Editor
Natalia Lebedeva
Pulmonologist
Focal pneumonia is an inflammatory process of the lung, predominantly of alveolar or interstitial tissue, affecting, unlike lobar pneumonia, only a limited area of the lung tissue: one or several segments of the lung.
Small foci can merge with each other, forming confluent pneumonia, which is more difficult and less treatable.
Classification according to ICD-10: categories J12-J18 .
Causes
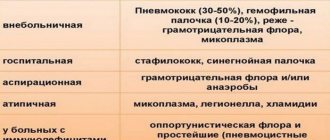
The etiology of pneumonia is divided into several forms.
Primary forms - the inflammatory process develops against the background of previously healthy lungs and is not a complication of another disease. Most often, infectious pathogens act as the damaging agent:
- bacterial: pneumococci;
- staphylococci;
- streptococci;
- mycoplasma;
- chlamydia;
- legionella;
- influenza virus;
- candida;
- caused by several pathogens at once.
Read more about the different types of pathogens
Secondary forms - the disease is formed as a complication of another disease.
Often these reasons are:
- acute respiratory viral infections (ARVI);
- acute or chronic bronchitis;
- extrapulmonary abscesses.
One of the forms also includes pneumonia with activation of opportunistic microflora in people with immunodeficiency (persons taking immunosuppressants, HIV-infected people).
More about pneumonia due to HIV
Factors contributing to the development of pneumonia:
- excessive emotional stress, stress;
- malnutrition, lack of vitamins and minerals;
- presence of bad habits: smoking;
- drinking alcohol;
- addiction.
Causes of the disease
Acute focal pneumonia most often acts as a complication that develops against the background of a severe course or complete lack of treatment for another pathology. In such situations, the formation of an inflammatory process may be caused by the following ailments:
- myocardial infarction;
- acquired, less often congenital heart defects;
- bronchitis and ARVI;
- malignant or benign tumors;
- measles and whooping cough;
- meningitis and scarlet fever;
- acute catarrh of the respiratory tract;
- furunculosis and typhoid fever;
- influenza and sepsis;
- chlamydia and osteomyelitis;
- purulent otitis and peritonitis;
- any pathologies of a purulent nature;
- diseases of the lungs and respiratory organs that have a chronic course.
It is noteworthy that in addition to the above factors, focal pneumonia in children can be caused by a severe stressful situation or nervous overstrain, as well as the influence of such factors:
- hypothermia of the body;
- penetration of a foreign object into the bronchi;
- inhalation of toxic or poisonous substances.
In cases where inflammation of the lung lobule acts as an independent disease, the pathology is caused by the influence of pathogenic agents, which are:
- pneumococci and staphylococci;
- streptococci and Escherichia coli;
- proteus and Friendlander's wand;
- influenza A and B viruses;
- microscopic fungi;
- mycoplasma and adenovirus;
- parainfluenza virus and rhinovirus.
It must be taken into account that most often the above microorganisms influence the development of community-acquired pneumonia.
Also among the predisposing factors, clinicians identify:
- lack of physical activity;
- decreased immune system resistance;
- excessive addiction to bad habits, in particular smoking cigarettes;
- poor nutrition;
- hypovitaminosis;
- previous operations, no matter what area the surgery was performed on;
- prolonged overheating of the body.
The pathogenesis of focal pneumonia has some features:
- localization of inflammation in one or more lobules of the lung;
- slow development of the pathological process, which is explained by the small area of the affected area;
- acquisition of intense permeability by the walls of the lung;
- a smooth transition from one degree of severity to another, while the symptoms do not change dramatically.
Pathogenesis
The mechanism of development of the focal form of pneumonia is the introduction of a pathogenic pathogen into the lung tissue. The bacterium begins to rapidly multiply, causing a focus or several lesions (focal-confluent form) of inflammation. The body produces antibodies against the microorganism, which, when interacting with it, releases cytokines that damage lung tissue. The liquid part of the plasma leaves the bloodstream and permeates the alveoli. Subsequently, the dead tissue is replaced by new one.
Routes of penetration of pathogenic agents:
- hematogenous – through the circulatory system;
- lymphogenous - through the lymphoid system;
- contact – transition of the inflammatory process from nearby tissues and organs;
- bronchogenic – entry of microorganisms along with inhaled air;
- aspiration - aspiration of contents from the nasal or oropharynx.
Morphological features of focal pneumonia:
- most often occurs in the posterior and posteroinferior segments of the lung;
- foci of inflammation are observed within the lobule;
- dense, have a bright appearance when cut;
- in the alveoli there is an accumulation of exudate with an admixture of cellular elements;
- serous nature of alveolar exudate;
- exudate is distributed unevenly, in some alveoli there is more of it than in others;
- bronchioles are infiltrated with leukocytes;
- Goblet cells predominate in the epithelium of bronchioles.
Online test: are you treating pneumonia correctly?
Causes of focal pneumonia
The reasons are multifaceted, but are entirely related to seasonality, falling during cooler seasons and epidemiologically unfavorable periods. Also, etiopathogenesis is directly proportional to the routes of spread of infection, namely lymphogenous, bronchogenic, hematogenous routes.
Signs of focal pneumonia are associated with a functional decrease in local and general body defenses, these include:
— Stressful conditions and influences in the neurological area that deplete the body.
— Poor nutrition and, as a result, hypovitaminosis and lack of mineral components.
— Adverse habits such as smoking, abuse of alcoholic beverages, potent medications or drug addiction.
- History of chronic diseases and frequent colds.
— Decreased immunity of any etiology.
— Infections of the otorhinolaryngological area.
— Prolonged cooling or overheating.
— Insufficiently physically developed organism, physical inactivity and lack of hardening.
— Inhalation of substances with a toxic effect, tropic to the lung tissue.
- Reduced ventilation characteristics of the lungs.
— Damaging meteorological factors due to fluctuations in air humidity, changes in barometric pressure indicators.
Pneumotropic pathogenic agents are pneumococci in 78% of cases, streptococci, staphylococci, Escherichia coli, respiratory syncytial viruses, parainfluenza viruses, Friedlander's bacillus, mycoplasmas, microbial associations, microscopic fungi, adenovirus, rhinovirus.
Secondary signs of focal pneumonia develop against the background of already present diseases, such as measles, scarlet fever, whooping cough, chlamydia, meningococcal meningitis, typhoid fever, liver abscess, dysentery, peritonitis, purulent otitis, furunculosis and osteomyelitis.
In focal form can occur:
- Aspiration form, when foreign substances penetrate into the lungs - toxic gases, tiny solid particles, food grains. The likelihood of aspiration of vomit is especially high in cases of loss of consciousness during vomiting and severe alcohol intoxication.
— Congestive pneumonia occurs in seriously ill, bedridden people and the elderly, as a result of physical inactivity. Against this background, stagnation occurs in the pulmonary circulation, which leads to impaired ventilation of the lungs with excess production of pathogenic sputum. Occurs with ischemia and stroke, heart defects, diabetes mellitus, bone and spinal column fractures, and cranial injuries.
Classification
By volume of lung damage:
- unilateral (left- or right-sided);
- two-sided.
Depending on the size of the focus, there are: small-focal and large-focal.
By current speed:
- Acute – symptoms develop over several days, a clear clinical picture.
- Protracted or chronic - the pathological process does not end within 4 weeks.
- Asymptomatic or hidden - described by an atypical or mild clinical picture (no cough, fever).
For reasons of occurrence:
- Primary and secondary (described above);
- Radiation – stands out as a separate form in the treatment of malignant lung tumors using x-rays.
- Toxic - formed as a result of inhalation of toxic substances that primarily affect the lungs.
- Post-traumatic – develops as a result of a violation of the integrity of the chest (surgery, trauma), which leads to disruption of bronchoalveolar lavage, which contributes to the development of infectious processes.
According to severity:
- mild severity: mild discomfort;
- minimal intoxication;
- 0 or 1 degree of respiratory failure;
- low-grade fever.
- moderate intoxication syndrome;
- febrile fever;
- psychosis;
If subdivided by the prevalence of the pathological process, focal pneumonia can be lobular.
Symptoms of focal pneumonia
The symptom complex includes:
— General manifestations in the form of migraine pain, loss of appetite, weakness and sweating, the addition of respiratory failure, cyanosis of the skin, often patients report chest pain when inhaling and exhaling and coughing, hyperthermia up to 38.2 - 39.6 ° C, in the weakened and elderly normothermia or low-grade fever . The cough is dry or productive with the discharge of clear mucus or purulent mucous sputum.
— An objective examination of the respiratory system shows weakened breathing over the focus and hard breathing over the rest of the surface of the lungs, auscultation distinct moist sonorous fine-bubble rales, as a result of bronchitis — scattered dry ones, and with the addition of pleurisy — pleural friction noise, percussion sound is muffled, tachycardia up to 120 beats\ min., tachypnea up to 30\min., muffled heart sounds.
One of the serious symptoms that should be given due attention is shortness of breath (lack of air). It is especially panicky for children, since it can appear in a state of complete rest or when the child is sleeping. It occurs when alveolar fluid accumulates and disruptions in capillary-alveolar gas exchange occur. Residual symptoms of shortness of breath are an important sign, as they signal further progression and ongoing destruction of lung tissue.
With successful resolution, clinical recovery occurs within up to two weeks, and is X-ray confirmed by the end of the third week of the disease.
Focal pneumonia in children manifests itself 6-7 days after the appearance of another inflammatory process in the body. In children, the symptoms are slightly different: an increase in temperature to 40-42°C, apathy is more pronounced, wheezing and creaking are observed when talking, blueness of the nasolabial triangle, especially during active actions - eating, talking, crying. Only for children, the main symptom is a change in skin texture in the form of retraction of the intercostal spaces inward, as well as the addition of nausea and vomiting.
Signs of focal pneumonia vary depending on the etiopathogenetic agent:
— Staphylococcal lesions are characterized by an acute onset of the disease, pain in the chest and temporal area, hemoptysis due to the destructive properties of the pathogen, confusion of thinking, and irregular fever. The staphylococcal factor is very dangerous in case of potential pyopneumothorax, bleeding from the lung, bacterial pericarditis, amyloidosis and even sepsis.
— Pneumococcal etiology occurs in 47% of cases. It begins with constant hyperthermia, there is a cough with sputum, and chills.
- Gram-negative Friedlander's diplobacillus affects the age group over 30 years old, with obvious alcoholism and poor nutrition. Hyperthermia is observed in combination with significant dyspnea, bluish discoloration of the skin and mucous membranes, cough with mucus with a foul odor. There is a tendency to abscess formation.
— With streptococcal etiology, it is not uncommon to be burdened with pleural empyema or even septic infection. Characterized by attacks of fever with large and sudden changes in temperature, severe sweating, and the release of mucus streaked with blood.
— Viral infection with acute onset and prolonged hyperthermic syndrome for up to 11-12 days, convulsions, nosebleeds, cough and hemoptysis. Complicated by thrombosis and bleeding.
— Focal pneumonia of postoperative origin is very dangerous due to the development of incompetence of the respiratory systems and vascular pathologies, the rapid progression of symptoms due to reduced immunological strength.
Acute focal pneumonia is characterized according to severity, distinguished:
- Light. Minor intoxication is manifested by low-grade fever, normal blood pressure, without disturbances of consciousness.
- Average. Increased temperature, weakness, dyspnea, sweating, decreased blood pressure.
- Heavy. Significant toxic effects, hyperthermia, local cyanosis, tachycardia and respiratory distress.
Stages
- Stage - exudation or flush of inflammation. An increase in the permeability of the walls of the capillaries of the alveoli, due to which serous exudate accumulates in the lumen of the alveoli with a high content of microorganisms.
- Stage - yellow or red hepatization. Lung tissue becomes denser due to the accumulation of large amounts of fibrin in the lumen of the alveoli. Red hepatization – migration of erythrocytes and their accumulation, gray – leukocytes.
- Stage - restoration (permission). Liquefaction and removal of inflammatory exudate through the bronchial tree.
More about the stages of flow
Diagnostics
Laboratory diagnosis of focal pneumonia involves various types of studies. The following are indicators characteristic of the focal form:
- complete blood count: slight neutrophilic leukocytosis;
- shift of the leukocyte formula of neutrophils to the left;
- increased ESR;
- increased content of fibrinogen, C-reactive protein, seromucoid, glycoproteins, globulins;
- mucopurulent discharge containing a large number of neutrophils.
Focal pneumonia on x-ray:
- foci of darkening of a non-homogeneous structure;
- unclear contours of the lesion;
- hydrothorax when the pleura is involved in the inflammatory process.
Biopsy (microscopic specimen “Focal pneumonia”) will show an accumulation of inflammatory exudate with a predominance of cellular elements, depending on the type of infectious pathogen.
Lobar (Pneumococcal) pneumonia.
Clinic. Usually it begins acutely, often after cooling: the patient experiences tremendous chills; body temperature rises to 39-40 °C, less often to 38 or 41 °C; pain when breathing on the side of the affected lung increases with coughing, initially dry, later with “rusty” or purulent viscous sputum mixed with blood. A similar or less violent onset of the disease is possible as a result of an acute respiratory disease or against the background of chronic bronchitis. Objectively. The patient's condition is usually serious. The skin of the face is hyperemic and cyanotic. From the very beginning of the disease, breathing is rapid, shallow, with flaring of the wings of the nose. Before the use of antibacterial therapy, the high temperature persists for an average of a week, decreasing sharply (critically); under the influence of antibacterial drugs, a gradual (lytic) decrease in temperature occurs. The chest lags behind in the act of breathing on the side of the affected lung, percussion of which, depending on the morphological stage of the disease, reveals dull tympanitis (tide stage), shortening (dullness) of the pulmonary sound (red and gray liver stage) and pulmonary sound (resolution stage). Depending on the staged nature of the morphological changes, auscultation reveals respectively increased vesicular breathing and crepitatio indux, bronchial breathing and vesicular or weakened vesicular breathing, against which crepitatio redus is heard. Due to damage to the pleura (parapneumonic serous-fibrinous pleurisy), a pleural friction noise is heard. At the height of the disease, the pulse is rapid, soft, and corresponds to decreased blood pressure. Laboratory examination: neutrophilic leukocytosis, occasionally hyperleukocytosis, is characteristic. The absence of leukocytosis, especially leukopenia, can be a prognostically unfavorable sign. ESR increases. X-ray examination reveals homogeneous shading of the entire affected lobe or part of it, especially on lateral radiographs. Fluoroscopy may not be sufficient in the first hours of illness. An atypical course is more often observed in persons suffering from alcoholism.
Symptoms
In the analysis of the clinical picture, medical history is of great importance. Focal pneumonia has a number of symptoms that appear in almost every patient.
1. Onset of the disease:
- symptoms develop gradually, over 3-4 days, often preceded by acute bronchitis;
- fever - 38-39°C;
- dry cough;
- weakness, decreased performance and other symptoms of intoxication;
- with bilateral pneumonia, symptoms develop faster and more aggressively.
2. The height of the disease:
- fever of the wrong type with lytic decline after 2-7 days;
- pain in the chest is visceral, dull, aching, not intense with involvement of the pleura on the affected side;
- cough with mucopurulent sputum, volume no more than 50-100 ml, odorless;
- shortness of breath of inspiratory or mixed types is a rare symptom;
- symptoms of intoxication;
- diffuse cyanosis (rare), facial hyperemia on the affected side (for left-sided - on the left, for right-sided - on the right);
- rapid breathing;
- lag of half of the chest on the affected side in the act of breathing;
- palpation of the chest: slight increase in vocal tremor over the source of pneumonia on the affected side;
- percussion of the lungs: dull-tympanic or dull sound over the inflammatory focus;
- Auscultation of the lungs: weakened vesicular breathing, sonorous fine rales. Crepitation is rarely detected.
Symptoms of the disease
Clinical manifestations will differ somewhat depending on the location of the pathological focus.
For example, for bilateral focal pneumonia the following will be characteristic:
- a sharp increase in temperature, which is very difficult to get rid of, even with the help of antipyretics;
- severe headaches;
- intense pain and burning in the chest. Such unpleasant symptoms tend to worsen when inhaling;
- increased sweating;
- shortness of breath and dry cough, which is accompanied by sputum as the disease progresses. In such cases, they talk about the development of purulent pneumonia;
- pale or bluish skin;
- appearance of rashes.
Right lower lobe pneumonia has the following symptoms:
- discomfort and pain localized on the right side of the chest;
- cough with sputum, which may contain streaks of pus or blood;
- chills and fever;
- sweating at night.
Changes in pneumonia
Symptoms of left-sided focal pneumonia are presented:
- low-grade fever;
- heaviness and pain in the right side;
- severe cough - may be dry or with sputum production;
- chills and general weakness;
- shortness of breath and sweating.
Any type of pneumonia can be accompanied by the following clinical manifestations:
- decreased performance;
- weakness and weakness;
- the appearance of wheezing when breathing;
- muscle and joint pain;
- decreased or complete lack of appetite;
- heart rate disturbance;
- confusion;
- pathological blush of the facial skin;
- unhealthy shine in the eyes;
- abdominal pain;
- disruption of the bowel movement process, which often results in diarrhea;
- attacks of nausea and vomiting.
The last category of symptoms is most typical for community-acquired focal pneumonia.
All of the above signs can be applied to both adults and children, but it is worth considering that in the latter the disease develops faster and is more severe.
Differences from lobar pneumonia
Nosologies affecting the respiratory tract are similar in their symptoms, but the main difference between focal pneumonia and lobar pneumonia is the mechanism of development:
- Lobar pneumonia is caused by a highly virulent strain of the microorganism and affects the entire lobe of the lung. The symptoms will be more pronounced and rapid compared to focal ones.
- Focal pneumonia - pathogens are less pathogenic. The disease is easier, less likely to lead to complications and is more treatable.
Forms
Since this type of disease most often occurs in children, the doctor must conduct a proper examination and find out the reasons for the development of the disease. It is this information that will make it possible to objectively assess the severity of the disease and choose the right treatment tactics. Modern medicine uses several systems to classify this disease. If we take the localization of the inflammatory process as a criterion, then the following forms are distinguished:
Right-handed
This species is more common than others, which is due to the anatomical features of the structure of the bronchial tree. The right bronchus is slightly wider and shorter, so the infection penetrates faster, and its smaller size is an easier route for infection to reach the right lung.
Clinical manifestations occur in waves, so it is very difficult to detect infection in the alveoli in the early stages.
Very often, when examining such a patient at the initial stage, a doctor can listen for wet and dry wheezing and diagnose bronchitis, but at the same time pneumonia is already developing in the human body.
Right-sided pneumonia can be successfully treated at home, as it responds well to specific therapy.
Left-handed
When the left bronchus is affected, the intoxication of the body is much lower. On examination, left-sided pneumonia may manifest itself as a lag in breathing of the left half from the right during the act of inhalation.
It is extremely difficult to diagnose this species. Left-sided lobar pneumonia may not appear on x-rays, so if suspected, some doctors recommend doing a computed tomography scan.
Double sided
The reason for the development of such an inflammatory process can be a person’s prolonged stay under anesthesia or on artificial ventilation.
Patients with bilateral inflammation experience severe intoxication of the body, they develop severe chest pain and chills.
If a patient is diagnosed with this type of disease, the doctor will immediately hospitalize him in the department for inpatient treatment.
Focal-confluent
This species is characterized by inflammatory processes in several segments of the lung, and there are cases of damage to the entire lobe. Upon examination, the doctor clearly diagnoses the lag of one lung from the other during breathing, cyanosis and shortness of breath appear.
Pathological changes in the lungs are very clearly visible on x-rays: areas with microabscesses and emphysematous changes appear. The symptomatic manifestations of this type are in most cases similar to lobar pneumonia.
Treatment of focal confluent pneumonia requires immediate hospitalization and treatment in a hospital setting.
Catarrhal
With a disease such as bronchitis, inflammatory processes can occur not only in the respiratory system itself, but also cause serious complications. Catarrhal pneumonia is a complication of bronchitis. During such a disease, inflammatory processes from the bronchi gradually move into the lung and affect its individual areas.
At the initial stage of development of this type of disease, the patient experiences:
- slight increase in temperature;
- decreased appetite;
- the appearance of a runny nose and cough with specific mucopurulent discharge;
- tachycardia or minor gastrointestinal problems.
This type requires proper and timely treatment, since if treatment is ignored, acute purulent pneumonia, abscess, and gangrene of the lungs can occur.
Purulent
During this type of disease, destructive processes begin in the lung tissues, which causes pneumosclerosis or bronchiectasis. Purulent focal pneumonia is characterized by the appearance of many purulent formations and lesions in all organs of the respiratory system.
The cause of the development of the disease can even be a foreign body in the bronchi, which closes the lumen in the small bronchus. It is the lack or complete absence of ventilation that causes the formation of an abscess.
The classic symptoms of this type are: high body temperature, acute intoxication of the body, cough, which is accompanied by foul-smelling sputum. The patient experiences a sharp decrease in body weight, and even anorexia is possible.
Further symptoms will depend on how the abscess behaves. If it ruptures, a person may experience a decrease in the manifestations of intoxication, and in a short period of time about 1 liter of fetid, purulent sputum will be released.
After the pus is removed from the lungs and bronchi, the patient develops an appetite. Breathing improves and the body begins to recover.
Right lower lobe
This type belongs to the infectious-allergic type, in which one or more lobes of the lung are affected. This disease affects different generations of patients. With this type, the patient feels a sharp deterioration in the body’s condition, a severe headache appears, the body temperature rises sharply, a wet cough, sweating, shortness of breath and weakness appear.
In most cases, doctors diagnose this disease in the right lobe of the lung in its lower part. All treatment takes place only in a hospital setting, as constant monitoring by a doctor is required. Full recovery occurs after a long period of time, since after the therapeutic course the patient must undergo preventive measures and physical procedures that help to return to the full functioning of the lung.
Basal
Basal form. Doctors call this form the most difficult, since the cause is infection. Pathogenic microorganisms enter the bronchi and actively multiply there. In most cases, the right lung is affected.
Focal hilar pneumonia can occur in two types: tumor-like and inflammatory. The second type is difficult and long. Remissions give way to exacerbations, and during such processes it becomes increasingly difficult to influence the disease itself. When a tumor appears in the lungs, small bumps become noticeable.
The symptoms are classic; the only thing that leads the doctor to suspect hilar pneumonia is a blood test. It clearly shows leukocytosis.
This requires urgent treatment, but the most important thing is the professionalism of the doctor. Unfortunately, this form is very similar in symptoms to lung cancer or tuberculosis. If the doctor fails to correctly diagnose the disease in time, the consequences can be disastrous.
Treatment
The main treatment method for focal pneumonia is antibiotic therapy. The drugs are first prescribed empirically. After bacterial culture, a treatment regimen is based on the identified pathogen. At the beginning, broad-spectrum antibiotics are prescribed to prevent the development of complications. Subsequently, sputum is taken for bacterial culture and the exact type of microorganism and its sensitivity to drugs are determined. The final course is administered with the selected drug. The medicine should also be used several days after the fever disappears.
Expert opinion
Anna Sandalova
Pulmonologist, doctor of the highest category
Ask a Question
Focal pneumonia is the task of highly qualified doctors. For adequate treatment, you should contact a medical facility. In large cities, pneumonia is treated in pulmonology departments.
More about treatment
Treatment of focal pneumonia
When applying treatment tactics, timely selection of treatment and an integrated approach are important. Treatment methods include:
— Antibacterial therapy. First of all, when determining treatment tactics, a test of the sensitivity of pathogenic flora to medications should be performed. And choose the route of administration - orally, intrapleurally, endobronchially, endolymphatically, but injection is considered the most acceptable.
The advantage of modern antibacterial drugs is their broad spectrum of action on microorganisms and at the same time minimal toxicity. These include semisynthetic penicillins, cephalosporin antibiotics, the fluoroquinolone group, and macrolides quite often in combination with cephalosporins. Aminoglycosides and tetracyclines are also applicable, but only if the benefits of use outweigh the risk of side effects.
— Symptomatic therapy includes antipyretics and NSAIDs, antiallergenic, bronchodilators, mucolytics, expectorants. Mucolytic drugs are in the lead because they are indispensable for the evacuation of mucus during a cough. Some mucolytics potentiate the antimicrobial effect. In acute cases, they resort to the use of sulfonamides.
— If a severe course is detected, infusion detoxification and oxygen therapy in a hospital setting, as well as plasmapheresis, are necessary.
— General rules include: rest, high-calorie diet, warm drinks, vitamin therapy.
— Physiotherapeutic methods: the use of modern nebulizers, exercise therapy, electrophoresis, UHF and UHF therapy, positional drainage, vibration massage with special massagers, percussion massage.
— Traditional treatment as an addition to the main therapy. These are herbal infusions and homeopathic supplements, warm foot baths, compresses.
— Surgical treatment for serious complications: cicatricial changes, the presence of purulent exudate with the formation of cavities, collapse of the lung. The operation is also carried out in cases of morphological changes in vital organs due to prolonged exposure to intoxication.
With adequate treatment, focal pneumonia is completely cured and leads to the restoration of lung tissue in 72% of cases, pneumosclerosis develops in 21%, and a decrease in the lobe of the lung in 3%.
Complications
Are divided into:
- Pulmonary:
- abscess or gangrene of the lung;
- inflammation of the pleura;
- bronchial obstruction;
- pulmonary edema;
- acute or chronic respiratory failure.
- Extrapulmonary:
- inflammation of the endocardium or pericardium of the heart;
- meningitis;
- encephalitis;
- systemic inflammatory response syndrome (sepsis).
To prevent the development of severe complications, you should promptly contact the pulmonology department of the hospital. It is more difficult for residents of small towns to find a pulmonologist; most likely, the treatment will be carried out by a therapist who has experience in managing such a pathology.
Prevention
Prevention measures are aimed at eliminating risk factors to prevent the development of the disease:
- avoidance of stressful situations;
- proper balanced nutrition;
- avoiding hypothermia;
- treatment of chronic diseases;
- playing sports;
- timely treatment of acute respiratory diseases.
More about prevention
Clinical guidelines and case histories (download)
| # | File | file size |
| 1 | Community-acquired pneumonia in adults - practical recommendations for diagnosis, treatment and prevention (a manual for doctors). RRO, MACMAH | 715 KB |
| 2 | Diagnostic algorithms and protocols for providing medical care for pneumonia | 3 MB |
| 3 | Clinical protocol. Pneumonia in adults | 458 KB |
| 4 | Disease history. Right-sided focal lower lobe pneumonia. DN - II Art. Acute bronchitis | 143 KB |
| 5 | Disease history. Focal pneumonia of the lower lobe of the right lung. Moderate weight. D.N. - 1st | 88 KB |
| 6 | Disease history. Acute focal confluent upper lobe pneumonia | 68 KB |
| 7 | Disease history. Bilateral focal pneumonia, acute, severe | 130 KB |