Causes of the disease
The cause of anular granuloma still remains unknown. Basically, there are several factors that can lead to the development of the disease:
- inherited predisposition (granulomatous diseases in relatives);
- the presence of severe systemic diseases (diabetes mellitus, rheumatism, tuberculosis, sarcoidosis);
- minor skin injuries;
- burns;
- herpes zoster;
- papillomas;
- impaired fat metabolism;
- the body's predisposition to allergies.
Treatment of granuloma annulare (in adults and children) will be discussed below.
Granuloma can be of two types - typical and atypical. Atypical has several varieties:
- localized. Papules are isolated from each other;
- disseminated. A large lesion is observed;
- subcutaneous The rash nodules are located deep under the skin. This granuloma often appears in children;
- erythematous. A wide rim of inflammation forms;
- perforating. Leaves scars after healing.
There are cases when this disease occurs at the site of tattoos and scars.
Causes of granuloma annulare
Granuloma annulare is still a mystery to researchers.
At this stage of medicine, scientists still do not know what causes the formation of these granuloma nodules on human skin.
Although it is not yet possible to name a single cause, recent research into this disease indicates that the occurrence of granuloma annulare may be associated with the following factors:
1. Granuloma annulare appears due to chronic infections: sarcoidosis, tuberculosis and rheumatic diseases. If the cause of granuloma annulare is the presence of these chronic infections, then granulation itself is considered as a result of changes in tissue reactivity.
2. Hereditary predisposition to this chronic disease.
3. There is a possibility that the disease occurs due to various skin lesions. For example, cuts or burns.
4. A relationship between the occurrence of granuloma annulare and diabetes mellitus was noted.
5. Allergic reactions of the body to various pathogens. Initially, allergies are considered by doctors as one of the prerequisites for granuloma annulare. Most likely, before nodules appear on the body, a person experiences an allergic reaction.
Prognosis and consequences of the disease
Granuloma annulare is not dangerous to life or ability to work. In most cases, it disappears spontaneously and does not require special treatment; rarely, small scars remain after papules. To reduce the likelihood of relapse of the disease, it is necessary to follow the rules of a healthy lifestyle and strengthen the immune system.
Granuloma annulare (anular granuloma) is a chronic and recurrent progressive dermatosis of unknown origin. The disease is characterized by the appearance of ring-shaped nodules with collagen destruction and a granulomatous inflammatory reaction. Lesions can appear at any age.
Causes
The causes of the disease remain unclear. It is believed that chronic infections (sarcoidosis, tuberculosis, rheumatism) play a certain role in its development. In this case, the granulomatous process is a consequence of changes in tissue reactivity.
Allergic reactions are also considered to be prerequisites for the occurrence of granuloma annulare. It is known that there is a connection between connective tissue diseases and granuloma annulare. A connection between the disease and diabetes mellitus and changes in carbohydrate metabolism has been noted.
The cause of the disease in children is considered to be changes in the immune system. Granuloma annulare in children appears after shingles and warts, as well as at the site of scars and tattoos.
Symptoms of granuloma annulare
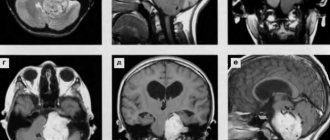
Initially, dense, smooth, shiny papules of red-pink, purple or flesh color appear on the skin. There are no subjective sensations. After a few months, the papules can form a ring-shaped plaque, which gradually increases in diameter and reaches 0.5-10 cm. In the center, the plaque has a normal skin color or a slightly bluish color. Very rarely, ulceration of the lesions occurs.
Most often, lesions are located on the back surfaces of the hands, elbows, knees, and feet. Rarely localized on the neck, buttocks, and forearms. In childhood, granuloma annulare appears on the joints of the feet.
Diagnostics
Diagnosis is based on clinical manifestations and often does not require additional research. In doubtful cases, a skin biopsy is performed with histological examination of the material.
Classification
There are several clinical forms of anular granuloma:
- Subcutaneous. Typical for children under 7 years of age. Rashes appear on the scalp, on the skin of the legs, forearms, and hands; sometimes in the eye area.
- Localized. A common form of granuloma annulare in children. Most patients develop a single lesion on the extremities. Less commonly, rashes appear on other parts of the body (for example, in the area of large joints). The rashes look like dense papules the color of healthy skin; in the center of the lesion the skin is usually normal.
- Disseminated. This form usually occurs in adult patients. Rashes appear all over the body in the form of papules the color of healthy skin or with a purple tint. Most often, rashes appear on the skin of the legs, arms and torso.
- Perforated. A rare type of anular granuloma. More often, rashes appear on the fingers and skin of the hands. The rash looks like papules with horny plugs and jelly-like contents. As the contents are released, the rash transforms into crusty elements with an indentation in the center. Scars may subsequently form at the site of the rash.
Patient Actions
If symptoms of granuloma annulare appear, it is recommended to consult a dermatologist to clarify the diagnosis and determine the appropriate treatment.
Treatment of granuloma annulare
Treatment includes correction of carbohydrate metabolism and treatment of concomitant pathologies. It is recommended to take medications to improve microcirculation and vitamins. An effective technique for injecting foci of granuloma annulare with triamcenolone acetonide, dapsone, and hydroxychloroquine. A course of ointments with a high concentration of topical steroids is prescribed.
Granulomas are treated with cold (irrigating the affected skin with chlorethyl).
Treatment with conservative methods is effective. Also, granuloma annulare can regress on its own.
Complications
Psychological discomfort caused by a cosmetic defect.
Prevention of granuloma annulare
Prevention of the formation of annular granulomas consists of timely diagnosis and treatment of chronic infectious diseases and metabolic disorders. It is also necessary to protect the skin from damage.
Kinds
A typical form of the pathological process affects the epidermis of the knees, dorsum of the feet, hands, buttocks, forearm, and cervical region. Atypical granulomas include:
- Localized, when dense nodules accumulate on the surface of the skin.
- Common, developing in adults. The disseminated form is manifested by multiple rashes and purple papules. This type of disease requires long-term therapy.
- Subcutaneous, affecting areas near the joints, scalp, upper eyelids. Most often, this granuloma affects girls under six years of age.
- Papular. With this type of disease, single lesions occur.
- Perforating, occurring after mechanical damage. In the center of the ring there is a plug, from which a jelly-like discharge sometimes comes out. After treatment, a crust forms, then the affected skin becomes covered with scars.
According to the morphological structure, papules are interstitial and frontal. In the first case, the pathological process is observed in the intercellular space of the dermis in a chaotic manner. Palisade granuloma is characterized by a fence-like accumulation of lymphocytes and proteins in the papillary layer of the epidermis.
Granuloma annulare causes
Granuloma annulare is a disease that belongs to the idiopathic group. This means that the nature of the disease is not fully understood. The probable cause of nodules is autoimmune inflammation in the skin layers against the background of a viral or bacterial infection. The multifactorial nature of the pathology is confirmed by the discovery in patients of chronic inflammatory processes in the form of tuberculosis infection, sarcoidosis and acute rheumatic fever and the connection of the disease with autoimmune processes of the thyroid gland and diabetes mellitus. The onset of the disease may be preceded by infection with Epstein-Barr viruses, herpes simplex, chickenpox or human immunodeficiency virus. The course of HIV infection is severe and widespread.
The association of granuloma annulare with long-term use of certain medications (vitamin D) and vaccination has been confirmed. There are known cases of rashes appearing against the background of BCG and the Mantoux test. The main component of pathogenesis is considered to be delayed hypersensitivity, or type IV, because it is characterized by the development of an allergic reaction within a few days after exposure to the allergen and a sluggish course.
Diagnostics
Due to the specific clinical manifestations, the diagnosis is often made after an external examination by a specialist. To clarify the type of pathology, biological material is taken for subsequent histological examination.
In the focal center, deformed protein fibers are localized, which are surrounded by an infiltrate consisting of lymphocytes. In the affected skin, a granulomatous inflammatory process is clearly visible.
In addition, the patient must undergo a general blood test and be checked for the presence of human papillomavirus, syphilis, and sexually transmitted infections in the body.
In addition, differential diagnosis is still important, since the symptoms of granuloma annulare are similar to the manifestations of syphilis, lichen, sarcoidosis, and rheumatoid arthritis. If alarming signs appear, you should immediately visit a dermatologist.
Prevention
Prevention of granuloma annulare consists of timely identification of foci of skin infection and their elimination. It is necessary to monitor metabolic processes in the body and maintain immunity at the proper level. And also avoid damage to the skin, hypothermia and overheating.
If pathological symptoms appear, consult a doctor.
To see new comments, press Ctrl+F5
All information is presented for educational purposes. Do not self-medicate, it is dangerous! Only a doctor can make an accurate diagnosis.
Hello, my daughter has some spots on her leg that look like a bruise. In the skin and venous disp. visually determined that it was granuloma annulare. No treatment was prescribed, they said that it would disappear over time, but more than a year has passed and everything is in the same place. What should we do?
Granuloma annulare can exist for years and disappears on its own. What it is is unclear, and why it appears is also unclear.
Symptoms of granuloma annulare
Most often, such lesions appear on the hands, forearms, legs and feet (sometimes in the area of the knee and elbow joints). The formation consists of papules in the shape of a ring or arc, with healthy skin in the center.
The process rarely involves an area of skin larger than 5 cm in diameter, but there are exceptions. An atrophic or keloid scar may form in place of the disappeared lesion. There should be no itching or pain.
How to clarify the diagnosis
Dermatologists determine this nosology (as in your case) offhand; to clarify, they perform a skin biopsy followed by histology. In the field of view of the microscope, foci of dead cells with mucin deposits, multinucleated cells in tissues, and signs of granulomatosis are visible. Simply put, it is not difficult to clarify the diagnosis.
A biopsy is performed for differential diagnosis with a fungal infection, lichen planus, or basal cell carcinoma. Basalioma in children is extremely rare and grows slowly. The rest does not pose a health hazard (even if the doctor made a mistake with the diagnosis).
Treatment of granuloma annulare
The process itself has no meaning. Only associated infections are treated.
To improve tissue metabolism, vitamins (A, D3, B, C) are prescribed, lesions are injected with hydroxychloroquine, dapsone, traditional methods are used, etc. Steroid (hormonal) ointments can be prescribed - in a word, “who knows what,” since the cause and pathogenesis of the disease is not clear.
Prognosis and prevention
The prognosis is favorable, it is recommended to wait and not worry about it. There is no adequate treatment - it is not worth wasting time and money on it. If the spot begins to grow, see a dermatologist for differential diagnosis. If a basal cell carcinoma is detected, oncologists will remove it (this tumor relatively rarely metastasizes, don’t worry).
Many diseases are accompanied by skin rashes. Among them there are those whose reasons for their development have not yet been fully studied. This group of diseases also includes granuloma annulare, a chronic dermatosis of unknown etiology.
Dangerous or not
Pyogenic granuloma causes discomfort to many patients. We have already clarified what it is, but does it pose a danger to human health? The neoplasm is often compared to malignant lesions, such as melonomas, fibromyxomas, and carcinomas. After removal of the lesion, it is sent for histological examination, which makes it possible to exclude the malignant origin of the granuloma. It is possible to prevent a dangerous condition if you seek help from a specialist in time and do not self-medicate.
Benign neoplasms include cherry hemangioma (a small bright red lesion of capillaries); fibrous papule localized on the nose and bacillary angiomatosis (an infection that consists of four nodular lesions and reaches a size of ten centimeters). All of these neoplasms are similar to granuloma, so it is best to diagnose the tumor in a clinical setting. The doctor will conduct a visual examination, histology and other tests.
Table A1 - Levels of evidence
| Levels reliability of evidence | Description |
| 1++ | High quality meta-analyses, systematic reviews of randomized controlled trials (RCTs) or RCTs with very low risk of bias |
| 1+ | Well-conducted meta-analyses, systematic ones, or RCTs with low risk of bias |
| 1- | Meta-analyses, systematic, or RCTs with a high risk of bias |
| 2++ | High-quality systematic reviews of case-control or cohort studies. High-quality reviews of case-control or cohort studies with very low risk of confounding effects or bias and moderate probability of causality |
| 2+ | Well-conducted case-control or cohort studies with moderate risk of confounding effects or bias and moderate probability of causality |
| 2- | Case-control or cohort studies with a high risk of confounding effects or bias and a moderate probability of causality |
| 3 | Non-analytical studies (eg case reports, case series) |
| 4 | Expert opinion |
Characteristics of the disease
Granuloma annulare is a complex type of skin pathology that is still under study. It is characterized by rashes in the form of nodules or compactions of different sizes. The disease may manifest itself without pain, but as it develops, the pain progresses or disappears completely. The nature of the pathology is benign with a chronic course.
The shape of skin rashes can be round or oval, resembling nodules. When formed, compactions appear in a chaotic manner. After some time, the rashes may disappear on their own.
A papule occurs on any part of the body. In medical practice, granulomas are more often diagnosed on the face, in the area of the hand, finger, elbow and on the leg (foot and knees). A person may not notice a suspicious spot for a long period of time.
During the process of growth and maturation, the compaction accumulates collagen, which leads to inflammation inside the diseased tissues and forms a kind of ring of nodules. Pathomorphology calls this manifestation “granuloma,” which gives the name of the pathology – granuloma annulare. An unknown nodule on the skin often does not cause discomfort - there is no itching or burning, and no painful sensations are observed either.
Granuloma annulare
The ICD-10 pathology code is L92.0 “Annular granuloma.” The disease can occur in adults and children. Women and small children suffer from skin rashes more often.
How to prevent the development of granuloma annulare
There are no special ways to prevent this disease. But you should try to avoid the influence of those factors that give impetus to the manifestation of the disease.
If infectious or inflammatory processes develop in the body, they need to be treated promptly. Any abnormalities in metabolism must be identified in a timely manner and supportive therapy carried out. Patients with diabetes should be monitored regularly by their physician.
Immunity needs to be strengthened, especially in children, since their defense mechanisms are not yet sufficiently developed. Maintaining a healthy lifestyle reduces the risk of shifts in the human immune system and the appearance of autoimmune diseases such as rheumatism, sarcoidosis, thyroiditis and others that affect connective tissue.
Preventing tuberculosis can also reduce the likelihood of developing granuloma in both adults and children. You should try to avoid any wounds to the skin. If the disease has already appeared, contamination of the affected areas of the body should not be allowed.
In the article we tried to consider all variants of this disease, incl. and granulomas photo. We want to believe that the article helped you!
Treatment
Treatment of granuloma annulare is carried out using the following methods:
- When concomitant diseases are identified (chronic infections, metabolic disorders, etc.), their persistent treatment is necessary.
- Drugs are used to improve microcirculation - Retinol, Tocopherol, Ergocalciferol.
- Vitamin therapy is prescribed - B vitamins, ascorbic acid.
- A fairly effective technique consists of injecting foci of granuloma annulare with Dapsone, Triamcinolone Acetonide, and Hydroxychloroquine.
- Ointments with a high concentration of topical steroids are used. These drugs are prescribed in short courses with breaks.
- Granulomas are also treated with cold. For example, the affected skin is irrigated with chlorethyl until a layer of “frost” forms on the skin. The procedures are carried out once a week, the full course is 3-5 procedures for each of the granuloma lesions.
Treatment with traditional methods
Celandine tincture is used to treat the disease.
There are also folk recipes that can help in the treatment of granuloma annulare.
Treatment of granuloma with celandine tincture. You need to buy or prepare a 30% celandine tincture yourself and mix it with an equal amount of pharmaceutical glycerin. Soak a cotton pad or a piece of gauze in the resulting mixture and apply a compress to the lesions of granuloma annulare. Keep the compress for at least 2 hours. By the way, a plant such as celandine effectively helps in the treatment of candidiasis of the skin of the inguinal folds, viral exanthems, mycosis of the skin of the hands, etc.
Treatment of granuloma with sea salt. Take sea salt, grind it in a coffee grinder to obtain a fine powder and mix with egg yolk until creamy. Apply to the affected areas for half an hour, then wash off the application and lubricate the skin with Vaseline or nourishing cream.
Treatment options
The course of treatment for granuloma annulare in children depends on the individual characteristics of the child’s body and the presence of concomitant diseases. In most cases, specialists use wait-and-see tactics .
Drug therapy is prescribed if there is no tendency to cure the disease on its own.
In addition to medications, special procedures can be used. These include liquid nitrogen, carbonic acid snow or irrigation of the affected area with Chlorethyl.
When treating granuloma annulare in children, the following types of drugs are used:
- means for improving blood microcirculation (Tocopherol, B vitamins, Retinol, iron supplements, Ascorbic acid);
- non-steroidal local agents (Phenylbutazone, Indomethacin);
- corticosteroid ointments (Psoriderm);
- hormonal ointments (Triderm, Dermovate);
- topical glucocorticoids (Hydrocortisone, Betamethasone valerate);
- drugs for injecting foci of the disease (Acetonide, Diapsone).
Folk remedies
When using traditional medicine to treat granuloma annulare in children, it is important to consider that this disease may be of an allergic nature .
The selection of alternative medicine recipes is carried out with the exclusion of ingredients that can aggravate the body's reaction to certain irritants.
For example, you should not use products based on honey, berries that can cause allergies, or other components with similar properties.
Examples of folk remedies used in the treatment of granuloma annulare in children:
- Celandine and glycerin . Mix pharmacy glycerin and 30% celandine tincture in equal quantities, use the resulting product to make compresses on the skin lesions, carry out the procedure once, preferably before bedtime.
- Herb tea. Mix five tablespoons of rosehip leaves with one tablespoon of crushed elecampane roots, pour boiling water over the preparation and boil for fifteen minutes, drink the resulting product as tea once a day.
- Radish, carrots and lemon juice.
Mix 200 ml each of radish and carrot juice, add one tablespoon of lemon juice.Take the product three times a day, one tablespoon at a time.
Types of pathology
Many doctors believe that granuloma annulare is a dermatosis with an unclear manifestation pattern. The appearance of a foreign spot on the skin should not be left without treatment - this can have unpleasant consequences for health.
The disease is classified according to the degree of proliferation of skin rashes and the distinctive characteristics of pathological nodules. The course of therapy depends on the type of pathology. Some forms can disappear on their own without requiring medical intervention.
The following types of disease are distinguished:
- The localized form occurs mainly in children. It occurs without pain, there is no itching or burning. Capable of self-healing.
- Subcutaneous granuloma affects children under 6 years of age. The papule is connected to nearby tissues, which can be characterized by deep germination into the deep layer of the skin.
- The perforating form differs from the localized form by the presence of a capsule that periodically secretes a yellowish liquid.
- The perforating appearance often occurs in the fingers and hand. The skin at the site of papule formation becomes lighter in color. Occurs mainly in childhood.
- The disseminated form is typical for adults. Children rarely get sick. The nodules spread throughout the body, affecting large areas. The ring form of the formation is often absent - nodules appear singly in a chaotic manner.
- The middle type is characterized by aggressive growth and proliferation throughout the body. Characterized by severe symptoms, urgent treatment is required.
- The cholesterol type is rare. It is characterized by inflammation of the bone of the temporal lobe of the skull caused by trauma or otitis media of the middle ear.
- The vascular form is papules containing a large number of blood vessels.
- Epithelioid granuloma is formed from epithelioid fiber cells.
- The purulent form is characterized by the development of nodules with purulent inflammation.
- The ligature form is a manifestation of pathology at the site of the postoperative suture. The reason for this is a foreign particle in the tissue.
- The sarcoid type is formed in the tissues of the lymph nodes and in the area of internal organs.
- The syphilitic form is a complication of severe syphilis.
- Tuberculosis granuloma occurs in the tissues of the respiratory tract when a pathogenic particle enters the lungs and bronchi.
- The giant cell species affects bone tissue. The nodules do not grow, remaining in the formation zone.
- The calcific form is characterized by the accumulation of calcareous deposits in the area where the nodule appears. The calcified form is treated with drug therapy.
The disease is divided into two types - typical and atypical granuloma. The typical form is localized pathology. All other types are classified as atypical forms.
Preventive measures against pathology
The exact causes of the disease are still unknown to doctors. Therefore, it is difficult to decide on the prevention of pathology. The difficulty lies in the spontaneous disappearance of the seals.
It is recommended to perform the following procedures to help prevent the development of dangerous papules:
- It is worth taking medications that enhance immunity.
- Promptly treat skin and other diseases that can provoke granuloma.
- It is recommended to treat allergies at an early stage of formation.
- Prevention of infectious and viral pathologies will prevent illness.
- Balance your diet – increase foods with plant fiber.
- Take vitamins regularly.
If you follow the rules of prevention, this will avoid the formation of papules on the skin. The disease does not cause serious consequences, but it does cause psychological and cosmetic discomfort. Therefore, when the first suspicious symptom appears, you need to consult a doctor and undergo an examination. Early treatment helps avoid other complications.
Select the city, desired date, click the “find” button and make an appointment without queuing:
Treatment of granuloma annulare
The effectiveness of granuloma treatment is based on the observational method. The disease is usually asymptomatic, so therapy is only necessary to get rid of a cosmetic defect.
There are cases when the doctor may advise you to follow a wait-and-see approach: the lesions go away on their own in about 6 to 18 months. It usually turns out that the effect of medications appears only against the background of self-treatment of the disease.
Drugs used in the treatment of granuloma:
- Hormonal-type drugs in the form of injections around the lesion - “Kenalog” 3-5 mg/cm3. in 4 injections.
- In cases where pain and discomfort from the rash appears, ointments of the corticosteroid group are used topically: Mometasone-Elocom, Akrikhin, Momat. Use daily for the first 2-3 weeks, and then once every 2-3 days.
- Anti-inflammatory ointments containing tacrolimus, which block skin atrophy: “Protopic”, “Tacropic”. Use 1-3 times a day for 6 weeks.
- Periodic retinoids help normalize the regenerative function of the skin: “Acnecutane”, “Roaccutane”, “Retasol” at a dose of 0.5-1 mg/kg every day for 3-4 weeks.
- Vitamin therapy: B vitamins, vitamin A 5000 IU, vitamin E 400 mg daily for 2-3 months.
- Cryotherapy with liquid nitrogen leads to remission in 80% of cases. This complication of treatment can lead to scarring.
- UVAL phototherapy cures granuloma annulare with approximately a 50% success rate. To achieve the greatest effect, 4-5 sessions are necessary.
- There are cases when recovery is facilitated by scarification cuts made at the site of the lesion.
In addition, a diet based on carbohydrate restriction is prescribed as additional therapy. The consumption of flour products, sweets, pasta, fast food, etc. is prohibited.
The patient must remember that this disease can be cured on its own. Although the rash is unpleasant, it is best to let the granulomas disappear naturally as there are side effects with any of the above methods.
But when the patient nevertheless chooses therapeutic treatment, he must undergo it under the strict supervision of a doctor.
Diagnosis and treatment of granuloma annulare
Clinical manifestations of the disease are easily recognized. The diagnosis is usually confirmed by a dermatologist with a visual examination. In some cases, histological examination of biological material is required.
Before the examination, you should not steam, pick, rub with a brush or a hard washcloth, or try to squeeze out the rash. Also, you cannot “dry” them under the sun’s rays and irradiate them with a UHF lamp.
In many cases, treatment for granuloma annulare is not required and the disease goes away on its own. To speed up the disappearance of the rash, external agents are often used - corticosteroids, over which waterproof bandages are applied.
Treatment of isolated foci of pathology is carried out using hydrocortisone ointment with ichthyol and phonophoresis. Therapy is also carried out that helps normalize the immune system and inhibits the process of antibody formation. Against the background of external treatment and measures that increase immunity, it is important to treat the disease against which the granuloma developed (diabetes mellitus, tuberculosis).
Other methods of treating granuloma annulare include:
- The use of ascorbic acid, tocopherol acetate, B vitamins, products containing iron;
- Injection of papules with triamcenolone acetonide;
- Use of dapsone, niacinamide, hydroxyloroquine and isotretinoin;
- Using chloroethyl to irrigate the affected areas, after which they become covered with “frost”;
- The use of carbonic acid or liquid nitrogen;
- PUVA therapy is a method that involves irradiating the skin with long-wave ultraviolet radiation and the use of psoralens.
Similar article - Photo of flat warts
To prevent a secondary infection, you can treat the affected areas with tincture of iodine 2-3 times a day. If the affected area is located on the legs, it is not recommended to walk barefoot on open ground.
Treatment with folk remedies for granuloma annulare is considered ineffective, since the disease is closely related to the immune system. Therefore, external therapy in the form of rubdowns, lotions or baths should not be carried out, but it is necessary to strengthen the immune system. For this it is recommended:
- Take echinacea in pill form or as a setup;
- Drink restorative herbal teas and natural juices;
- To live an active lifestyle.
Typically, granuloma annulare is cured within 1.5-2 years in 60-80% of cases, and relapses that occur usually go away faster than the primary rash. The prognosis of the disease improves following the principles of a healthy lifestyle.
Data on the effectiveness of various treatment methods
are based on small observational series that are not randomized controlled trials. This disease is asymptomatic, and treatment is solely for cosmetic purposes. Often the best solution is to allow the lesions to resolve on their own without any intervention. Although many therapies appear promising, they may only be effective if the disease resolves naturally.
Treatment of localized granuloma annulare
: • In a retrospective study of children with localized granuloma annulare (mean age 8.6 years), 39 of 42 patients had complete resolution of the lesions within two years. The average duration of the disease was one year. Researchers believe that most treatments are unnecessary because the disease resolves on its own. The main tactic is watchful waiting. • Corticosteroids can be injected into granuloma annulare lesions to resolve them. The injection is carried out directly into the ring of the lesion by subcutaneously injecting 3-5 mg/cm3 of triamcinolone acetonide (Kenalog) using a 27 G needle. For a lesion in the form of a complete ring (with a circle of 360°), four injections may be required. The main complications include hypopigmentation and skin atrophy at the injection site. • Nitric oxide cryotherapy was used in 9 patients and liquid nitrogen in 22 patients. After a single freezing, remission was achieved in 80% of cases; however, 4 of 19 patients treated with liquid nitrogen developed atrophic scars (>4 cm). All patients developed blisters. Atrophy due to cryotherapy can be prevented by avoiding freeze-thaw cycles lasting more than 10 seconds and ensuring that cryotherapy areas do not overlap.
Treatment of generalized/disseminated granuloma annulare
: • This variant is less responsive to treatment and often lasts longer than localized granuloma annulare. Conducted studies of the effectiveness of various treatment methods included a small number of patients and were not randomized. • Successful treatment of six patients with granuloma annulare was achieved with dapsone 100 mg once daily. Complete resolution of symptoms of the disease in all patients took from four weeks to three months. • UVA-1 phototherapy produced good or excellent results in half of 20 patients with disseminated granuloma annulare. In patients with a satisfactory response to treatment, the disease relapsed after treatment was stopped.
• In a study of four patients, topical imiquimod 5% cream was effective when applied once daily for an average of two months. After stopping treatment, three patients experienced no relapses for an average of 12 months; the fourth patient relapsed 11 days after stopping treatment, but after an additional six weeks of once-daily application of the cream, he experienced complete remission for 18 months. • Four patients used topical tacrolimus ointment 0.1% twice daily for 6 weeks; in all cases, improvement occurred within 10-21 days. After completion of treatment, two patients experienced complete clinical remission, and two other patients showed significant improvement. • Numerous studies with small numbers of patients have shown positive results with isotretinoin at doses of 0.5-1.0 mg/kg daily; however, due to potential side effects, this therapy should be reserved for very severe and resistant cases. • Three patients were treated with vitamin E 400 IU daily and zileuton 2400 mg daily. In all cases, complete clinical resolution of the lesions was achieved within three months after treatment.
Treatment of perforating and subcutaneous granuloma annulare
: • Although there are no data on specific treatments for these less common types of granuloma annulare, the same therapy recommended for cases of localized and disseminated granuloma annulare can be used based on the clinical presentation, severity of the patient's condition, and patient preference.
Recommendations for patients with granuloma annulare
.
The patient must be explained that his disease resolves on its own. Although unpleasant in appearance, it is best to allow the lesions to resolve naturally. Treatment may cause side effects that are as undesirable as granuloma annulare itself and may also be more persistent than granuloma annulare lesions. Patients seeking drug treatment
should be offered observation with periodic examination.
Clinical example of granuloma annulare
. A 39-year-old woman consulted a doctor about raised ring-shaped lesions on the dorsum of her right hand. Previously, without establishing an accurate diagnosis, the therapist prescribed her local steroids and antifungal agents, which turned out to be ineffective. Upon subsequent consultation with a dermatologist, based on the typical clinical picture, granuloma annulare was diagnosed and intralesional steroids were recommended. Over the following weeks, the patient noted an improvement, but after a month new rashes began to appear on the other arm.
Additional injections were given, and although the lesions had regressed a month later, the rash reappeared on the right arm. During the next visit, new lesions were also observed on the patient's foot. A diagnosis of disseminated granuloma annulare was made and systemic treatment was initiated.
— Return to the table of contents of the section “
Dermatology"
Symptoms of anular granuloma
The pathological process begins with the appearance of single lacquered, pale pink papules. The elements of the rash do not itch or cause pain.
After some time, the papules increase in size, forming a large round plaque. The plaque can gradually increase in size up to 5-10 cm in diameter.
The formation is unevenly colored: the middle may be pale pink (normal healthy color) or bluish, and the edges may be bright red. Neighboring plaques may have different stages of development. Ulceration of the rash elements occurs very rarely.
The duration of the disease is from six months to 2 years.
Favorite localization:
- dorsum of hands, elbows, knees and feet;
- buttocks;
- shoulders and forearms;
- chest and stomach;
- rarely - on the face.
Disseminated
granuloma develops in 15% of patients; such a disease is difficult to find in children. Round pink or purple rash elements form across the entire surface of the body.
Perforating
The course of the disease is typical for young people. The rash is localized on the fingers and hands. Papular granulomas have a small plug in the center through which yellowish contents drain. It dries out and forms a crust with a depression in the middle. As a result of healing, scars may remain at the site of the rash. Perforating annular granulomas are characterized by slight itching and pain at the site of the lesion.
Disseminated form Perforating form with crust in the center
Pathogenesis
The pathological process can last several months, or even several years. It presumably begins with a lymphocytic immune reaction, leading to the activation of macrophages and degradation of connective tissue, mediated by cytokines, which leads to the formation of a lenticular papule, which has a clearly defined, somewhat atrophic retraction in the central part, which grows with remitting progression, sometimes accelerating, sometimes slowing down in growth .
The granuloma annulare itself is a plaque measuring 5 square cm or more, slightly rising above the surface of the healthy skin and only matching the tone with it in the center. The skin easily gathers into folds, but around the sunken area there is a dense, waxy, shiny burgundy or slightly pinkish ring or crescent, which is not a very wide ridge (up to 2-3 mm). It may consist of individual grayish papules with pinkish rims that are not fused to the underlying layers of skin.
The rings are sharply defined, with their inner edges descending into sunken central areas. Thanks to palpation, a tumor-like neoplasm can be detected in the thickness of the epithelium, which gradually passes into the surrounding integument. In its structure, it has epithelioid cells and fibroblasts, which are surrounded on the periphery predominantly by lymphoid cells, as well as less common plasma cells and mast cells. The location of the round cell infiltrate is along the main course of the vessels, accompanied by the formation of powerful plexuses from argentophilic fibers. The separation of nodes occurs due to trabeculae and collagen fibers. The central parts are pronounced foci of necrosis and destruction of elastic fibers. The walls of the vessels gradually thicken, endothelial proliferation is observed, which can lead to blockage of individual vessels.
Annular granulomas can be located in the deep layers of the skin itself and even in the subcutaneous fat. They are felt as a peculiar type of nodules, reminiscent of dense peas or beans, which do not change the structure of the skin on the surface.
Varieties
Despite the common name, there are many types of granulomas. Let's look at the most common subtypes of the disease and their characteristics.
Pyogenic granuloma
This type occurs due to pyococcal infection. In appearance, the granuloma looks like a fairly large soft formation, up to 3 cm wide. The lesion can have either a smooth surface or a raised one.
Often such a granuloma is post-traumatic, that is, it occurs at the site of skin damage, after a presumably staphylococcal infection has been introduced there. The pyogenic form appears on the hands and fingers, feet, or face.
Granuloma annulare
It is a collection of small nodules in the shape of a ring, hence the name. No one knows for sure why such a lesion occurs on the skin. People with diabetes, tuberculosis, and rheumatism are prone to granuloma annulare.
Granuloma annulare is a benign formation, since it is not a tumor, but an inflammation in the skin. This type of granuloma cannot always be seen on the skin; inflammatory cells are located in the deep layer - the dermis. Granuloma annulare can manifest itself under external irritants - an abundance of sunlight, after insect bites. The typical form of granuloma annulare is most often located on the feet, hands, under the knees, and less often on the buttocks and neck.
Dermatologist Galina Vladimirovna Menshikova will tell you about granuloma annulare:
Tuberculous granuloma
This form is a consequence of infectious diseases, in particular tuberculosis, leprosy, and syphilis. A tuberculous granuloma is a focus of necrosis (dead tissue) surrounded by epithelial cells (connective tissue) and white blood cells. This is not just a cosmetic defect, it is a dangerous symptom. Such granulomas are located not only on the skin, but in the lungs, lymph nodes, respiratory tract, and tissues of the excretory system.
Granuloma venereum
This is a chronic process provoked by a sexually transmitted infection - syphilis, gonorrhea, chlamydia. This granuloma looks like a small red pimple and is located in the groin area and on the genitals.
The inflammation progresses slowly and can cause obvious discomfort.
Men are more prone to this type than women.
Eosinophilic granuloma
This type occurs as a result of an autoimmune reaction, that is, the body produces antibodies - eosinophils - for no reason, causing inflammation to appear on the skin, developing into granulomas.
The problem is that not only the skin is affected, but also the bones and internal organs.
Postoperative granuloma
Occurs as a reaction to suture material. It can also appear when an infection enters the wound. It appears at the site of the scar. After an immune response to an irritant in the form of suture material or infection, phagocyte cells accumulate, which is why a postoperative granuloma occurs.
Subcutaneous granuloma migrans
Appears as a result of chronic osteomyelitis or periodontitis - inflammatory processes in the periodontium (connective tissue at the root of the tooth) of the teeth or bone marrow and surrounding tissues.
Often such a granuloma appears in the lower jaw; the skin in this area has a blue tint. Inflammation changes location, which is why the granuloma is called migrating.
Classification and forms
Classification of granuloma annulare is carried out depending on the degree of spread of the disease and the characteristics of the process of formation of nodules.
The form of the disease plays an important role in determining the course of therapy. Some types of granuloma annulare are initially distinguished by their ability to quickly heal themselves. In this case, there is no need to take special measures.
Forms of granuloma annulare:
- Localized type (this form of the disease is characterized by the ability to heal itself, in most cases it manifests itself in childhood and does not cause discomfort to the small patient).
- Subcutaneous type (papules can connect with neighboring tissues, the pathology is typical for preschool children, foci of the inflammatory process differ in the depth of formation of papules);
- Perforating type (visually this form of the disease does not differ from the localized type, but a nuance of this pathology is the presence of a specific plug from which a yellowish liquid is regularly released).
- Perforating type (nodules appear mainly on the fingers and hands; in most cases, lightened areas of skin form at the site of the formations; this form of the disease is most often found in preschool children).
- Disseminated type (in childhood, this disease practically does not occur, lesions can be numerous and spread throughout the body, the connection of papules into a ring may not be observed).
Granuloma annulare is classified into typical and atypical forms. The first category includes the localized type, the second - the disseminated, perforating and subcutaneous type of the disease.
Perforating granuloma annulare is a separate type of disease. The nodules may secrete yellowish contents or not contain much fluid.
Diagnostic methods
In most cases, diagnosis of granuloma annulare in children is limited to visual examination . If there are suspicions of concomitant diseases, doctors prescribe additional types of examination.
In some cases, there is a need for differential diagnosis from lichen planus, pyogenic granuloma and rheumatoid nodules.
Methods for diagnosing granuloma annulare:
- skin test from the affected area;
- general analysis of urine and blood;
- histological examination;
- biochemical analysis of blood and urine.
Read about the causes and treatment of alopecia in children here.
Fighting disease using traditional medicine
For the best result, granuloma annulare must be treated comprehensively. Together with medications prescribed by a doctor, you can use infusions, solutions or ointments made at home.
An infusion is made from oak bark.
Take a handful of dry bark and steam it with half a liter of boiling water. It is better to brew in a thermos and leave overnight. This infusion is diluted as tea and drunk.
Rose hip.
To strengthen the immune system, take a glass of rosehip, a large spoon of elecampane (a perennial herb from the Asteraceae family), fill it with hot water, and bring it to a boil. This infusion should be drunk instead of tea, first diluted with boiling water.
Collection.
Another remedy to boost the immune system. Take half a glass of fresh carrot juice, radish juice, a large spoonful of liquid honey and lemon juice (squeeze half a lemon), mix all the ingredients, take it in the morning, afternoon and evening before meals.
The treatment will be effective if you use celandine tincture. You can buy it or prepare it yourself. The tincture should be diluted with glycerin (1:1) and lotions should be made.
White mistletoe tincture. Take 10 g of mistletoe for half a liter of alcohol and infuse it for a month; shake the infusion periodically. Then filter and take 30 drops before meals with plenty of water. The course lasts a month, then a pause, and after a month you can continue treatment
Mistletoe is a poisonous substance, so it is important not to exceed the dosage or reduce it to 25 drops
Elderberry tincture. It is prepared exactly like the mistletoe tincture, but it must be infused for up to 40 days. The dosage depends on the person’s weight, so for 80 kg, take 30 drops of infusion, which must be chewed on rye bread, greased with sunflower oil and garlic. The course of treatment is 30 days.
For treatment to be effective, it is necessary to normalize the functioning of the gastrointestinal tract and, as recommended, drink mint or lingonberry tea before meals.
In addition to tinctures and solutions, treatment can be done with homemade creams and ointments.
- Sea salt works well when used in conjunction with other remedies. The salt must be passed through a coffee grinder until it becomes powdery, add the yolk, and stir until it reaches a creamy consistency. Apply and leave for half an hour, rinse, moisten the affected areas with cream or Vaseline.
- Convert arnica root into powder, mix with pork fat, after melting it. Store the ointment in the refrigerator and apply in the morning, afternoon, and evening.
Remember that the disease is cured in 80% of 100% of cases within 2 years, but a relapse can occur, which goes away much faster, unlike the primary lesions. Treatment with folk remedies is only an addition to drug therapy to obtain a better effect, so you should not abuse them.
Granuloma annulare is a dermatous skin lesion, the origin of which is not fully understood. This is a chronic skin disease, manifested by the formation of ring-shaped areas of different sizes with nodules.
Ring-shaped, or anular, granuloma can appear at any age and in any person. However, it most often occurs in adult women and young children; men are almost not susceptible to this disease. Dermatosis develops very slowly and may not cause any discomfort to a person for years. And sometimes it even disappears without treatment. The disease is localized mainly on the skin of the extremities: elbows, hands, knees and feet.