions often mask another pathology and cause incorrect triage with corresponding consequences.
Features of the clinic
Clinical manifestations in patients with hemoptysis can be very diverse, even completely absent, and depend mainly on the underlying disease. Features of a clinical examination that require the doctor’s attention can be presented in the form of a table (Table 6).
Table 6
Clinical picture of hemoptysis
A combined assessment of anamnesis, social status and objective data in the vast majority of cases makes it possible to formulate the most likely preliminary diagnosis. But in any case, assumptions require confirmation using laboratory and instrumental research methods.
Laboratory diagnosis for hemoptysis
First-line laboratory tests include: clinical blood test (hemoglobin, red blood cells, leukocytes and leukocyte formula, ESR), coagulogram, detailed biochemical blood test.
In addition, cytological and bacteriological examination of sputum is mandatory. In case of social maladjustment, a blood test for HIV is necessary. Clinical blood test
Changes in the general blood test in most cases are not specific, but can serve as a certain differential diagnostic criterion.
Thus, high leukocytosis with a band shift, accelerated ESR indicate an active inflammatory process. A decrease in hemoglobin levels is alarming regarding the oncological process. A high hemoglobin level accompanied by a low ESR is most often characteristic of long-term chronic lung diseases. In any case, the results of a clinical blood test are interpreted solely taking into account the anamnesis and objective examination. Coagulogram
Study of the blood coagulation system is mandatory in all patients with hemoptysis.
First of all, this is due to the direct connection between the pathology of hemostasis and the risk of bleeding as such. At particular risk are patients taking oral anticoagulants for a long time, as well as patients with congenital and acquired blood diseases. Cytological and bacteriological examination of sputum
Sputum analysis is also a mandatory test in patients with hemoptysis. First of all, the importance of these tests is dictated by the need to exclude or confirm the most significant diseases from the point of view of prognosis and further tactics - tuberculosis and cancer. In most cases of chronic lung diseases, sputum analysis is characterized by the identification of inflammatory changes.
Instrumental diagnostics for hemoptysis
Instrumental diagnostics for hemoptysis should first of all include an X-ray examination of the chest organs, followed by MSCT or fibrobronchoscopy if there are indications for them.
Chest X-ray
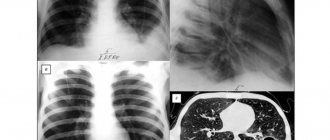
X-ray examination is of great importance in the diagnosis of hemoptysis. Being a first-line study, chest radiography allows in most cases to determine the leading nosology, and in some cases, based on the results of the study, the source of bleeding can be identified (Fig. 10).
Rice.
10. Diversity of the X-ray picture of hemoptysis
However, in 50% of cases in patients with hemoptysis due to chronic bronchitis, COPD and bronchiectasis, pathological changes are not detected on radiographs.
Currently, CT is used to diagnose bronchiectasis. For diseases of the bronchi and lungs, CT increases diagnostic accuracy by 42%. MSCT of the chest
Today, computed tomography has acquired the status of a routine examination for lung pathology. In particular, it is CT that makes it possible to clarify and detail the localization of the pathological process, its prevalence, shape, structure, which in some cases makes it possible to determine further treatment tactics, as well as identify indications for surgical intervention for a number of nosologies (Fig. 11).
Rice.
11. Variety of CT images for hemoptysis Fiber- optic bronchoscopy
Bronchoscopy is the most accessible for widespread practical use and an objective method for identifying the localization of the source of hemoptysis and pulmonary hemorrhage, and in some cases, a method for stopping it (Fig. 12).
Rice.
12. Endoscopic findings in hemoptysis
It is important to note that bronchoscopy is indicated even with minimal hemoptysis to exclude lung cancer in persons under 40 years of age with hemoptysis lasting less than a week and a normal chest x-ray.
Additional studies include endoscopy (if gastrointestinal tract is suspected), angiopulmonography (if necessary to exclude pulmonary embolism).
Hemoptysis: from syndrome to diagnosis
No talent can overcome a passion for detail.
"Murphy's Laws"
It's no secret that it is impossible to make a reliable diagnosis based on only one symptom. As was demonstrated above, hemoptysis can be a manifestation of a number of nosologies that are completely different in their mechanism of development and pathogenesis. That is why it is important to know the pathogenetic and clinical features of these very diseases.
Prevention
Even if hemoptysis appears after a prolonged winter or spring cold, it is necessary to consult a doctor immediately. This symptom may indicate that the disease has not gone away, but has become chronic, which poses a serious danger.
It is important to pay attention to symptoms such as: increased dry mouth, sore throat, the desire to drink cold water at night, followed by an unproductive cough, dry eyes or redness of the proteins that are not eliminated by medications.
If there is minimal suspicion of tuberculosis infection, a simple diagnostic method will help: increased sweating of the head during sleep, especially in the occipital region.
Folk remedies
Traditional recipes can be a real salvation for repeated episodes of blood discharge from the lungs with coughing. Their use can relieve pain and reduce the cough reflex. You can use folk remedies for hemoptysis only after visiting a doctor.
Recipes :
- During an attack. Make any sour warm drink, open the windows, calm down. Every quarter of an hour, eat a teaspoon of fine salt diluted with water.
- To reduce hemoptysis from the lungs. Squeeze out the radish juice and mix with honey. Drink up. Contraindications: cardiovascular and liver diseases.
- For the prevention and treatment of coughing up blood. Steam a tablespoon of dry burnet with a glass of boiling water and boil for a quarter of an hour. Let it brew, strain. Drink a tablespoon 7 times a day. Contraindicated for pregnant women.
Treatment
At the moment when a person develops an aggravated form of pathology and hemoptysis begins, he needs urgent support from specialists. In order to provide proper assistance and maintain the patient’s normal condition, the patient himself must know what first aid should be for hemoptysis and what procedures should be carried out.
Doctors recommend not to resort to any specific medical measures so as not to worsen the patient’s condition. First aid for hemoptysis is to calm the patient, give him a little rest, give him a half-lying position, and reduce any movements and conversations. To quickly improve the condition during an attack of sputum discharge with blood, doctors recommend applying a cool compress, maybe ice, to the chest. If hemoptysis occurs, you should immediately call an ambulance.
After the doctors arrive, the patient is provided with specialized emergency care for hemoptysis using various drugs. Subsequent therapy of the patient continues in the hospital, and treatment is prescribed after diagnosis and determination of the cause of the symptom.
In the hospital, the patient is treated with medication for hemoptysis:
- codeine is administered intravenously to prevent such attacks;
- Promedol solution is used for severe cough and pulmonary hemorrhage;
- hemostatic therapy;
- taking antifibrinolytic drugs;
- Colloidal or saline solutions are administered intravenously.
Sometimes non-traditional methods are used in the treatment of symptoms. They consist in the use of folk remedies. Instead of symptomatic medications, you can use hemostatic plants - chicory, yarrow, geranium root, nettle, peppermint, plantain leaves, knotweed and horsetail. However, before taking any alternative medicine, you need to consult a doctor and choose the optimal method of therapy that is beneficial for a particular pathology.