Labyrinthopathies are the general name for non-purulent lesions of the inner ear. The most common diseases in this group are vestibular neuronitis, cochleopathy and Meniere's disease. Clinical manifestations include sensorineural hearing loss and vestibular syndrome of varying severity. Diagnosis is based on anamnestic data, results of otoscopy, Rinne and Weber tests, vestibular tests, audiometry, CT, MRI. Treatment is complex and involves the use of medications, physiotherapeutic agents, and, if necessary, surgical interventions.
Labyrinthopathies
Labyrinthopathies are a common group of diseases of the hearing system. The incidence rate is between 12-15 cases per 10,000 population and continues to increase every year. Meniere's disease is most common in the population. After exacerbations, from 32 to 65% of patients lose their ability to work for a long time, and 11-19% eventually become disabled due to complete loss of hearing. People in adolescence and middle age, from 18 to 50 years old, are most susceptible to diseases of this group. Pathologies are widespread, occurring with equal frequency among males and females.
Etiology
The source of infection is most often a focus of inflammation in the cavities of the middle ear or skull, located in close proximity to the labyrinth, but the disease can also occur as a result of hematogenous (through vessels and lymphatic pathways) spread of infection.
Inflammation of the middle ear is the most common cause of labyrinthitis. Infection from the labyrinth can spread to the meninges or brain matter. As a result, various intracranial complications may occur (meningitis, subdural abscess, brain and cerebellar abscesses).
Based on the prevalence of the inflammatory process, a distinction is made between limited labyrinthitis, when the inflammatory process is noted in one part of the labyrinth, and diffuse labyrinthitis, which involves the entire labyrinth.
According to the severity of clinical symptoms - acute and chronic.
According to the nature of inflammation, labyrinthitis is divided into aseptic, serous, purulent and necrotic.
Due to the widespread use of antibiotics, purulent and necrotizing labyrinthitis are now less common, and there is a tendency towards an increase in its local, limited forms.
Causes of labyrinthopathy
The etiology of the diseases is not fully understood. In young patients, the cause of changes in the cochlear or vestibular apparatus often cannot be determined. In people over 60 years of age, labyrinthopathy is regarded as a result of natural aging processes. It is customary to identify a number of factors that can potentiate the development of pathologies of the inner ear. These include:
- Mechanical impact. Tissue dystrophy of the organ of Corti may be associated with chronic acoustic trauma and severe traumatic brain injury in the temporal region. Sometimes the cause of the disease is the consequences of previous surgical interventions in this area.
- Chemical substances. Damage to the inner ear can be caused by a variety of poisons and toxins that the patient comes into contact with at home and at work. Their list includes quinine, aniline, hydrogen sulfide, gasoline, fluorine, sulfuric acid, mercury, arsenic, phosphorus. Food poisoning from spoiled meat, fish, and low-quality alcohol plays a similar role.
- Bacterial toxins. Dystrophic reactions are triggered by exotoxins and endotoxins, produced in large quantities by pathogens of the following infectious diseases: typhoid and typhus, measles, malaria, scarlet fever, influenza, mumps.
- Disorders of local and systemic metabolism. Dysfunctions of the labyrinth occur against the background of severe hypovitaminosis, endemic goiter, gout, toxicosis of pregnancy, menopausal hormonal imbalance, and diabetes mellitus. Local trophic changes can be caused by pathologies of regional blood vessels: atherosclerosis, developmental anomalies.
Pathogenesis
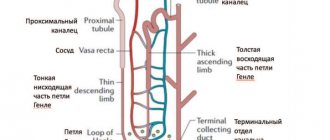
The pathogenesis of labyrinthopathy is based on several factors: disruption of the autonomic innervation of blood vessels, excessive secretion of endolymph (hydrops) and deterioration of its reabsorption. An increase in the volume of the ear lymph causes an increase in the size of the endolymphatic and a compensatory decrease in the perilymphatic space. As a result, the pressure inside the labyrinth cavity increases and the receptors of sensitive structures are irritated. The first to suffer are hair cells, regional nerve fibers and structures of the spiral ganglion, mainly the main helix. Subsequently, supporting cells are involved in the process, which causes atrophy of the entire organ of Corti.
Symptoms of labyrinthopathy
The clinical picture often occurs soon after acute respiratory viral infections, influenza and other infectious diseases. The main manifestations are vestibular syndrome and sensorineural hearing loss. The first is accompanied by unsteadiness of walking with nausea, vomiting, tachycardia, increased breathing, and sweating. In some patients, against this background, stool disorders such as diarrhea are observed. Patients also complain of motion sickness in transport, episodes of dizziness, aggravated by sudden turns of the head. Spontaneous horizontal nystagmus often develops.
Sensorineural hearing loss is characterized by a progressive decrease in hearing acuity. The perception of whispered speech and spoken speech in conditions of extraneous noise deteriorates, then difficulties appear during normal communication. Often a ringing or humming occurs inside the ears, drowning out all perceived sounds, causing patients to experience a feeling of “stuffiness.” In Meniere's disease, all symptoms have a paroxysmal course; there is an alternation of labyrinthine crises lasting from 5 to 48 hours with periods of remission lasting from several days to months.
Classification of the disease
The prevalence of the pathology among other inflammations of the inner ear is up to 4.2%; no age or gender predisposition has been identified; it is equally common in adults and children of both sexes.
Labyrinthitis has a large number of types, the definition of which takes into account the pathogens, the nature of the inflammation, the area of damage and concomitant pathologies.
There are the following types of disease:
- Hematogenous - occurs as a result of the entry of pathogens of viral infectious diseases into the inner ear through the bloodstream;
- Diffuse (purulent or serous) - affects all parts of the membranous or bony labyrinth;
- Purulent - caused by pathogenic microorganisms of purulent infection, characterized by the appearance of granulations;
- Meningogenic - occurs as a result of meningitis, when the pathogen affects the inner ear, penetrating through the internal auditory canal, cochlear aqueduct or subarachnoid space;
- Necrotic - the appearance of locations with dying soft tissue and areas of the bone labyrinth, often alternating with purulent foci;
- Limited - with this type, only the area of the bone labyrinth is affected; such inflammation is often associated with cholesteatoma pressure or the development of granulating otitis;
- Acute (purulent or serous) - occurs suddenly and is accompanied by such severe symptoms as dizziness, nausea, vomiting, disturbance of static or dynamic balance, noise in the ear, decreased hearing acuity. The serous subtype is characterized by the disappearance of symptoms 2-3 weeks after appearance, and the purulent subtype is characterized by a transition to a chronic form;
- Serous - characterized by swelling of the endosteum of the labyrinth, an increase in the volume of the perilymph, the appearance of blood cells in the peri- and endolymph of fibrin (fluids that are responsible for conducting sound vibrations);
- Tympanogenic - provoked by the penetration of a virus or bacteria through the windows of the labyrinth and the cavity of the middle ear;
- Traumatic - the trigger for development is severe trauma (gunshot wound to the head, fracture of the base of the skull);
- Chronic - symptoms are mild and develop gradually.
Attention, the content may be unpleasant to view.
Surgery for purulent diffuse labyrinthitis
Infection can spread to the medulla or lining of the brain, which causes the development of serious complications such as abscesses (brain, cerebellum, subdural), meningitis.
It is precisely because of the risk of increasing the area of inflammation that diagnosis and treatment of labyrinthitis at an early stage of occurrence is important.
Complications
Complications of labyrinthopathy are associated with the lack of timely elimination of etiological factors and adequate therapy. Most often, the progression of inner ear diseases leads to worsening sensorineural hearing loss. This, in turn, causes disability and loss of performance. Significant impairment of auditory function and complete deafness can cause the formation of psycho-emotional disorders, including severe depression. In elderly people, labyrinthopathy in combination with cerebral vascular lesions provokes progressive memory loss, deterioration of thinking processes, and the development of sound hallucinations.
Symptoms
The symptoms of the disease are quite varied and they can manifest themselves either partially or in full. They are most pronounced in the case of the development of an acute process. The general clinical picture is represented by the following symptoms:
- sweating;
- nausea and vomiting;
- pale skin;
- loss of coordination;
- dizziness;
- tachycardia.
Symptoms of labyrinthitis
Dizziness occurs in attacks. One such attack can last from two minutes to several hours. The patient experiences nausea and vomiting. Symptoms intensify if a person tries to make any movements. Loss of balance can vary in severity. A person may only stagger slightly and may even fall while walking.
On the second day of the disease, the patient experiences the following symptoms:
- earache;
- noise in ears;
- hearing loss. In case of development of an acute purulent process, deafness is observed.
If the catarrhal form of labyrinthitis is diagnosed, the symptoms usually disappear within 5 days from the onset of the disease. If complications develop, the symptoms last for another two weeks. It is important to begin treating the pathological process in a timely manner, since without adequate therapy the process of death of the nerve receptors that are located in the cavity of the inner ear will begin. This causes complete hearing loss. It is impossible to restore it.
Diagnostics
Making a diagnosis of labyrinthopathy is associated with certain difficulties due to the lack of objective changes during otoscopy and signs of inflammatory reactions in blood tests. Anamnesis plays an important role. When interviewing a patient, the otolaryngologist pays attention to the patient’s working conditions - contact with chemicals or prolonged exposure to noise. The doctor determines the presence of recent severe infectious diseases, concomitant metabolic disorders, and surgical interventions on the temporal bone. Further examination includes:
- Samples with tuning forks. The Weber test reveals deterioration in sound perception on both sides. When the pathological process is more pronounced on one side, the vibration of the tuning fork is better perceived on the opposite side. With the Rinne test, patients hear sound better when the tuning fork is positioned directly opposite the ear canal.
- Tone threshold audiometry. On the audiogram, patients with labyrinthopathy show a decrease in both air and bone conduction, which indicates damage to the sound-receiving apparatus located in the inner ear.
- Vestibular tests. When performing the Romberg test, the patient’s inability to maintain balance is revealed. When studying the function of the vestibular apparatus by cephalography, type III of the image is obtained, corresponding to bilateral damage to the labyrinths.
- MRI and CT scan of the temporal bone. Computed tomography or magnetic resonance imaging is prescribed to exclude other possible lesions of the structures of the inner ear: benign and malignant tumors, developmental anomalies, traumatic injuries. Sometimes it is possible to determine the deformation of the membranous labyrinth in the photographs.
How is labyrinthitis diagnosed?
If there are typical complaints of paroxysmal hearing loss, systemic dizziness and ear pain one to two weeks before the disease, it is not difficult to suspect a diagnosis of labyrinthitis. In the chronic course of the disease, clinical manifestations may be erased. Vestibular tests and the appearance of hidden nystagmus help in making a diagnosis.
Treatment of labyrinthopathy
The main treatment is carried out on an outpatient basis, with physical activity, training of the vestibular apparatus and supportive drug therapy playing a major role. During severe exacerbations, the patient is hospitalized in an otolaryngological hospital, where he is prescribed bed rest and intensive infusion therapy. The treatment program consists of the following activities:
- Pharmacotherapy. Depending on the clinical situation and etiology of labyrinthopathy, neuroleptics, diuretics, vasodilators and angistamines, calcium, bromine and iodine preparations, anticholinergics, strychnine, vitamins B and C are used. Immediately after attacks, acidosis is corrected by infusion of sodium bicarbonate.
- Surgery. Indicated when pharmacotherapy is ineffective. The purpose of the operations is to decompress the endolymphatic space and improve the outflow of endolymph. This effect can be achieved by drainage through the tympanic cavity, perforation of the base of the stapes, fenestration of the semicircular canal, and laser destruction of the labyrinth. Chemical ablation is also performed with alcohol or streptomycin.
- Physiotherapy. In the interictal period, darsonvalization, electrophoresis with previously prescribed drugs, and ultraviolet irradiation are used to normalize regional blood circulation. Sea and pine baths have positive properties.
Prognosis and prevention
The prognosis for life is favorable, but for health it is doubtful. The outcome of the disease largely depends on the etiology of labyrinthopathy, the timeliness and quality of treatment. Most patients eventually have to use external hearing aids or resort to surgical hearing aids. Prevention of this group of pathologies consists of eliminating or minimizing contacts with ototoxic substances, early treatment of infectious pathologies, correction of metabolic disorders, limiting the time of work in noisy rooms and the use of personal protective equipment.
| Literature1. Diagnosis of early forms of labyrinthopathy of professional origin: Abstract of the dissertation / Voloshin I.M. – 2007.2. Neuro-otorhinolaryngology: A guide for doctors / Babiyak V.I., Gofman V.R., Nakatis Ya.A. – 2002.3. Otorhinolaryngology in clinical practice – Lopatin A.S. – 2012. | ICD-10H83.2 code |
VKontakte
LiveJournal