Caesarean section technique
The general principle of performing a transsection may seem quite simple, and the operation itself has been practiced for decades. However, it is still classified as an intervention of increased complexity. A horizontal incision in the lower uterine segment is considered the most appropriate, both from the point of view of risk and from the point of view of aesthetic effect.
Depending on the characteristics of the incision, lower median laparotomy, Pfannenstiel and Joel-Cohen sections are used for caesarean section. The choice of a specific type of operation occurs individually, taking into account changes in the myometrium and abdominal wall, the urgency of the operation, and the skills of the surgeon. During the intervention, self-absorbable suture material is used - vicryl, dexon, etc.
It is worth noting that the direction of the incision of the abdominal tissue does not always and does not necessarily coincide with the dissection of the uterine wall. Thus, with lower median laparotomy, the uterus can be opened as desired, and the Pfannenstiel incision involves isthmicocorporeal or corporal transection. The simplest method is considered to be a lower median laparotomy, which is preferable for a corporal section; a transverse incision in the lower segment is more conveniently made through the Pfannenstiel or Joel-Cohen approach.
Corporal caesarean section (CCS)
Corporal caesarean section is rarely performed when there are:
- Severe adhesive disease, in which the path to the lower segment is impossible;
- Varicose veins in the lower segment;
- The need for hysterectomy after removing the child;
- Insolvent scar after a previously performed corporal transection;
- Prematurity;
- Conjoined twins;
- A living fetus in a dying woman;
- Transverse position of the child, which cannot be changed.
The approach for CCS is usually a lower median laparotomy, in which the skin and underlying tissue are dissected to the aponeurosis at the level from the umbilical ring to the pubic joint strictly in the middle. The aponeurosis is opened longitudinally over a short distance with a scalpel, and then enlarged with scissors up and down.
suturing the uterus during corporal CS
The second caesarean section must be carried out very carefully due to the risk of damage to the intestines and bladder . In addition, the existing scar may not be dense enough to maintain the integrity of the organ, which is dangerous for uterine rupture. The second and subsequent transsections are often carried out on the finished scar with its subsequent removal, and the remaining aspects of the operation are standard.
With CCS, the uterus is opened exactly in the middle; for this, it is rotated so that a cut of at least 12 cm in length is located at an equal distance from the round ligaments. This stage of the intervention should be carried out as quickly as possible due to extensive blood loss. The amniotic sac is opened with a scalpel or fingers, the fetus is removed by hand, the umbilical cord is pinched and intersected.
To speed up uterine contraction and evacuation of the placenta, oxytocin is administered into a vein or muscle, and broad-spectrum antibiotics are used intravenously to prevent infectious complications.
To form a durable scar, prevent infections, and ensure safety during subsequent pregnancies and childbirth, it is extremely important to adequately align the edges of the incision. The first suture is placed 1 cm away from the corners of the incision, and the uterus is sutured in layers.
After removing the fetus and suturing the uterus, it is mandatory to examine the appendages, appendix and nearby abdominal organs. When the abdominal cavity is washed, the uterus has shrunk and become dense, the surgeon sutured the incisions layer by layer.
Isthmicocorporeal caesarean section
Isthmiccorporeal transection is carried out according to the same principles as CCS, with the only difference that before opening the uterus, the surgeon cuts transversely the fold of the peritoneum between the bladder and the uterus, and the bladder itself moves downwards. The uterus is dissected 12 cm in length, the incision goes longitudinally in the middle of the organ above the bladder.
Incision in the lower uterine segment
During a caesarean section in the lower segment, the abdominal wall is cut along the suprapubic line - according to Pfannenstiel. This approach has some advantages: it is cosmetic, it is less likely to cause subsequent hernias and other complications, the rehabilitation period is shorter and easier than after a median laparotomy.
incision technique in the lower uterine segment
The incision of the skin and soft tissues goes in an arcuate manner across the pubic symphysis. The aponeurosis is opened slightly above the skin incision, after which it is peeled off from the muscle bundles down to the pubic symphysis and up to the navel. The rectus abdominis muscles are pulled apart with the fingers.
The serous cover is opened with a scalpel at a distance of up to 2 cm, and then enlarged with scissors. The uterus is exposed, the folds of peritoneum between it and the bladder are cut horizontally, the bladder is retracted to the womb with a mirror. It should be remembered that during childbirth the bladder is located above the pubis, so there is a risk of injury to it if you use a scalpel carelessly.
The lower uterine segment is opened horizontally, carefully so as not to damage the baby's head with a sharp instrument, the incision is increased with the fingers to the right and left to 10-12 cm, so that it is enough to pass the newborn's head.
If the baby's head is low or large, the wound can be enlarged, but the risk of damage to the uterine arteries with severe bleeding is extremely high, so it is more advisable to make the incision in an arcuate manner slightly upward.
The amniotic sac is opened together with the uterus or with a scalpel separately, spreading the edges apart. With his left hand, the surgeon penetrates the fetal sac, carefully tilts the baby’s head and turns it towards the wound with the occipital region.
To facilitate the extraction of the fetus, the assistant gently presses on the fundus of the uterus, and the surgeon at this time carefully pulls the head, helping the baby’s shoulders to come out, and then pulls him out by the armpits. In a breech presentation, the baby is removed by the groin or leg. The umbilical cord is cut, the newborn is handed over to the midwife, and the placenta is removed by traction on the umbilical cord.
At the final stage, the surgeon makes sure that there are no fragments of membranes or placenta left in the uterus, and that there are no myomatous nodes or other pathological processes. After the umbilical cord is cut, the woman is given antibiotics to prevent infectious complications, as well as oxytocin, which accelerates the contraction of the myometrium. The tissues are sutured tightly in layers, matching their edges as accurately as possible.
In recent years, the method of transection in the lower segment without detachment of the bladder through the Joel-Cohen incision has gained popularity. It has many advantages:
- The baby is removed quickly;
- The duration of the intervention is significantly reduced;
- Blood loss is less than with bladder detachment and CCS;
- Less pain;
- Lower risk of complications after the intervention.
With this type of cesarean section, the incision is made transversely 2 cm below the line conventionally drawn between the anterior superior iliac spines. The aponeurotic leaf is dissected with a scalpel, its edges are retracted with scissors, the rectus muscles are moved back, and the peritoneum is opened with the fingers. This sequence of actions minimizes the risk of bladder injury. The wall of the uterus is cut over 12 cm simultaneously with the vesicouterine fold. Further actions are the same as with all other methods of transection.
When the operation is completed, the obstetrician examines the vagina, removes blood clots from it and the lower part of the uterus, and rinses it with sterile saline, which facilitates the recovery period.
Methods of surgical delivery
There are several techniques for caesarean section.
Classic caesarean section
Caesarean section in the lower uterine segment is the most common and safest.
This operation promotes the formation of a durable scar.
How to do a caesarean section:
- A skin incision is made (usually a suprapubic incision is made).
- Layer-by-layer opening of the subcutaneous tissue and aponeurosis.
- The muscles are not cut, but bluntly pushed back.
- Opening of the parietal layer of the peritoneum.
- An incision is made on the uterus in the lower segment (the area located in the area of the isthmus of the uterus).
- Extraction of the fetus.
- Removing the placenta.
- Curettage of the uterus using a curette to remove remaining placental tissue.
- Checking the patency of the cervical canal (to ensure the outflow of bloody discharge in the postoperative period).
- Changing gloves (since the cervical canal is non-sterile).
- Suturing the incision on the uterus (suture material usually used is vicryl).
- Peritonization of the suture on the uterus by the vesicouterine fold of the peritoneum.
- Inspection of abdominal organs, removal of blood clots.
- Layer-by-layer suturing of all dissected tissues.
Corporal caesarean section
Less commonly used is a corporal cesarean section—an incision into the uterine body in the midline.
The reason is the formation in some cases of an incompetent scar, and an increased risk of uterine rupture during subsequent pregnancy.
This method is often used to extract the fetus as carefully as possible, for example, in cases of extreme prematurity.
Corporal caesarean section technique:
- The tissues of the anterior abdominal wall are dissected layer by layer.
- An incision on the uterus is made along the body of the uterus.
- Suturing the uterus.
- Reconstruction of the abdominal wall.
Stark modification
The Stark surgical technique deserves special attention. In this technique, the use of sharp and cutting objects is minimized (the tissues are incised with a scalpel and separated with fingers).
When suturing, only the integrity of the aponeurosis and skin is restored. No sutures are applied to the remaining layers of the abdominal wall. This technique can significantly reduce the time of surgical intervention.
Absolute indications for elective caesarean section
Absolute indications for a cesarean section include reasons when natural childbirth is impossible or poses a very high risk to the health of the mother or fetus.
Narrow pelvis
Sometimes the anatomical structure of a woman does not allow the child to pass through the pelvic ring: the size of the mother’s pelvis is smaller than the presenting part (usually the head) of the child. There are criteria for the size of a normal and narrow pelvis based on the degree of narrowing.
With an anatomically very narrow pelvis:
- Grade III-IV surgery will be performed as planned;
- II degree of narrowing, the decision will be made during childbirth;
- I degree birth will take place naturally in the absence of other indications.
Mechanical obstacles preventing natural childbirth
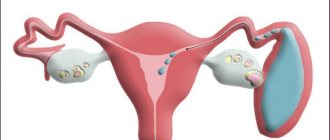
This may be uterine fibroids in the isthmus region (i.e., the area where the uterus meets the cervix), ovarian tumors, tumors and deformities of the pelvic bones.
Threat of uterine rupture
It most often occurs when there is a scar on the uterus, for example due to a previous cesarean section, as well as due to numerous previous births, when the walls of the uterus are very thin. The health of the scar is determined by ultrasound and its condition before and during childbirth.
Placenta previa
Sometimes the placenta is attached in the lower third and even directly above the cervix, blocking the exit of the fetus. This is fraught with severe bleeding, which is dangerous for the mother and baby and can lead to placental abruption. Diagnosed by ultrasound, surgery is scheduled for 33 weeks of pregnancy or earlier if bleeding is detected, indicating placental abruption.
In these cases, it is necessary to carry out surgical delivery using a cesarean section, regardless of all other conditions and possible contraindications.
encyclopedia of life answers
alex2
C-section
(Latin caesarea “royal” and sectio “incision”) - carrying out childbirth using abdominal surgery, in which the newborn is removed through an incision in the abdominal wall of the uterus. Previously, a caesarean section was performed only according to medical certificates, but nowadays the operation is increasingly performed at the request of the woman in labor.
A little bit from the history of caesarean section
The first reliable caesarean section on a living woman was performed in 1610 by Dr. Trautmann ( I. Trautmann
) from Wittenberg. The child was extracted alive, and the mother died 4 weeks later (the cause of death was not related to the operation). In Russia, the first caesarean section was performed in 1756 by I. Erasmus. One of the first surgeons in Russia to practice caesarean section was E. H. Ikavitz.
In 2000, Mexican woman Ines Ramirez Perez performed a caesarean section on herself.
Before, during and after surgery
Before the operation, the pubis is shaved in advance and a catheter is inserted into the bladder to avoid problems with the kidneys later. After anesthesia, the woman is placed on the operating table and the upper part of the body is fenced off with a screen.
During the operation, the doctor makes two incisions: the first incision is in the abdominal wall (skin, fat and connective tissue), the second is in the uterus. (The abdominal muscles are not cut; they are pulled apart to allow them to heal more easily). Both cuts can be vertical or horizontal (transverse), or one can be vertical and the other horizontal. For example, the skin incision can be horizontal, and the uterus can be vertical. It is important for the next birth to know what incision of the uterus was previously, so you need to ask the doctor and write it down for yourself.
There are two classes of skin incisions for caesarean section. A transverse incision (or bikini incision) is used more often; it is made horizontally just above the pubic bone. The midline incision is made vertically between the navel and pubic bone. This incision allows you to quickly remove the fetus in emergency circumstances and may be preferable in some other cases (for example, if the mother is obese).
There are three classes of uterine incisions.
A traditional incision is made vertically at the highest part of the uterus. Currently, it is done occasionally, except in cases of danger to the life of the fetus, placenta previa and transverse position of the fetus. After a traditional incision, vaginal delivery is usually not recommended.
More often at the moment, a lower transverse incision of the uterus is practiced. It is associated with the least blood loss and the least risk of postpartum infection, but requires more time than a traditional incision. The next birth can occur through the natural birth canal, as this incision heals well and leaves a strong scar.
A vertical incision in the lower sector of the uterus is made only when the lower part of the uterus is undeveloped or too thin for a transverse incision (as in the case of some early labor).
To control bleeding from the incisions, the doctor ties or cauterizes the ends of the cut blood vessels. Then the doctor sucks out the amniotic fluid from the uterus, removes the baby, quickly points it to the woman in labor and hands it over to the nurse. Later, the doctor manually separates and removes the placenta. At this moment there is an opportunity to feel some pressure. The nurse cleans the baby's mouth and nose to remove fluid and mucus, as in the case of vaginal birth. The baby is dried, assessed on the Apgar scale, examined and given the necessary medical care.
After the baby and placenta are removed, the doctor checks the uterus and begins restoration. The incisions in the uterus and abdominal wall are sutured with dissolvable surgical suture. The skin is connected with soluble or insoluble thread, clamps or staples, which are removed before discharge from the clinic.
Stitching usually takes about 30-45 minutes. A bandage is applied over the incisions. Pitocin is then given intravenously to contract the uterus. In that case, the operation was performed under local anesthesia, by this time you will feel sick and feel nauseous. Trembling throughout the body is also possible. It is not entirely clear where this reaction comes from, but everything goes away in about an hour. They may give medications that will make the woman in labor doze off or fall asleep for the entire period. It is necessary to ask in advance about these medications. It is possible to renounce them if desired. Warm blankets will help reduce shivering. In this case, general anesthesia was used, the woman in labor will remain unconscious for an hour or more after the operation.
In this case, the partner of the woman in labor is in the operating room and the baby’s condition is not bad, he will be able to hold the baby, and then both will be able to look and touch him. Otherwise, the child will be transferred to the neonatal ward, and the happy parents will see him later. In this case, the child breathes well and is generally healthy; he can be brought to the postoperative ward so that he can be held, nursed and breastfed. Nurses will closely monitor the baby for several hours or days, separately if there are difficulties with breathing, maintaining body temperature, or suspicion of other difficulties.
In the recovery room, the nurse will check your blood pressure, the condition of your stitches, the tightness of your uterus, and the leakage of lochia into the lining. The woman in labor will be monitored until the end of the anesthesia (from 2 to 4 hours).
In that case, the woman in labor was given spinal anesthesia; spinal pain in the head may appear when raising the head. In this case, she will be advised to lie down for 8-12 hours or a blood filling will be given. In that case, the operation was performed under general anesthesia; the throat and neck may hurt for a number of days due to the tube inserted there through which the anesthesia was administered.
Indications for caesarean section
A caesarean section may be needed in any of the following cases:
Craniopelvic disproportion
The baby's head is very large, and the mother's pelvis is very narrow, or a combination of both. Craniopelvic disproportion can rarely be diagnosed (although it can be suspected) before the onset of labor, since even in the case of a large baby’s head and a relatively small mother’s pelvis, the head shrinks slightly, and the pelvic joint moves apart during childbirth. In that case, quite some time had passed and the contractions were strong, but there was no progress in labor; a diagnosis of craniopelvic disproportion could be made. From time to time it is difficult to distinguish this case from poor fetal articulation.
Unsuccessful presentation or erection
The baby is placed in the uterus unsuccessfully for vaginal delivery. Examples could be a transverse position of the fetus (the baby lies horizontally), certain types of breech presentation (full or foot), facial and frontal presentation, a stable posterior occipital presentation, or asynclitism (the baby’s head is turned so that it does not fit into the pelvic inlet). Read more in the article about severe presentations.
Lack of progress (or prolonged labor)
Contractions are not strong enough or there is no progress in dilating the cervix and descending the fetus, even after attempts to relax the uterus or provoke stronger contractions. Such a diagnosis cannot be made before the onset of the active phase of labor (after 5 cm of dilation), since the usual latent phase often lasts a very long time.
Fetal disease
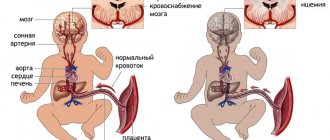
Special fetal heart rate patterns detected by auscultation or electrical monitoring devices may indicate difficulties with the baby. These configurations demonstrate that the baby conserves oxygen when its supply is limited (for example, when the umbilical cord is compressed or the blood flow to the placenta is reduced. The following tests - head stimulation or blood tests - will show whether the baby is well compensated or has begun to suffer from a lack of oxygen. B If the child is no longer able to cope with the lack of oxygen, a caesarean section is necessary.
The main danger of a lack of oxygen is that it (the lack) can cause brain damage (cerebral palsy, delayed intellectual development, epilepsy). Although brain damage can occur during childbirth, countless studies show that it occurs more often before labor begins, during pregnancy. Brain damage cannot be detected while the fetus is in the protective environment of the uterus. This can only appear after the onset of labor, when fetal pulse abnormalities are observed due to stress, or after the birth of the baby, when signs of neurological disorders occur. A caesarean section can neither prevent nor cure problems that have already occurred, although it can free such children from the stress of childbirth for which they are not prepared.
Umbilical cord prolapse
When the umbilical cord descends into the neck of the uterus before the baby, the baby's body can pinch the umbilical cord, reducing oxygen supply to hell, and an immediate caesarean section is necessary.
Placenta previa
The placenta covers (in whole or in part) the neck of the uterus. When the cervix dilates, the placenta separates from the wall of the uterus, causing painless bleeding in the mother and depriving the baby of oxygen. Placenta previa occurs approximately once in 200 pregnancies. This is a condition where the placenta is implanted (at least partially) to the neck of the uterus. A more relevant symptom is vaginal bleeding, in most cases after 7 months of pregnancy. Bleeding, usually intermittent, is not accompanied by pain. Healing may include bed rest, constant medical monitoring of mother and fetus, and cesarean section.
Placental abruption
The placenta is separated from the wall of the uterus in advance. This can cause bleeding from the vagina or hidden bleeding and constant pain in the tummy. Abruption reduces the oxygen supply to the fetus and, depending on the severity of the abruption, a cesarean section may be required. Detachment occurs in most cases in the third trimester or during childbirth. Although it happens from time to time in the absence of obvious circumstances, the risk is greater in women with high blood pressure or who smoke or drink heavily. In this case, the bleeding is small, the contractions last and the fetal heartbeat remains normal, doctors usually allow labor to continue as usual. Otherwise, a caesarean section is performed.
Threat of uterine rupture
This situation appears either during repeated births, in which case the first one was performed by cesarean section, or after other abdominal operations on the uterus, after which a scar remained. With normal healing of the uterine wall with muscle tissue, uterine rupture does not threaten. However, it happens that the scar on the uterus turns out to be insolvent, in other words, there is a danger of rupture.
The failure of the scar is determined by ultrasound data (the thickness of the scar is less than 3 mm, its contours are uneven and there are inclusions of connective tissue). The failure of the uterine scar may also be indicated by a complicated course of the postoperative period after the first operation: an increase in body temperature, inflammation of the uterus, long healing of the suture on the skin.
A cesarean section is also performed after 2 or more previous cesarean sections, since this situation also increases the risk of uterine rupture along the scar during childbirth. Numerous births in history, leading to thinning of the uterine wall, can also create a danger of uterine rupture.
Obviously, in each case, the condition of the scar is checked personally by ultrasound and more than once during pregnancy. So the doctor knows about the failure of the uterine scar in advance and can prescribe a planned cesarean section.
Mechanical obstacles
It is also possible to find in advance an indication for a cesarean section, such as mechanical obstacles that interfere with childbirth through the natural birth canal. This could be, for example, uterine fibroids located in the isthmus area, ovarian tumors, etc. In most cases, this obstacle is determined by ultrasound, and on its basis the doctor prescribes a planned cesarean section. The same applies to tumors and deformations of the pelvic bones, which will also prevent the child from passing through the birth canal.
Mom's illness
If the expectant mother has diabetes, unhealthy kidneys, asthma, hypertension, preeclampsia (toxicosis), heart disease or other serious illness, then the child may not be able to bear the stress of labor and birth through natural means. The presence of herpes in or near the vagina is also an indication for a cesarean section, since the baby can become infected when passing through the birth canal. Also, the indication for surgery is often the mother’s myopia of more than 5 diopters and the risk of retinal detachment, which leads to blindness. In this case, a caesarean section is used to eliminate pushing.
Multiple pregnancy
The possibility of a cesarean section for the birth of twins (or more twins) is higher due to possible complications, such as toxicosis, prematurity, breech presentation and umbilical cord prolapse.
Repeated caesarean section
A new cesarean section may be performed because the prerequisites for the first cesarean section are still present, or because the doctor or patient chooses a cesarean section over vaginal delivery. Also, an indication may be the poor condition of the postoperative scar on the uterus after a previous cesarean section.
For the next birth, vaginal delivery may be possible and even recommended in the near future, in which case there are no medical indications. If this new approach is accepted, the percentage of repeat cesarean sections will decrease.
Relative contraindications to caesarean section on the part of the mother
Diseases of the mother not related to pregnancy, in which the burden of natural childbirth threatens the life and health of the mother.
Such diseases include any cardiovascular pathologies, kidney diseases, high myopia with changes in the fundus of the eye, diseases of the nervous system, diabetes, cancer of any localization and some other diseases.
In addition, indications for a cesarean section are exacerbations in the mother of acquired diseases of the genital tract (for example, genital herpes), when during a natural birth the disease can be transmitted to the child.
Complications of pregnancy
A relative indication for a cesarean section is also certain complications of pregnancy that can endanger the life of the baby or the mother herself during natural childbirth.
First, this is gestosis - later aggravation of pregnancy, in which there is a disorder in the function of important organs, especially the vascular system and blood flow.
The severe manifestations of gestosis are preeclampsia and eclampsia. With all this, microcirculation in the central nervous system is disrupted, which can lead to severe complications for both the mother and the fetus.
Stubborn weakness of labor
A relative indication for cesarean section is stubborn weakness of labor, when labor that began normally subsides for some reason, or goes on for a long time without noticeable progress, and drug intervention does not bring success. In this case, with all this, the devices demonstrate that the fetal condition is worsening (for example, due to hypoxia), then surgical delivery may be possible.
Clinically narrow mother's pelvis
A situation where the size of a woman’s pelvis does not correspond to the size of the baby’s presenting part is also a relative indication for a caesarean section.
It is often possible to hear that for a primiparous woman, age over 35 years is also an indication for a caesarean section. This is not entirely true. A relative indication can be considered age over 35 years, coupled with pathology.
This means that in a situation where a younger woman has the opportunity to risk giving birth herself, a woman over 35 years old is better off not to do this. The simple fact is that after 35 years a woman’s general health is, most often, worse than in her first youth. Still, everything is decided personally, and age itself is not an obstacle to natural childbirth.
Pros of caesarean section
Medical indications for caesarean section: list
Relative indications for cesarean section do not exclude the possibility of vaginal delivery, but are a serious reason to think about their necessity.
In this case, vaginal birth may be associated with the possibility of a serious threat to the health and life of the mother and her baby, but this issue must be resolved individually.
Relative medical indications are:
- diseases and pathologies of the cardiovascular system in the mother
- kidney disease
- myopia
- diabetes
- malignant tumors
- exacerbation of any chronic diseases
- damage to the nervous system
- gestosis
- mother's age from 30 years
- malpresentation
- large fruit
- entanglement
IMPORTANT: The combination of several relative readings can be regarded as an absolute reading. In such cases, a caesarean section is performed.
Large fetus - relative indication for caesarean section
Indications
Indications for a caesarean section can be absolute when there is no other choice, since the life and health of the mother and child are in the balance. They can also be relative, when the threat is not so great. In the latter case, the spouses’ opinions are asked whether they agree to the CS or not. Depending on which side the pathologies are found on, the reasons for the operation may relate to the conditions of the woman in labor or the fetus.
Testimony from the mother
- Narrow pelvis;
- risk of uterine rupture;
- abnormal placenta previa;
- its detachment;
- scars on the uterus;
- previous corporal (peritoneal) caesarean section;
- T or J-shaped uterine incision;
- previously performed uterine operations of any nature;
- two or more CS already performed;
- HIV infection;
- genital herpes;
- any kind of cardiovascular disease;
- vision problems;
- pathologies of a pulmonary, neurological, gastroenterological nature;
- injuries, tumors of any origin of the pelvic organs;
- late toxicosis in severe form;
- plastic surgeries performed on the perineum;
- genitourinary or entero-genital fistulas;
- gastroschisis - prolapse of intestinal loops (this can be other internal organs) through a cleft in the abdominal cavity;
- teratoma - ovarian tumor;
- abdominal infections;
- uterine cancer;
- weak labor activity;
- gestosis;
- diabetes;
- preeclampsia is a type of gestosis with obvious signs of cerebrovascular accident.
Fetal indications
- breech or transverse presentation;
- malpresentation during multiple pregnancy;
- monoamniotic twins;
- too long dehydration in the fetus;
- twin fusion;
- delayed development of one fetus in multiple pregnancies;
- fetal hypoxia;
- premature birth.
Here are the cases in which a cesarean section is performed: the medical indications for this operation must be observed very strictly. In their absence, a woman’s mere desire to give birth this way is not enough. To carry out abdominal surgery, which will have a lot of consequences for the health of the mother and child, good reasons are needed. Fear of pain during childbirth is not one of them. After identifying the indications, a decision is made about a CS and the preparation stage begins.
Attention! If an ultrasound shows that monoamniotic twins are developing in the womb, they can be born exclusively by caesarean section. These twins develop in the same bladder, they share one placenta, and they cannot be born on their own without injury.
Risks of a caesarean section for a woman in labor
Like any other surgical procedure, a cesarean section can cause some difficulties and complications for the mother in labor. These include:
- Wound infection.
- Infection of the inner mucous membrane of the uterus - endometritis. Its consequences may include acute pain, unusual vaginal discharge, and fever.
- Urinary tract infection.
- The development of vein thrombosis, which, in the absence of emergency treatment, can result in rupture of blood vessels or blood entering the lungs.
- Bleeding.
- Damage to the urinary tract, which can only be repaired by surgery.
To prevent such complications from affecting you, make sure that you are given a special antibiotic before your cesarean section. Under its influence, infection and infection will be impossible.
But during a cesarean section, another dangerous complication remains possible - “aspiration”. We are talking about a situation where, due to gag reflexes, particles of stomach contents enter the lungs of a woman in labor. The consequences of aspiration are very serious - swelling or even inflammation of the lungs (aspiration pneumonia).
Aspiration can be prevented. To do this, before a planned cesarean section, a woman in labor should not eat or drink much, or even better, replace food with special isotonic drinks that contain equal amounts of salt and sugar and do not change the osmotic pressure of the blood. Thanks to this fluid, the pregnant woman's stomach will remain practically empty, but her body will receive enough energy to undergo a cesarean section.
Complications during surgery
Although caesarean section is used to reduce maternal and perinatal mortality, this operation is not completely safe.
Possible complications during surgical delivery:
- Injury to a large vessel (for example, the uterine artery).
- With a pronounced adhesive process, as a result of a significant change in tissue anatomy, in rare cases, damage to the intestines, bladder wall, and abnormally located ureters is possible.
- Bleeding from the placental site.
- Hematoma formation.
- Hypotonic bleeding (with a decrease in uterine contractility).
Risks of caesarean section for baby
There is no statistical evidence that surgical removal of a baby can cause health complications such as damage to the nerve endings of the arms and neck, intracranial hemorrhage, cerebral palsy or death. Such complications occur only in 20 cases out of 10 thousand, and they are not always associated with the actions of doctors.
Most often, in babies born by cesarean section, difficulties arise only with breathing, which becomes abnormally rapid (but this tendency is more likely to be characteristic of those babies who were born prematurely). But if a woman has surgery after 39 weeks, the risk of her baby developing breathing problems remains the same as during a vaginal birth.
Rapid breathing in newborns, which is medically referred to as “transient tachypnea,” usually lasts no more than 3 days. Only in some cases are children offered additional treatment with oxygen. But if your baby’s breathing really causes anxiety, consult your doctors about possible treatment.
What is a caesarean section: types of surgery
Caesarean section has a complex classification. It can be carried out in different ways and have corresponding features. We invite you to understand what types of this method of delivery there are:
- Caesarean section at the site of the incision of the uterus and abdominal cavity:
- Abdominal cesarean section - during which the doctor makes an incision either above the woman's pubis (the seam is horizontal) or from the navel to the pubis (the seam is vertical). This type of operation is the most common; everything is done very quickly so that the child does not receive the dose of anesthesia that was injected into the mother.
- Corporal caesarean section - during which the entire abdominal cavity is cut. With this type of operation, the likelihood of severe bleeding is low.
- Extraperitoneal cesarean section - during this, a longitudinal incision is made in the abdomen, as in an abdominal cesarean section, but it is slightly shifted to the left side so that only the muscles are dissected (for women who have already had several cesarean sections or other operations, this type of delivery is contraindicated).
- A vaginal cesarean section is an abortion that is performed in the first and second trimesters of pregnancy if a woman has a placental abruption or her health has deteriorated. With it, only a small part of the uterus along the anterior wall is dissected through the vagina. If placental abruption occurs already in the third trimester, then a small caesarean section is performed, during which not only the uterus, but also the cervix is cut.
- Caesarean section according to the urgency of the operation:
- Planned caesarean section - a woman prepares for it throughout her pregnancy if she has contraindications to natural childbirth. A caesarean section may also be planned in the last weeks of pregnancy after an ultrasound shows that the baby is in the wrong position in the womb and will not be able to be born on its own without injury or a threat to life.
- Emergency caesarean section - this operation is performed if natural childbirth is prolonged, serious complications of pregnancy have arisen (the placenta has separated, the woman has found herself in a force majeure situation - anything can happen here).
Any of the above types of cesarean section is today performed at a very high level by professional obstetricians and gynecologists. The risk to the health of the woman and her child is minimal.
Methods of anesthesia for caesarean section
There are general (endotracheal) and regional (epidural or spinal anesthesia) methods of pain relief for caesarean section.
Endotracheal anesthesia puts the woman in labor into a medicated sleep, and anesthesia is administered into the respiratory tract through a tube. General anesthesia works faster, but after waking up it often causes unpleasant consequences: nausea, shoulder pain, burning, drowsiness.
More on the topic Caesarean section: the pros and cons of the operation Is it possible to get pregnant a month after giving birth Natural birth after a cesarean section The condition of the uterus after a cesarean section Possible consequences of a cesarean section for the child and mother
An epidural involves an injection into the spinal canal. Only the lower part of the body is numbed. During the operation, the woman in labor is conscious, but does not feel pain. You won’t have to see the whole process—medical workers will hang a special screen at the level of the pregnant woman’s chest. After the anesthesia has taken effect, the doctor carefully cuts the abdominal wall, then the uterus. The baby is removed after 2-5 minutes. As soon as the baby is born, the mother can see him and attach him to the breast. Epidural surgery lasts about 40-45 minutes and is primarily suitable for mothers who are worried that under anesthesia they will not feel all the magic of childbirth and will not be the first to see their babies.
Caesarean section: history of occurrence
Caesarean section turns out to be an ancient operation. Thus, the world-famous commander Julius Caesar was born. It was he who issued a decree in his state that all women who could not withstand the pains of childbirth should have their bellies cut open and their children taken out so that they could live. There is a legend that the word “Caesarean” is associated with the name “Caesar” (in some sources Julius Caesar is spelled as Julius Caesar).
- The ancient Chinese also performed caesarean sections on their pregnant women. At the same time, they performed operations on living women who died, as a rule, after such births, because doctors then did not know how to sew up the uterus. The organ was constantly bleeding, and the woman died because of this.
- In 1500, the first successful caesarean section was performed by the Swiss Jakob Nufer. He was a veterinarian by profession, and mostly only castrated pigs. However, when his wife could not give birth for 3 days, the man turned to the local authorities with a request that they give him permission to cut his wife’s stomach and uterus so that his son could be born. Jacob received permission. He managed to save the life of his wife and child. In addition, after this operation, the son lived for 70 years, and his wife gave birth to several more children.
- The term “caesarean section” entered official medicine only in 1600, thanks to the scientific work of the French physician Jacques Guillemot.
- In 1846, caesarean sections reached a new level. During its implementation, doctors began to use ether as an antiseptic. As a result, the mortality rate of women in childbirth has decreased significantly.
- To solve the issue of postoperative bleeding, which caused so many women to die, the Italian professor Porro simply removed the pregnant woman’s uterus during the operation so that it would not bleed. This saved the lives of many, but made it impossible to ever have a child again.
- In 1882, a doctor named Saumlnger began the practice of placing silver wire sutures on incisions of the uterus. His innovation was a revolution in obstetrics.
- In the twentieth century, they began to use catgut threads when suturing a woman’s uterus and abdomen. Mortality decreased by 90%.
Today, special anesthesia is even used for caesarean section, which allows the woman in labor to be conscious at the time of the operation and see the birth of her child. This method of delivery in Germany is called “imperial birth”. The woman in labor lies calmly on her bed, sees and understands everything, and at the same time does not experience any pain from contractions and pushing. How good and bad this is, we will tell you later in this article.
How is the operation performed, what happens after it?
The operation begins with anesthesia. General anesthesia is possible; with local anesthesia, a special partition is placed on the chest so that the process, which lasts from 20 to 40 minutes, is not visible.
Remove the baby immediately, no later than 5 minutes.
How is a caesarean section performed?
- the abdominal cavity is cut, then the uterus and bladder;
- the doctor immediately removes the baby;
- while the midwife holds the baby, the doctor squeezes out the place;
- with special threads for operations that spontaneously resolve, the uterus is sutured. Then the abdominal cavity;
- the uterus must actively contract; for this, cold is placed on the stomach;
- The woman in labor is taken to her room.
After surgery you need recovery. A woman is prescribed painkillers because she is experiencing pain.
Antibiotics and anti-bloating medications are also possible. Constipation and gas formation after cesarean section are quite common.
After a day, doctors recommend moving and getting out of bed more often. For relief, you can wear a postpartum bandage. It helps tighten the stomach and reduce pain when walking.
After surgery, a diet is required. On the first day, only water is allowed. Then only light and liquid food.
If bowel function has been established for 3 days, the mother switches to normal nutrition, which is allowed during breastfeeding.
Progress of surgical birth step by step
It should be noted that there are many methods of performing the operation. The surgeon chooses a specific one depending on the situation, circumstances, anamnesis, indications and own preferences. There are techniques in which each layer is then cut and sutured, there are methods in which tissue dissection is minimized, and the muscle tissue is simply manually pulled aside. The incision can be either vertical or horizontal.
A low horizontal incision in the lower uterine segment is considered the best option, since such sutures heal better, allow you to endure a subsequent pregnancy without problems and even give birth to a second child naturally, if the woman wants it and there are no medical contraindications.
Whatever the method of delivery chosen by the doctor, the operation will include the main stages, which we will talk about in more detail.
Laparotomy
The abdomen is treated with an antiseptic, isolated from other parts of the body with sterile tissue, and the anterior abdominal wall is dissected. With a vertical dissection, an inferomedian laparotomy is performed - an incision is made four centimeters below the navel and brought to a point located four centimeters above the pubic symphysis. For a horizontal section, which is called a Pfannenstiel laparotomy, an arcuate incision is made along the skin fold above the pubis, 12 to 15 centimeters long, longer if necessary.
A Joel-Cohen laparotomy may also be performed, in which the incision is horizontal below the umbilicus but well above the peripubic fold. If necessary, this incision can be lengthened with special scissors.
The muscles are carefully moved aside, and the bladder is temporarily removed to the side so as not to accidentally injure it. Only the wall of the uterus separates the doctor from the child.
Uterine dissection
The reproductive organ can also be dissected in different ways. If the surgeon is a big fan of the traditional technique, he can make an incision along the body of the uterus horizontally, vertically along the midline using the Sanger method, or a pubic incision according to Fritsch, which passes through the entire uterus - from one end to the other.
The most gentle and recommended first is an incision in the lower segment of the female reproductive organ. It can be transverse according to Rusakov, semilunar or vertical according to Selheim.
The doctor uses his hand or a surgical instrument to open the amniotic sac. If the birth is premature, it is considered the best option not to open the membranes; it will be more comfortable for the baby to be born in them, and adaptation will be easier.
Fetal extraction
The most crucial moment is coming. When a child is born physiologically or during surgical procedures, doctors are equally worried, because the likelihood of injury to the fetus during a CS, although insignificant, still exists. To reduce such risks, the surgeon inserts four fingers of the right hand into the uterus. If the baby is positioned head down, the doctor's palm approaches the back of the head. Carefully cut the head into the incision on the uterus and remove the shoulders one by one. If the child is in a breech position, he is removed by the leg or inguinal fold. If the baby lies across, pull it out by the leg.
The umbilical cord is cut. The baby is given to a pediatrician, neonatologist or nurse in the children's department for weighing, placing a clothespin on the umbilical cord and other procedures. If a woman is not sleeping, then they show her the baby, tell her the gender, weight, height, and can put him to the breast immediately after birth. During surgical childbirth under general anesthesia, the meeting between mother and baby is postponed to a later time, when the woman comes to her senses and recovers from anesthesia.
Placenta extraction
The placenta is detached by hand. If it has grown in, it may be necessary to excise part of the endometrium and myometrium. In case of total ingrowth, the uterus is completely removed. The surgeon also inspects the uterine cavity, checks that there is nothing left in it, checks the patency of the cervical canal of the cervix; if it is impassable, it is dilated manually. This is necessary so that lochia (postpartum discharge) in the postpartum period can freely leave the uterine cavity without causing stagnation and inflammation.
Suturing the uterus
A single-row or double-row suture is applied to the cut edges of the uterus. Double row is considered preferable. It is more durable, although it takes a little longer to apply. Each surgeon has his own suturing technique.
The main thing is that the edges of the wound are joined as accurately as possible. Then the scar on the uterus will form smooth, uniform, and consistent, which will not interfere with the next pregnancy.
Suturing the abdominal wall
The aponeurosis is usually sutured with separate silk or vicryl threads or with a continuous suture. Separate staples or stitches are placed on the skin. Sometimes the skin is sutured with a continuous cosmetic suture, which is very neat.
Features of the postoperative period
After giving birth, the new mother is taken to the recovery room, where doctors monitor her condition. A woman in labor will be able to get out of bed only after 6 hours, and walk after three days. Then the woman undergoes an ultrasound and tests, and if all is well, she is discharged in a week.
It will take 6-8 weeks for the mother’s body to recover. During this period, you should not lift weights, get your stitches or stomach wet during the first week. Doctors also do not recommend exercising, resuming sexual activity, or taking a bath for 3-4 months after a cesarean section—only showering is allowed. Obstetricians advise planning to become pregnant again no earlier than in one and a half to two years. And don’t be sad: even if a woman gave birth for the first time by cesarean section, the second baby still has a chance to see the world naturally.
For some time after a cesarean section, the woman in labor is bothered by the stitches - for several weeks the wound aches, hurts, and sometimes itches. The incision on the uterus is sutured with self-absorbing or removable threads. The latter are removed in a week. If suddenly complications arise - suppuration or diastasis (divergence) of the sutures - consult a doctor immediately.
How long does it take for a stitch to heal?
Pain in the suture area will be most severe on days 1–3 after surgery, then its intensity gradually decreases. If there is persistent pain on days 5-6, it is possible that nerve endings are involved in the scar. The discomfort will pass, but it will take a longer period.
Discharge during CS occurs on days 5–7, depending on the condition of the mother and child. At the same time, the woman can already move around calmly.
When does the seam become invisible? This depends on the tissue’s ability to regenerate and the suture material used. Catgut completely dissolves in 30 days, Vicryl in 2-3 months, Maxon in about six months.
Adaptation to normal life after cesarean section
Complete restoration of tissues, the integrity of which was damaged during cesarean section, will occur only after 6 weeks. However, even during this period, a woman will be able to practically fully care not only for herself, but also for her baby.
During the recovery period after cesarean section, a woman is not recommended to perform sports exercises, carry heavy loads and have sex. You should begin such tasks only after you have regained confidence in your abilities and the danger of tearing the seams has disappeared. Contact a doctor if you cannot independently determine the condition of your postoperative wound.
You should also not start driving a car immediately after a cesarean section, as a sitting position may be uncomfortable for you, and the need to press the pedals may cause pain in the scar area. Please note that many insurance companies do not agree to compensate for damages caused by a woman driving a car after such an operation. Therefore, before driving, you should wait until the wounds have completely healed.
Features of the recovery period after cesarean section
The most difficult thing after a cesarean section is the recovery process. It includes a lot of restrictions that do not allow a new mother to fully live and care for her newborn child:
- You need to eat only diet food. The diet should include foods that do not provoke allergic reactions and stimulate the restoration of the digestive tract.
- To get rid of excess weight gained during pregnancy, you need to wait at least 9 months after giving birth. You need to take care of yourself very carefully so that the seam does not rupture.
- The uterus will take longer to recover after a caesarean section. Therefore, discharge from it will continue for 2-2.5 months.
- A woman who has had a caesarean section can have sex only after 4 months, and then after she visits a doctor, and he is convinced that sexual intercourse will not pose any threat to life.
- At first, a woman will have to constantly treat her suture, which may bleed and ooze. This is a very painful process - treating the wound and making bandages, but it cannot be avoided in any way, so as not to introduce infection into it.
Every new mother should receive tremendous psychological support from her family. They need to take on all the housework so that the woman can recover after the operation.
Is natural childbirth possible after cesarean?
After two months, the body fully recovers after the operation. Intimate relationships are allowed again, but doctors advise using protection for a couple more years.
Afterwards you can become pregnant and possibly give birth on your own. It all depends on how well the scar has healed, what condition the uterus is in, and so on.
During pregnancy, the doctor will monitor the condition of the mother and fetus.
In the absence of contraindications, the likelihood of natural childbirth is high.
Recovery process
Recovery may take a long time. It is believed that this occurs within two months. Recovery takes place in two stages. The first is carried out in a hospital. Specialists prescribe daily treatment of sutures. The technical process is carried out using antiseptic solutions. The patient is also observed by a gynecologist. Accumulation of fluid in the uterine cavity and bleeding should be excluded. Only after this can mom be discharged home.
At home, you must adhere to a special diet. After surgery, a decrease in the absorption capacity of the intestine is observed. This may cause problems with bowel movements. To avoid problems you need to eat right. The diet excludes salty, fried and fatty foods. It is also recommended to avoid various fruits containing acids. Compliance with all these conditions contributes to the rapid healing of wounds.
It is also necessary to avoid carrying heavy objects.
This is especially recommended in the first days after childbirth. When the muscle frame is strained, suture separation may occur. This circumstance also applies to carrying a child in your arms. If a woman does not do this, the healing time increases. Many couples cannot get pregnant for a long time. This also causes anxiety during pregnancy. Surgery is used to preserve the health of the mother and fetus. It's easy to do. You should consult your doctor for advice.
Advantages and disadvantages
Of course, the most important advantage is the birth of a baby, while natural childbirth is impossible.
In addition, we can highlight:
- The genitals remain intact, there are no tears or seams.
- The genitourinary system is not affected.
- Childbirth occurs faster than the normal birth process.
In addition to the positive aspects, mom needs to be prepared for negative consequences, namely:
- A feeling of alienation towards the baby, the maternal instinct can wake up much later than during natural childbirth.
- Recovery after surgery is longer.
- Physical activity is excluded; during the first days you cannot hold the child in your arms.
- Scar on the body.
- Possible pain in the stitches.
Important! If you're thinking about having a surgical birth, talk to your doctor and learn all about cesarean section. Do not rule out the possibility of a natural birth just because of pain.
Advantages and disadvantages
Doctors in different countries have significantly different opinions about how justified a cesarean section is without direct indications. In a number of states, the desire of a woman is put in first place - trying to rid herself of ruptures of the external genitalia, the inevitable expansion of the vagina, as well as labor pains. The World Health Organization takes a different position - emphasizing that getting rid of some unpleasant consequences can bring others (problems with lactation, long postoperative recovery, etc.).
Since there is currently no single approach to how and why to choose one way or another, we will list the main pros and cons of childbirth by cesarean section.
Advantages
- The first important advantage is that the operation lasts no more than 20-40 minutes. (while traditional delivery can last more than 12 hours);
- the second advantage is the preservation of the genital organs intact (which is especially important for women who have an active sex life).
Flaws
For moms:
- prolonged pain that finally goes away no earlier than a few months later;
- inability to live a full life (including sexual life) for some time;
- a scar remaining on the abdomen;
- psychological discomfort (some women feel “guilty” for allegedly not giving birth to a child the way they should have, naturally).
For children:
- partial penetration of anesthesia drugs into the baby’s blood;
- non-zero probability of amniotic fluid entering the baby’s lungs;
- There are still unconfirmed (although not refuted) statements according to which children born by Caesarean section lag behind their peers in development and are less psychologically stable.
Consequences of the operation
The consequences after cesarean section for the mother include:
- stitches after surgery. Possible complications, discrepancies between the rectus muscles;
- restoration of menstruation. If the operation was completed without complications, then the menstrual cycle quickly becomes the same as it was, otherwise it takes a long time;
- At best, sexual life can begin after 2 months, with contraception. In the worst case, with the permission of the gynecologist after consultation. Abortions and other operations on the uterus cannot be performed for 2-3 years;
- full physical activity can be started no earlier than after 8 weeks;
- After surgery, various drugs and antibiotics are often injected. They affect breast milk, so babies are not put to the breast right away. Subsequently, it is difficult for the mother to establish lactation.
For a child, surgery is also stressful. It does not pass through the birth canal, so it is believed that its adaptation occurs much later.
In rare cases, anesthetic substances enter the child’s bloodstream, which depress the nervous system of the newborn and develop certain diseases.
Complications
The most common complications after childbirth surgery:
- the appearance of adhesions;
- bleeding;
- inflammatory process, fever;
- purulent discharge on the sutures;
- swelling and redness, scar separation;
- the appearance of compactions.
Some complications can be avoided by following a postoperative regimen. But most of them depend on a successful caesarean section.
When is the intervention carried out?
You should know what a caesarean section is. This is a surgical form of induced childbirth. Like all operations, the section is carried out within a certain time frame.
Women wonder what week they have a caesarean section. Often exposure is carried out at the end of the last trimester. For many it is carried out at 38 weeks. But sometimes, for various reasons, intervention is carried out earlier. The 36th week is considered a safe period. How many weeks the intervention is performed depends on the obstetric date of the expected birth. This is what doctors use before performing a caesarean section.
Preparatory activities
Like all operations, cesarean surgery requires certain preparation of the patient. The measures depend on what types of cesarean section will be used and at what time the operation is performed. There are general requirements that must be met before an intervention is carried out:
- cleansing the intestines of waste products;
- nutritional features;
- medical examination.
The woman must go to the hospital several days before the operation. Before starting the procedure, she must undergo a full examination. This process is necessary to prevent the child from becoming infected. A blood sample, urine and bacterial culture of the vaginal microflora are taken.
A day before the section, the woman is prescribed a special diet that promotes rapid bowel movements. If self-cleaning does not occur, then an enema procedure is prescribed. In the morning, the patient is prohibited from eating; drinking is stopped 3 hours before the section. Only after all these measures are surgical interventions permitted.
Diet and exercise
After a CS, the maximum weight a woman can lift for 2 months is 3-4 kg. It is important that in the first postoperative days there is a loved one nearby who takes care of the child.
The first physical activity is on the first day after surgery. This is wiggling your fingers and feet, bending and straightening your legs at the knees, raising your arms above your head, turning your head to the sides, and gently turning to your side. After discharge, slow walks are a useful and safe form of exercise.
Nutrition on the first day after surgery is limited to drinking water with lemon. On the 2nd day you can eat low-fat broth, after that - cottage cheese, yogurt, meatballs. Products are introduced into the diet gradually, observing the principles of fractional nutrition.
Caesarean section is a procedure that cannot be “asked” from the doctor, and which cannot be refused if indicated. The health or even the life of the mother and newborn depends on the right decision. It is recommended to prepare for the process psychologically, discuss the possible consequences with a doctor, and conduct a thorough preliminary examination.
At home after CS
If an older child is waiting for his mother at home, then you should try to pay attention to him, but not pick him up. Also, under no circumstances should you be nervous. And of course, you shouldn’t forget about your diet, which may become more familiar, but still the use of some foods should be canceled. In just 10-14 days you will be able to take a shower, but you should forget about the bath for at least a month and a half. And for two months you should avoid strenuous physical activity. And an important issue will be contraception. After all, planning the next pregnancy is possible only in two years.
How many times can you have a caesarean section?
It is recommended to perform no more than 3 caesarean sections.
A scar on the uterus is not a limitation for subsequent pregnancy, but you should refrain from planning a child for at least 2 years. Both conception and termination of pregnancy are prohibited. There are cases when women underwent 4-5 CS operations without harm to their health, but the risk of complications is higher each time. In each specific case, you should focus on the individual characteristics of the body.
Singer, designer, businesswoman Victoria Beckham underwent 4 caesarean sections, and Ethel Kennedy had 11 operations.
Planned and emergency caesarean section
Planned surgery is always preferable to emergency surgery.
Lack of proper preparation for the operation, organizational problems, and the woman’s psychological unpreparedness - all this increases the risk of complications.
Absolute indications for elective caesarean section:
- Placenta previa.
- Oblique or transverse position of the fetus.
- Two or more scars on the uterus.
- Third and fourth degree of pelvic narrowing.
- Extensor insertion of the head (anteroparietal, frontal, facial).
- Pelvic tumors that prevent natural childbirth.
- Diseases of the mother in which natural childbirth is contraindicated (for example, high myopia).
- Multiple large uterine fibroids.
- Severe symphysitis.
- Genital herpes in the acute stage.
- History of maternal injuries (surgeries on the hip joints, pelvic bones, ankylosis of the hip joints).
- Some malformations of the child (omphalocele, gastroschisis, hydrocephalus).
Relative readings:
- Breech presentation of the fetus in combination with a large fetus, or an extended head.
- Scar on the uterus.
- Aged primigravida.
- Pregnancy resulting from assisted reproductive technologies.
- Long-term history of infertility.
- Multiple pregnancy.
- Chronic fetal hypoxia.
Electively, a caesarean section is usually performed at 40 weeks' gestation, which usually coincides with the estimated due date.
Preparation for surgery:
- In the evening and morning, two hours before the operation, it is necessary to do a cleansing enema.
- The patient should not eat or drink on the day of surgery.
- Elastic bandaging of the lower extremities is necessary to prevent thrombotic complications.
- The night before surgery, rest and proper sleep are necessary.
In what cases is an emergency caesarean section performed (absolute indications):
- Placental abruption.
- Loss of umbilical cord loops.
- Loss of fetal parts
- Clinically narrow pelvis.
- Preeclampsia.
- Eclampsia.
- Threatening uterine rupture.
- Discoordination of labor.
- Acute intrauterine fetal hypoxia.
- The agony of a woman.
Relative readings:
- Prenatal breaking of water in combination with the unpreparedness of the birth canal for childbirth.
- Weakness of labor.