Pancreatic necrosis (acute pancreatic necrosis) is a condition in which the pancreas dissolves in its own secretion.
All enzymes are released simultaneously, especially proteolytic, amylase and lipase, enzymes that destroy the structure of adjacent organs and tissues. This condition is very dangerous and threatens the patient’s life. Symptoms and clinical manifestations require urgent surgical intervention, the probability of death from pancreatic necrosis is 30-80%. Typically, the risks of necrosis increase in older people, with a long course of the disease and with impaired diet and life.
Normal anatomy and morphology
Relevance of the problem and epidemiology
Symptoms of pancreatic necrosis indicate a borderline state of the patient. This is a pathology that every surgeon should know about its treatment.
This syndrome is a severe complication of acute pancreatitis. As the underlying disease progresses, the organ ceases to resist the effect of pancreatic enzymes, which begin to digest the organ and destroy its structure.
According to statistics, most complications occur in patients suffering from alcoholism, less often due to other intoxications and infections. Alcoholism – 70%, 30% etiology is cholelithiasis of various etiologies.
The need to study this problem is that chronic pancreatitis is increasingly aggravated by necrosis of the pancreas, which increases mortality.
Appearance of the organ during necrosis
Prevention
Proper nutrition, quitting smoking and drinking alcohol, and leading an active lifestyle help prevent the development of pancreatic necrosis. It is necessary to promptly treat diseases of the digestive system, remove stones from the gallbladder, and restore the functions of the pancreas.
Among the most common diseases of the pancreas, characterized by a sudden onset, there is such an ailment as necrosis, which in medical terminology is called acute hemorrhagic pancreatitis. This pathology poses a potential danger to human life. In some cases, death cannot be ruled out.
General information about the disease
Chronic pancreatitis is a multifactorial disease that manifests itself with periods of remission and exacerbations. During remission, the clinic is erased, and the pain feels relatively satisfactory.
During exacerbations of life, the patient is at risk of multiple organ failure, which occurs due to the release of many enzymes into the abdominal cavity.
Mortality increases with age and the presence of comorbidities. Risk factors for complications of pancreatitis with necrosis:
- Elderly age;
- Chronic alcoholism, drug addiction;
- Female gender (more often affects postmenopausal women);
- Reduced general resistance of the body (with chronic concomitant diseases, organ failure);
- Late diagnosis, incorrect assessment of the patient’s condition, development of peritonitis, sepsis, shock.
The prognosis improves if organ death is diagnosed in a timely manner and correct treatment is carried out.
Stages of development of acute pancreatitis
Causes of hemorrhagic pancreatitis
The reasons for the development of acute hemorrhagic pancreatitis are the following:
- intoxication of the body due to food poisoning;
- improper nutrition: abuse of spicy, fatty and fried foods, marinades and smoked meats;
- development of an allergic reaction due to certain reasons;
- intestinal flu;
- violation of the functional characteristics of the pancreas;
- drug overdose;
- injuries in the back and abdominal area.
The disease can affect people at any age, regardless of gender. According to medical statistics, hemorrhagic pancreatitis most often develops in men at a young age, especially in those who are prone to gaining excess weight and abusing alcohol. The process of development of the disease itself is accompanied by activation of trypsin in the pancreas, while in a normal situation this should occur only in the internal cavity of the intestine.
In most cases, the development of acute hemorrhagic pancreatitis occurs instantly and is accompanied by acute pain radiating to the lumbar region. And its main location is the pancreas.
Etiology
List of diseases that can cause the development of pancreatic necrosis:
- Chronic pancreatitis of various etiologies, evolution and stages;
- Long-term diabetes mellitus, with the development of total insulin deficiency and dependence on exogenous insulin;
- Acute intoxication, in particular alcohol poisoning, can occur with a single use or due to prolonged abuse;
- Infections that cause bacteria to migrate through the bloodstream (septicemia);
- Sepsis and multiple organ failure;
- Trauma to the organ, release of enzymes beyond the gland and the development of autodigestion.
It is worth understanding that all of the above reasons in themselves are serious pathologies that lead to life-threatening complications, pancreatic necrosis is one of them.
Treatment of pancreatic necrosis
Therapy of pancreatic necrosis is carried out exclusively in a medical institution. The patient must be provided with complete rest, avoid eating any food and apply a cold compress to the pancreas area. Conservative treatment of pathology includes the use of the following medications:
- antispasmodics and narcotic analgesics to eliminate pain;
- drugs that block the activity of the pancreas (proton pump inhibitors, antienzyme drugs, anticholinergics); in the absence of cholelithiasis, choleretic drugs are prescribed;
- antibiotics to fight a bacterial infection that develops when the pancreas is damaged;
- somatostatin is a hypothalamic hormone that suppresses the production of gastric juice and prevents the development of bleeding in the internal organs;
- glucose with insulin and saline solution are administered to remove from the body aggressive substances that enter the blood from the affected pancreas.
If there is no effect from conservative therapy, patients are shown surgical intervention - restoring the function of the pancreatic ducts, removing foci of dead tissue, removing excess fluid from the abdominal cavity, stopping internal bleeding. As a rule, surgical intervention is postponed for several days until the acute manifestations of the disease are stopped. Immediate surgery is necessary only in severe cases - with the development of total organ damage or purulent-septic processes.
For reference: surgical intervention performed for pannecrosis can negatively affect the patient’s entire subsequent life - sometimes during the operation it is necessary to remove neighboring organs. If it is not possible to stop the process of destruction of pancreatic tissue, the patient will need another operation.
Pathogenesis
Due to the influence of the etiological factors listed above, inflammation of the organ develops, various cells migrate to it, infiltrate the organ and secrete inflammatory factors, platelets, and clotting factors.
The pathogenetic process is an aseptic, that is, sterile, uninfected decomposition, necrosis of pancreatic cells, as a result of which all secreted enzymes are released and affect nearby tissues and organs.
Necrotic lesions spread and lead to the following consequences:
- Bleeding;
- Multiple organ failure;
- Increased thrombus formation;
- Fatty infiltration;
- Calcium deposits;
- Proliferation of fibrous tissue.
The most dangerous signs:
- Drop in blood pressure;
- Tachycardia, arrhythmia, cardiac arrest;
- Fluid retention in the body due to kidney failure;
- Metabolic acidosis;
- Impaired consciousness up to coma;
- Intestinal obstruction.
Epidemiology
Classification
Various classifications give an idea of the severity of the lesion and methods of further treatment.
By lesion size:
- Small lesions are diffuse;
- Large lesions;
- Subtotal defeat;
- Total damage.
Infection with bacterial flora can also lead to a necrosis process, in which case the pathology is characterized as infectious.
Based on the nature of the pathological process that predominates, the following types of pancreatic necrosis are distinguished:
- Fatty;
- Hemorrhagic;
- Mixed.
Stages of necrosis:
- Toxemia (release of all coagulation factors, toxins into the blood with a serious toxic-infectious syndrome or shock);
- The formation of an abscess, which has its own stages;
- Spread of necrosis to adjacent tissues.
Classifications determine the tactics of the operation and show what preliminary treatment is necessary to stabilize the patient and ensure the correct dose of anesthesia and painkillers.
Types of operations
Clinical picture
Symptoms of pancreatic necrosis of the pancreas can be bright, similar to a state of shock; in some situations, especially in older people and in patients in a decompensated state, the blade may not be so pronounced, which can mislead doctors and lead to underestimation of the severity of the condition.
Classic symptoms:
- Severe pain in the left hypochondrium;
- Fountain vomiting, frequent, leading to dehydration and metabolic acidosis;
- Decreased blood pressure;
- Severe weakness, impaired consciousness;
- Pale skin, increased sweating;
- Diarrhea or constipation, up to intestinal obstruction;
- Peripheral edema (of the lower extremities), as well as ascites, pleural effusion, cardiac tamponade, cerebral edema.
The clinic can lead to coma and shock, which is why the patient must be transferred to the intensive care unit and urgently prepared for surgery. Surgical treatment is contraindicated if the general condition is unstable; it is necessary to minimize the risks of death during surgery for pancreatic necrosis.
Alcoholism, types, signs, consequences, treatment
Rehabilitation after treatment of pancreatic necrosis
After treatment for pancreatic necrosis, the patient remains incapacitated for some time - if treatment is limited to conservative therapy, the recovery period takes several weeks, after surgery it increases to 3-4 months.
The most important part of rehabilitation is proper nutrition - at first you are allowed to eat crackers, unsweetened tea, pureed soups with vegetable broth. Next, the patient can switch to a gentle diet containing the following products:
- stale bread, unhealthy pastries;
- lean fish and meat, chopped and steamed;
- vegetable broth soups, to which you can add small vermicelli and cereals;
- vegetable and butter, no more than 10 and 20 g per day, respectively;
- dairy products;
- soft (ripe or overripe) fruits without peel and seeds;
- dried fruit compotes;
- egg white omelettes;
- herbal infusions.
Food should be steamed or boiled, and taken several times a day at the same time in small portions - hunger or overeating should not be allowed. Prohibited products include:
- fatty, smoked and salty dishes;
- products containing chemical additives;
- semi-finished products and fast food;
- fruits and vegetables that promote fermentation and gas formation in the intestines (legumes, cabbage, spicy and sour fruits);
- sweets, especially cakes, pastries, pastries, chocolate.
In addition, the patient should give up smoking, alcohol, heavy physical activity, reduce the amount of stress and spend time in the fresh air as often as possible. If symptoms of pancreatic necrosis develop again, you should consult a doctor as soon as possible - they may indicate a relapse of the disease or the development of complications.
Often, a person who has suffered from this disease has to change jobs or give up work altogether. He is registered with a dispensary, and every few months blood sugar tests and instrumental examinations of the pancreas are carried out in order not to miss the development of complications.
Prevention of pancreatic necrosis is to prevent the development of pancreatitis, for which the following rules must be observed:
- eat a balanced diet;
- lead a healthy lifestyle;
- stop drinking alcohol;
- promptly treat gastrointestinal diseases, inflammatory processes in the body, helminthic infestations;
- Do not take medications without consulting a doctor.
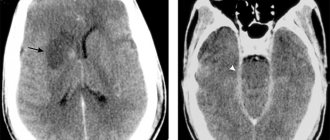
Diagnostics
Due to the rapid development of the clinic, the patient is hospitalized in the intensive care unit.
The first important step in making a diagnosis is the characteristic clinical picture and external signs. During a general examination, the doctor should perform basic maneuvers:
- Measurement of pulse, pressure, blood oxygen saturation, body temperature;
- Examination of the skin for color, moisture, turgor, presence of rash;
- Auscultation of the lungs, determining the presence of edema;
- Auscultation of the heart, it is necessary to ensure the absence of insufficiency;
- Palpation of the abdomen, determination of intestinal patency;
- Determination of the Shchetkin-Blumberg symptom, the presence of peritonitis;
- Differential diagnosis with perforation of an ulcer of the digestive tract, appendicitis, cholecystitis.
Paraclinical methods and instrumental tests:
- Complete blood count, information about volume levels, presence of infection;
- General urine test, kidney condition, separately for amylase in urine;
- Biochemical blood test (kidney, liver, pancreas, heart enzymes);
- X-ray examination of the abdominal organs (indirect signs);
- Ultrasound examination (determines the presence of destruction, necrosis, inflammation);
- CT scan;
- Magnetic resonance imaging;
- Angiography;
- Diagnostic laparoscopy;
- Endoscopic studies.
In severe critical condition, diagnostic procedures should take a minimum of time. An ultrasound and CT scan are prescribed, as a result of which the cause is established, and the patient is sent to prepare for surgery.
Pathological specimen
Complications
The difficulty in treating the pathology is that complications occur quickly; the patient can be taken to the hospital already in shock or in a coma. Possible consequences:
- Hypovolemic shock;
- Toxic, septic shock;
- Acute heart failure;
- Renal acidosis;
- Coma;
- Hypotension, collapse;
- Failure of several organs at the same time.
It is the complications that lead to death and increase the risk of chronic consequences:
- Chronic renal failure;
- Anemia after large blood loss;
- Diabetes;
- Chronic insufficiency of pancreatic enzyme secretion;
- Indigestion, symptomatic ulcers.