Hepatitis B - what is it? How to treat and avoid hepatitis B
Hepatitis B is a potentially very dangerous viral disease, which, according to WHO, kills about 780 thousand people every year. For this reason, the disease is considered a key issue facing global health. It is not so much the viral hepatitis B itself that is dangerous, but the complications it causes, which can lead to cirrhosis or liver cancer.
In total, there are about 250 million people in the world suffering from the chronic consequences of this disease. Often, hepatitis B comes not alone, but in combination with hepatitis D, which significantly aggravates the course of the disease and complicates treatment. Vaccination, which with a 95% probability protects against this viral infection, can save you from infection.
Today we will look at hepatitis B, what it is and how it is transmitted, how it is treated and how to avoid infection.
Etiology
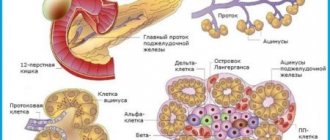
Hepatitis B virus (HBV) belongs to a family of pathogens conventionally called Hepadnaviridae (Latin hepar - liver, English DNA - DNA). Hepatitis B virions (Dane particles) are complexly organized spherical ultrastructures with a diameter of 42-45 nm, have an outer shell and an internal dense core. The DNA of the virus is circular, double-stranded, but has a single-stranded section. The core of the virus contains the enzyme DNA polymerase. Along with complete virions, there are polymorphic and tubular formations, composed only of fragments of the outer shell of the virion. These are defective, non-infectious particles that do not contain DNA.
Virus reproduction occurs in one of two possible ways: productive or integrative. In the case of productive reproduction, full-fledged integrative virions are formed - DNA integration with the cellular gene takes place. The integration of the viral genome or individual genes near the cellular genome leads to the synthesis of a huge number of defective viral particles. It is assumed that in this case the synthesis of viral proteins does not occur, so the person is non-infectious to others even if the surface antigen of the hepatitis B virus - HBsAg - is present in the blood.
Chronic Viral Hepatitis Delta (D).
The disease is the outcome of CVH-D, which occurs in the form of superinfection in patients with CVH-B. Virus D has a cytopathogenic effect on hepatocytes, continuously maintains activity and, consequently, progression of the pathological process in the liver, suppresses the replication of the hepatitis B virus. Symptoms of CHV-D . In the majority, it is characterized by a severe course with severe symptoms of hepatic cellular failure (severe weakness, drowsiness during the day, insomnia at night, bleeding, loss of body mass, etc.). Most develop jaundice and itchy skin. The liver is usually enlarged, but with a high degree of activity its size decreases. Often patients develop systemic lesions. In most cases, the disease takes on a progressive course with the rapid formation of cirrhosis. Examination reveals necrosis of the parenchyma. In the blood there is a constant increase in the activity of aminotransferases, bilirubin, and less often alkaline phosphatase (usually no more than 2 norms). The majority exhibit moderate hypergammaglobulinemia, disimmunoglobulinemia, and an increase in ESR. During the transition to LC, markers of integration of the hepatitis D virus and antibodies to it (Ig G, Ig M) are detected in the blood.
How is hepatitis B transmitted?
The source of infection is a sick person at almost any stage of the disease (including before the onset of symptoms of the disease), as well as a carrier of the virus. Any biological fluids of the patient are dangerous to others: blood and lymph, vaginal secretions and sperm, saliva, bile, urine.
How is hepatitis B transmitted? The main route of transmission of hepatitis B is parenteral, that is, through various contacts with blood. This is possible in the following situations:
- transfusion of blood or its components from an unscreened donor;
- when undergoing a treatment procedure in the hemodialysis department;
- various medical operations using reusable instruments (tissue biopsy, tooth extraction and other dental procedures);
- injecting drug use from one syringe by several persons;
- in hairdressing salons when performing manicure and pedicure procedures with reusable, poorly sterilized instruments, when performing tattooing or piercing.
Unprotected sex is also dangerous. The risk group for this disease includes surgical doctors, procedural and surgical nurses, children born to mothers with chronic hepatitis B or carriers of the virus. It should be noted that the likelihood of contracting hepatitis B is quite high even with a single contact.
Hepatitis C
Viral hepatitis C is the most unfavorable variant of inflammatory liver damage. This type of hepatitis is also called the “gentle killer.” Infection with hepatitis C occurs mainly through the parenteral route (through blood transfusion, surgery, etc.) or through unprotected sex. It is possible for a child to become infected by the mother during intrauterine development. A special feature of viral hepatitis C is the difficulty of diagnosing it. In most cases, the disease develops unnoticed, so even sometimes it is impossible to establish a relationship with the source of infection. If the patient has not undergone medical examinations, during which it was possible to detect infection with the hepatitis C virus, then the patient will learn about the disease when most of the liver is already affected. With hepatitis C, liver cancer develops more often than with other types of hepatitis. Due to the high variability of the virus that causes this disease, therapeutic and preventive measures are difficult.
Forms
There is an acute and chronic course of the disease; in addition, a separate variant is the carriage of hepatitis B.
- The acute form can occur immediately after infection, occurs with pronounced clinical symptoms, and sometimes with fulminant development. Up to 95% of people are completely cured; in the remaining part, acute hepatitis becomes chronic, and in newborns, chronicity of the disease occurs in 90% of cases.
- The chronic form may occur after acute hepatitis, or may initially occur without an acute phase of the disease. Its manifestations can vary from asymptomatic (carriage of the virus) to active hepatitis with transition to cirrhosis.
Causes and conditions of infection
The etiology of viral hepatitis infection includes:
- poor personal hygiene (unwashed hands);
- drinking raw, unpurified water;
- unwashed vegetables, fruits, unprocessed foods;
- contact with infected blood (unsanitary conditions in manicure, pedicure and tattoo salons, in the dentist’s office);
- drug addiction (re-use of syringes);
- unprotected sex.
All types of virus are transmitted in 2 common ways:
- fecal-oral;
- through contact with the blood of a carrier of the disease.
The main signs of hepatitis are:
Feeling weak and tired may be signs of hepatitis
- feeling of weakness;
- fatigue;
- disruption of the digestive system;
- pain in the area of the liver;
- dark urine and light feces;
- yellow skin.
Infectious form of the disease
Hepatitis, which can be transmitted to a person from the external environment, is called infectious. These include the following types of virus - A, B, C, D, E, G. The symptoms that appear when a viral infection enters the body have some similarities, but develop with different intensities. In this case, the inflammatory process proceeds differently and the level of liver damage differs. You can compare the incubation periods of hepatitis A and C. In the first case, the incubation period is almost two months (50 days), and in the second it is around 20 years.
Hepatitis A is most common and affects children under 15 years of age. There is one adult for every five sick children. This type of virus responds well to treatment with medications.
Hepatitis B has an incubation period of up to six months. This virus can be contracted through unprotected sexual contact with a sick person, as well as through blood. The manifestation of symptoms is similar to other types, but additionally other signs occur:
- rash on the body;
- joint pain.
The most complex form of the disease is hepatitis C. The route of infection is through the blood. It becomes chronic in most cases and leads to oncology and cirrhosis.
Hepatitis E poses a great danger to the expectant mother and fetus during pregnancy. Symptoms are similar to hepatitis A.
Non-infectious hepatitis
Non-infectious forms include diseases that arise against the background of:
- excessive alcohol consumption;
- consequences of diabetes and excess weight;
- side effects of medications;
- poisoning with toxic substances and poisons;
- autoimmune processes;
- metabolic failure;
- disturbances in the outflow of bile (biliary hepatitis);
- radioactive exposure.
Stages of the disease
There are the following stages of hepatitis B:
| Incubation period | duration - from 2 to 6 months, more often - 12-15 weeks, during which active replication of the virus occurs in liver cells. After the number of viral particles reaches a critical value, the first symptoms appear - the disease moves to the next stage. |
| Prodromal period | the occurrence of nonspecific signs of an infectious disease (weakness, lethargy, pain in the muscles and joints, lack of appetite). |
| The height of the disease | the appearance of specific signs (the liver increases in size, icteric staining of the sclera and skin appears, intoxication syndrome develops). |
| Last period | recovery (convalescence) or transition of the disease to a chronic form. |
Principles of treatment
In the treatment of any hepatitis, three points are important: properly selected drug therapy, diet and abandonment of all unhealthy habits.
Drug treatment has two goals:
- Eliminate the cause of the disease.
- Restore liver function and prevent further damage to the organ.
Therapy intended to fulfill the first point is determined by the etiology of hepatitis:
- if the viral nature of the disease is proven, the patient is prescribed antiviral drugs and interferons;
- if toxic - specific antidotes, sorbents, detoxification therapy;
- if autoimmune - glucocorticosteroids.
To restore liver function and protect the organ from harmful effects, hepatoprotectors are prescribed. There are a large number of such drugs; the active component in them may be one of the following substances:
- Silymarin, obtained from milk thistle. This substance stops the processes of peroxidation and destruction of hepatocytes.
- Essential phospholipids, which are elements of the cell membranes of hepatocytes, contribute to their restoration and normalization of metabolic processes in liver cells.
- Ornithine. It protects not only liver cells, but also cleanses the body of toxins.
- Lecithin (also a phospholipid).
- Ademetionine is a substance derived from the amino acid methionine that normalizes the biochemical processes occurring in the liver.
Symptoms of hepatitis B
Many patients with hepatitis B have no symptoms at all for a long time. The virus can only be detected through a laboratory blood test, which is necessary for medical examination or pregnancy registration. In such cases, a special test is done - a blood test to detect the “Australian antigen”.
When hepatitis B develops in the human body and has external signs, patients may experience the following symptoms:
- Nausea;
- Dizziness;
- Fast fatiguability;
- Rhinitis;
- Increased body temperature (often the temperature reaches 39-40 degrees);
- Cough;
- General weakness;
- Pain in the nasopharynx;
- Severe headaches;
- Change in skin color (jaundice);
- Yellowing of mucous membranes, eye sclera, palms;
- Change in the color of urine (it begins to foam, and the color resembles dark beer or strong tea);
- Pain syndrome in the joints;
- Loss of appetite;
- Change in the color of stool (discoloration occurs);
- Heaviness in the right hypochondrium;
- Chills.
When hepatitis B enters the chronic stage, patients, in addition to the main symptoms, develop signs of liver failure, which causes intoxication of the body. If at this stage of the development of the disease the patient does not undergo comprehensive treatment, he will suffer damage to the central nervous system.
Non-infectious hepatitis: symptoms and treatment
Signs and symptoms of the disease usually appear within a few days or weeks, but may take several months to occur. At the initial stage of non-viral hepatitis, symptoms may be mistaken for the flu. These include:
- Mild abdominal pain (upper right side);
- Nausea (may cause vomiting);
- Diarrhea;
- Fatigue;
- Loss of appetite;
- Fever;
- Muscle or joint pain;
- Weight loss.
At the late stage of non-infectious hepatitis, symptoms may include the following:
- Jaundice (staining of the skin and whites of the eyes yellow);
- Dark colored urine;
- Light, pale-colored stools;
- Enlargement or swelling of the liver;
- Severe abdominal pain;
- Changes in mental state (confusion, lethargy, dizziness);
- Hepatic encephalitis;
- Coma.
Living with any type of non-infectious hepatitis requires regular medical examinations and a treatment plan.
The first step in treating non-viral hepatitis is to remove the source of inflammation. Patients who have recently taken a substance that causes inflammation require gastric lavage. They will need blood tests to check for elevated liver enzymes, which is a symptom of damage to this organ.
Doctors usually prescribe corticosteroids to reduce inflammation. When non-infectious hepatitis leads to liver failure, liver transplantation is the only treatment option that improves the patient's survival.
Autoimmune hepatitis usually responds well to immunosuppressants with prednisone and azathioprine.
Character of the current
According to the nature of the course, hepatitis B is divided into:
| Fulminant | the disease goes through all stages in a maximum of two months, as a result of which the liver does not have time to regenerate, liver failure (encephalopathy) and even coma in the last stage are possible. Hepatic encephalopathy can be diagnosed at any stage of hepatitis disease. Symptoms of the disease appear more acutely; the patient also experiences low blood pressure and swelling. |
| Spicy | lasts a maximum of six months. Its signs in each person are expressed individually, depending on the type of hepatitis B virus. If the body is strong, it copes with the disease itself; if not, then it becomes chronic. |
| Chronic | The disease occurs with periods of exacerbation and remission. Due to the constant action of viruses, liver cells die, cirrhosis or liver cancer occurs. |
Doctors and scientists say that a virus that enters the body does not always cause hepatitis. If a person has a strong immune system, the virus does not pose a danger to him, although others around him may become infected. WHO notes that there are several hundred million potential carriers of the virus in the world who do not even know it.
Old classification
The disease, which caused yellowing of the skin and eyes, was described as early as the fifth century BC. Hepatitis, as an infectious disease, was first described by S. P. Botkin at the end of the 19th century. The scientist discovered a connection between the disease and the occurrence of liver cirrhosis. In the future, jaundice disease began to be called in honor of the discoverer - “Botkin”.
Until the 70s of the 20th century, the classification of viral hepatitis included three types: A, B and C. A little later, scientists discovered two more - D and E. In 1995, another group was identified - G.
Regarding hepatitis F, there is still debate among virologists around the world. In 1997, another type of disease was discovered - the TT virus.
Depending on how the inflammatory processes in the liver occur and why, types and forms are distinguished:
- Viral - divided into 5 common types (A, B, C, D, E), causing liver dysfunction and inflammation.
- Toxic. With frequent exposure to toxic substances, intoxication of the body and liver occurs. These substances include: alcohol, drugs, medications, as well as poisons of plant and industrial origin.
- Autoimmune. In this case, the disease develops against the background of a malfunction of the human immune system.
- The acute form appears unexpectedly and is accompanied by fever, yellowing of the skin, and symptoms of poisoning. The acute form is easier to cure if you catch it in time.
- The chronic form may not manifest itself in any way for a long period. By the time it is detected, the disease has already caused serious harm.
Complications of hepatitis B
The most common complication is damage to the bile ducts - in 12-15% of convalescents.
A frequent complication of chronic hepatitis B cirrhosis of the liver is numerous extrahepatic manifestations - colitis, - pancreatitis, arthralia, vascular damage, bleeding from the veins of the sac. Hepatic coma in cirrhosis - porto-caval or mixed type. Chronic persistent hepatitis B can last for many years with long-term remissions. “The mortality rate of patients with chronically active form of hepatitis B and liver cirrhosis is high, mainly in the first 5-10 years of the disease.
Forecast. The mortality rate is 0.1-0.3%, associated with the malignant (fulminant) form of the disease. The chronic form of hepatitis B occurs in approximately 10% of patients, liver cirrhosis - in 0.6% of patients. Most cases of chronic hepatitis B are associated with a history of anicteric form of the disease.
Clinical manifestations of the disease
Symptoms may depend on the cause, activity, and duration of the disease. The body's defenses also have a special effect.
If we talk about the general features of pathology, it is worth highlighting:
- malaise;
- loss of strength;
- decrease in the level of previous performance;
- detection of pain in the right hypochondrium;
- attacks of nausea;
- gagging, both constant and increasing from time to time;
- bowel dysfunction associated with increased flatulence, diarrhea, constipation;
- stool lightening;
- darkening of urine;
- yellowing of the skin;
- enlargement of the liver and spleen organs.
This symptomatology is inherent in the acute form of the pathology. If chronic hepatitis is observed, it is possible that the disease will become less evident in the clinical picture.
The symptoms will gradually subside. The jaundice will pass, feces and urine will become the same color, but if the pathology worsens again, the signs will make themselves felt again.
Very often, the chronic form develops into cirrhosis of the liver, which has unfavorable outcomes.
Symptoms also include extrahepatic manifestations. This may be palmar erythema, which means redness of the palms of a person infected with hepatitis.
Manifestations of minor hemorrhages on the skin and bleeding are not excluded. Hemorrhoids, general swelling and ascites should also be considered symptoms.
Women may experience disruptions in menstruation, and the opposite sex may experience decreased libido and potency.
Extreme manifestations of severe hepatitis may include liver failure, coma, and encephalopathy.
Diagnostics
Diagnosis of viral hepatitis B is carried out based on the detection of specific virus antigens (HbeAg, HbsAg) in the blood serum, as well as the detection of antibodies to them (anti-Hbs, anti-Hbe, anti-Hbc IgM).
The degree of activity of the infectious process can be assessed based on the result of a quantitative polymerase chain reaction (PCR). This analysis allows you to detect the DNA of the virus, as well as count the number of viral copies per unit volume of blood.
To assess the functional state of the liver, as well as monitor the dynamics of the disease, the following laboratory tests are regularly performed:
- blood chemistry;
- coagulogram;
- general blood and urine analysis.
Dynamic ultrasound of the liver is mandatory. If indicated, a puncture biopsy of the liver is performed, followed by histological and cytological examination of the punctate.
Chronic autoimmune hepatitis
Most often the disease occurs in women. Associated with hypergammaglobulinemia, major histocompatibility complex antigens and the following autoimmune syndromes: ulcerative colitis, thyroiditis, Sjögren's syndrome. At the same time, serum antibodies characteristic of this disease are determined: anti-LKM, ANA, antibodies to smooth muscle, soluble hepatopancreatic and liver antigens. Antimitochondrial antibodies and serological markers of hepatotropic viruses are absent.
As such, the actual factors that trigger the autoimmune process have not yet been established. These include environmental factors and infectious agents. In terms of serological and clinical manifestations, autoimmune hepatitis is heterogeneous. Unlike viral species, treatment with immunosuppressants and corticosteroids gives a rapid positive effect.
Chronic hepatitis B
In cases where chronic hepatitis is not the outcome of acute hepatitis, the onset of the disease occurs gradually, the disease appears gradually, and often the patient cannot say when the first signs of the disease appeared.
- The first sign of hepatitis B is fatigue, which gradually increases, accompanied by weakness and drowsiness. Often patients cannot wake up in the morning.
- There is a disturbance in the sleep-wake cycle: daytime drowsiness is replaced by nighttime insomnia.
- Lack of appetite, nausea, bloating, and vomiting occur.
- Jaundice appears. Just as in the acute form, first the urine darkens, then the sclera and mucous membranes yellow, and then the skin. Jaundice in chronic hepatitis B is persistent or recurrent (recurring periodically).
Chronic hepatitis B can be asymptomatic, however, both with asymptomatic course and with frequent exacerbations, numerous complications and adverse consequences of hepatitis B can develop.
Diagnostics. Treatment. Prevention
If liver damage is suspected, the doctor will conduct a thorough examination, determining the size of the liver and spleen by palpation of the abdomen. Before visiting a doctor, a list of medications that the patient has taken recently should be compiled. Next, clinical tests are carried out to detect viral hepatitis, a detailed biochemical blood test, and liver function indicators are determined (bilirubin, AST, ALT, Gamma-GGT, protein, alkaline phosphatase, albumin and others) and an analysis for autoantibodies. An ultrasound of the entire abdominal cavity, a liver biopsy and, in some cases, a computed tomography scan are also performed.
The method of treatment depends on the type of chronic hepatitis. During the treatment, alpha interferons, cytostatics, glucocorticosteroids are used, and symptomatic therapy is carried out. As for the autoimmune type, treatment requires hormonal and cytostatic therapy. In especially severe cases, liver transplantation is even performed.
In the treatment of a toxic species, the main goal is to eliminate the effects of the toxic factor. The liver itself is a unique organ, since it is capable of restoring its functions even after relatively severe damage. In this regard, stopping exposure to toxic agents together with taking hepatoprotectors often allows the patient to be cured.
Prevention is carried out only under the supervision of a doctor. Its main ways are adherence to the regime and dietary nutrition, as well as drinking heated mineral waters, such as Essentuki-4, Smirnovskaya, Slavyanovskaya, etc.). The courses are repeated 2 times a year. For preventive purposes, choleretic drugs, hepatoprotectors, enterosorbents are used, and sanatorium-resort treatment is carried out.
To date, prevention of hepatitis B has been developed. Vaccines against hepatitis C and D have not yet been created. Prevention of drug-induced and toxic hepatitis consists of following the general rules for storing hepatotropic poisons, as well as prescribing medications, taking into account their pharmacokinetics. Prevention of autoimmune hepatitis has not yet been developed.
Chronic hepatitis is a disease that can develop either independently or be a consequence of acute hepatitis. In any case, a patient with chronic hepatitis should be constantly under the supervision of a doctor and strictly follow all his recommendations.
Causes of chronic hepatitis and its types
Chronic hepatitis is an inflammatory process in the liver that lasts at least six months. The cause of chronic hepatitis is most often a viral infection - hepatitis B, C, D viruses. These viruses have a direct damaging effect on liver cells (hepatocytes). Is chronic hepatitis contagious? Chronic viral hepatitis is contagious, the infection is transmitted from a sick person to a healthy person through sexual contact and through blood transfusion, organ transplantation, and also through the use of insufficiently sterilized medical instruments.
Chronic liver hepatitis can develop due to toxic damage to hepatocytes by drugs, alcohol (chronic alcoholic hepatitis) or various chemicals. All these agents have a direct destructive effect on liver cells. Chronic drug-induced hepatitis Drug-induced hepatitis is not such a rare disease
may develop when taking medications such as halothane, methyldopa, isoniazid, rifampicin, pyrazinamide, phenytoin, zidovudine, ketoconazole, tetracyclines, clarithromycin, nifedipine, ibuprofen, indomethacin, as well as hormonal contraceptives. Chronic toxic hepatitisToxic hepatitis - exposure to harmful substances on the liver is not contagious.
Chronic hepatitis can also develop against the background of autoimmune processes, in which the immune system “does not recognize” liver cells and produces antibodies to them that destroy them. Today it has been established that chronic autoimmune hepatitis develops with certain congenital disorders.
Chronic cryptogenic hepatitis is a liver disease with liver changes characteristic of chronic hepatitis, with the exclusion of viral, autoimmune and drug causes of its development. That is, in fact, it is hepatitis of unspecified origin.
Chronic reactive hepatitisHepatitis is the scourge of our time
develops against the background of severe long-term diseases of other organs and systems. It is often called nonspecific, secondary hepatitis.
Classification of chronic hepatitis according to the characteristics of the disease:
chronic persistent hepatitis (CPH) - benign, usually without complications, sometimes it is called inactive, but this is not entirely true; chronic active hepatitis (CAH) - aggressively occurring with large areas of necrosis and progressive destruction of liver cells, often progresses to cirrhosis of the liver with partial loss of liver function.
There is also chronic cholestatic hepatitis, a disease that occurs with a violation of the outflow of bile through the small bile ducts.
Signs of chronic hepatitis
Acute and chronic hepatitis have similar symptoms, but the signs of chronic hepatitis are usually less pronounced. They can be different, it all depends on the cause of the disease, the characteristics and duration of its course and the degree of damage to liver cells. Common symptoms of the disease are weakness, fatigue, heaviness or pain in the right hypochondrium, lack of appetite, nausea, intolerance to fatty foods, increased bleeding, periodic itching of the skin, pain in the joints Pain in the joints - how to figure out what is happening?
and muscles, increased temperature.
Exacerbation of chronic hepatitis is accompanied by increased itching of the skin, the appearance of icteric discoloration of the skin and mucous membranes (the sclera turns yellow especially clearly - this is the earliest sign of exacerbation), dark urine and discolored feces. A sign of exacerbation is also an enlargement of the liver and increased pain.
Chronic hepatitis in children most often has a persistent nature, periods of exacerbation are replaced by clinical and laboratory remission. Exacerbations often occur 1-2 times a year, less often - more than twice a year. But a continuously relapsing course (chronic active hepatitis) is also possible; it is more common with the acute onset of the disease. But more often, chronic hepatitis in children develops gradually, with a slow increase in manifestations and exacerbations associated with acute respiratory diseases.
Diagnosis of chronic hepatitis
Despite the characteristic signs of the disease, the diagnosis of “Chronic hepatitis” must be confirmed by additional research data. An ultrasound examination of the abdominal organs is mandatory; if necessary, a percutaneous liver biopsy is performed under ultrasound control, followed by a histological examination of the tissue taken.
Laboratory tests include: general blood and urine tests, blood tests for liver enzymes and bilirubin, and autoantibody tests.
How to treat chronic hepatitis
In case of exacerbation, treatment of chronic hepatitis begins with bed rest and proper nutrition. The diet for chronic hepatitis should exclude foods that have a negative effect on the liver. Drug therapy depends on the type of hepatitis and the degree of its activity, therefore it is selected by the doctor individually.
Prevention of chronic hepatitis is the prevention of viral infections and the elimination of any toxic effects on the liver. If a patient vitally needs medications with hepatotoxic effects, their administration should be accompanied by regular liver function tests.
Galina Romanenko
Chronic hepatitis is a disease characterized by low-grade inflammation of the liver and most often occurs against the background of untreated acute hepatitis of various etiologies.
The inflammatory process may be caused by the entry of certain viruses into the body, the presence of certain pathologies of the liver and neighboring organs, helminthic infestations, poisoning or uncontrolled use of certain medications.
Depending on the cause, chronic hepatitis can be considered as an independent disease or as a manifestation of any disease of the abdominal cavity (intestines, stomach).
How to treat hepatitis B
In most cases, acute hepatitis B does not require treatment, as most adults can cope with the infection on their own without the use of medications. Early antiviral treatment may be required in less than 1% of cases: patients with aggressive infection.
If, with the development of hepatitis B, treatment is carried out at home, which is sometimes practiced when the disease is mild and constant medical supervision is possible, some rules must be followed:
- Drinking plenty of fluids helps with detoxification - removing toxins from the body, and also prevents dehydration, which can develop due to excessive vomiting.
- Do not use medications without a doctor’s prescription: many medications have a negative effect on the liver, and taking them can lead to a rapid worsening of the disease.
- Don't drink alcohol.
- It is necessary to eat adequately - food should be high in calories; it is necessary to adhere to a therapeutic diet.
- You should not overuse physical activity - physical activity should correspond to your general condition.
- If unusual, new symptoms appear, you should immediately call a doctor!
Drug treatment for hepatitis B:
- The basis of treatment is detoxification therapy: intravenous administration of certain solutions to accelerate the elimination of toxins and replenish fluid lost through vomiting and diarrhea.
- Drugs to reduce intestinal absorption function. A lot of toxins are formed in the intestines, the absorption of which into the blood when the liver is not functioning effectively is extremely dangerous.
- Interferon α is an antiviral agent. However, its effectiveness depends on the rate of virus reproduction, i.e. infection activity.
Other treatments, including various antiviral drugs, have limited effectiveness and high treatment costs.
Prevention of hepatitis
Basic measures to prevent viral hepatitis:
- Vaccination against hepatitis B (against hepatitis A before traveling to regions with a high incidence of this infection).
- Clean hands, food, water.
- Protected sexual relations.
- Careful handling of blood and secretions from patients with parenteral hepatitis (B, C, D).
Well, to prevent the development of non-infectious hepatitis, it is important to take medications only as prescribed by a doctor, lead a healthy lifestyle, and be careful with industrial poisons, mushrooms, and poisonous plants.
Zubkova Olga Sergeevna, medical observer, epidemiologist
28, total, today
( 40 votes, average: 4.43 out of 5)
Botkin's disease in children: symptoms and children
Parainfluenza: symptoms, diagnosis, treatment and prevention
Related Posts
How to avoid infection?
Prevention, both specific (vaccination) and nonspecific, aimed at interrupting the transmission of hepatitis B: correction of human behavior; use of one-time tools; careful adherence to the rules of hygiene at home; restriction of transfusions of biological fluids; use of effective disinfectants; the presence of a single healthy sexual partner or, otherwise, protected sex (the latter does not provide a 100% guarantee of non-infection, since in any case there is unprotected contact with other biological secretions of the partner - saliva, sweat, etc.).
Vaccination is widely used to prevent hepatitis B infection. Routine vaccination is accepted in almost all countries of the world. WHO recommends starting to vaccinate a child in the first day after birth, unvaccinated children of school age, as well as people from risk groups: professional groups (medics, emergency services, military, etc.), people with non-traditional sexual preferences, drug addicts, patients who frequently receive drugs blood, persons on program hemodialysis, married couples in which one of the members is infected with the virus, and some others. For vaccination, the vaccine against the hepatitis B virus is usually used, which is a protein shell of the viral particle, the so-called. HBs antigen. In some countries (for example, China) a plasma vaccine is used. Both types of vaccines are safe and highly effective. The vaccination course usually consists of three doses of the vaccine administered intramuscularly at intervals.
The effectiveness of vaccination of newborn children born from infected mothers, provided that the first dose was administered in the first 12 hours of life, is up to 95%. Emergency vaccination in case of close contact with an infected person, when infected blood enters the blood of a healthy person, is sometimes combined with the administration of a specific immunoglobulin, which theoretically should increase the chances that hepatitis will not develop.
UK guidelines state that initial responders (those who are immune through vaccination) need further protection (this applies to people at risk of hepatitis B). To maintain immunity to the hepatitis B virus, they are recommended to undergo repeated vaccination every five years.
TREATMENT OF ACUTE HEPATITIS.
There are no specific treatment methods and therefore most patients receive basic treatment (see treatment of chronic viral hepatitis, below).
- Bed rest is not necessary for most patients.
- Careful personal hygiene (hand washing, separate dishes, etc.).
- Hospitalization is necessary in severe cases of the disease and in the absence of the possibility of maintaining a regimen at home. Patient care must include measures to prevent the transmission of infection (disinfection, working with gloves, etc.)
- A strict diet is not necessary, but you need to exclude fats from your diet and drink juices.
Persons in contact with sick people.
- With viral hepatitis A, persons who are in contact with the patient can usually already be infected by the time jaundice appears and therefore do not need isolation and treatment. For prophylactic purposes, it is possible to administer intramuscularly human Ig (5 ml once).
- Sexual partners of patients with viral hepatitis B are subject to examination to determine serum markers, and in their absence, these persons are advised to administer the Recombined HBV vaccine. It is possible to administer Hyperimmune HBV immunoglobulin for 2-4 weeks.
Observations of patients who have had acute hepatitis.
- Abstinence from drinking alcohol until liver function is completely normalized (normalization of ALT, AST, GGTP, etc.), but a small amount of alcohol (4-8 servings per week) does not have a negative effect on the course of the recovery period. Complete abstinence from alcohol is necessary only for alcoholic hepatitis.
- Repeated testing of liver enzymes, mainly ALT and AST, is carried out 4-6 weeks from the onset of the disease, and if they remain unchanged, then they are repeated after 6 months. An increase in transaminase levels by more than 2 times after 6 months is the basis for an in-depth study, including a liver biopsy.
Immunization. Hepatitis A. Passive immunization with intramuscular injection of 5 ml of normal human Ig is effective for 4 months. It is carried out for preventive purposes. 1. Persons traveling to epidemiological regions (Indonesia, Middle East, South America, Mexico, etc.). 2. Persons located in; close contact with patients.
Hepatitis B. Passive immunization is carried out to persons who are in close contact with patients. IM administration of hyperimmune HBV immunoglobulin 500 units twice with an interval of 1 month.
Chronic Viral Hepatitis B.
Develops as a result of acute viral hepatitis B. Hepatitis B (HBV) does not have a cytopathogenic effect on hepatocytes, and their damage is associated with immunopathological reactions. A sharp increase in the immune response leads not only to massive damage to the liver parenchyma, but also to mutation of the virus genome, which subsequently leads to the destruction of hepatocytes over a long period of time. The virus can also impact outside the liver: mononuclear cells, gonads, thyroid gland, salivary glands (immunological aggression). Symptoms of CHV- B.
Complications
In adults, complications are mainly associated with late diagnosis of the disease. Since the symptoms of acute viral hepatitis are not so specific, it is easiest to suspect hepatitis by chronic signs of the disease, when the liver is significantly affected. Among the complications, the most common are cirrhosis - compensated and decompensated, portal hypertension, ascites and hepatocellular carcinoma. With a compensated form of cirrhosis, the disease can be cured in almost one hundred percent of cases with the help of the latest direct-acting drugs, but with the development of decompensated cirrhosis and liver cancer, the prognosis is not so positive.
Doctor's actions
If a person suspects that he has the hepatitis virus, he needs to see a doctor.
A qualified professional will need to carry out the inspection. Having identified the etiology of the pathology, he will prescribe a course of treatment and provide diet therapy for the patient.
Today, it is customary to vaccinate all newborns against hepatitis B while still in the maternity hospital. There is also a special vaccine against hepatitis type A.
You should never assume that you will not be able to catch the hepatitis virus during a blood transfusion or organ transplant.
To monitor your health, you need to get tested for the marker six months later.
Medical institutions are sensitive to the condition of blood and organ donors, but there is a time period when antibodies to the pathogen are not detected, i.e. It is simply impossible to understand whether there is hepatitis in biological materials or not.
Features of hepatitis virus separation
There is a whole table of classification of hepatitis, the disease is divided depending on the course, as mentioned above, but also according to etiology.
There are: alcoholic, viral, autoimmune, bacterial, toxic, drug-induced, cholestatic and hereditary hepatitis.
In fact, one cannot say that this division is exact. The whole point is that it is conditional.
After all, hepatitis viruses B and C are characterized by an autoimmune reaction that is provoked by viruses.
What can we say about other types, or rather alcoholic, medicinal and toxic, then the course of hepatitis is similar here too.
Analyzing the morphological picture of chronic hepatitis, it is customary to distinguish 2 phases: active and persistent. In turn, there are stages of remission and exacerbation of this type of disease.
It is very important for the doctor to correctly diagnose in order to understand exactly what type of pathology affected the person, what exactly caused the disease and what its phase is.
The patient is required to contact the doctor at the hospital in a timely manner and follow all instructions without deviating from therapy of his own free will.