Dermatoses are a group of skin diseases caused by various causes and with different clinical presentations. The disease can manifest at any age under the influence of both external and internal factors. Currently, more than 2,000 manifestations of dermatoses are known, this number includes such serious diseases as psoriasis, neurodermatitis, polymorphic dermatosis (Dühring's disease), and blistering dermatosis. A large group consists of various dermatitis. External factors that cause pathology include mechanical damage, reaction to increased or decreased temperature, chemical and thermal burns.
The appearance of the disease can also be triggered by pathogenic microorganisms, insect and animal bites (so-called dermatozoonoses). Internal factors are endocrine disorders, long-term infectious and inflammatory diseases, problems with the circulatory, digestive and nervous systems. Skin rashes are treated with general and local medications. Local medications (dermatosol, biopin) are used to relieve irritation, itching, and swelling. General therapy is aimed at eliminating the underlying disease, due to which the symptoms of dermatosis appeared.
Congenital skin pathologies are quite common. Hereditary diseases may be present at the time of birth, or may appear after some time, for example, allergic dermatosis. In addition, itchy dermatoses often occur due to intrauterine intoxication. Most of these diseases caused by intoxication are successfully eliminated in the first weeks of life.
Causes of the disease
Most skin pathologies arise due to disruption of internal organs. The skin displays the consequences of improper metabolism and a weakened immune system. Any of these disorders can cause allergic or bullous dermatoses (the appearance of multiple blisters). Neurological disorders and stress cause pathologies such as itchy rashes, which include urticaria and neurodermatitis. The initial manifestations of these pathologies are easily eliminated by diet and non-hormonal ointment dermatosol.
Various skin diseases are often observed in patients with a disturbed hematopoietic system (with lymphomas, leukemia). Chronic foci of infection, such as caries, sinusitis, cause itchy dermatosis, such as urticaria and exudative erythema. The pathology can accompany a person throughout his life, or it can be temporary, for example, dermatosis of pregnant women.
Diagnostics
The diagnosis of “pruritic dermatosis” is established by a dermatologist, based on the patient’s medical history, complaints and the nature of skin changes. To determine the cause of the disease, skin allergy tests are performed: a drop of various allergens is applied to the patient’s forearm, after which the doctor makes scratches with a needle according to the amount of solutions applied. An allergen entering the epithelium causes a reaction from the immune system. If the result is positive (the presence of sensitization to a certain substance), the scratch with it sharply turns red, swells and begins to itch. Additionally, a biochemical blood test, a general blood test are performed, and the level of Ig E is examined - the main marker of sensitization and allergic reactions.
Classification
- Itchy dermatoses. This group includes neurodermatitis, eczema, polymorphic dermatosis of pregnant women. The disease manifests itself on the skin as crusts, weeping, and lichenification.
- Blistering dermatoses (or bullous). This group includes infectious skin rashes (herpes, impetigo), autoimmune diseases (Dühring's dermatosis, acquired epidermolysis bullosa, blistering dermatitis). Pathologies are manifested by bubbles and vesicles.
- Illnesses caused by mental disorders. This includes dermatozoal delusion (a form of psychosis in which the patient is convinced that he is infected with parasites). Constant psychological stress often ends in the appearance of skin rashes, the etiology of which resembles dermatozoonoses.
- Allergic rashes. These include contact dermatitis and toxicoderma, dermatozoonoses. The skin can manifest itself as rashes of a very different nature: rash, redness, swelling, blisters.
How does the pathology manifest itself (symptoms)
At different age periods, skin pathologies have their own clinical characteristics. In childhood, the onset of the disease can be caused by hereditary diseases and congenital defects. Against the background of these disorders, allergic dermatosis often occurs. During adolescence, acne on the face and seborrheic dermatitis are observed. In infants, scabies dermatosis occurs on the arms, legs or face.
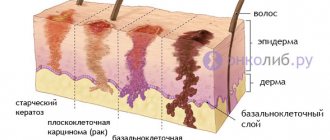
Old age is characterized by senile dermatitis (warts, skin atrophy), various viral dermatoses. The causative agents of pathologies are mostly staphylococci, streptococci and pyogenic bacteria. They penetrate the skin through mechanical damage (scratches, microtraumas, abrasions). Often, pathogenic microorganisms form secondarily infected dermatoses (against the background of an old disease, a new pathology caused by infection is formed).
At any age, viral, fungal, pustular and parasitic dermatoses can appear. The occurrence of these diseases is associated with weakened immunity and, as a result, low resistance to harmful microorganisms. The most common representatives of this group are dermatozoonoses, for example, scabies, caused by infection after an insect bite. To eliminate the consequences of insect bites, it is advisable to use non-hormonal external preparations, for example, dermatosol.
According to clinical manifestations, skin diseases can be divided into several groups. The first group includes pathologies without pronounced manifestations on the skin, but with general symptoms (fever, weakness). The second group includes diseases accompanied by subjective sensations on the skin. This may be itching, burning, numbness, for example, psoriasiform dermatosis. This also includes diseases with skin rashes that are not accompanied by any painful sensations, for example, pigmentary dermatosis.
Chronic inflammatory dermatoses of the palmoplantar localization
About the article
9410
0
Regular issues of "RMZh" No. 8 dated 04/09/2013 p. 393
Category: Dermatology
Authors: Belousova T.A. 1, Goryachkina M.V. 1 State Budgetary Educational Institution of Higher Professional Education “First Moscow State Medical University named after. THEM. Sechenov" Ministry of Health of the Russian Federation, Moscow
For quotation:
Belousova T.A., Goryachkina M.V. Chronic inflammatory dermatoses of the palmoplantar localization. RMJ. 2013;21(8):393.
In clinical dermatological practice, dermatoses of the palmoplantar localization (DPPL) are usually called chronic inflammatory diseases, the favorite localization of which is the palms and soles. Damage to these areas of the skin can be caused by many reasons, including: and fungal infection. Among non-infectious dermatoses, damage to the skin of the palms and soles is caused by eczema, psoriasis, and various forms of congenital and acquired keratoderma. Congenital keratoderma is a rare genodermatosis, manifests itself in early childhood and is combined with other malformations of the skin, internal organs, nervous system and musculoskeletal system. The debut of most DLPLs, as a rule, occurs between 30 and 40 years, i.e. at the most active working age. The majority of patients are women, who suffer from this pathology 3 times more often than men. DPPL is characterized by a long chronic course with periods of exacerbations, severe or moderate inflammatory changes, accompanied by itching, burning and soreness of the skin. The particular torpidity of the course of DPPL is largely determined by the constant irritation and traumatization of the skin of the palms and soles by external environmental influences (frequent washing, use of cosmetics and detergents, wearing shoes) [1, 4].
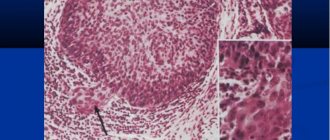
Damage to the most “working”, constantly functionally loaded areas of the skin significantly limits the physical capabilities of patients. Disfiguring cosmetic defects in visible areas of the skin bring patients deep mental suffering. Due to worries about the disease, patients, most of whom are women, develop severe emotional disorders, which causes disharmony in interpersonal and family relationships and underlies low self-esteem. Patients experience great difficulties in performing household and professional duties, choosing a profession, and finding employment. All this leads to a significant decrease in the quality of life. The social significance of DPPL is determined by the fact that in 30% of patients, a progressive increase in the severity of the process and the lack of effect from treatment cause temporary or long-term loss of ability to work, which negatively affects a professional career, leads to a decrease in social status and a deterioration in financial situation [2]. The structure of DLPL in adults is dominated by various forms of eczema (dyshidrotic, tylotic), which account for more than half of all cases. Eczema of the palms and soles is a chronic, relapsing disease with many causes and contributing factors. Allergens are the cause of dermatosis in a quarter of patients. An immediate type I inflammatory reaction according to the classification of P. Gill and R. Coombs can occur to latex in rubber gloves or when hands come into contact with food. However, a delayed type IV reaction is more often formed. Causative allergens often include nickel, chemical ingredients in cosmetics and medications, dyes and materials from which shoes are made. Among the accompanying irritant factors are detergents, alkalis, solvents, disinfectants, prolonged contact with water, friction, cold, and low humidity. The disease may be a reaction to a fungal or bacterial infection. Dyshidrotic eczema manifests itself acutely in the form of development against the background of slight hyperemia of blisters the size of a small pea, sometimes larger and multi-chambered, in the area of the palms, soles and lateral surfaces of the fingers (Fig. 1). After opening the blisters, weeping erosions form, gradually drying into serous crusts, and when a bacterial infection is attached, into purulent ones. After a relapse, the skin of the palms and soles remains dry, peeling and cracked. The cracks can be deep and very painful. The process is persistent, accompanied by severe itching and burning of the skin. During the transition to the chronic stage, infiltration and lichenification increase, hyperemia becomes stagnant, cracks become permanent. Against this background, with exacerbations of the process, blisters appear again, hyperemia, swelling of the skin and itching intensify. A rare type of chronic eczema is horny eczema (eczema tyloticum) (Fig. 2). In this form, there are no symptoms of acute inflammation of the skin in the form of swelling, blistering rashes and itching. On the skin of the palms there are limited areas of hyperkeratosis in the central or marginal zones of the palms and more or less deep cracks. Patients' complaints boil down to roughness and stiffness of the skin of the palms and pain in the area of cracks. A special type of chronic eczema is eczema of the fingertips. The skin of the fingertips is pink-red, dry, flaky, cracked. Vesicles are not typical. Itching is minimal and often completely absent. Soreness and a burning sensation of the skin in the affected area are typical. The process is limited to the distal phalanx of one or more fingers. Atopy may be a predisposing factor; irritants (detergents, contact with water, friction), allergens (glue, medications, foods, plants) may play a role. It is often observed in people of certain professions: dentists, flower growers, office workers, hairdressers. The process tends to be protracted over a long period of time. In a number of patients, the process, starting at the fingertips, slowly spreads to all fingers and the palm and develops into exfoliative keratolysis. This chronic dermatosis is characterized by widespread symmetrical peeling of the skin of the palms. At the beginning, the peeling zones are small in size, up to 2–3 mm in diameter, and have a rounded outline. Gradually they increase in size due to peripheral growth, merge, forming large rounded areas. The central zone becomes hyperemic and painful [3]. The second position (approximately 20%) in this group is occupied by patients with menopausal palmoplantar keratoderma (Haxthousen syndrome). Dermatosis is an acquired form of diffuse keratoderma. The disease mainly affects women in the 5th decade of life. In men, the disease occurs less frequently and at a later age – between 50–60 years. The development of the disease is facilitated by estrogen deficiency and a decrease in the functional activity of the thyroid gland. Patients often have somatic diseases comorbid with dermatosis: obesity, hypertension, cardiovascular diseases, deforming arthritis. The skin of the palms and/or soles, starting from the central zone, is gradually covered with horny layers, the number of which slowly increases both in volume and area. The horny masses crack, pain appears in the area of the lesions, especially when walking, and mild itching. Hyperkeratotic layers can be diffuse or focal with increased horny layers along the edges of the palms and soles. Hyperkeratosis is especially pronounced in areas of pressure and friction. Some patients may have areas of keratosis, incl. with psoriasiform peeling and on other areas of the skin, primarily on the extensor surfaces of the extremities (elbows, knees) [5]. In 10% of patients, skin lesions on the palms and soles are caused by psoriasis (Fig. 3). Most often, this dermatosis occurs between the ages of 30 and 50 years, but can also appear at a later period. A predisposing factor is constant trauma to the skin of the palms during physical labor. The process is represented by infiltrated plaques with clear boundaries of scalloped burgundy-red outlines that protrude above the surface of the surrounding skin. Over time, the plaques, due to peripheral growth, merge into a continuous lesion that occupies the entire surface of the palms or soles. The plaques are covered over the entire surface with thick, firmly seated silvery-white scales, less often with yellowish-gray crusts, after exfoliation of which the bright red surface of the plaque is exposed. Often, with constant trauma, the surface of the rash cracks with the formation of painful, deep bleeding cracks [6]. Despite the fact that the dermatoses included in the group under consideration have their own individual etiopathogenetic mechanisms of development, their clinical symptoms are very similar. This is largely due to the peculiar structure of the skin of the palms and soles. It is known that the skin, depending on the thickness of the epidermis, is divided into two types: thick and thin. The skin of the palms and soles is classified as thick skin (the thickness of the epidermis is 5–8 mm), while in areas of thin skin its thickness does not exceed 1–2 mm. In thick skin, all 5 layers of the epidermis are present, with the spinous layer being 3 times thicker than in thin skin. Thick skin is distinguished by an extremely developed stratum corneum, consisting of 15–20 layers of keratinized cells (in thin skin there are 3–4 rows). At the same time, the thickness of the dermis is small, with well-defined papillae, which increases the area of the basal layer and the ability for a large number of keratinocytes to enter into differentiation. In this regard, DLPL are characterized not only by inflammatory infiltration of the dermis, but also by significant pathological changes in the epidermis. Disorders of keratinization processes are characterized by pronounced pathological changes in the proliferation and differentiation of keratinocytes (acanthosis, hyperkeratosis, parakeratosis). Clinically, this is manifested by intense peeling, focal or diffuse hyperkeratosis, dryness, superficial or deep cracks [7]. External therapy for DLPL is the leading component of the therapeutic complex. The morphological characteristics of the skin of the palms and soles largely determine the therapeutic effect of a particular externally applied drug. It is known that the absorption of external medications depends on the structure (thickness) of the skin. Comparative studies have revealed significant differences in the absorption of the same drug applied to different areas of the skin. This indicator in the forearm area was equal to 1.0; on the back -1.7; on the scalp – 3.5; on the skin of the face –13; on eyelids – 42; and on the palms - only 0.83, on the feet - only 0.14. Thus, even pathologically intact thick skin is capable of absorbing externally applied drugs only in small quantities. With inflammatory changes, impaired desquamation, and thickening of the stratum corneum, the absorption of drugs decreases to an even greater extent. Therefore, the area of the palms and soles is one of the “difficult” localizations for external treatment. According to the frequency of use of various external agents used in the treatment of DPPL, they can be ranked as follows: topical steroids, keratolytics, emollients and moisturizers (emollients), tar preparations and other reducing agents, topical retinoids, calcipotriol (a synthetic analogue of vitamin D3), hydroxyanthrones (ditranol, cignolin). The last three groups are mainly used in the treatment of psoriasis. As clinical practice shows, topical steroids in combination with keratolytics and emollients have an effective therapeutic effect in 75% of patients with DPPL. However, when choosing a specific external steroid, it is necessary to take into account a number of factors that influence their therapeutic effect, primarily the absorption of the steroid, which in less permeable thick skin will be significantly lower than in thin skin. Therefore, to obtain an effect in the first case, a longer duration of treatment and the use of a stronger steroid are necessary than in the second. The penetration of the steroid through the phospholipid layers of the epidermis into the dermis increases with the esterification of the steroid molecule and the lipophilicity of the drug base. An important pharmacodynamic characteristic of a topical steroid is the concentration gradient - the amount of drug transferred into the skin per unit time. Occlusion increases the absorption of the drug many times over. Ointment forms of topical steroids have the greatest penetrating ability. And, finally, the speed of onset of the effect and its duration depend on the rate of binding of the hormone to the cytosolic receptors of keratinocytes and the duration of the association of the steroid with a specific GCS receptor. Thus, the choice of a specific topical steroid for DPPL should be determined by several criteria. The steroid must have significant therapeutic potency (belong to the class of strong steroids) and be applied in the form of an ointment using occlusive dressings. This ensures rapid penetration of the drug through the thick and pathologically altered stratum corneum and the creation of the necessary therapeutic concentration in the focus of chronic inflammation. It is necessary to adhere to the daily frequency of use of a specific steroid, which contributes to the active accumulation and maintenance of the therapeutic concentration of the drug in the pathologically altered skin during the course of therapy. The correct tactics of using a steroid ensures active suppression of inflammation and itching, rapid achievement of a clinical effect with minimal risk of side effects [8]. In the treatment of squamous-hyperkeratotic conditions, keratolytics are actively used, and primarily ointments containing salicylic acid in a concentration of 2–10%. Salicylic acid, by dissolving the intercellular binding substance of epidermocytes, promotes exfoliation of dead horn cells, active rejection of scales and removal of crusts. Possessing hygroscopicity, it attracts water from the subepidermal layers, providing a moisturizing and macerating effect on the epidermis, which also significantly increases its permeability to other medicinal effects. Being a strong b-hydroxy acid, it helps restore the natural acid reaction of the skin, preventing the development of bacterial and mycotic flora, thereby reducing the risk of developing unwanted infectious complications. The use of a combination of topical steroids with 2–10% salicylic acid in the form of an ointment significantly increases the possibility of active penetration of the steroid into the skin [9]. The basic means of external therapy for chronic squamous-hyperkeratotic diseases of the palms and soles, accompanied by severe dryness, peeling, and cracking of the skin, are emollients (from the French molle - soft). In modern dermatological practice, emollients are recognized as highly effective agents, indispensable in the management of patients with dry skin prone to hyperkeratosis and desquamation. These drugs have the ability to moisturize, soften, saturate the skin with fatty components, and restore its aesthetic appearance. They reduce transepidermal water loss and replenish layers of intercorneocytic lipids. The action of emollients is partly due to the effect of filling gaps between exfoliating keratinocytes, but their most important therapeutic effect is to increase the water content in the stratum corneum. Restoring hydration has a beneficial effect not only on the mechanical properties of the stratum corneum, improving the extensibility and flexibility of the skin, but also actively contributes to the normalization of skin desquamation processes. An increase in the concentration of free water molecules in the skin increases the activity of proteolytic enzymes and accelerates the process of destruction of corneodesmosomes, which leads to a more complete and uniform separation of horny scales from the surface of the skin. The use of emollients as part of complex dermatological treatment helps to increase the activity of therapy, reduce the duration of treatment, lengthen periods of remission, improve the prognosis of the disease in general, and therefore improve the patient’s quality of life [10–12]. Thus, the modern arsenal of external therapeutic agents makes it possible to create a program for effective external treatment of a patient with DPPL, taking into account the characteristics of the clinical picture of the disease, the individual and age-related characteristics of the patient’s skin.
Literature 1. Raznatovsky K.I. The role of socio-psychological and emotional stress factors in the development of hemodynamic, microcirculatory and hormonal disorders in dermatoses of the palmoplantar localization: abstract of thesis. dis. doc. honey. Sci. – St. Petersburg, 1997. 22 p. 2. Belousova T.A. Experience of using Elokom S in the treatment of inflammatory dermatoses of the palmoplantar localization // Breast cancer. 2006. No. 5. pp. 357–360. 3. Thomas P. Habiff. Skin diseases. Diagnosis and treatment. – M.: MEDpress-inform, 2006. P. 32–41. 4. Akimov. V.G. Palmoplantar keratoderma of hereditary and acquired nature // Consilium Medicum (add. “Dermatology”). 2011. No. 3. P. 6–10. 5. Albanova V.I. Dermatoses of menopause. //Rus. magazine leather and veins bol. 2002. No. 2. P. 38–42. 6. Wolfe K., Johnson R., Surmond D. Fitzpatrick Dermatology; lane from English; 2nd ed. 2007. pp. 98–117. 7. Myadelets O.D., Adaskevich V.P. Functional morphology and general pathology of the skin. – Vitebsk: Publishing House of the Vitebsk Medical Institute, 1997. 269 p. 8. Fitzpatrick D.E., Eling D.L. Secrets of dermatology. – M.: Binom, 1999. P. 55–63. 9. Kruglova L.S. Modern possibilities of external therapy for psoriasis. 10. Loden M. The clinical benefit of moisturizers // JEADV. 2005. Vol. 19. P. 672–688. 11. Marks R. Actions and effects of emollients // Sophisticated Emollients. – Stuttgart, New York: Georg Thieme Verlag, 2002. P. 12–23. 12. Trapp M. Is there room for improvement in the emollients for adjuvant therapy? // JEADV. 2007. Vol. 21(2). P. 14–18.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Occupational diseases
Occupational dermatoses are skin pathologies associated with production characteristics. Occupational diseases must be distinguished from physical skin defects acquired at work (scars, calluses). They should also not be confused with skin diseases that worsen during work at work under the influence of harmful substances, for example, neurodermatitis. Occupational dermatoses are classified according to etiological principles.
Classification of occupational skin diseases:
- Pathologies caused by chemical factors (acids, alkalis, lubricating oils, drugs, etc.). This group includes allergic dermatoses, toxicermia, contact dermatitis, and various bullous dermatoses.
- Diseases of infectious etiology. For example, mycoses, infectious blistering dermatoses.
- Diseases arising under the influence of physical factors: thermal burns, current, radiation.
- Occupational dermatoses that arise from constant contact with dust, asbestos, and fiberglass. For example, asbestos warts, allergic dermatosis.
Skin diseases of pregnant women
Pregnancy dermatoses include skin diseases associated with pregnancy. Itching is observed in 2% of women in the 3rd trimester of pregnancy. This is due to the increased secretion of bile acids under the influence of progesterone and estrogen. Prurigo may appear at an earlier stage. The clinical picture of this pathology is characterized by rashes with a hemorrhagic crust, and sometimes blistering dermatosis is observed.
Shortly before birth, polymorphic dermatosis of pregnancy may develop. The occurrence of pathology is associated with a sharp increase in the weight of the expectant mother and fetus, and skin stretching. The following clinical picture is observed: large blisters appear on the skin of the thighs and abdomen, accompanied by severe itching. Pregnancy dermatosis usually disappears a few weeks after birth. To treat skin rashes in pregnant women, local medications are used to relieve symptoms: dermatosol, creams with calamine.
Treatment
Therapy for skin diseases should be general and local. General treatment usually includes symptomatic, pathogenetic and etiological therapy. First of all, the cause of the pathology is eliminated. For example, parasitic dermatoses require the removal of pathogens from the body, paraneoplastic dermatoses (caused by tumors of internal organs) require the elimination of neoplasms.
External agents (ointments, aerosols, lotions) mainly have a symptomatic effect: destructive, anti-inflammatory, antipruritic. Viral dermatoses are treated with antimicrobial drugs, blistering dermatosis with soothing and anti-inflammatory ointments (dermatosol).
Methods such as diet therapy, physiotherapy, and sanatorium treatment have proven themselves well. The development of skin diseases is always accompanied by inflammatory processes. Glucocorticosteroids are often used to relieve them. These drugs cause accelerated skin regeneration, removal of inflammation, restoration and cleansing of the skin. Hormonal drugs are prescribed for diagnoses such as polymorphic dermatosis and many other skin pathologies, including cystic dermatosis. The medications are prescribed by the doctor, taking into account the specifics and stage of the disease, the gender and age of the patient, and the presence of other pathologies.
The appearance of some skin pathologies is caused not by physical, but by psychosomatic reasons. The most well-known disease of this group is dermatozoal delirium. With this disease, the patient first needs the help of a psychiatrist or psychologist. To relieve skin rashes in this case, it is recommended to use external agents without hormones and fluoride, for example, dermatosol.
Types of dermatitis
The concept of dermatitis includes a large number of skin diseases with different etiologies. Therefore, when dermatitis is detected, treatment is determined primarily by the main irritating factor, and its technique varies significantly in different cases of the disease.
Due to the difficulty of diagnosing the type of dermatitis, treatment should be prescribed after a thorough examination by a dermatologist. The treatment method can be based on different methods: medication, physiotherapy, invasive methods, folk remedies, etc. Quite effective treatment can be carried out at home, but only after consultation with a doctor.
Based on the manifestation of signs of the disease and the nature of the pathogenesis, some dermatitis can be noted. They have specific properties and are widespread.
It should be noted that itchy dermatitis has several forms. So, it has three types: acute, subacute and chronic itchy. So, the first type is characterized by the formation of tiny blisters only in some skin areas. If these blisters are opened, pinpoint abrasions with fluid may appear. In addition, it will not be possible to avoid weeping acute eczema.
During subacute dermatosis, unpleasant peeling appears on the affected areas. As a rule, this stage occurs when a person received insufficient treatment or did not seek it at all. In this case, some bubbles, even if they are not opened, will dry out and form a crust.
Dermatosis in children
Allergic dermatoses occur very often in childhood. This is due to feeding the baby with artificial formulas, the state of the environment, the use of clothing made from synthetic materials and many other factors. If treatment measures are not taken in time, dermatosis can become severe or chronic.
Treatment of a child first begins with an examination by a doctor, as well as passing the necessary tests. After this, the specialist determines the cause of the disease and prescribes appropriate treatment.
It is also necessary to follow a proper diet and exclude the consumption of chocolate, citrus fruits, nuts, honey, cocoa and other hypoallergenic products.
Phytotherapy
Drug therapy for skin diseases can be supplemented with treatment with folk remedies. Bullous dermatoses and other skin rashes can be treated with herbal remedies that have anti-inflammatory, antiallergic and reparative effects. Such collections usually include knotweed, tricolor violet, oats, juniper, string, and agrimony. Dermatozoonoses can be eliminated with the juice of fresh parsley, a strong decoction of mint, and compresses of grated raw potatoes.
Many skin pathologies, for example, paraneoplastic dermatoses caused by neoplasms, are accompanied by weakened immunity. In these cases, Eleutherococcus, Aralia, and Leuzea are prescribed. To relieve intoxication, it is recommended to use products such as milk thistle-based silybor and convaflavin from lily of the valley. To relieve external symptoms - propolis ointment, dermatosol.
Blistering dermatosis with local rashes, irrigated with a decoction of belladonna and celandine. Parasitic dermatoses are treated with lotions made from essential oils (lavender, sandalwood, rosemary and cloves in equal parts). Mustard oil mixed with garlic helps a lot. Mix 0.5 liters of mustard oil with 100 g of grated garlic, cook for about 20 minutes. Strain the resulting mixture and use it as compresses on the affected area.
Diagnostics
If you suspect the development of itchy dermatosis, the patient should visit a dermatologist. The doctor will clarify the nature of the reaction and the frequency of occurrence of negative symptoms.
Prohibited names:
- full fat milk;
- cocoa beans in any form;
- seafood;
- fish caviar;
- peanuts, almonds, hazelnuts, walnuts;
- citrus;
- eggs, especially whites;
- fruits and vegetables, the pulp and peel of which have a bright color: red, orange;
- coffee;
- exotic fruits;
- spices, sauces;
- canned food;
- semi-finished products, sausages, boiled and smoked sausage;
- pickled vegetables, pickles;
- cheeses;
- ready-made mayonnaise;
- products with synthetic fillers: emulsifiers, flavors, dyes.
Drug therapy
Therapy for diseases accompanied by skin reactions includes a complex of drugs:
- for oral administration. Allergy pills suppress the release of histamine, reduce the severity of allergic inflammation, and prevent relapses in the chronic form of the disease. In case of a lightning-fast reaction, classic formulations (1st generation) are used: they reduce swelling of the epidermis and prevent secondary infection in severe forms of allergic dermatoses. Skin-Cap, Bepanten, Psilo-balm, Desitin, La-Cri, Vundehil, Solcoseryl, Fenistil-gel, Gistan, Protopic, Epidel;
- hormonal ointments and. Glucocorticosteroids reduce the local activity of the immune system, prevent the production of inflammatory mediators, and stop allergic inflammation. Potent drugs are prescribed only for severe reactions for a short period of time (up to 10 days). The following medications are suitable for adults: Prednisolone, Hydrocortisone, Advantan, Elokom, Lokoid, Flucort, Sinaflan, Gistan N;
- tablets and solutions for injections that reduce sensitization of the body. The compositions reduce capillary permeability, prevent swelling, strengthen the immune system, and ensure the supply of beneficial microelements. , sodium bromide, calcium gluconate, ascorbic acid;
- . Oral intake of tablets, hydrogel, suspension with active adsorbing properties cleanses the body and prevents further penetration of antigens into tissues. Removing irritant molecules reduces the strength of skin reactions and speeds up recovery. The best option is to use sorbents with high absorbency. Modern means: Multisorb, Laktofiltrum, White coal, Smecta, Carbosorb, Enterumin;
- soothing compounds. Itching is one of the unpleasant signs of allergic dermatoses. In the chronic course of the disease, the patient becomes irritable and suffers from insomnia. To normalize the state of the nervous system, non-addictive drugs are prescribed: Novopassit, Karvelis, valerian tablets, motherwort tincture, decoction of mint, lemon balm, a soothing herbal mixture.
Folk remedies and recipes
To reduce the severity of negative symptoms in allergic dermatoses, remedies based on medicinal plants are suitable:
- Decoctions for oral administration. The compositions cleanse the body and exhibit a weak anti-inflammatory effect. Ingredients: viburnum branches, elecampane and burdock roots, mint, nettle, .
- Therapeutic baths. Herbs: string, sage, chamomile, mint, yarrow, calendula. Oak bark is useful;
- Lotions with decoctions of medicinal plants listed in paragraph 2.
- . Dissolve a small amount of mountain resin in water and take daily for 10 days. For a year - 4 courses.
- . Grind the washed, dried, film-free natural product from raw eggs to a powder and mix with lemon juice. Take if you have a negative reaction to food.