Ulcerative colitis is the cause of frequent trips to the toilet, chronic appetite and sleep disturbances, and acute pain in the abdominal area. The sooner chronic ulcerative colitis can be recognized, the better the prognosis for treatment. In most cases, complete remission can be achieved.
Nonspecific ulcerative colitis (also known as UC) is a diffuse inflammatory process that is localized in the mucous tissues of the rectum. Acute periods of painful inflammation are followed by remission, which under favorable conditions will last for many years. According to general features - symptoms, leading therapeutic methods and leading methods of prevention - the disease is similar to other chronic lesions of the intestinal tract. The difference is in the area: with ulcerative colitis, the damaged area is limited to the large intestine.
Ulcerative colitis can manifest itself as the body's response to a stressful situation, unfavorable environmental conditions, unhealthy diet, lack of sleep and regular overload. The impetus for the first manifestation of inflammation can be an acute bacterial or viral infection. Most often, colitis is diagnosed in people with a genetic predisposition between the ages of 20 and 40 years. With timely detection of the inflammatory process, the prognosis is favorable for most patients. Life-threatening cases arise when damage to the rectum develops at an accelerated pace. Against the background of intense pain and tissue destruction, malignant tumors appear with an unfavorable prognosis.
What is ulcerative colitis
Currently, the disease remains poorly understood. Because the main cause remains unclear.
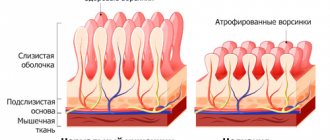
Ulcerative colitis is a nonspecific process in the large intestine, which is manifested by inflammation and necrosis of the mucous membrane. The lesion extends from the anus in a proximal direction. Most often, changes are recorded in the sigmoid region and rectum.
The disease has a chronic course with periodic relapses. Therefore, treating ulcerative colitis is quite difficult. Often the disease is combined with other pathologies of the digestive tract. Symptoms may differ from the typical clinical picture, which requires careful differential diagnosis.
Surgical treatment and preventive measures
For ulcerative colitis of the intestine, the symptoms and treatment are determined by the doctor. This could be a colonoproctologist, therapist or gastroenterologist. Indications for radical treatment are:
- large blood loss (100 ml or more per day);
- perforation of the intestinal wall;
- abscess formation;
- intestinal obstruction;
- megacolon formation;
- fistulas;
- malignancy.
The most common procedure is a colectomy (removal of the large intestine). Sometimes only a small area is cleaned. After resection, an ileorectal anastomosis is performed. The ileum is connected to the anus. A proctocolectomy is often performed. Experienced doctors know not only the symptoms and treatment of ulcerative colitis in adults, but also preventive measures.
In order to reduce the risk of developing this pathology, you need to give up alcohol, quit smoking, eat right, and treat other diseases of the digestive system. There is no specific prevention. With the development of ulcerative colitis, the frequency of exacerbations can be reduced. To do this, you need to take medications prescribed by your doctor, change your lifestyle and follow a diet.
Herbal treatment should only be carried out with the consent of a doctor. Thus, ulcerative colitis is a chronic disease. It is difficult to treat and can lead to serious consequences if left untreated. One of them is the development of colorectal cancer. This occurs due to malignancy of ulcers.
Causes
Experts recognize the multivariate nature of the disease. In most cases, ulcerative colitis in adults develops due to a combination of several etiological and pathogenetic factors. The main reason is called hereditary predisposition. But not all patients with genetic markers of UC develop symptoms of the disease during their lifetime.
Risk factors include:
- intestinal infections (bacterial and viral);
- allergic processes;
- autoimmune pathology;
- taking oral contraceptives for a long period of time;
- smoking;
- changes in the nature of nutrition, including following certain types of diets;
- psycho-emotional stress, stress.
Surgical treatment
Surgery for intestinal inflammation is required in situations:
- primary acute inflammatory process or worsening of ulcerative colitis, if there is no positive response of the body to drug therapy for 2-4 weeks;
- progressive chronic ulcerative colitis with regular relapses and no improvement with anti-inflammatory drugs for 6 months;
- total damage to mucous tissues with degeneration of the structure of the mucous membranes of the rectum or colon;
- concomitant life-threatening diseases (including perforation, peritonitis, megacolon, abdominal abscesses, intestinal obstruction) - for any location of ulcerative colitis.
If the disease threatens the patient's life, surgery is performed immediately. When treating chronic ulcerative colitis, the doctor has more options for planning. Preparation for planned intestinal surgery may include dietary changes and auxiliary courses of medications.
Photo: sasint / Pixabay.com
On average, one in 10 patients suffering from intestinal colitis requires surgery. 25% of cases of surgical intervention are due to intestinal pancolitis. Operations are divided into two groups:
- Bringing a section of the colon to the surface of the abdomen - colostomy or ileostomy. Reasons for surgery include life-threatening exacerbations of ulcerative colitis and critical destructive changes in areas of the intestine above the colon. A small section of the colon is selected above the area where the disease is located so that the inflamed section of the intestine is not involved in digestion. To collect stool directly from the designated area of the intestine, the patient will have to use a colostomy bag. In most cases, changes in bowel function are limited to a short period of time. The prognosis for recovery is favorable. The absence of digestive stress allows the intestines to recover and plan further procedures. After recovery, the hole is eliminated. If ulcerative colitis is advanced, this method is often the only way to achieve long-term remission. In this case, coloproctectomy with the formation of an opening is advisable. The formed ileostomy remains accessible for care and hygiene procedures. This method greatly facilitates the patient’s daily life and reduces the likelihood of postoperative depression.
- Removal of the affected area of the intestine or the entire rectum. Reasons include advanced colitis in the terminal stage, degradation of certain parts of the intestines, and the development of dangerous diseases against the background of ulcerative colitis. It is recommended only in extreme cases when it is impossible to achieve remission in a more gentle way.
After the first surgical intervention, long-term remission occurs. Appetite normalizes, the patient gains weight, and begins to sleep normally at night. The normal balance of vitamins and minerals in the body gradually returns, and signs of immunodeficiency disappear. When hemoglobin levels stabilize and long-term remission is achieved, you can proceed to radical measures - removal of the damaged area of the rectum.
The recovery period before the last operation takes from 2-3 to 6 months. At this stage, many patients begin to doubt the advisability of repeated surgery. The doctor’s task is to determine whether there is a reason to remove a section of intestine and to persuade the patient to consent to the operation. For many patients, the deciding factor is understanding how much better the colon and the rest of the intestines will cope with their functions.
Classification
To clarify the nature of the lesion and the extent of the process, gastroenterologists use the classification. The diagnosis of ulcerative colitis is made based on the criteria presented in Table 1.
Table 1. Classification of UC
| Category | Kinds |
| By localization | Distal form: proctitis; proctosigmoiditis; Left-sided form (to the middle of the colon) Subtotal Total Total colitis with retrograde ileitis |
| With the flow | Spicy Chronic Recurrent |
| Stage | Exacerbations Remission |
| By severity | Lightweight Average Heavy Extremely Heavy Attack: lightning; sudden. |
During the examination, specialists are guided by the data obtained as a result of colonoscopy. Imaging features according to Schroeder endoscopic activity are presented in Table 2.
Table 2. UC activity
| Activity in points | Signs |
| 0 points - normal | Pathological changes in the mucous membrane are not visualized |
| 1 point - minimal activity | Slight tissue hyperemia, blurred vascular pattern, slight vulnerability upon contact with the epithelium |
| 2 points - moderate activity | More pronounced hyperemia with the presence of ulcers, no vascular pattern, moderate vulnerability upon contact with the epithelium |
| 3 points - pronounced activity | An erosive-ulcerative process is detected against the background of bright hyperemia, spontaneous vulnerability upon contact with the epithelium. In the super-severe form, extensive areas of ulceration are observed against the background of infiltration of the mucous membrane. |
Description of the disease
Ulcerative colitis of the large intestine is an inflammation of the mucous membrane in the chronic phase, which appears due to genetic and external factors.
The disease may worsen, causing more severe symptoms. The pathology affects the rectum, and after a while the inflammation spreads to other parts of the intestine. In medicine, this disease is called nonspecific ulcerative colitis.
Most often, the disease develops in people 20-35 years old, as well as in old age after 60 years. Children are almost never exposed to this pathology, but there are cases when colitis appears in a child.
In medical practice, only 15% of cases of pathology in children have been recorded. Moreover, girls in adolescence are most susceptible to pathology, and for younger children, colitis is typical for boys.
Ulcerative colitis of the intestine is divided into several types, its classification is as follows:
- According to the clinical course, the pathology can be typical, atypical, chronic.
- Based on localization, distal colitis (proctitis), left-sided, which appears in the transverse colon, approximately to its middle, is distinguished. They also distinguish total with different types.
- According to the severity of symptoms.
Pathology changes the structure of the mucous membrane of the large intestine and in most patients inflammation and ulcer formation occur at the end points of the intestine, namely the rectum and sigmoid.
Much less often in medicine there are facts of damage to the entire intestine.
Symptoms of Ulcerative Colitis
Signs of the disease depend on the prevalence of the process, the severity and course of the pathology. Symptoms of ulcerative colitis are caused by damage to the lower gastrointestinal tract. As the condition progresses, syndromes are observed that indicate systemic disorders in the body. Manifestations of a typical and atypical nature are presented in Table 3.
Table 3. Symptoms of ulcerative colitis
| Intestinal | Extraintestinal |
| Changes in the nature and frequency of bowel movements - increased frequency of stools, urge to defecate, attacks at night | Dry skin, mucous membranes Increased temperature to subfebrile or febrile levels |
| Stool mixed with blood and mucus | Anemia |
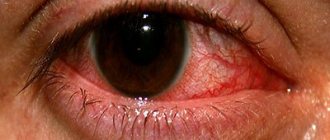
| Painful sensations in the lower abdomen, more often in the left half, occur periodically, are cramping in nature, intensify before the passage of feces, and subside after defecation | Protein-free edema Joint pain Eye damage - uveitis, iridocyclitis |
| Increase in temperature to subfebrile or febrile values | Damage to the skin, mucous membranes - erythema nodosum, pyoderma, aphthous stomatitis, psoriasis |
| Dehydration, electrolyte disturbances | Fatigue, weakness |
| Weight loss | Reduced pressure |
| Vomit | Damage to the liver and gallbladder - primary sclerosing cholangitis, pericholangitis, cholelithiasis, steatosis, steatolithiasis |
Important!
The severity of the clinic is determined by the activity of the inflammatory process.
Diarrhea can occur up to 20-30 times a day. Some patients experience constant stool discharge with pathological impurities, which is due to weakness of the anal sphincter. Some patients experience constipation with rectal bleeding.
Diagnostics
At the first stage, the doctor conducts an objective examination of the patient. It includes clarification of complaints, life history and illness, and examination of the patient. Subsequently, the specialist prescribes a list of studies to clarify the condition, which are presented:
- general clinical blood and urine tests;
- coagulogram;
- biochemical blood parameters;
- coprocytogram;
- determination of occult blood in feces;
- culture of feces on the intestinal group;
- cyto tests for viral intestinal infections;
- fluoroscopy and radiography using a contrast agent;
- CT and MRI;
- colonoscopy with biopsy of the mucous membrane;
- Ultrasound;
- transabdominal and transrectal scanning of various parts of the large intestine.
For extraintestinal manifestations, an additional consultation is prescribed:
- endocrinologist;
- dermatologist;
- rheumatologist;
- gynecologist;
- psychotherapist.
More accurate diagnosis allows you to find differences that help make a diagnosis and recommend adequate treatment. Ulcerative colitis must first be differentiated from the following diseases:
- Crohn's disease;
- bacterial and viral acute intestinal infections;
- helminthic infestations;
- intestinal tuberculosis;
- pseudomembranous colitis;
- colon cancer;
- diverticulitis;
- radiation, collagen, lymphocytic colitis.
Complications and consequences
If you do not treat colitis, do not use the right lifestyle, corrected nutrition, then the pathology leads to complications.
In this case, the main symptoms will become stronger, and characteristic signs may appear:
- Strong, copious discharge of blood.
- Anemia.
- Megacolon formation.
- Peritonitis.
- Perforation.
- Inflammation of the joints.
- Violation and deformation of internal organs.
The consequences of the disease can be the most dire, therefore, if the main symptoms of the disease develop, you should immediately consult a doctor for diagnosis and selection of a treatment regimen.
How dangerous is the disease?
Complications of ulcerative colitis, which occur with unfavorable development of the disease or lack of treatment:
- intestinal bleeding;
- toxic intestinal dilatation;
- perforation;
- colorectal cancer.
Bleeding from the intestine is considered to be a blood loss of more than 100 ml per day. The severity of the pathology is determined by clinical signs and increasing anemia during therapy. Deterioration of the condition threatens massive blood loss with the development of hemorrhagic shock. In such cases, emergency hospitalization for intensive care and surgical treatment is indicated.
Dilatation of the colon of more than 6 cm against the background of sudden stool retention and increasing intoxication indicates toxic megacolon - toxic dilatation of the intestine. If the patient develops the condition for the first time, intensive therapy with electrolyte solutions and hormonal treatment is carried out. When the situation is noted against the background of planned medication use, the issue of colectomy is decided.
Intestinal perforation is a very dangerous consequence, given its high mortality rate. A local rupture of the intestinal wall is noted in the area of ulceration. In this case, the contents of the lower gastrointestinal tract penetrate into the free abdominal cavity, which is characterized by symptoms of peritonitis.
Patients with ulcerative colitis are at risk for developing colorectal cancer. Therefore, it is important to undergo an annual examination to detect epithelial metaplasia. Once the diagnosis is confirmed, a consultation with an oncologist is necessary to determine treatment options.
Drug therapy, groups of drugs used and dosage regimens
Drug therapy is carried out not only to eliminate the symptoms of ulcerative colitis, but also to prolong the period of remission. The treatment schedule for each patient is drawn up individually. Patients undergo a long course of therapy with minor breaks.
UC (treatment for exacerbation of the inflammatory process is carried out under the strict supervision of a specialized specialist) requires the use of the following medications:
| Group of drugs | Name | Application |
| Antibacterial agents | Cifran, Ciprofloxacin | The dosage of the drug depends on the patient’s condition and is 250-750 mg every 12 hours. It is recommended to take the medicine before meals. |
| Restoring intestinal normobiosis | Bifidumbacterin, Linex | The medicine should be taken orally with meals. The standard dosage is 2 capsules 2-3 times a day. The course of treatment lasts 5-7 days. In severe situations, the period is extended to 3 weeks. |
| Immunomodulatory therapy | Cyclosporine, Azathioprine | Medicines suppress the action of one’s own immunity, which kills healthy cells in the body. The recommended dosage for adults is 3 mg/kg, divided into 2 doses. The course of therapy lasts 6-12 weeks. |
| Stabilization of the gastrointestinal tract | Riabal, Platyfillin | The drugs help eliminate diarrhea and restore the functioning of the digestive system. The medicine is administered subcutaneously. Adult patients are prescribed 1-2 ml 1-2 times a day. The course of treatment lasts 10-20 days. |
| Corticosteroids | Prednisolone, Budesonide | Medicines have a powerful anti-inflammatory effect. Patients are prescribed 20-30 mg per day (4-6 tablets). The indicated dosage should be divided into 2-3 doses. The tablets are taken orally after meals with a sufficient amount of liquid. |
| Painkillers | Paracetamol, Ibuprofen | The standard dosage is 1 tablet. It should be taken 3-4 times a day every 6-8 hours. The course of therapy lasts 3-4 days. |
| Tranquilizers | Elenium, Seduxenus | Medicines restore the functioning of the central nervous system if UC provoked psycho-emotional disorders in a person. For adult patients, the drug is prescribed orally at a dose of 5-10 mg per day. If necessary, the dosage is increased to 30-50 mg and divided into 3-4 doses. |
| Aminosalicylates | Mesalazine, Sulfasalazine | The drugs stabilize the condition of a person with ulcerative colitis and prolong the period of remission. The medicine must be taken orally after meals. Swallow the tablets whole with plenty of water. For patients with ulcerative colitis, the dosage is 4 g per day, it should be divided into 2-4 doses. The course of treatment lasts 2-3 months. |
Additionally, patients are prescribed medications that contain iron. They help reduce symptoms of anemia. Vitamin-mineral complexes are necessary to compensate for the lack of vitamins in the patient’s body.
Treatment
Treatment of ulcerative colitis includes several areas. The main methods include conservative therapy. A set of measures is prescribed to patients with mild to moderate severity. Surgical intervention is performed according to strict indications in case of ineffective assistance with medications and the presence of complications.
Ulcerative colitis can be cured using an integrated approach, which is represented by a number of stages:
- Use of medications.
- Diet.
- Folk remedies.
- Psychosocial support.
Drugs
The first line of help is the use of medications that effectively and quickly reduce inflammation and eliminate other intestinal and extraintestinal manifestations. Medicines are prescribed in tablets, capsules, and solutions. Therapy for ulcerative colitis is aimed at the pathogenetic links of the process. The main drugs used for UC are represented by the following groups:
- Aminosalicylates - Sulfasalazine, Mesalazine.
- Glucocorticosteroids - Hydrocortisone, Budesonide.
- Immunosuppressants and biological drugs - Azathioprine, Mercaptopurine, Cyclosporine, Infliximab, Tacrolimus.
When an acute intestinal infection occurs, antibacterial agents, sorbents, and probiotics are included.
Nutrition
The menu is developed taking into account the severity of the pathology and the individual needs of the patient. The diet for ulcerative colitis corresponds to table 4 and its modifications, taking into account periods of exacerbation and remission. Food should be high in calories, up to 3000 kcal per day. The exception is for overweight patients.
Meals are divided into 5-6 servings. The last dish is given no later than 2 hours before bedtime. They steam, boil, and stew food.
You can eat:
- thermally processed vegetables and fruits;
- slimy soups and cereals;
- lean meat, fish;
- yeast-free bakery products;
- scrambled eggs.
Compotes and jelly made from dogwood, quince, blueberry, and bird cherry are allowed.
Prohibited products include:
- plant foods rich in fiber;
- coarse wheat porridge;
- broths;
- dairy products;
- fatty meats and fish;
- sweet dough.
Avoid alcoholic drinks, soda, strong coffee and tea.
Folk remedies
For pathological processes of the colon, medications made from natural ingredients are widely used. They gently eliminate symptoms, promote healing of the mucous membrane, and reduce inflammation. Ulcerative colitis is treated with folk remedies based on:
- burdock leaves and roots;
- calendula herbs;
- rosehip roots;
- oak bark;
- burnet roots;
- peppermint herbs;
- stinging nettle leaves;
- horsetail grass;
- Colgan root.
Diet 4B and nutrition for acute ulcerative colitis
A specially formulated diet for patients with ulcerative colitis will help reduce the symptoms of the disease, prevent irritation of the mucous epithelium and improve the general condition.
| Authorized Products | Prohibited Products |
|
|
Additionally, patients need to remember simple recommendations from a specialist regarding diet:
- You should eat food in small portions. Overeating is strictly prohibited.
- The food should be warm. Hot or cold foods are prohibited.
- Before going to bed, the last meal is taken no later than 7 pm.
- The diet must contain fortified foods, which also contain essential microelements.
- It is necessary to drink enough fluids; many patients are dehydrated.
- Food should be chewed thoroughly so that the necessary substances are well absorbed.
When treating an exacerbation of ulcerative colitis, patients are advised to strictly adhere to bed rest until the symptoms of the disease subside.
With UC (nonspecific ulcerative colitis), it is important to follow a diet
Sample daily menu for nonspecific ulcerative colitis:
- First breakfast – steamed omelette, light tea.
- Second breakfast – baked apples.
- Lunch – chicken broth, carrot puree, steamed cutlets, jelly.
- Afternoon snack – cocoa prepared with water.
- Dinner – mashed potatoes, boiled fish, weak tea.
Before a night's rest, patients with ulcerative colitis are recommended to drink jelly. Diet is a must for patients with colitis who want to achieve long-term remission.
Do they take you into the army?
If males over the age of 18 have the disease, the question arises whether they can be drafted into the army. Exemption from service of young people with ulcerative colitis is carried out after the conclusion of a special commission. Young men who have been diagnosed with a severe form of pathology with a chronic course are not liable for military service.
Evidence must be provided to confirm the diagnosis. These include official documents, discharge summaries, which contain convincing data on the state of a person’s health. Copies are submitted to the commission. The originals are kept by the patient.
Predictions and prevention
The prognosis of the disease depends on the severity of the condition and the extent of the process. With total damage, the likelihood of a severe course is higher than with local colitis. Against the background of anti-relapse treatment, half of the patients manage to avoid re-exacerbation. The more aggressive the pathology, the higher the risk of surgical intervention.
Factors that provoke the unfavorable development of UC include childhood, primary sclerosing cholangitis and rapid progression of inflammation.
Ulcerative colitis can be prevented at several stages. Primary prevention consists of:
- reducing the influence of negative factors;
- timely treatment of acute and chronic diseases;
- quitting smoking;
- proper nutrition.
Adequate diagnosis and treatment can reduce the risk of developing severe complications and improve the patient’s quality of life.
If ulcerative colitis is diagnosed, treatment recommendations must be strictly followed. It is important to adhere to an adequate dose of drugs and duration of therapy. You should regularly visit a gastroenterologist, conduct general clinical and instrumental studies to monitor the course and symptoms of the inflammatory process.
Prevention
To prevent the development of ulcerative colitis, it is necessary to pay special attention to nutrition, daily routine, and overall health. The key to successful treatment of colitis is its timely diagnosis. When the first symptoms of the disease appear, it is recommended not to delay a visit to a medical specialist.
It is important to remember that the chronic course of erosive ulcerative colitis can provoke the development of more serious diseases. Timely diagnosis of ulcerative colitis allows you to avoid serious complications.