Differences between benign and malignant tumors
When making an accurate diagnosis, a biopsy (examination of biological material taken) is performed to determine the nature of the origin of a malignant or benign tumor.
The main differences between the two tumors:
- According to general statistics, malignant tumors are growing rapidly in comparison with benign ones. In this case, opposite cases occur;
- Spreadability. Benign tumors have a local expansion, and malignant ones can metastasize to other organs when they enter the general bloodstream through the lymph;
- Benign tumors are located locally, and malignant tumors can re-develop in distant places (lungs, bones, liver, brain);
- The presence of a “sticky” effect in benign cells, since they do not have the ability to separate and move in comparison with malignant formations;
- Development of tissue invasion. Malignant tumors most often grow and are localized in other organs. At the same time, benign formations do not have the ability to develop in other organs, but can grow greatly and put pressure on nearby areas of the body;
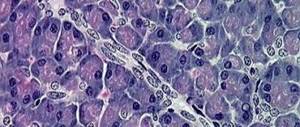
- Changing the appearance of cells. When studying benign and malignant cellular structures under a microscope, the nuclei of cancer cells have a darker shade;
- Treatment difference. Benign tumors are easily eliminated through surgery. Cancers require chemotherapy, radiation, and surgery if possible. This technique is aimed at eliminating the re-development of the oncological process;
- The occurrence of relapse. After removal of a benign tumor, recurrence of the tumor is diagnosed quite rarely. If we talk about the malignant course of the process, then it is repeated much more often;
- Obtaining a systemic effect, which is observed during the development of malignant tumors (general weakness, weight loss), since cancer cells affect other vital systems in the body. Benign formations do not have such a large list of side effects;
- Fatality statistics indicate that benign tumors cause about 13,000 thousand deaths per year, and malignant tumors cause more than 570,000 thousand deaths.
Benign and malignant tumors also have some similarities in the form of large sizes, degree of danger in the absence of the correct treatment regimen, and local recurrence after immediate removal.
Why is pancreatic adenoma dangerous and how to cure it?
Tumors can affect any organ. Adenoma is one of the types of benign neoplasms. Most often, this disease affects adults over 45 years of age.
About the disease
Pancreatic adenoma is not very widespread. But now, the incidence of this disease has increased significantly. This may be due to significant environmental deterioration and poor nutrition, which is typical for the majority of the population.
The tumor affects any of the parts of this organ: head, body, tail. But the majority of neoplasms (70%) occur in the head of the pancreas. The tumor may be single or have multiple processes.
The structure of the pancreas
This type of tumor originates from glandular tissue. The course of the pathological process, if benign in nature, will most likely end happily. Adenoma has a number of characteristic symptom complexes:
- no metastasis to nearby systems and regional lymph nodes;
- structurally, tumor tissue is identical to a healthy organ;
- no germination into nearby tissues and organs;
- has a capsule and is clearly demarcated.
Under certain circumstances, a pancreatic adenoma can develop into a malignant neoplasm.
With surgical intervention, the survival rate is much higher than with the degeneration of an adenoma into a malignant process.
What causes it to form
The formation of adenoma can be triggered by several factors. The most common include:
- constant exposure to harmful chemical compounds (work in hazardous industries);
- frequent smoking;
- cirrhosis of the liver;
- pancreatitis (chronic);
- poor diet (excess fatty foods);
- cystic formations in the gland itself;
- endocrine diseases (diabetes mellitus);
- calculous cholecystitis.
The development of prostate adenoma against the background of alcohol dependence has not been experimentally established.
Kinds
When examined for histology, in 80% of cases the tumor is of epithelial origin. From acinar cells - adenoma, from ductal epithelium - cystadenomas. There is a division of the tumor into microadenoma, macroadenoma and a process that is intermediate.
| Type of tumor | Characteristic |
| Microadenoma | Formation measuring 0.5mm-0.5cm. The tumor process is discovered by chance. It has a high content of hormones (insulin, somatostatin, glucagon, pancreatic polypeptide), but there are no clinical symptoms. |
| Macroadenoma | Diameter of tumor formation: 0.5cm-2cm. It looks like a node with distinct outlines. Most likely it is encapsulated. Contains a large number of endocrine markers and hormones. |
| Intermediate | Size over 2 cm. It has a secretory function and produces the most common hormones. The main symptoms are determined by their excess production. Tumor processes also occur, characterized by a course without pronounced symptoms. |
Based on its functional manifestations, benign adenoma can be divided into hormonally active and inactive tumors. A tumor that does not produce hormones has no clinical symptoms. Therefore, it may be detected by chance.
Tumors that produce hormones include:
- insulinoma (pathological cells produce insulin);
- islet adenoma (hypoglycemia + hyperinsulinism).
Benign adenoma refers to cystic tumors . According to this characteristic, it is divided into 4 subspecies:
- serous;
- mucinous;
- border;
- intraductal papillary mucinous.
| View | Characteristic |
| Serous cystadenoma | Most likely it occurs from epithelial cells as a result of a malfunction in the structure of the chromosomal apparatus. Difference from others: the presence of multiple partitions inside the formation. There is no degeneration into a malignant neoplasm. Surgery is prescribed only if significant tumor growth is observed (more than 6 cm). |
| Mucinous cystadenoma | It has a cyst-like structure (up to 10 cm-15 cm), filled with hemorrhagic contents or mucus. It begins its formation from ovarian tissue. It enters the pancreas during the period of intrauterine development. It has a very high percentage of degeneration into a malignant process. |
| Borderline cystadenoma | It is a transitional state between benign and malignant neoplasms. |
| Intraductal papillary mucinous tumor | Rare subspecies. Develops from the epithelium of the pancreatic ducts. It may produce thick mucus. A pronounced pathological process may be observed in one of the sections of the pancreas. Method of treatment: total resection. |
What harm does
If a benign tumor is detected at the initial stage, the prognosis is very favorable. But its presence can bring a lot of inconvenience to the patient or threaten serious complications.
A rapidly growing tumor process can compress the bile duct. The result is bile intoxication.
As an adenoma grows from the cells of the islets of Langerhans, insulin secretion increases and the blood glucose level decreases. There is a high risk of degeneration of certain types of benign processes into malignant neoplasms.
A benign adenoma can cause the development of inflammatory processes . In particular – pancreatitis.
Symptoms
The symptoms of the disease are influenced by many factors: size, location, histology analysis.
All symptoms can be divided into two categories: early and late. Early symptoms appear when the tumor process is not yet pronounced and the adenoma itself has not reached a large size.
With late symptoms, the growing benign process begins to appear in all its glory. The symptoms correspond to the ongoing processes: pressure on the vessels, nerves, pancreatic ducts, neighboring organs and tissues.
During the early stage of the pathological process, symptoms may not be observed. In this case, the cyst may be discovered completely by accident. If symptoms are still present, they may be as follows:
- pain in the abdominal area;
- pain under the ribs on the left or right side;
- pain radiates to the back area;
- at night the pain may intensify;
- discomfort occurs after eating;
- the patient’s weight gradually begins to decrease;
- nausea;
- loss of appetite;
- constant weakness;
- decreased performance.
As the tumor process grows, the symptoms worsen. It is the deterioration of the condition that makes the patient think about the disease and serves as a reason to see a doctor.
The very first sign of deterioration of the condition are symptoms that are associated with the pressure of the growing pancreatic adenoma on the biliary tract. They can completely overlap. Characteristic signs of the emergence of this process will be:
- yellowness of the skin and visible mucous membranes;
- urine is dark in color;
- feces become significantly lighter (discoloration occurs);
- nausea;
- indigestion;
- feeling of chills;
- epigastric pain;
- symptoms of general intoxication of the body.
Late symptoms of benign adenoma are characterized by:
- frequent bouts of vomiting observed after eating;
- significant pain in the anterior abdominal wall;
- feeling of fullness;
- unreasonable feeling of fear;
- sweating
As the tumor grows, compression of the duodenum may occur. In this case, the diet is immediately disrupted. Hypoglycemia and weakness occur throughout the body. In women, this pathological process causes a disruption in the menstrual cycle.
Symptoms may increase gradually or occur suddenly.
Treatment
Despite the fact that adenoma is a benign neoplasm, therapy is only surgical. After the operation, a piece of the removed tumor is necessarily sent for histological analysis in order to clarify the type of disease.
If the tumor is hormone-dependent, insulin levels are stabilized with medications.
After surgery to remove an adenoma, it is necessary to undergo a course of rehabilitation therapy. It is as follows:
- certain dietary therapy lasting 12 months;
- use of enzymatic medications;
- removal of heavy physical activity for six months;
- use of a special bandage for 3 months. after operation;
- sanatorium treatment.
To maintain a certain diet, you must follow the following recommendations:
- the portion of food taken is reduced to the size of the patient’s fist (the load on the stomach and intestines is reduced);
- have a snack every 3 hours;
- take food warm;
- exclude smoked, flour, fatty foods;
- from meat: beef, veal, chicken, turkey;
- fish – lean;
- from dairy products: low-fat cottage cheese;
- exclude: carbonated drinks, chocolate, ice cream, marinades, spices, store-bought convenience foods.
The pancreatic adenoma itself does not pose a threat to the patient’s life. After the operation there is a 100% recovery. Its possible degeneration into a malignant process is dangerous. To prevent this from happening, at the slightest suspicion of a disease, you must consult a doctor.
How resection is done using the laparoscopic method is shown in this video:
, please select a piece of text and press Ctrl+Enter.
Source: https://stoprak.info/vidy/zhkt-kishechnik/podzheludochnaya-zheleza/adenoma-opisanie-oslozhneniya-reshenie-problemy.html
ICD 10 code
The International Classification of Diseases subdivides special codes for malignant tumors of the pancreas:
- C25. 0 (damage to the head of the pancreas);
- C25.1 (body of the pancreas);
- C25.2 (tail of the pancreas);
- C25.3 (pancreatic duct);
- C25.4 (defeat of the “islands of Langerhans”);
- C25.7 (other parts of the pancreas);
- C25.8 (organ damage that extends beyond the specified localizations);
- C25.9 (unspecified lesion of the pancreas).
Edema and diseases of the pancreas
As a rule, swelling of the pancreas is the result of improper activity of the digestive enzymes that it produces. Impaired functioning most often causes a primary disease. The most common are:
- cholelithiasis (occurs very quickly);
- alcohol abuse (long process).
Acute pancreatitis can be caused by other diseases:
- diabetes;
- damage to the pancreas due to injury or surgery;
- infectious diseases;
- blocked ducts;
- malignant tumors.
Return to contents
Types of tumors
Pancreatic tumors are classified into benign and malignant tumors. An accurate diagnosis is based on the location, changes in cellular structures (histology), and the effect on the normal functionality of the organ.
The tumor can develop in the body, tail, and head of the organ. Malignant cells can have the following types:
- Adenoma;
- Acinar cell carcinoma;
- Adenocarcinoma;
- Squamous cell carcinoma.
Cells formed as a result of endocrine disorders have names such as gastrinoma, insulinoma, carcinoid.
A type of malignant tumor is blastoma, which occurs during intrauterine development, which contributes to the formation of cancer in childhood.
The stage of the oncological process depends on the size of the resulting formation:
- The formation of mutated cells, which are characterized as “cancer in the zero stage”;
- The first stage implies the presence of a tumor measuring 2 cm without pronounced clinical symptoms;
- At the second stage, the growth of cancer cells and the spread of metastases are noted;
- The third stage involves damage to the portal vein and other large organs;
- At the fourth stage, the patient’s general condition is unstable, and examination reveals extensive metastases throughout the body.
Benign tumors develop slowly and do not metastasize, since the cells do not change differentiation. When performing an ultrasound, a formation with hypoechoic edges containing fluid inside is clearly visualized.
Serous tumor
This type of benign neoplasm is characterized by the presence of several cystic cavities filled with serous fluid. Each part of the cystadenoma is separated from the other by partitions. It is believed that a serous tumor develops as a result of a gene mutation in one of the chromosomes.
The internal part of the neoplasm is lined with epithelium, consisting of single-layer cubic cells. In addition, the tumor contains glycogen, combined into several granules.
In rare cases, people develop serous cystadenomas with a single cavity. Such formations have no partitions.
On this topic
- Digestive system
The role of hormonal contraceptives in the development of liver hemangioma
- Natalya Gennadievna Butsyk
- December 6, 2020
Serous tumor is characterized by slow growth. The cells of these cystic cavities do not transform into cancerous ones. On average, serous cystadenomas reach 7 cm.
An important feature of tumors of this type is the absence of pronounced clinical phenomena that occur as the tumor grows. Therefore, surgical intervention is rarely performed for such neoplasms. Surgeries are prescribed if the size of the cystic cavity exceeds 6 cm or the development of the tumor is accompanied by severe symptoms.
Causes of tumors
The etiology of the origin of pancreatic tumors does not have exact causes that cause the development of pathologies in the body. Possible provoking factors:
- The presence of chronic pancreatitis with frequent exacerbations;
- Genetic predisposition;
- Abuse of bad habits (alcohol, cigarettes, high-calorie foods);
- Endocrine disorders in the body (development of diabetes, obesity);
- Severe stress, nervous disorders;
- Chronic diseases (stomach and intestinal ulcers, caries, inflammation in the oral cavity).
Peculiarities
Cystadenoma is mainly diagnosed in women aged 25-75 years. In most cases, a pathological neoplasm does not pose a threat to the life and health of the patient. However, cystadenoma requires surgical removal, otherwise there is a risk of degeneration of the cystic cavity into a malignant tumor.
This type of formation is formed from epithelial cells of the pancreas. The shape of the tumor is predominantly oval or round.
The shell of cystadenoma is dense, up to 1.5 cm thick. This neoplasm consists of multiple small cavities. The latter are connected to each other through thin partitions. Large tumors consist of single cavities.
On this topic
- Digestive system
Differences between sigmoidoscopy and colonoscopy
- Natalya Gennadievna Butsyk
- December 9, 2020
The exact causes of cystadenoma remain unknown. It is believed that the development of a tumor can lead to:
- smoking;
- poor nutrition;
- poor environmental situation.
A number of researchers believe that the appearance of cystadenoma may be due to genetic predisposition.
Main symptoms
The symptoms of tumor development in the body depend on the nature of their origin. In benign formations, the signs of intoxication are mild, the presence of cysts and the absence of a genetic predisposition for the occurrence of malignant formations are possible.
Benign formations can be large and easily palpable through the abdominal wall. However, they do not cause great danger to the body, and when neighboring organs are compressed, the patient may experience characteristic symptoms.
A pronounced clinical picture is presented with the development of hormonally active tumors during an endocrine disorder in the body. The growth of education increases the level of gastrin, which leads to signs of peptic ulcers, stool disorders, and a pronounced decrease in electrolytes in the blood.
Malignant tumors also have pronounced symptoms, which, as the tumor grows, manifest themselves in the form of severe weight loss, general weakness, and digestive disorders (nausea, vomiting with blood, flatulence).
Making an accurate diagnosis is possible after a thorough examination and a mandatory biopsy to determine the nature of the identified formation.
Possible complications
In addition to a cancerous tumor, the appearance of cystadenoma provokes the development of:
- pancreatitis (inflammation of the pancreas);
- poisoning of the body with bile;
- dysfunction of the endocrine system;
- diabetes mellitus
On this topic
- Digestive system
Irrigoscopy or colonoscopy
- Olga Vladimirovna Khazova
- December 3, 2020
In the case of severe compression of the duodenum, stenosis may develop, which manifests itself in the form of:
- belching;
- frequent vomiting, which brings relief;
- asymmetrical bloating ;
- constipation;
- gases
Compression of the bile ducts causes darkening of the urine and lightening of the stool. If left untreated, this type of disorder can lead to liver failure.
Symptoms and treatment methods for pancreatic tumors in women
The clinical picture of pancreatic tumors has the same symptoms in men and women, which depend on certain factors:
- Type of tumor;
- Localization location;
- Degree of malignancy;
- Prevalence of metastases.
At the initial stage of development, the neoplasm does not have pronounced symptoms, but with gradual development characteristic signs appear:
- Fatigue, weakness;
- Constant heaviness and bloating;
- Stool disorder (diarrhea, constipation);
- Loss of appetite.
Subsequently, the pathology causes compression of the bile ducts, which leads to obstructive jaundice with exacerbation of pain in the left hypochondrium.
Jaundice occurs with severe symptoms:
- Yellow staining of mucous membranes and sclera;
- Discoloration of stool;
- Enlarged liver, gall bladder;
- The appearance of skin itching.
A malignant formation in the body or tail of the pancreas does not have pronounced symptoms for a long time, and as it develops, severe pain in the epigastric region appears.
Severe inoperable cancer is characterized by the following symptoms:
- Growth of the primary tumor into neighboring organs;
- Spread of metastases;
- The presence of digestive insufficiency;
- General intoxication of the body;
- Violation of the blood clotting process.
Symptoms of stage 4 pancreatic cancer:
- Severe weight loss and weakness;
- The appearance of fluid in the abdominal cavity;
- Blood clot formation;
- Enlarged lymph nodes in the collarbone area;
- Palpation of the formation at the site of localization.
Treatment of pancreatic tumors is based on surgery. If we are talking about a malignant formation, then chemotherapy is required as prescribed by a doctor, and therapeutic measures to maintain immunity.
The prognosis depends on the extent of the lesion, the location of the formation and the prevalence of cancer cells. The last stage most often leads to death.
Mucinous tumor
Mucinous cystadenoma is a multilocular benign tumor that usually reaches large sizes. The inside of the cystic cavities is filled with hemorrhagic contents or viscous mucus. In this case, the formation of a mucinous tumor with a single cavity is possible.
It is assumed that this type of cystadenoma occurs due to the penetration of ovarian tissue into the pancreas. Similar events occur during the intrauterine development of a child.
This type of tumor tends to grow rapidly. Primary signs usually occur when the cystadenoma reaches 10-15 cm in diameter. The development of a neoplasm is often accompanied by pain and discomfort in the upper abdomen.
Due to the fact that mucinous tumors often degenerate into malignant tumors and are also prone to rapid growth, treatment is carried out primarily through surgery.
Diagnostics
Diagnosis of pancreatic tumors is based on consultation with doctors such as a gastroenterologist, oncologist, surgeon, and endoscopist. The following types of laboratory and instrumental studies are prescribed:
- General and biochemical blood test to identify changes in key indicators;
- Coprogram (stool analysis to detect blood, fat, mucus);
- Carrying out EGFDS (determination of the secretion of digestive juices);
- Ultrasound for visualization of formation;
- X-ray of the abdominal organs;
- CT, MRI;
- Detection of hormone levels and the presence of cancer markers in the blood;
- Biopsy (sampling of biological material) for histology.
Treatment of edema with pancreatitis
Treatment of the pancreas is aimed at relieving signs of the disease (swelling, pain), and then eliminating the immediate cause. Specialists prescribe therapy for the pathology based on the diagnosis. Edema due to diabetes mellitus, cholelithiasis or alcohol syndrome requires an individual approach. Basically, for edema with signs of pancreatitis, therapy includes a medication approach, diet, and in serious situations, surgery.
Medicines
General treatment includes the use of a number of mandatory medications. Drugs based on antispasmodics or novocaine help relieve pain due to swelling. The use of medications that suppress the activity of trypsin, plasmin and other pancreatic enzymes is mandatory. To avoid complications such as acute infections, antibiotics are prescribed.
To avoid recurrence of exacerbations, after prescribing general drug therapy, medications that eliminate the underlying disease that caused the acute condition are added to the prescriptions. If it is diabetes, insulin medications are included in the prescriptions. One of the safest ones is Humalog. Long-acting medications include Lantus and short-acting Novorapid.
If the cause of the edema is cholelithiasis, the patient is prescribed drugs based on bear bile (ursodeoxycholic acid). Using all possible modern medications, you can quickly relieve the unpleasant symptoms of the disease and restore the functions of the pancreas.
Diet food
During pancreatic therapy and in the future, to prevent recurrent complications, the patient is advised to follow a balanced diet, which helps eliminate the signs of the disease. During the acute period, fasting is recommended during the day; subsequently, meals should be in small and frequent portions. A special diet is prescribed:
- Dietary nutrition is based on reducing the amount of salt consumed and prohibiting salty, smoked and fried foods. Completely exclude canned food, alcohol, and baked goods from the menu;
- All dishes for the patient are served in a pureed, semi-liquid consistency. It is recommended to steam cutlets, lean fish, and chicken. Potatoes are allowed for vegetables, and for decoctions - rose hips, currants, weak black tea.
If swelling occurs due to diabetes, limit the intake of carbohydrates. Pumpkin, cabbage, zucchini, carrots, and peppers are great for cooking, but potatoes, corn, baked goods, dairy products, and fruits are not recommended for people with diabetes.
Surgery
In severe forms of complications, surgical treatment is indicated. The type of operation depends directly on the characteristics of the inflammation. If the structure of the organ tissue is destroyed, laparotomy is used, in which the damaged areas are removed. In particularly difficult cases, the pancreas is removed completely, sometimes along with the gall bladder. The doctor eliminates the resulting accumulation of fluid in the abdomen using peritoneal lavage. If the cause of the swelling is a violation of the head of the organ, the doctor eliminates the problem through surgery. Cancer can also be treated with surgery.
Treatment method
Treatment of pancreatic tumors is carried out in special diagnostic centers, which conduct a range of studies, and the conclusion of specialists determines the further treatment regimen.
The main method is surgical intervention, depending on the location of the lesion and the type of formation that has arisen. The procedures used are discussed in more detail below.
Head resection
This operation is performed when a tumor forms in the tail of the organ and is performed as a partial resection with the removal of part of the pancreatic parenchyma. Complete excision of the head is quite difficult, since it is connected by a large number of blood vessels to the duodenum.
Enucleation
Removal of the resulting tumor by exfoliation of tissue. This procedure is performed when hormonal disorders occur (gastrinoma, insulinoma, somatostatinoma). The operation can be carried out if there are clear boundaries and dimensions of no more than 2 cm.
Contraindications are glucagonoma and the presence of chronic pancreatitis. The technique is carried out using laparoscopy (a small incision in the abdominal cavity and removal of the cavity). Recovery lasts 3–4 days, and then it is necessary to follow the therapeutic diet No. 5 with moderate physical activity.
Pancreaticoduodenectomy
Pancreatoduodenal resection involves complete excision of the head, gallbladder, part of the small intestine, stomach, and lymph nodes. This procedure is quite complex and should only be carried out by highly qualified specialists.
Indications for surgery are large benign or malignant tumors. The organs are removed sequentially and an artificial duct is created in the resulting space.
Gastrectomy
During gastrectomy, the stomach is completely removed and an anastomosis is formed. The operation is performed for indications such as multiple ulcers due to the development of gastrinoma. At the same time, resection of the initial section of the intestine is performed.
Selective arterial embolization
This technique is based on the introduction of a special substance that thromboses blood into the vessels of the organ, which reduces the size of the formation and prevents the development of computed angiography. The removed tumor must undergo histology.
Treatment methods
The choice of a restorative course in the treatment of pancreatic adenoma depends on its size and additional factors. Small opuoles are usually not removed, but observed. But large seals require surgical intervention. chemical methods of influence do not help, therefore they are not used.
Drugs
At the early stage of the pathology, the doctor chooses a wait-and-see approach. The dynamics of the development of the tumor and its impact on the patient’s condition are monitored. If the capsule size is small and there is no serious threat to health, drugs are prescribed to stimulate the digestive tract.
They help improve the functioning of the gastrointestinal tract and make you feel better. Drug treatment is also used in situations where surgery is contraindicated for some reason.
Surgery
When a large adenoma is detected, the doctor almost always insists on its surgical removal. The operation will reduce the risk of relapse and relieve discomfort. One of the types of operational influences is used:
- enucleation (also known as enucleation). Provides for the removal of the capsule from the gland tissue. There is a possibility of re-formation of a cavity, since tissues can become damaged on the surface of the organ,
- laparoscopy. A minimally invasive method of intervention that involves making pinpoint punctures. Prescribed if the cystic thickening is localized in the east and has slightly increased in diameter,
- resection is a cavity operation in which healthy tissue is excised to get to the opuoli itself and remove it,
- pancreatoduodenal resection is the most radical type of treatment. It involves removing not only the tumor, but also part of the gland. This method is used when seals are large and it is impossible to use other surgical methods.
Treatment with folk remedies
Alternative treatment for benign tumors is used only to alleviate the condition and reduce unpleasant symptoms. Medicinal herbs do not cope with the neoplasm. And it can be used only after agreement with your doctor.
To improve well-being, take parsley juice, which is pre-mixed with honey in equal proportions. The product is taken orally, 2 teaspoons several times a day.
Another folk method is chaga mushroom in combination with some medicinal herbs. You can take hazel or a spade. Mix the ingredients in equal proportions and brew with boiling water. Boil for several minutes, cool and take 2 tsp orally.
Prognosis and prevention
The prognosis for detecting pancreatic tumors varies, since much depends on the type and degree of damage to the organ. If formations are detected at the initial stage without the presence of malignant cells, then the probability of a favorable outcome is high.
In case of malignant formations, it is important to promptly identify the formation and carry out removal after the completed course of chemotherapy. If the total area of the lesion is large with parallel formation of metastases, then the probability of death is high.
Prevention is based on following simple recommendations:
- Proper nutrition, excluding foods containing artificial additives;
- Elimination of bad habits (alcohol, cigarettes, high-calorie and fatty foods in large quantities);
- Timely visit to the doctor and completion of the necessary tests;
- Maintaining a healthy lifestyle and moderate exercise.
What is pancreatic adenoma, and how to treat it?
Pancreatic adenoma is a tumor that forms from the glandular component of the epithelial tissues of the digestive organ, and in most cases is directly related to hormonal disorders. The development of pancreatic adenoma begins under the influence of disruptions that occur in the natural chain of cell activity - division-reproduction-growth-death.
Symptoms and treatment of adenoma in the pancreas
Under the influence of negative factors that disrupt natural processes, a slowly developing formation atypical for a given organ is formed, which is characterized by:
- development in an isolated area of glandular epithelium, limited from surrounding tissue structures;
- failure to metastasize. Metastases in adenoma can appear only when a benign tumor, in the absence of treatment, rapidly progresses and becomes malignant;
- inability to have a negative impact on the body;
- susceptibility to most therapeutic measures;
- favorable prognosis for full recovery.
In clinical practice, there are often cases when pancreatic adenoma remains in its original state for a long time and then disappears. But, unfortunately, such an outcome is not always observed in the disease.
Sometimes an active process of malignancy begins in a benign tumor structure.
Under a certain set of circumstances and the absence of adequate therapy, the tumor structure begins to actively grow and in a short time turns into adenocarcinoma or pancreatic cancer.
Worth knowing! Patients with pancreatic adenoma are mainly middle-aged women. Representatives of the fairer sex are usually diagnosed with active forms of adenoma, which form against the background of irreversible sclerotic changes (replacement of the functioning cellular structures of the digestive organ with connective tissue elements).
Types of pancreatic adenoma
Due to the dual functioning of the digestive organ, adenomas are divided into two types:
- islets, which originate in endocrine cells that produce endocrine hormones;
- excretory, affecting cellular structures that secrete digestive enzymes.
In clinical practice, tumors are often divided by size into:
- microadenoma (0.5mm-0.5cm);
- macroadenoma (0.5cm-2cm);
- intermediate structure (diameter exceeds 2 cm).
All types have a high content of hormones actively produced by the gland, but their effect on the body, provoking the appearance of negative specific symptoms determined by the excess production of a certain hormone, is not the same. It increases from micro to macro formations, and is most pronounced in the intermediate form.
In addition, benign pancreatic adenoma is divided into 4 subtypes:
- Serous . It is provoked by chromosomal abnormalities, consists of many thin partitions and is characterized by the absence of a tendency to malignant degeneration.
- Mucinous . It looks like a cluster of cysts filled with mucus or hemorrhagic exudate, the diameter of which can reach 15 cm, originates in the germinal tissues of the reproductive organs, from where it penetrates into the pancreas and has a very high percentage of malignancy.
- Borderline, intraductal papillary-mucinous . Precancer, a transitional state between a benign and a malignant tumor.
Causes of pancreatic adenoma
The prerequisites that give impetus to the development of benign tumors prone to malignancy have not yet been fully established, although most experts believe that the main role is played by heredity, which predisposes to the onset of the neoplastic process.
In addition to the direct influence of genetics, oncologists indicate a number of factors under the influence of which pancreatic adenoma is most likely to develop:
- Hereditary or chronic forms of pancreatitis. A long course of the disease can lead to the development of a mutation process in the cellular structures of the gland.
- Alcohol abuse and tendency to smoke. These bad habits contribute to disruption of metabolic processes and blood circulation in the pancreas.
- Poor diet and sedentary lifestyle, contributing to the development of obesity, which negatively affects the functioning of the organ.
- A history of endocrine diseases (diabetes mellitus), Crohn's disease and ulcerative lesions of the stomach and duodenum.
Important! Based on the above reasons, experts identify a certain category of patients who are at risk for the development of this pathological condition.
It includes people living in areas contaminated by chemical emissions or radiation, who abuse alcohol and are addicted to nicotine.
This also includes patients with a history of chronic inflammatory diseases of the digestive organs.
Symptoms and manifestations of pancreatic adenoma
It is quite difficult to detect an adenoma long after the onset of the pathological process, which is associated with the asymptomatic development of the disease in the first stages.
The main symptoms of pancreatic adenoma appear several years after genetic or chromosomal damage to cells, when the tumor structure begins to increase in size and put pressure on tissues and vessels in the immediate vicinity.
Most often, the first signs of pancreatic adenoma are as follows:
- pain syndrome localized in the upper abdomen, directly under the ribs. It may be worse at night, felt on the right or left, and also radiate to the back;
- discomfort in the epigastric region, sour belching, heartburn, constant nausea, alternating regardless of food intake, gagging;
- loss of performance, general weakness and apathy;
- unreasonable decrease in appetite.
If the first signs are ignored and medical help is not sought, the pancreatic adenoma will continue to grow, resulting in compression of the pancreatic and bile ducts.
The pathological condition leads to the entry of aggressive fluids into the bloodstream and the development of more serious and dangerous symptoms.
At this stage, the disease is manifested by dark (beer-colored) urine, discolored feces, frequent diarrhea, and fever.
The best way to detect a pathological process is considered to be undergoing regular scheduled medical examinations, but, unfortunately, this is not always possible. In this case, experts recommend that you pay more attention to changes in your condition and, when the first, not entirely specific, alarming signs appear, consult a therapist and undergo an examination.
Diagnosis of pancreatic adenoma
For effective treatment, experts recommend paying attention to the most nonspecific symptoms that appear with pancreatic adenoma.
First of all, to identify a pathological condition, patients are prescribed a number of laboratory tests:
- coprogram;
- biochemical tests of urine and blood.
If their results reveal pathological changes, the patient is recommended to undergo an instrumental, more accurate diagnosis of pancreatic adenoma.
It is carried out using the following methods:
- Ultrasound. Ultrasound examination has been introduced into the standard of screening examinations for benign pancreatic tumors.
- MRI or CT. Such a visual examination for pancreatic adenoma allows the specialist to see the size and structure of the tumor in the resulting images.
- Esophagogastroduodenoscopy is an examination of the digestive organs using a special probe. It allows you to study their mucous membrane in detail and collect digestive juice for further laboratory analysis.
These techniques make it possible to detect the presence of a pathological, unusual formation in the pancreas, the diameter of which does not exceed a centimeter. But it is necessary to remember that it is impossible to determine the nature of the tumor structure developing in the digestive organ even with the help of the most modern diagnostic equipment.
The answer to this question can only be given by histological examination. In addition, a differential diagnosis of pancreatic adenoma must be established.
It is necessary to subdivide this benign, but prone to malignancy pathology with tumors of the retroperitoneal space and intestinal mesentery, pancreatic cysts, and chronic pancreatitis.
Treatment of pancreatic adenoma
This disease, before it begins to grow and enters the stage of malignancy, is classified as easily curable.
The doctor’s tactics when selecting a therapeutic course with which the treatment of pancreatic adenoma will be more effective depends on a large number of factors, but despite this, surgical intervention remains the main method of therapy when a benign tumor is detected in the pancreas.
The following types of operations are used to treat pancreatic adenoma:
- Laparoscopy. Using minimally invasive surgery, it is possible to remove a benign tumor located in the tail of the digestive organ.
- Resection. This type of operation involves excision of a pancreatic adenoma located in any of its parts - tail, body or head.
- Enucleation (husking). There is no radical effect on the pancreas during this surgical procedure, since the neoplasm in this case is simply “picked off” from the surface of the damaged organ.
- Pancreatoduodenal resection. This operation is considered the most radical, since the pancreatic adenoma is removed by resection of the entire organ and part of the duodenum. This type of surgical intervention is prescribed only for adenomas that have reached large sizes and have begun to compress the duodenum.
When surgical treatment of pancreatic adenoma is performed, directly during the operation, the specialist takes a biopsy material for further histological examination. This tactic, used during surgical interventions to remove an adenoma from the pancreas, makes it possible to exclude the onset of the oncological process in the tumor structure.
Radiation and chemotherapy are not used for pancreatic adenoma, as they are completely ineffective, but patients with a partially or completely removed digestive organ are necessarily prescribed drug therapy. It consists of constantly taking enzymatic preparations that restore the functioning of the digestive system, and is selected individually for each specific patient.
Life prognosis for pancreatic adenoma
While the adenoma in the pancreas is benign, it has a calm, favorable course and the best prognosis for cure. The survival rate of patients in this case is very high - 9 out of 10 operated patients who were diagnosed with a benign adenoma fully recover.
Postoperative complications and recurrence are considered very rare in clinical practice.
To completely eliminate them, doctors observe the operated patients for a year, after which the disease is considered completely cured.
A worse prognosis for pancreatic adenoma occurs if the sick person refuses surgery. In this case, despite the benign nature of the tumor, there is a real threat of developing serious complications.
Namely:
- the beginning of the process of malignancy;
- development of obstructive jaundice;
- the appearance of obstruction in the upper intestines.
Important! Despite the fact that the treatment of pancreatic adenoma was carried out successfully, patients with a history of this disease will need to monitor their health and follow a diet for the rest of their lives.
Ivanov Alexander Andreevich, general practitioner (therapist), medical observer.
Source: https://onkolog-24.ru/chem-opasna-adenoma-podzheludochnoj-zhelezy-i-kak-ee-lechit.html
Cost of treatment
The cost of treating pancreatic tumors is discussed in detail in the table below.
| Procedure name | Cost in rubles |
| Ultrasound of the abdominal organs | 2000–2100 |
| Consultation with a gastroenterologist | 1800–2000 |
| Ultrasound of the pancreas | 950–1000 |
| Study (histology) of biopsy specimens of the stomach and intestines | 2300–2400 |
| MRI of the organ | 5500–6000 |
| Alpha-amylase level determination | 270–300 |
| Determination of lipase level | 350–400 |
| Total gastrectomy | 120000 |
| Determination of pancreatic alpha-amylase | 330–350 |
| Determination of alpha-amylase in urine | 250–300 |
| Distal pancreat resection | 75000 |
| Pancreaticoduodenectomy | 130000 |
| Fecal analysis for pancreatic elastase-1 content | 2000–2100 |
| Determination of pancreatic enzymes in the blood | 950–1000 |
| Oncologist consultation | 2000–2500 |
| Enucleation | 95000 |
| Blood biochemistry | 1500 |
| Resection of the organ head | 68000 |
| Median resection | 134000 |
| MRI of the abdominal cavity | 8500 |
| Needle biopsy of an organ | 9000 |
| Contrast during MRI | 5500–6000 |
| Determination of pancreatic alpha-amylase in urine | 270–300 |
| Determination of enzymes in urine | |
| X-ray endovascular artery embolization | 50000 |
If we evaluate the dynamics of the presented prices, then restoring the normal functioning of the pancreas requires large expenses, so it is best to take timely preventive measures to prevent complications.
Treatment options
Often, at the beginning of treatment, medications are prescribed to normalize the concentration of insulin in the body. This approach eliminates most of the symptoms that occur with pancreatic dysfunction.
On this topic
- Digestive system
Can I drink water before a colonoscopy?
- Olga Vladimirovna Khazova
- December 3, 2020
If the tumor continues to grow or cystadenocarcinoma is detected during the examination, the problematic tissue is removed using the following methods:
- Resection. Provides complete removal of problem areas of the pancreas.
- Enucleation (husking). The method allows you to remove only cystadenoma.
- Distal resection. During the operation, the affected areas of the pancreas and part of the duodenum are removed.
- Pancreatoduodenal resection. The operation involves excision of the head and pacreatoduodenal zone of the pancreas.
- Laparoscopy. It is prescribed if a tumor occurs in the tail of the pancreas.
Radical methods are used if there are appropriate indications. If the tumor is inoperable or small in size, transperitoneal drainage of the problem area is prescribed.
In this case, a special catheter is inserted into the cystic cavity, with the help of which the contents of the tumor are sucked out. This approach makes it possible to reduce the size of the tumor, reduce the intensity of general symptoms and the degree of compression of neighboring organs.
In case of cystadenoma infection, extraperitoneal drainage is prescribed. A different approach is less commonly used, which involves placing an anastomosis in the area between the cyst and the stomach or intestinal loop. After completion of the procedure, the contents are removed from the cystic cavity through the indicated organs.
Signs
When the pancreas swells, active enzymes and breakdown products are released into the circulatory system and lead to poisoning of the body.
First of all, swelling occurs during inflammation, as evidenced by pain. The inflamed organ sharply increases in volume, its tissues become very dense. Quite large nerve trunks pass through the pancreas and their compression is the cause of acute and increasing pain. Nerve endings are also involved in the pathological process, which increases pain.
The person experiences great discomfort, expressed by acute girdling pain. Analgesics help little in this case. First of all, the patient looks for the most comfortable position, in which the pain is slightly dulled. Most often this is a sitting position with the body slightly tilted forward.
The entry of toxins into the blood causes an increase in temperature in the human body. The skin turns pale, general weakness and cold sweat appear. Poisoning provokes uncontrollable vomiting, and it does not bring relief. This is perhaps the main distinguishing feature of pancreatitis from other inflammatory diseases of the digestive tract.
In children, swelling of the pancreas and intoxication of the body are especially dangerous. It is necessary to closely monitor the child’s nutrition and condition during the introduction of complementary foods, teething and during adolescence.
When conducting an ultrasound examination, the pancreas with edema is greatly increased in size, its echogenicity is reduced and the degree of signal reflection decreases. Similar signs of pancreatic edema are observed in the acute period of pancreatitis.
Repeated cases of illness indicate the presence of a chronic disease. Periodic inflammation of the pancreas is each time accompanied by swelling. The organ changes its size and structure. The channels for the outflow of pancreatic juice expand and bend. The parenchyma of the gland thickens to the point of solidity and becomes nodular.
A sufficient amount of produced enzymes does not reach the intestines to digest food. The process of its breakdown, digestion and absorption of nutrients from it is disrupted. This leads to bloating, flatulence and diarrhea.
Another scenario is also possible, in a calmer form. After eating for some time, the patient feels heaviness in the stomach. Then comes weakness in the body, dizziness, and headaches. The person loses his appetite.
If the intestines do not receive the required amount of enzymes for a fairly long period, then the body does not have enough nutrients and vitamins, and this leads to weight loss.
Acute edematous pancreatitis
Acute edematous pancreatitis is familiar to a considerable number of people. Pathology occurs as a result of the inflammatory process. Patients themselves contribute to its occurrence. By eating improperly and abusing alcohol, people create favorable conditions for the development of the disease. Often the cause is problems in the duodenum. Gastritis provokes the disease.
With proper treatment, the disease is curable. A frivolous attitude towards lifestyle and nutrition becomes the cause of pancreatic necrosis, during which the pancreas becomes inflamed, enlarges, and edema appears. Edematous pancreatitis is a mild form of inflammation. The structure of the gland has a lobular appearance; foci of necrosis and exudate may occur in the abdominal cavity.
- Fried or fatty foods;
- A sharp transition from lean foods to fatty foods;
- Failure to comply with the gradual transition to the usual regimen after dietary nutrition;
- Toxic drugs;
- Change of basic food products (to spicy unusual foods);
- Alcohol consumption;
- Ingestion of toxic substances into the body.
Doctors say that edematous pancreatitis often occurs due to problems in the digestive system, due to improper food intake, a sudden diet break, or alcohol consumption. Some patients mistakenly talk about the relationship between microbes and the appearance of edema, but the cause of the inflammatory process and swelling is spasm and disturbances in digestive secretion.
Pancreatic enzymes are very aggressive and long-term exposure causes destructive processes in the body. It is necessary to identify swelling in time and begin treatment, avoiding necrosis. Edematous pancreatitis also affects other areas responsible for the endocrine system. For this reason, the secretion of enzymes decreases, and impaired synthesizing processes of glucagon and insulin lead to diabetes mellitus.
Symptoms and specifics of edematous pancreatitis
Acute edematous pancreatitis is inflammation of pancreatic tissue without signs of necrosis, resulting from increased production of enzymes.
This pathology in most cases is caused by a bacterial infection. The disease is diagnosed mainly in working age (30-60 years).
In recent years, the number of patients with pancreatitis has doubled, which is associated with consumption of alcohol, fast food and smoking.
Acute edematous pancreatitis is inflammation of pancreatic tissue without signs of necrosis, resulting from increased production of enzymes.
Causes
In 90% of cases, this pathology develops against the background of alcohol abuse. Ethyl alcohol has a toxic effect on the organ, enhancing the production of enzymes. The latter begin to digest the gland, which causes tissue swelling. Other common causes of pancreatitis are:
- hyperparathyroidism (excessive production of parathyroid hormone by the parathyroid glands);
- cholelithiasis;
- cholecystitis;
- irrational use of medications (tetracyclines, estrogens, systemic corticosteroids, thiazide diuretics);
- operations;
- injuries (bruises);
- mumps (viral infection of the salivary glands);
- enterovirus infection;
- infection of the body with mycobacteria and campylobacteria;
- developmental anomalies;
- cystic fibrosis (damage to the exocrine glands);
- hepatitis (liver damage);
- combined infectious inflammation of the stomach and small intestine;
- circulatory disorders;
- high levels of calcium in the blood;
- errors in nutrition (violation of the regime, excess of spicy, fatty and fried foods in the menu, overeating);
- smoking.
Pancreatitis may be a consequence of toxic substances.
Symptoms
If a person has developed an edematous form of inflammation of the pancreas, then the following signs are possible:
- Pain. Intense and constant. It is felt in the hypochondrium on the left, right, or encircles. Lasts several hours or days. Does not disappear when using antacids. Radiates to the shoulder, back and shoulder blade on the left. Dull or cutting.
- Increased body temperature. It is a response to the penetration of microbes. The temperature rises to +38…+39ºC. Indicates that the body is intoxicated.
- Chills.
- Lack of appetite. The reason is insufficient supply of enzymes to the duodenum and, as a result, difficulty in digesting food.
- Vomit. It can be indomitable. Vomit contains bile. Does not bring relief to a sick person.
- Frequent heartbeat. Pulse exceeds 80 beats/min.
- Skin that is cold and damp to the touch.
- Jaundice color of the skin and sclera of the eyes.
- Reduced blood pressure. Severe hypotension indicates fluid loss and shock.
- Frequent, loose stools. Occurs as a result of stagnation of enzymes in the organ.
- Bluish spots in the face, neck or navel.
- Muscle tension on the left side.
- Feeling of abdominal distension.
- Bloating.
- Belching.
- Hiccups.
- Dry mouth.
- Dyspnea. It results from loss of electrolytes through repeated vomiting.
- Weakness.
- Headache.
With pancreatitis, not all of the listed symptoms may be present.
Analyzes
If you suspect acute pancreatitis you will need:
- general and biochemical blood tests;
- general and biochemical urine tests;
- stool examination;
- ionogram.
With pancreatitis, leukocytes, amylase, lipase, C-reactive protein, glucose, urea increase in the blood, and ESR also increases. During an acute inflammatory process, the following decreases: total protein, hematocrit, albumin, globulins, concentration of magnesium, calcium and potassium. In acute pancreatitis, the amylase content in the urine increases.
Differential diagnosis is carried out with other pathologies of the digestive organs (cholecystitis, peptic ulcers, colitis, Crohn's disease, appendicitis), as well as diseases of the genital organs.
Treatment
Treatment for acute pancreatitis is complex. It begins after consultation with a gastroenterologist. Therapy is aimed at relieving edema, normalizing the outflow of pancreatic juice and bile, eliminating symptoms and preventing complications (pancreatic necrosis, abscesses, cysts).
Basic principles of drug therapy
For acute pancreatitis, the following medications are used:
- Antispasmodics (No-shpa, Drotaverine). These drugs eliminate pain by relaxing the muscles of the organ wall.
- Anesthetics (Novocaine). They are used during blockades in the presence of severe pain.
- Proton pump inhibitors (Omez, Pariet). They block the substance responsible for the formation of hydrochloric acid.
- Antacids (Gaviscon, Phosphalugel).
- Saline and protein solutions.
- Antibiotics. Prescribed by injection or in tablet form. The drugs of choice are cephalosporins, carbapenems, fluoroquinolones and penicillins.
- Analgesics (Tramadol, Analgin-Ultra).
- Proteinase deactivators (Aprotex).
- Diuretics (Lasix).
- Plasma replacement and perfusion solutions (Reopoliglyukin);
- Antipyretics (Panadol, Efferalgan). Indicated for fever above 38ºC.
When gallstones are detected, medications are used to dissolve them. After pain relief, enzymes (Pangrol, Festal, Creon) are often prescribed.
They are contraindicated in the acute stage of the disease. In case of acidosis (pH shift to the acidic side), treatment with alkaline solutions is possible.
Traditional medicine methods
Traditional medicine cannot replace hospital treatment. Their inept use can cause harm and cause complications. They are used with the permission of a gastroenterologist. For acute pancreatitis, the following can be used:
- infusion based on yarrow, immortelle, calendula, chamomile, string, St. John's wort and sage;
- decoction of barberry bark;
- decoction of golden mustache;
- propolis;
- cranberries mashed with honey;
- beans;
- oatmeal jelly;
- fresh potato juice;
- sauerkraut brine.
Traditional medicine cannot replace hospital treatment.
You can prepare an infusion based on elecampane, mint and string. To do this, you need to take 1 tsp of dried herbs. and pour the mixture with 400 ml of boiling water. The infusion takes 3-4 minutes to prepare. This product should be taken 1/3 cup 2 times a day before meals after preliminary filtration.
Consuming compote for pancreatitis has a beneficial effect on the pancreas.
Surgical
After hospitalization of a person with acute pancreatitis, the doctor may raise the question of surgical intervention. The most frequently performed types of operations are:
- removal of stones;
- drainage (removal of fluid);
- resection (partial removal of an organ);
- cystogastrostomy (anastomosis).
With the edematous form of pancreatitis, radical treatment is rarely required. It is indicated in case of development of purulent complications or concomitant cholelithiasis. Endoscopic operations are most often performed. Their feature is low trauma and the ability to visualize the organ on the screen through a tube with a camera. All operations are performed within the walls of the hospital.
Diet
In the first 2-3 days after the onset of an attack of pancreatitis, table No. 0 is prescribed. This means that the patient needs to fast. In this condition, you can drink water without gases, rosehip decoction and jelly. The amount of fluid consumed should be 2-2.5 liters per day. On days 3-5 from the onset of pancreatitis, diet No. 5 is prescribed.
It is allowed to eat liquid porridges (with the exception of wheat), low-fat soups, dried bread, fermented milk products, weak tea, low-fat fish, mashed potatoes, cereals, baked and boiled vegetables, sweet fruits and steam omelettes.
In the first 2-3 days after the onset of an attack of pancreatitis, table No. 0 is prescribed. This means that the patient needs to fast.
Therapeutic nutrition for pancreatitis involves excluding from the diet fatty foods, sweets with rich cream, baked goods, coffee, chocolate, sparkling water, pickles, raw vegetables, alcohol and mushrooms.
What to do if your legs begin to swell
With pancreatitis, the leg sometimes swells. This indicates the development of complications (thrombosis, circulatory disorders, compression of the portal vein by the cyst). In this case, diuretics (Furosemide, Lasix) or surgical removal of the cyst may be prescribed.
Complications
If acute pancreatitis is not treated in a timely manner, the following consequences are possible:
- pancreatic necrosis;
- sepsis (blood infection by bacteria and their toxins);
- shock;
- renal and liver failure;
- aseptic or purulent lesion of the abdominal wall;
- inflammation of the pleura;
- respiratory failure;
- shock lung;
- collapsed lung;
- multiple organ failure;
- encephalopathy (brain damage due to chronic lack of oxygen);
- depression;
- psychosis;
- thrombosis of large vessels;
- suppuration with the formation of abscesses;
- formation of cysts;
- bleeding;
- diabetes;
- jaundice;
- anemia (decreased levels of red blood cells and hemoglobin);
- drop in blood pressure;
- formation of fistulas between the pancreas and the stomach or intestines;
- tumors.
Complications of pancreatitis can be early (in the first days of the disease) and late (develop after 1-2 weeks or later).
Development of oncology
A serious complication of acute pancreatitis is the formation of a benign or malignant tumor. This happens when gland cells degenerate. This pathology develops slowly in people who do not follow treatment recommendations.
A serious complication of acute pancreatitis is the formation of a benign or malignant tumor. This pathology develops slowly in people who do not follow treatment recommendations.
Necrosis
Edematous pancreatitis can be complicated by necrosis (death) of pancreatic tissue. Pancreatic necrosis develops. The mortality rate for this pathology reaches 30-80%. Most often, tissue necrosis is preceded by the consumption of large amounts of alcohol. Pancreatic necrosis can be fatty (with increased activity of the lipase enzyme), hemorrhagic (with impaired microcirculation) and mixed.
Tissue necrosis in pancreatitis is characterized by severe pain, uncontrollable vomiting not associated with food consumption, increased sensitivity of the skin in the projection of the organ, signs of vascular and respiratory disorders. Pancreatic necrosis often leads to abscess, phlegmon (spread purulent melting of tissue) and fibrosis (overgrowth of connective tissue) of the gland.
Massive cell death causes enzymatic deficiency.
Cyst
Pseudocysts in pancreatitis are formed due to incomplete resorption of necrotic tissue. As a result, a capsule and connective tissue are formed, inside which pus or other secretion is located. Cysts form in the body, head or tail of the pancreas. Cysts up to 5 cm in size may not cause symptoms.
Formations localized in the area of the ducts of the organ are prone to spontaneous resorption. Large cysts are manifested by severe pain, which soon decreases. There is a typical period when a person experiences an imaginary improvement in well-being after acute pancreatitis.
Large cysts can compress surrounding tissue and rupture. In the latter case, the pain syndrome intensifies. When the ureters are compressed, dysuria in the form of urinary retention or pain is possible. Sometimes cysts develop intestinal obstruction.