Causes of the disease
The reasons why leukoplakia may develop in the mouth vary. Often the appearance is influenced by external or internal factors. The occurrence of this disease is facilitated by the environment, irritants that affect the mucous membrane and injure it. Provoking factors can be chemical, mechanical, thermal. Often these factors are:
- smoking,
- strong alcohol,
- long-term use of medications, in this case leukoplakia occurs as a side effect,
- fillings, crowns, dentures that are placed poorly and constantly injure the oral cavity,
- salty, sour, bitter foods,
- cold or hot drinks.
Internal factors include: some progressive diseases of the intestines or stomach, lack of vitamins, diabetes, hormonal imbalances, anemia, stomatitis, HIV, heredity.
Prevention of leukoplakia
To avoid leukoplakia, you should pay special attention to hygiene rules. In particular, it is important to sanitize the oral cavity and provide rational prosthetics. Quitting smoking will protect against the risk of Tappeiner's leukoplakia.
In addition, it is important to promptly identify and treat sexually transmitted diseases, correct hormonal imbalances in the female body, and prevent metabolic disorders and deterioration of the body’s protective functions.
Source: https://medside.ru/leykoplakiya
Manifestations and symptoms
Leukoplakia can affect any mucous membrane of the tissue : the uterus, internal genital organs, oral mucosa, larynx and esophagus.
It is not always possible to independently identify the onset of the disease, but there is a better chance of detecting it in the mouth even in the primary stages than in other organs.
There are several forms of this disease, which develop from one another. Flat leukoplakia, under the influence of negative factors, turns into verrucous, and if treatment is neglected, it develops into erosive. Leukoplakia of smokers has nothing to do with this.
Several similar forms of the disorder may appear within the oral cavity at different sites. Most often this type is found on the gums and palate. Under unfavorable circumstances, it turns into malignant formations.
This stage of the disease can be easily overcome if you stop drinking, smoking and take care of your health. The primary symptoms are mild inflammation of the inside of the mouth, covering small areas. The affected mucous membrane becomes cloudy and subsequently gray plaques appear in this place, similar to plaque, which do not go away and do not lose their color even when treated with iodine.
The affected areas are small, about 2-4 cm in diameter. We list the possible localization options for inflammation:
- inner cheek,
- corners of the mouth, contour of the lips,
- the lower or lateral surface of the tongue plate,
- upper part of the gums.
It may take a couple of weeks or months for such spots to form . The affected areas become slightly denser and rise above the healthy surface. To the touch, the injured surface does not seem dense, but you can feel the roughness of the damaged tissue and notice a change in color.
Flat leukoplakia at the initial stage does not cause inconvenience or discomfort. In rare cases, you may experience a feeling of dryness and tightness in the damaged area.
Depending on how severely the damaged areas have become keratinized, they may appear gray or white. The edges of the foci of inflammation are clearly defined, in this form they can remain throughout life without causing concern to the patient.
If injury to the inflamed area of the mucosa continues, keratinization of the tissue may intensify, the size of the lesion will increase, and the stage of the disease will change to verrucous.
Forms of leukoplakia
- Simple (flat);
- Erosive-ulcerative;
- Verrucous (plaque or warty);
- Smoker's leukoplakia (Tappeiner's leukoplakia);
- Soft.
Flat leukoplakia
Usually, with this form, leukoplakia can be noticed only visually; subjective sensations in the oral cavity are either absent or limited to a slight burning sensation of the mucous membrane at the site of the lesion. On the mucous membrane of the oral cavity or on the tongue, you can find a focus of keratosis (that is, keratinization) of a whitish color. It is formed precisely by a layer of cells, unlike plaque, for example, with candidiasis, and is not removed with instruments. Leukoplakia on the tongue usually looks like an oval or round spot, usually on the lateral surface. The buccal mucosa is affected in the form of a broken line, coinciding with the line of closure of the teeth.
This white line occurs in patients all the time and is accepted by many doctors as the norm. However, in reality, this is a manifestation of simple leukoplakia, and if not treated, then it is imperative to monitor its development! A star-shaped lesion can be located where the dentition ends - usually due to trauma to the retromolar area with a wisdom tooth.
In addition to the forms described, the lesions can have any other, often irregular pattern, and branch. Around the whitish lesion there are inflammatory signs - redness, swelling may be observed.
Verrucous leukoplakia
This form is a development of simple leukoplakia. In addition to the presence of a lesion, there may be complaints such as dry mouth, roughness of the mucous membrane, felt by the tongue, causing discomfort, especially when talking. There is also a burning sensation.
In the plaque form, the lesions rise above the surface, are rough, and have clearly defined boundaries. The warty appearance is lumpy formations on the oral mucosa.
As a rule, this lesion is located near the traumatic factor, it feels very dense to the touch, it is impossible to collect the mucous membrane into a fold. In addition to whitish, the color can be bright, straw-yellow. The pearlescent sheen present at the beginning of the disease is gradually lost and the area becomes cloudy, which means the process is progressing. If the leukoplakia lesion has darkened, the likelihood of it becoming malignant is very high.
Diagnostics
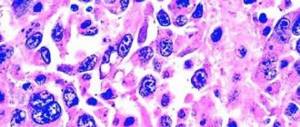
Under a microscope, a pronounced thickening of the epithelial membrane can be determined. When examined under fluorescent light, the radiation is yellowish with a benign course, and with malignancy it becomes violet. When examining cellular material, nuclear degeneration is determined. Histology shows thickening and proliferation of surface layers with an increased content of keratohyalin, a protein that promotes keratinization. A deep layer of connective tissue protrudes significantly into the damaged integumentary layers, and an inflammatory process, looseness, and swelling appear.
Ulcerative-erosive leukoplakia
The pronounced clinical picture causes serious concern in patients, forcing them to consult a doctor with complaints of pain, burning, rawness, intensified by irritation of the mucous membranes. Bleeding may also occur, although not always. Erosion is visible on the tongue or mucous membranes, usually up to 5 millimeters in diameter. Under the influence of the sun or in cold weather, leukoplakia on the red border of the lips does not heal for a long time, especially as a result of self-medication. Lymph nodes are usually without pathology. Erosive-ulcerative leukoplakia of the oral cavity has a brown glow during luminescent examination. Under a microscope, keratinized areas alternate with epithelial defects. Cytology shows many young, immature cellular elements. On histology, the layers are significantly thickened, including due to the expansion of intercellular spaces. The epithelium is loose, with several nuclei in the cells. Strands are formed that protrude deeply into the underlying connective tissue. There are no areas of epithelium at the site of erosion. Blood cells responsible for the immune response are present in large numbers in the lesion.
Soft leukoplakia
As a rule, the development of this variant of the disease is provoked by general factors, such as nervous exhaustion, depression, overload, mental trauma and similar problems. Bad habits contribute to the appearance of foci of leukoplakia - smoking, biting lips, cheeks, drinking too hot drinks, addiction to alcohol. The occurrence of these factors is most typical for young and middle-aged people, which distinguishes this option from those described above. Leukoplakia of the mucous membrane is manifested by a breakdown of the compensatory mechanism, in which dystrophic processes sharply prevail over regeneration. Histologically, it is revealed that the epithelial layer suffers most, in which the cells lose their main structural elements and are vacuolated, that is, filled with fluid.
Foci of keratinization appear as a result of painless biting of the mucous membranes; roughness and slight thickening of the tissue may be felt. A number of patients may note a decrease in taste or temperature sensitivity as a concomitant symptom. There are limited and diffuse forms, depending on the volume and area of distribution of the lesions. White foci of keratinization in this form can be removed with a spatula; they are easily separated from the surface. Another difference from typical forms is the absence of an inflammatory component.
Diagnostics
In a typical picture, the main complaint is dryness in the affected area. The cheeks, corners of the mouth, lips (mainly the lower), lateral surfaces of the tongue, bottom of the cavity, palate, and gums are affected. When examining fingerprint smears, epithelial cells are present in large numbers, both nucleated and non-nucleated. The glow is bluish and uneven. Dentistry reveals a grayish-white epithelium, located in a thin layer, reminiscent of a washcloth.
Diffuse lesions give a feeling of discomfort when bulging, rough areas of thickening interfere with conversation. Manifestations are simultaneously detected in all places on the mucous membrane typical for the disease. The comparison with a washcloth can be applied to the appearance of the mucous membrane even with the naked eye. In the diffuse form, lips are almost always affected; the epithelial scales are constantly sloughed off.
The atypical form is misleading due to the patient’s lack of complaints characteristic of leukoplakia. As a rule, atypical leukoplakia manifests itself as a slightly raised white line; in the diffuse version, it is a total lesion of the mucous membranes, expressed by turbidity. When examined, the connective tissue has pronounced vasodilation, stasis, swollen collagen fibers and thinned, fragmented elastic fibers.
Nicotine leukoplakia
In 1949, this form was first described, although references to symptoms were found a century earlier. Tobacco smoking causes disease through a combination of chemical and temperature effects. The most dangerous substance in the destruction of nicotine tars is pyridine - a strong carcinogen. The main effect is on the mucous membranes of the hard and soft palate; it is this localization that is characteristic of Tappeiner’s leukoplakia. Initially white spots, gradually acquire a brown, then black color due to constant exposure to tobacco smoke. In this form, the excretory ducts of the salivary glands become like tubercles, soft in consistency, and hyperemic.
If leukoplakia in the mouth has not turned into a malignant form, stopping smoking will gradually lead to a decrease and then complete disappearance of the lesions.
The histological picture shows no changes in the connective tissue, that is, the pathology is superficial. Structural changes in the epithelium of the excretory ducts in advanced cases degenerate into squamous cell carcinoma.
Verrucous stage of leukoplakia
This is an advanced stage of the initial stage or flat leukoplakia of the oral cavity. At this stage, not only the compaction of the tissue is strongly expressed, but its embossed or rough state is noticeable. The lesions acquire a bright white color, which stands out well from healthy skin. Damaged areas hurt when exposed to spicy or salty foods, hot or cold drinks.
The verrucous stage can be divided into 2 forms:
- Plaque , in which leukoplakia of the tongue manifests itself in the form of protruding white or yellowish plaques.
- Warty , the most common, has the shape of gray tubercles protruding 1-2 millimeters.
If measures are not taken in time and irritating factors are not cut off, leukoplakia can degenerate into a tumor. The verrucous stage of the disease precedes oncology. But such oral leukoplakia does not always develop into malignant formations. Most often it affects the tongue plate; if the affected areas on it are uneven and pronounced, this increases the chance of degeneration into a tumor.
Leukoplakia of the oral mucosa does not cause any discomfort; it is discovered by chance. Therefore, there is a possibility of starting the disease. Hardened plaques sometimes burst, and the sharp crust can injure the mucous membrane. The beginning of this process determines the development of cancer.
Causes of oral leukoplakia
To date, scientists cannot name the exact causes of oral leukoplakia. However, they have identified some factors that increase the likelihood of developing the disease. The main one is considered to be chronic injury to the oral mucosa.
Other reasons include:
- Smoking. Not only inhaling smoke from regular cigarettes is harmful, but also smoking hookahs and chewing tobacco. The toxic substances they contain lead to the fact that the epithelium does not have time to recover, thereby creating the preconditions for pathological changes in its cells.
- Drinking very hot or very cold food (drinks). In this regard, spicy, salty and sour dishes pose a danger.
- Alcohol abuse.
- Injuries to the oral cavity. A common cause of mechanical damage to the mucous membranes are crowns, fragments of teeth, orthodontic structures, and dentures.
- The effect of current on the body when there are metal crowns in the mouth.
- Working in a hazardous enterprise. Contact with varnishes, resins, aniline dyes and other chemicals has a negative impact on health.
- Hereditary predisposition to leukoplakia.
- HIV infection or stage of AIDS.
- Exposure to ultraviolet radiation on the body.
- Taking medications.
- Vitamin A deficiency in the body.
- Deficiency of iron, potassium and magnesium in the body.
- Anemia.
- Chronic diseases of the digestive system.
- Diabetes.
- Diseases of the endocrine system, accompanied by hormonal imbalance.
Simple or flat leukoplakia
The most common stage is the primary stage, which is asymptomatic and has no pain or other irritating sensations. It is often discovered by chance during an examination by a dentist; the reason for seeking treatment is for completely different reasons.
Occasionally, the patient may complain of a burning sensation or tightness, or discoloration of the affected area. There are often complaints of loss of taste when leukoplakia of the tongue develops. All inflamed areas of the mucous membrane have the appearance of foci outlined by contours. All are at the same level as healthy tissue; the shape and size of the lesion may vary. To the touch, these are slightly rough, lumpy tissues.
The color of the spots varies from gray to white, depending on the intensification of tissue compaction. You may feel the roughness and dryness of the damaged areas. It is difficult to detect inflammation during a visual examination; the seals are not noticeable.
Depending on the location of the lesion, the lesions may vary in color, shape and size. Triangle-like spots appear in the corners of the mouth. Elongated lines, discontinuous or solid, are formed on the inner surface of the cheeks.
On the edges of the lips these are shapeless white spots. Wide continuous stripes are formed on the tongue and palate, taking up a lot of space. The flat stage can progress to the vurrucous stage, or it can remain at its initial stage all his life and not bother the patient.
Diagnosis and treatment of oral leukoplakia
During a visual examination, the dentist can make a preliminary diagnosis, but for an accurate diagnosis of leukoplakia, a biopsy is necessary. The biopsy is performed under local anesthesia, and the resulting material is examined in a cytology laboratory.
The treatment tactics for oral leukoplakia boils down to eliminating the source of irritation. This includes minimizing or completely quitting smoking, correction of dentures, restoration of teeth when their edges are broken, and sharpening of sharp tooth edges. In cases where the causes of leukoplakia are internal diseases, cryodestruction of the affected areas, correction of the underlying disease and clinical observation of the patient are indicated.
Leukoplakia is a precancerous condition of the mucous membrane, and if leukoplakia spots lose their shine, the surface becomes rough, covered with growths and ulcers, then, as a rule, the prognosis in these cases is unfavorable and leukoplakia degenerates into oral cancer. Approximately 10% of cases of leukoplakia of the oral mucosa result in malignancy.
Prevention
Preventing the occurrence of the disease is not difficult, you will have to remember and adhere to the rules:
- Strengthen your immune system.
- Stop smoking and drinking alcohol.
- Contact only trusted specialists, avoiding poorly placed fillings, dentures and crowns.
- Visit the dentist once every six months.
Leukoplakia tends to degenerate into oncology. The onset of changes depends on the stage and consequences of the disease.
If this disease is detected, you must register and undergo prescribed examinations. This is necessary, since leukoplakia has the ability to recur when the above risk factors worsen.
Soft leukoplakia
This is a benign neoplasm of the oral mucosa, an independent disease that occurs regardless of whether there is a history of hyperkeratosis. The development of the disease may be preceded by other forms of this pathology. The negative nature of the course may arise due to the same provoking factors.
The membrane affected by the disease turns pale and swells, there is no clear boundary of the neoplasms. The pathology is characterized by exfoliation of degenerated cells.
The patient develops the habit of biting raised areas. Neoplasms are found mainly along the edges of the lips and along the line of closure of the teeth, on the inner surface of the cheeks.
What is leukoplakia?
Leukoplakia
– this is a disease that affects the mucous membranes, causing keratinization of the integumentary epithelium of varying severity. Leukoplakia mainly affects the mucous membranes of the cheeks, especially the corners of the mouth, the lower lip, and also occurs on the back or side surface of the tongue, the alveolar process and in the area of the floor of the mouth. The surface of the integumentary epithelium is covered with unevenly keratinized scales.
The risk group is mainly for people aged 30 years. This disease begins to develop in the area of mucous surfaces, such as the tongue, corner and bottom of the mouth, lower lip, cheeks; in the vagina, on the clitoris and vulva, in the cervix, and occurs, but less frequently, in the area of the preputial sac and glans penis or in the area of the anus. If leukoplakia begins on the cheeks and tongue, then keratinization occurs along the line of connection of the teeth. Leukoplakia is a consequence of smoking and alcoholism. It provokes a lack of vitamins, and is accompanied by sluggish chronic inflammation. It has an immune effect on chronic irritation of the mucous surface. Leukoplakia is divided into different forms.
Leukoplakia of Tappeiner smokers
Leukoplakia affects the hard palate and adjacent areas of the soft palate. Some patients experience negative changes in the marginal area of the gums. In some fragments the mucous membrane is folded and, due to the disease, acquires a grayish-white tint. The light spot is covered with visible red dots of cyst-like dilated ducts of the salivary glands.
Due to blockage due to the accumulation of cells that have undergone a process of hyperkeratosis, the ducts externally look like nodules.
Leukoplakia of this form often occurs in conjunction with other types of disorders that are associated with damage to the corners of the mouth, cheeks and lower lip. The disease in question is characterized by the ability to restore its previous state.
After getting rid of the bad habit, the spots disappear, because the soft tissues of the oral cavity are no longer affected by irritants that contribute to negative changes.
Treatment
Treatment depends on the form of oral leukoplakia, the size of the lesions and the speed of development of the process. First of all, it is necessary to eliminate the causes of the pathology - give up bad habits, especially smoking, sanitize the oral cavity, correct the bite and incorrect position of the teeth, get rid of chips, select suitable dentures, use protective equipment against ultraviolet radiation and harmful substances at work, conduct an examination internal organs.
To improve immunity, Immunal and vitamin complexes are prescribed. The use of vitamin A internally and in the form of applications to the affected areas is especially effective.
Simple (flat) leukoplakia is quite easy to cure. To treat complex forms of the disease, they resort to surgical methods and use medications that promote regeneration and epithelization of the mucous membrane. To treat wounds and ulcers, antiseptic and wound-healing agents are used, for example, Solcoseryl, Olazol, Stomatofit ointments; if necessary, pain relief is prescribed (we recommend reading: instructions for use and composition of the drug “Stomatofit”).
READ ALSO: how to differentiate between lichen planus and leukoplakia in the mouth?
In the hospital
If conservative treatment does not bring results, then the lesions are removed using:
- diathermocoagulation (thermal cauterization of areas affected by leukoplakia),
- laser,
- cryodestruction (exposure to liquid nitrogen),
- chemical composition (cauterization with Condilin, Nycomed to remove warts, papillomas),
- electroexcision (excision with an electric knife),
- radio wave method (exposure to radio waves).
The procedures are carried out in a hospital setting. You should not remove warts and papillomas yourself, so as not to damage neighboring tissues! The most strict contraindication for the use of Condilin is pregnancy, since it can cause developmental pathologies in the fetus. Medicines used for disinfection (solution of Furacilin, Chlorhexidine, boric acid, hydrogen peroxide) and tissue restoration (applications of Retinol, Cigerol) are prescribed.
READ ALSO: how to properly dilute Chlorhexidine to rinse your mouth?
Drug therapy at home
At home, the same medications are used as in the hospital. It is important to strictly observe oral hygiene, rinse your mouth with antiseptic agents at least 5 times a day, especially after eating. At least 3 times a day, applications with wound healing and anesthetic agents should be applied to the lesions. To avoid injuring damaged areas, teeth should be brushed carefully, using brushes of minimal hardness and a paste containing chlorophyll. The food should be liquid or pasty.
Folk remedies
Treatment of leukoplakia is also possible with folk remedies. For disinfection, decoctions and infusions of chamomile, calendula, and sage are used. To speed up healing, wounds are lubricated with cabbage, aloe, yarrow juice, sea buckthorn or rosehip oil.
Folk remedies can increase the body's resistance to harmful environmental influences and strengthen the strength to fight diseases. To increase immunity, herbs and berries are used - teas are prepared from St. John's wort, elecampane, oregano, lingonberries, raspberries, currants, and rowan. Freshly prepared juices are effective - carrot, cabbage, apple. In order not to unnecessarily irritate the mucous membrane, they need to be diluted with water. Folk remedies are used as an addition to the main treatment of leukoplakia.
READ ALSO: What protects the oral mucosa?
Erosive leukoplakia
In the absence of timely treatment for simple and verrucous forms of leukoplakia, the patient’s condition becomes more complicated, the disease passes into another form - erosive. This result is due to the presence of traumatic factors that are constantly present and are not eliminated.
The erosive process is manifested by pain, which becomes more pronounced when exposed to irritants. In the case of the development of complicated verrucous or simple leukoplakia, when examining the problem area against the background of existing whitish spots, erosions, cracks, and ulcers can be detected. It is worth noting that erosions are difficult to treat and constantly re-form.
The greatest discomfort for the patient is caused by damage to the red border of the lips, which is associated with their vulnerability to the influence of external factors. Constantly exposed to irritants, the inflamed mucous membrane is not restored, its condition worsens, and the pain becomes stronger.
Diagnostic measures
Dentists are able to identify the disease visually and by palpation. For an accurate diagnosis, it is necessary to perform a diagnosis. The following studies are performed: cytology, biopsy, analysis of biological fluid from a vein for the Wasserman reaction, other studies are prescribed as necessary.
It is important to exclude the presence of other diseases. Taking into account the characteristic features of leukoplakia, differential diagnosis is made with individual pathologies.
Chronic hyperplastic candidiasis affecting the oral cavity . After the transition to the chronic form, similarities between the symptoms of the disease and the manifestations of leukoplakia are noted. The main difference between candidiasis is the ability to remove plaque. In addition, in this case the tissues become cloudy and do not undergo hyperkeratosis.
Lupus erythematosus . The affected tissues turn red and atrophy; with leukoplakia, such manifestations are absent.
Lichen planus . An inflammatory reaction is observed that spreads to the skin, which is not typical for leukoplakia.
Bowen's disease . With the development of this pathology, the affected areas are pasty, hyperemic, covered with a layer of plaque that can be removed. After cleansing, red, rough tissue is observed.
Limited precancerous hyperkeratosis . The tissue is covered with scales and, in altered areas, sinks at a central point. To make a final diagnosis, it is necessary to have histological results.
Secondary syphilis . The fabric is covered with bubbles and a white coating that is easily removed. In addition, the affected areas are characterized by infiltration. The diagnosis is made taking into account the results of a blood test.
Diagnosis of oral leukoplakia
First, the doctor examines the oral cavity and palpates the affected areas. It is important to study the patient’s medical history, as well as clarify his health status and the presence of chronic diseases.
To confirm the diagnosis, it is necessary to perform a biopsy of the changed tissues and conduct a cytological analysis. If the need arises, the doctor prescribes additional tests for the patient.
It is important to carry out differential diagnosis with such pathologies as:
- Chronic candidiasis of the oral cavity.
During a fungal infection, the affected tissues will be well separated, and regenerated cells will be found underneath them.
- Lichen planus.
It concentrates not only in the mouth, but also on the skin.
- Systemic lupus erythematosus. Fabrics
atrophy, foci of inflammation have a rich red color.
- Bowen's disease. Plots
mucous membranes are red, pasty. Removing plaque is not difficult, but underneath it you can see rough red spots. The skin is affected, not just the mucous membranes of the oral cavity.
- Erythroplakia.
Damaged tissues turn red and itch. The spots reach 20 mm in diameter, have clear boundaries, and are located on the tongue near the throat. Sometimes they form on the labia, near the vagina. This disease, like leukoplakia, can become malignant.
- Leukopenia.
With this pathology, ulcerative defects form in the oral cavity. They can appear not only in the mouth, but also on the walls of the intestines. The patient's body temperature rises, weakness increases, and he is haunted by a headache. The tonsils swell and hurt, the spleen increases in size.
- Pachydermia.
With this disease, plaques form on the mucous membranes of the larynx, which in appearance resemble warts. They also form on the vocal cords. The color of the plaques is yellow or whitish-gray. The mucous membrane becomes loose and has a blue color.
- Pachyderma of the head.
The scalp suffers from this disease. It becomes covered with folds, the skin thickens. Due to the disease, the surface of the head begins to resemble the brain.
- SOPR.
This pathology affects the mucous membrane of the oral cavity. The cause of its development may be lichen planus, viral infections, and stomatitis. If the pathology is not treated, it threatens to turn into a cancerous tumor.