Causes of the disease
The nerve, which runs in a canal made of hard tissue, is reliably protected from external influences. But at the same time, it can suffer from deformations of the canal, the walls of which surround it. Deformations are caused by overstrain of ligaments and tendons, causing a temporary deterioration in the blood supply to the tissues and a deficiency of nutrients in them. With constant loads on this area, the changes are consolidated and become permanent: the tissues of the tunnel thicken, loosen or swell. As a result, there is no free space left in the tunnel and the pressure on the nerve trunk increases, after which disturbances in its functions begin to develop - the conduction of motor signals.
Much less commonly, tunnel syndrome can be caused by swelling of the nerve itself. This condition can develop due to general intoxication of the body with salts of heavy metals, derivatives of arsenic and mercury and other toxic substances. The prolonged course of someone's disease requiring the use of antibiotics, diuretics and vasodilators can also lead to the development of tunnel neuropathy.
Risk factors
Carpal tunnel syndrome usually develops in areas exposed to constant or regular stress in the form of monotonous, repetitive movements. But besides mechanical irritation of the nerve and surrounding tissues, other factors can lead to the disease.
The risk group for carpal tunnel syndrome includes the following categories of the population:
- people whose professional or everyday activities include the same type of flexion-extension movements (hairdressers, typists, tennis players, sign language interpreters, musicians - most often violinists, guitarists, painters, etc.);
- people over 50 years of age (age-related changes that occur throughout the body invariably affect bone tissue);
- people suffering from endocrine diseases (diabetes mellitus, dysfunction of the thyroid gland, pituitary gland), which significantly impair the ability of tissues to recover;
- people who have a family history of musculoskeletal diseases or suffer from these diseases (arthritis, osteochondrosis, etc.);
- people who are often exposed to microtrauma of joints and ligaments (loaders, bodybuilders, masons, etc.);
- people with autoimmune diseases (systemic lupus erythematosus, HIV, etc.)
Causes
The main reason why carpal tunnel syndrome develops is an increase in the volume of synovial membranes that surround the tendons and put pressure on the median nerve.
The synovial membranes are capable of producing a secretion necessary to reduce friction between the walls of the tendons, which facilitates their work.
All predisposing factors that can provoke the development of carpal tunnel syndrome can be divided into two categories:
Direct – this includes all the prerequisites that directly affect the pinched nerve:
- uncontrolled increase in body weight, which promotes growth and increase in the volume of muscles and tendons;
- hormonal diseases;
- acromegaly is a pathology of the anterior pituitary gland, in which there is uncontrolled growth of bone tissue, which is accompanied by thickening and widening of the hands;
- hereditary predisposition;
- age after 55 years;
- fluid retention in the body, in which all the water that enters the body is not excreted by the kidneys, but accumulates in the tissues, causing edema;
- neoplasms (cysts) in the wrist area, which rapidly increase in size and put pressure on the nerve;
- rheumatoid arthritis, arthrosis, chronic inflammatory processes in muscles and tendons;
- Tenosynovitis is a disease in which the inflammatory process affects the tendons, causing them to become swollen and loose.
Indirect - this group includes those factors that can accelerate the development of the disease, as well as aggravate its course, when a person has chronic diseases.
These include the following common risk factors for developing the disease:
- the presence of bad habits, especially chronic alcoholism;
- frequent injuries to the wrist area (fractures, tendon ruptures, pinching);
- long-term mechanical work with the hands: computer layout, work at the machine, playing musical keyboards, embroidery and cutting clothes.
The risk group includes people over the age of 45, when, against the background of hormonal changes, weight may increase sharply, and systemic diseases such as arthritis, arthrosis, and gout may develop.
Types of tunnel syndrome
Carpal tunnel syndrome is the most common type of tunnel neuropathy and is very often mistaken for the only form of the disease.
But this condition can develop when the following nerve trunks are infringed:
- suprascapular nerve - suprascapular notch syndrome (most often found in track and field athletes involved in shot throwing and javelin, in tennis players, volleyball players - the syndrome develops on the “working” side of the body);
- ulnar nerve;
- median palmar nerve;
- radial nerve;
- median carpal nerve;
- peroneal nerve;
- tibial nerve;
- digital plantar nerve.
Compression of any of the listed nerves falls into the category of tunnel syndromes and has similar symptoms.
General information
The disease is caused by irritation or damage to the median nerve of the hand when high pressure is constantly applied to it in the wrist area.
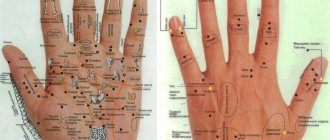
Each arm is equipped with three nerves that are responsible for both movement (motor fibers) and sensations and sensitivity in the area (sensory fibers). The median nerve provides movement and sensation to the inside of the hand and the muscles that move the thumb.
Carpal Tunnel Syndrome
The median nerve runs from the shoulder and forearm to the hand. On the inside of the wrist it passes through what is called the carpal tunnel. This passage is formed by the carpal bones and the stabilizing ligament. In addition to the nerve, the finger flexor tendons also pass through the carpal tunnel.
Carpal tunnel syndrome occurs in various forms. In mild cases, only mild discomfort is noted; in severe cases, permanent paralysis may develop.
Some people seem to be “destined” for carpal tunnel syndrome because they have a narrow carpal tunnel that is anatomically conditioned from birth. If the same movement is carried out for a long time or strains the wrist during work, carpal tunnel syndrome develops quickly. Another possible cause is compression of the nerve as a result of inflammation and swelling of the tendons, which also lie in the carpal tunnel.
Disease frequency
Carpal tunnel syndrome can develop in anyone and is usually bilateral. Doctors believe that up to ten percent of the population exhibits symptoms, but not all cases require treatment.
Every year, three in 1,000 people are newly diagnosed with carpal tunnel syndrome. Women are three times more likely to be affected than men. Carpal tunnel syndrome usually first occurs between the ages of 40 and 70. It is rare in children.
Symptoms
Compression of the nerve trunk develops gradually and the intensity of symptoms increases at the same pace. In the initial stage, the syndrome practically does not manifest itself: a person may only experience a feeling of discomfort with prolonged stress on the area of the body in which the nerve is pinched. As the canal narrows, more and more significant dysfunctions of the nerve occur, which are manifested by the following symptoms:
- pain in the affected area, increasing after physical activity;
- pain may occur at rest (most often at night);
- in the peripheral part of the body (the one that is located further than the point of pinching of the nerve), numbness and tingling are felt;
- When you try to “stretch” the affected joint or ligament or when you tap this area, the pain intensifies.
- If the tunnel is significantly narrowed, the listed symptoms are joined by more pronounced ones:
- stiffness of the affected joint;
- deterioration of muscle tone in the area of nerve compression;
- with simultaneous tension of symmetrical muscles (for example, when clenching both palms into fists), the muscles on the affected limb are less pronounced, which indicates their atrophy.
One of the distinctive signs of tunnel neuropathy is that when a nerve is pinched in a large joint (scapula, elbow, thigh), pain can manifest itself at a considerable distance from the affected area, which makes diagnosis difficult. For example, if you have shoulder pain accompanied by numbness in the shoulder, forearm, or upper back, the nerve may be compressed in both the elbow joint and the scapula.
Symptomatic picture
The pathological process is characterized by the presence of pain and tingling on the plantar surface for several months or years. At the initial stages of the pathology, patients complain of pain on the sole while walking, and then it arises spontaneously at night. The pain syndrome spreads from the foot to the buttock along the posterior plane of the lower limb, intensifying during extension of the foot. After some time (years), weakness occurs in the phalanges of the foot. Approximately 60% of patients complain of a burning sensation, numbness and tingling in the foot. Symptoms increase or decrease over the years, exacerbation occurs during the period of wearing uncomfortable shoes.
An objective examination of the patient reveals pain during palpation and percussion of the nerve at the tarsal canal, radiating pain and numbness to the foot (95-95%), pain when palpating along the sciatic nerve from the foot to the buttock (1/2 cases), plantar hypoesthesia planes (60%), hypotonia of the plantar arch supports of the foot and toes (70%), hypotrophic phenomena of the muscle fibers of the foot (65%); difficulty or general inability to walk “on tiptoe” (95%). Paresthesias in the foot are observed (63%).
Tinel and Phalen symptoms are observed in 2/3 of cases. Weakness of the plantar arch supports of the foot and toes
Complications
Most often, tunnel neuropathy becomes a chronic state, when exacerbations of the disease alternate with periods of remission (asymptomatic course of the disease).
The good news for people suffering from carpal tunnel syndrome is that the pathology rarely extends beyond the affected area and the worst that can happen is an increase in symptoms and pain.
Therefore, this condition is not life-threatening. But it can greatly disrupt its quality. The pain, which becomes longer and stronger over time, can cause disturbances in sleep, appetite, extreme irritability and ultimately lead to other diseases of the nervous system, such as chronic insomnia, anorexia, bulimia, etc.
Diagnostics
with constant loads on this area, the changes are fixed and become permanent
First of all, the doctor examining the patient excludes other diseases that have symptoms similar to the clinical picture of tunnel neuropathy. Among such diseases are arthritis, arthrosis, neuralgia, myalgia, etc.
After this, to clarify the diagnosis, neurological tests are used to identify damage in the nerve trunk. The most commonly used test is called the Tinel sign, in which the doctor taps the skin over the canal that contains the damaged nerve. With carpal tunnel syndrome, the patient feels numbness, tingling, and pinpoint itching (the so-called “crawling sensation”). If the syndrome has developed in an area inaccessible to the Tinel test, electromyography may be prescribed, which examines the ability of the nerve to conduct impulses.
Examinations and diagnostics
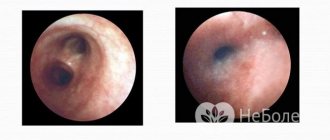
ENMG examination for carpal tunnel syndrome
First of all, the doctor examines the muscles and arteries, checking whether muscle atrophy has occurred. In the case of atrophied thumb muscle, the affected person can no longer move the thumb. As a rule, the test is to ask the doctor to hold a bottle in his hand. Depending on the stage of muscle atrophy, this is either barely possible or not possible at all (positive bottle test).
Sensitivity is checked by the doctor by patting the patient's palm. If the patient does not perceive this touch, the sensitivity of the surface is impaired.
The sense of touch and fine motor skills of the fingers are tested by the patient's ability to pick up coins or paper clips. If this fails, then the sense of touch is impaired.
If the doctor is not yet sure of the diagnosis, he performs provocative tests:
- Hoffman-Tinel test: tapping (percussion) along the median nerve causes pain and discomfort in the patient.
- Phalen's test: This test requires the patient to place their hands with their palms behind their back, which will make the wrists more arched. If the pain intensifies, this is a positive Phalen's sign and also an indicator of carpal tunnel syndrome.
Neurological instrumental testing
You can be absolutely sure that carpal tunnel syndrome is present only after a neurological examination. Electroneuromyography (ENMG) measures how the median nerve conducts received impulses and transmits them to muscles. During the examination, electrodes are placed on the skin, and the conduction velocity of the median nerve is compared with that of another healthy nerve. The examination is usually painless.
We recommend
We recommend reading the article about yoga for treating joints. How yoga helps in the recovery process for arthritis, what program for exercise it is advisable to choose, how exercises help relieve pain, you can learn more in this article.
Additional Research
To rule out other conditions with similar symptoms (differential diagnosis), the doctor will often examine the area of the elbow, neck, and shoulder, where the nerve may also be narrowed:
- Ultrasound examination (sonography) of the soft tissues of the hand and forearm determines how far the carpal tunnel is laid.
- X-rays are used to check whether changes in the bones and joints of the wrist are responsible for the compression.
- Magnetic resonance imaging (MRI) is done if the doctor suspects that a tumor may be causing the symptoms.
Treatment
Treatment of tunnel neuropathy is aimed at relieving the inflammatory process and eliminating swelling in the affected area, relieving the patient of pain and preventing more severe nerve entrapment.
Drug treatment
Among medications, the following groups have confirmed their effectiveness:
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as Ibuprofen, Ketorolac, Indomethacin, Nimesulide, etc., in addition to relieving inflammation, provide an analgesic effect;
- hormonal drugs (Hydrocortisone, Prednisolone) are introduced into the affected area by injection and/or applied to this area in the form of an ointment;
- calcium chloride is injected intravenously to relieve inflammation and stabilize the immune system response;
- vitamin preparations are prescribed to improve the conduction of nerve signals and normalize blood circulation in the area of nerve compression.
Physiotherapy
When treating tunnel neuropathy, a course of thermal physiotherapeutic procedures is recommended, using anti-inflammatory and hormonal drugs (electrophoresis, phonophoresis) and reflexology, which normalizes the functions of the nervous system.
Physical therapy is prescribed on an individual basis, depending on the results of the examination and the degree of compression of the nerve - in some cases, with tunnel neuropathy, it is recommended to exclude any stress on the affected joint.
Surgery
In cases where conservative treatment of carpal tunnel syndrome is ineffective, the doctor may recommend surgical treatment. During the operation, which is performed under general anesthesia and lasts about an hour, the surgeon excises the thickening in the tissue that is compressing the nerve, which allows its function to be restored.
The disadvantages of this treatment method include the fact that it is impossible to predict in advance how effective the operation will be. In a small percentage of cases (about 2-3%), patients experience an increase in symptoms after surgery.
Neurological complications of diabetes mellitus: carpal tunnel syndrome
Diabetes mellitus (DM) ranks seventh in the world among the causes of decreased quality of life, in particular due to neurological complications. In diabetes, tunnel (compression) neuropathies are widespread, mainly carpal tunnel syndrome (CTS). Today, the double damage model is recognized as the basis of its pathogenesis. Based on the clinical manifestations, three stages of CTS are distinguished. In the early stages, characteristic night pain and tingling are noted, localized mainly in the distal parts of the hand and the zone of innervation of the median nerve. Later, stiffness and awkwardness in the hand during the daytime appear. With a long course - atrophy of the thenar muscles. The diagnosis of CTS is made based on clinical manifestations. However, tests and electroneuromyography may be used. The latter allows you to determine the type of neuropathy (axonal or demyelinating), the severity of the process and exclude other causes of nerve damage. Therapy for CTS in diabetes involves the use of non-drug, drug and surgical methods, depending on the stage of the disease and the severity of symptoms. The simplest non-drug treatment methods are considered to be immobilization of the hand and changing the motor pattern. Pharmacotherapy involves the prescription of non-steroidal anti-inflammatory drugs, anticonvulsants and antidepressants, B vitamins and alpha-lipoic acid. If there is no effect, surgical intervention is indicated.
Pathogenesis of CTS in diabetes (double damage model)
Clinical stages of CTS
Introduction
Diabetes mellitus (DM) ranks seventh among the causes of decreased quality of life, including due to neurological complications [1]. The most common is diabetic neuropathy (DN). According to some data, it occurs with a frequency of up to 50% [2]. In the large EURODIAB study, diabetic neuropathy was observed in 28% of patients with diabetes [3]. Considering that there are about 415 million patients with diabetes in the world, about 140 million suffer from DN [4].
In 2011, the Toronto Expert Panel on Diabetic Neuropathy presented an updated classification, as well as diagnostic criteria and assessment of disease severity [1, 5]. According to this classification, generalized and focal/multifocal forms of DN are distinguished. The first includes typical distal sensorimotor and atypical sensory (acute, painful) neuropathies, the second includes multiple mononeuropathies, cranial neuropathies, tunnel neuropathies and thoracolumbar radiculopathy. Moreover, 80% of cases account for chronic distal symmetric sensory and sensorimotor polyneuropathy [6].
Among focal/multifocal neuropathies, the most common are tunnel (compression) neuropathies, predominantly carpal tunnel syndrome (CTS), or carpal tunnel syndrome.
The cause of CTS is compression and stretching of the median nerve in the osteofibrous canal. The nerve is located between the transverse ligament and the bones of the wrist.
The disease can develop at any stage of diabetes and is often asymptomatic.
Epidemiology
The incidence of CTS in the general population ranges from 3 to 5%, and the lifetime risk of developing it can reach 10% [7].
Among patients with diabetes, the prevalence of clinically manifest CTS, especially asymptomatic CTS, is higher. In the Rochester study, this was detected in 11 and 6% of patients with type 1 and type 2 diabetes, respectively [8]. In the long-term observational Fremantle study involving 1284 patients with diabetes, the incidence of CTS was 5.5 cases per 1000 patients per year, which is 4.2 times higher than in the general population [9]. Apparently, there is also an inverse relationship, since a number of prospective studies in patients with CTS have documented a twofold increase in the risk of developing diabetes, and 80% of patients have at least insulin resistance [10, 11].
The prevalence of CTS among patients with diabetes varies depending on the age, sex of the population, geography of the study, diagnostic criteria, and the presence of risk factors for the development of the pathology in the subjects.
B. Perkins et al. found that CTS is caused by symmetrical distal sensorimotor or sensory polyneuropathy. Thus, pathology was diagnosed in 14% of patients with diabetes without polyneuropathy and 30% of patients with diabetes with polyneuropathy [12].
A higher lifetime risk of developing CTS has been reported in people with type 1 diabetes; after 54 years of illness, it increases to 85% [13].
In patients with newly diagnosed diabetes, pathology was detected in 28% of cases, with a long course of the disease (on average 14.5 years) – in 63% [14, 15]. These data suggested that the risk of developing CTS is more related to the duration of diabetes rather than to the age of the patients.
Carpal tunnel syndrome in diabetes, as in the general population, is more common in women. In a study involving 146 patients with diabetes, the disease was observed in 39% of cases: in women – in 46%, in men – in 28% [16].
Pathogenesis
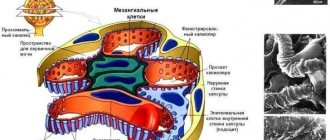
Currently, the double damage model is considered to be the basis of the pathogenesis of CTS in diabetes (Figure) [17, 18]. Due to hyperglycemia, peripheral nerves are affected and become more susceptible to secondary damage from local compressive factors such as pressure, strain and/or stretch [19].
Damage to peripheral nerves and a slowdown in reparative processes in nerve fibers in diabetes are associated not only with hyperglycemia, but also with a lack of insulin and C-peptide. These disorders lead to a cascade of metabolic and vascular changes.
One of the main mechanisms of damage to the nervous system is considered to be activation of the polyol pathway for glucose utilization. As a result, sorbitol and fructose accumulate in the nervous tissue, protein kinase C is activated, myo-inositol is depleted, and Na+-K+-ATPases are inhibited. The consequence is intraneuronal Na+ accumulation, fluid retention, myelin sheath swelling, reduction in the number of axonal glial cells, and ultimately peripheral nerve degeneration.
A significant role is played by oxidative stress, which produces free radicals that contribute to endoneurial hypoxia.
Factors such as endothelial dysfunction, damage to small arteries, and genetic predisposition may be involved [20].
The endoneural, perineural metabolic and vascular disorders described above lead to functional and structural changes in peripheral nerves, which increases the likelihood of compression in anatomically narrow canals. It has been proven that when the hand is flexed/extended at the wrist, the pressure in the carpal tunnel increases eight to ten times and the nerve is stretched, which causes a decrease in intraneural microcirculation, damage to the myelin sheath, impaired axonal function, as well as dysplasia of connective tissue structures [18].
Clinical picture
In the early stages of the disease, pain and unpleasant sensory symptoms may occur - tingling in the hand. Pain and numbness are most often localized in the distal parts of the hand, the zone of innervation of the median nerve (the area of the thumb, index and middle fingers, as well as on the radial surface of the ring finger). These symptoms usually appear at night.
During the daytime, patients complain of awkwardness in the hand when performing movements that require flexion at the wrist [21]. To reduce numbness and awkwardness, patients simply need to shake the hand (shaking or clicking symptom) [22].
In CTS, the dominant hand is usually affected, but bilateral involvement is also possible [16].
In case of damage to the autonomic fibers that make up the median nerve, autonomic-trophic disorders are noted: changes in hand temperature, sensitivity to cold, and sweating disorder [23].
Depending on the presence of certain symptoms, three stages of CTS are distinguished (table) [21].
In most patients, symptoms are localized not only in the zone of innervation of the median nerve, but also in the zone of innervation of the ulnar nerve, as well as in the area of the hand, forearm, elbow, shoulder and neck [24].
Some patients experience an atypical course - for example, writer's cramp or weakness and pain in the shoulder, or forearm, or middle finger [21].
However, CTS in diabetes is often asymptomatic and is detected only during electroneuromyography. During screening, pathology is detected in 30–36% of people with newly diagnosed diabetes. This fact confirms that damage to the proximal nerve segment and/or sensory fibers in DN may reduce the likelihood of developing clinically significant CTS [25].
Pain syndrome
Pain syndrome with any etiology of CTS is observed in 52–85% of cases [26, 27]. At the same time, paresthesia can also be painful. It has been established that paresthesia and pain in CTS occur with the same frequency – 88.4 and 84.5% of cases, respectively [27].
In CTS, the intensity of pain does not depend on the severity of electrophysiological changes, gender, age and duration of the disease. It is associated mainly with the patient's misconception of pain, depression, and the presence of several additional sources of pain [28]. When CTS is combined with a painful form of diabetic polyneuropathy (DPN), the pain intensity may increase.
Despite the signs of neuropathic pain often described in the literature (allodynia, hyperpathy, electric shock-type shooting), data on the frequency of its occurrence in CTS are contradictory.
M. Sonohata et al. Using the Pain DETECT questionnaire, a reliable neuropathic component of pain was found only in 10.5% of patients with CTS, a probable one – in 20.3%. Moreover, a positive test result was associated with the paroxysmal nature of pain at night [29].
In another study (all participants complained of nocturnal pain), a neuropathic component was observed in 92% of patients with pain, which seems more likely [30].
However, pain in CTS is caused not only by a neuropathic, but also by a nociceptive component. Biopsies of patients with symptomatic CTS have revealed increased expression of prostaglandin E2 and vascular endothelial growth factor, leading to vascular proliferation and fibrosis with the formation of scar tissue around the median nerve and, as a result, its compression. At the same time, tenosynovitis and inflammation of the synovial tissue of the flexor tendons progress. This leads to increased pressure in the carpal tunnel [31].
Diagnostics
Diagnosis of CTS is based on clinical manifestations.
In the absence of pronounced sensory and motor phenomena, great importance is given to collecting an anamnesis. It is necessary to establish the time of onset of symptoms (night paresthesia), provoking factors (hand position, repetitive movements), occupational hazards (use of vibrating tools in work), factors that alleviate symptoms (shaking the hand, changing its position), the presence of descending or ascending irradiation of pain [ 32].
The following tools are used to verify the diagnosis [33]:
Tinel test. Tapping the wrist with a neurological hammer from the side of the palm at the site of the median nerve causes tingling in the fingers. The sensitivity of this test ranges from 26 to 79%, specificity - from 40 to 100%;
Phalen test. Flexion/extension of the wrist 90 degrees (with the elbow straight) for 60 seconds or less leads to numbness and paresthesia in the area of the median nerve innervation. The test allows you to confirm the diagnosis in 67–83% of cases, its specificity varies from 47 to 100%;
Paley and McMurphy test. It is considered positive if pressure at the point of projection of the median nerve (1–2 cm proximal to the flexure of the wrist) leads to the appearance or intensification of pain and paresthesia. The sensitivity of the test is 89%, specificity is 45%.
A cross-validation of the sensitivity of symptoms and tests demonstrated the greatest diagnostic significance of nocturnal acroparesthesia (96%) and the Paley and McMurphy test (89%).
The accuracy of the diagnosis increases (0.86) if a positive response is obtained from three tests and nocturnal acroparesthesia is noted.
If the results of three tests are negative, there is no acroparesthesia, the probability of CTS is extremely low (0.0068) [33].
To determine the severity of the syndrome and the functional impairments caused by it, the Boston Carpal Tunnel Questionnaire (BCTQ) was developed [34]. The results obtained using the questionnaire correlate not only with respect to the clinical picture, but also with respect to electrophysiological changes. To date, the Boston Questionnaire has been recognized as a reliable and sensitive tool for standardizing the severity of the process and assessing treatment outcomes.
A number of publications have demonstrated the validity of this diagnostic method in patients with CTS associated with diabetes and concomitant DPN [35].
Differential diagnosis of CTS is carried out with arthritis of the carpometacarpal joint of the thumb, cervical radiculopathy (especially the C6 and C7 roots), brachial plexopathy, DPN, neuropathy of the proximal median nerve, etc. [21].
Electrophysiological methods for studying the conductive function of the nerve are the basis for the diagnosis of compression neuropathies, in particular CTS [36]. Assessment of the conductive function of the motor and sensory fibers of the median nerve allows us to confirm compressive neuropathy, a sign of which is local changes in the conductivity of the affected nerve in anatomically narrow canals.
It is believed that sensory response parameters are more significant for diagnosing CTS. Sensory fibers of the median nerve have a large proportion of thick myelinated fibers with high energy demands, making them more susceptible to ischemic and metabolic damage. Electroneuromyography also helps determine the type of neuropathy (axonal or demyelinating), the severity of the process and exclude other pathologies.
Features of electrodiagnostics of CTS are described in the monograph of the American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) [36, 37].
Thus, in patients with diabetes and CTS, in contrast to the general population of patients with CTS, in order to avoid a false positive result, it is not recommended to compare the amplitudes and latencies of the median nerve responses with the average population norms, since a number of factors (age, gender, thumb diameter, systemic diseases, obesity and etc.) may affect the accuracy of the study. It is more correct to compare the indicators obtained from the same patient in different areas of the median nerve, for example, in the carpal tunnel area and in the intact area of the median nerve.
In patients with diabetes, when CTS and DPN are suspected, comparative studies of the median, ulnar and radial nerves are mandatory [36, 37].
Recently, ultrasound methods for studying peripheral nerves have been widely used. They have a number of advantages: non-invasiveness, absence of contraindications, reduction of treatment time, etc. [38]. The main signs of tunnel neuropathy on ultrasound examination are local thickening of the nerve and an increase in cross-sectional area in the proximal direction from the location of the compression. The diagnostic value and specificity of ultrasound examination exceed 85% [39]. Less common signs of the disease are a hypoechoic structure, flattening of the nerve at the site of compression, an increase in the number of single or multiple fascicles, and increased vascularization of the nerve [39].
Magnetic resonance imaging can exclude rare causes of CTS, such as hemangioma, osteomyelitis and bone deformation, Charcot arthropathy.
Recently, magnetic resonance tractography has been introduced to assess the severity of morphological changes and inflammation. However, its availability is still limited [40].
Treatment and prevention
Treatment of CTS involves the use of non-drug, drug and surgical methods, depending on the stage of the disease and the severity of symptoms. Unfortunately, we have to admit that patients seek help already at an advanced stage of the disease, most often with a complaint of pain or atrophy of the thenar muscles.
Among non-drug methods, the first place is changing motor stereotypes (avoiding hand movements and lifting heavy objects). Educational programs are conducted to help patients. Immobilization of the damaged area is also indicated, which allows stopping or limiting physical impact and reducing swelling. Splints, orthoses, braces, and splints for the wrist joint help to achieve immobilization in the area of injury. However, despite the presence of randomized controlled trials (RCTs) with splinting for up to eight weeks, the level of evidence for this method is considered moderate.
The possibilities of laser therapy, transcutaneous electrical neurostimulation, phonophoresis with glucocorticosteroids, acupuncture, and therapeutic exercises are also discussed [27].
Drug therapy involves influencing various components of the pain syndrome: nociceptive, neuropathic and, in some cases, dysfunctional. Nonsteroidal anti-inflammatory drugs (NSAIDs) are indicated to influence the nociceptive component of pain, as well as to reduce inflammation. However, this group of drugs for CTS, widely studied in other nosologies, has not been sufficiently studied from the standpoint of evidence-based medicine [27].
In this regard, it is of interest to study the effectiveness of the drug meloxicam. In patients with CTS, the drug was used for ten days. During the therapy, the intensity of pain decreased, as well as the level of substance P, one of the main mediators of pain. At the same time, a decrease was noted in the synovial sheath of the tendons (paraneural), but not in the adventitia of the median nerve, which confirms the selectivity of the drug’s action in relation to the nociceptive component of pain [41].
To date, a number of bioequivalent analogues of meloxicam have been registered, including the Russian drug Artrosan, which is produced in injectable and tablet forms.
When choosing NSAIDs, it is necessary to take into account the risk of gastrointestinal and cardiovascular complications and take measures to reduce them [42].
If a neuropathic component of pain is detected, it is also advisable to prescribe anticonvulsants (gabapentin (Convalis), pregabalin), antidepressants (venlafaxine, duloxetine, amitriptyline) [43].
The use of these drugs would be justified to relieve pain in both DPN and CTS. However, if in the painful form of DPN the use of these drugs has a high level of evidence, then in CTS only gabapentin has been studied. Gabapentin has demonstrated effectiveness in relieving pain in CTS at both low (300–600 mg/day) and medium therapeutic (1800 mg/day) doses. The follow-up period ranged from two to six months [44–47].
When prescribing gabapentin, a dose titration schedule should be followed and the possibility of transient side effects, such as dizziness and drowsiness, should be taken into account.
In Russia, in addition to the original gabapentin, its analogues are registered, for example the drug Convalis. In a Russian study, the latter confirmed its effectiveness in patients with DPN [48].
Alpha lipoic acid (Octolipen) and B vitamins (Combilipen) should be considered as additional treatment methods for CTS that has developed against the background of DPN.
In DPN, the administration of alpha-lipoic acid is recognized as pathogenetically justified due to the drug’s ability to bind free radicals and thus prevent neurovascular disorders [49].
The results of a meta-analysis of RCTs using alpha-lipoic acid 300–600 mg intravenously for two to four weeks in patients with DPN indicate that such therapy not only reduces pain, but also increases the speed of nerve conduction [50].
Considering the peculiarities of the pathogenesis of CTS against the background of diabetes and the functional and structural changes in nerves described above, the use of alpha-lipoic acid (Octolipen) in such patients is justified.
In addition, one RCT demonstrated greater effectiveness of the combination of gabapentin and alpha-lipoic acid compared with placebo and monotherapy with these drugs in relieving neuropathic pain [51].
Another RCT compared the effects of a combination of gabapentin + B vitamins and pregabalin in patients with painful DPN. After 12 weeks of treatment, a 30% reduction in pain was achieved with 900 mg gabapentin plus 100 mg vitamin B1/20 mg vitamin B12 and 300 mg pregabalin. It was concluded that the combination of gabapentin with B vitamins allows for reduced doses of gabapentin, which in turn improves tolerability and adherence to therapy [52].
When targeting the nociceptive component of pain, it is important to consider the synergism of B vitamins and NSAIDs. It has been established that in some cases this combination allows one to achieve a better analgesic effect than NSAID monotherapy; in others, the effectiveness of the combination and monotherapy is comparable, however, when using the combination, a lower dose of NSAID is required, which increases the safety of treatment [53, 54].
Among the invasive treatments for CTS, the most studied are injections of glucocorticosteroids into the carpal tunnel area. In terms of pain relief and symptom reduction, their effect is superior to placebo, local anesthetics and NSAIDs.
Using the palmar approach is more effective than inserting a needle into the wrist, and ultrasound-guided procedures ensure precision.
One RCT demonstrated the effectiveness of local injections of lidocaine [27].
In the absence of a significant effect from conservative treatment, surgical treatment is indicated. Surgical treatment of CTS involves decompressing the median nerve by cutting the transverse carpal ligament. The operation can be open access (both extensive and minimal) or endoscopic. These two approaches do not differ significantly in terms of reducing the severity of clinical manifestations and improving the functional state of the hand. However, a recent study demonstrated the advantage of the latter [55].
Data on the effectiveness of surgical decompression for CTS due to diabetes and idiopathic CTS are contradictory. A number of long-term prospective observations have noted that the long-term effect of surgical intervention in patients with CTS and diabetes is somewhat lower than in the general population [56]. Other studies found no differences between groups in long-term treatment outcomes [57].
Prevention of CTS in diabetes lies primarily in the control of body weight and glycemia. The patient also needs to properly organize his workplace if his professional activity involves increased stress on the wrist (working at a computer, repetitive movements, etc.) [21, 27].
Conclusion
CTS, which developed as a result of diabetes, especially with a long course and the presence of DPN, is quite common. Therefore, the doctor is required to be wary of this pathology and prescribe additional diagnostic tests to detect it at an early stage. This will allow us to limit ourselves to conservative treatment methods.
Lifestyle correction
Many people prefer a “convenient” treatment option, in which the doctor prescribes effective medications or procedures without requiring any action from the patient. Unfortunately, tunnel neuropathy requires the active participation of the patient in the treatment process.
The main condition for recovery or achieving long-term remission is the elimination of stereotypic movements that led to compression of the nerve. Often this becomes the only effective measure that alleviates the symptoms of carpal tunnel syndrome.
Try to perform normal activities with your healthy hand if you have a pinched nerve in the elbow, wrist, or shoulder. If this is not possible, minimize the load on your sore hand: perform only the most necessary actions with it, shifting the bulk of the work to your healthy one.
Get into the habit of sleeping on the side opposite your sore arm, leg, or shoulder blade. This will allow the affected area to “rest” during your night’s sleep and thus compensate for daytime stress.