Myocardial infarction is the death of a section of the myocardium, which occurs as a result of complete or partial cessation of blood supply to a certain area of the heart muscle. Every adult should know the main symptoms of this disease, since it is very important to respond in time and provide assistance to the patient. So, the following signs indicate an acute heart attack:
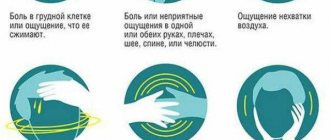
- The appearance of intense pain behind the sternum, in the left half of the chest, left arm, left shoulder blade, left half of the neck and lower jaw. These painful sensations have certain characteristics: they can occur both during exercise and in complete calm; last for tens of minutes; difficult to remove with nitroglycerin; have a wave-like character (either increasing or decreasing).
- Anxiety and fear of death. The patient may rush around the room and not find a place for himself.
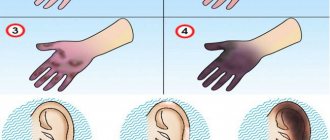
- Marked weakness. Sometimes this symptom comes first if a heart attack develops without intense pain. This happens rarely and mainly in patients with diabetes.
- Cold sweat, paleness.
- Nausea.
Signs of a heart attack may be atypical and resemble an asthmatic attack or acute pancreatitis, which causes intense abdominal pain, vomiting, and flatulence. Therefore, it is necessary to evaluate all the described symptoms in a complex manner, always taking into account the presence of heart attacks in the patient in the past. If a stranger becomes ill, you should definitely find out if he has heart problems.
Not every case of myocardial ischemia (this is the scientific name for oxygen starvation of cardiac muscle cells) leads to a heart attack. Experts have developed an intermediate diagnosis of “acute coronary syndrome”, which is given to any patient with coronary heart disease when certain objective and subjective symptoms appear:
- chest pain that does not go away on its own or after taking 3 tablets of nitroglycerin within 20 minutes;
- characteristic irradiation of pain that can radiate to the left arm, scapula, interscapular region, neck, lower jaw;
- pale skin, cold sweat, weakness (these symptoms signal impending cardiogenic shock);
- fear of imminent death;
- shortness of breath that occurs at rest;
- changes in blood pressure levels;
- the appearance of various kinds of arrhythmias, etc.
The first signs of myocardial infarction
The onset of a myocardial infarction is signaled by the following symptoms:
- sudden or paroxysmal severe pain in the chest, lasting more than half an hour (up to 2 hours);
- the pain is burning, tearing, stabbing in nature, usually occurs after physical activity (sometimes immediately after sleep) and does not become less pronounced even after a state of rest;
- the pain is not eliminated (as during an attack of angina) by taking Nitroglycerin and after taking the pill (and even a repeat dose), a person may feel only a slight decrease in pain;
- severe weakness (up to pre-fainting or fainting);
- nausea;
- pain sensations radiate to the left (sometimes to the right) arm, neck area, interscapular area, teeth, scapula, lower jaw;
- severe pallor;
- the appearance of cold and sticky sweat on the skin;
- pronounced anxiety and fear of death.
Approximately half of patients with myocardial infarction experience signs of heart failure: difficulty breathing, shortness of breath, nonproductive cough, arrhythmic pulse, atrial fibrillation, sudden short-term cardiac arrest.
Video: What are the symptoms of myocardial infarction?
In some patients, the heart attack occurs in atypical forms. The following symptoms may indicate the occurrence of such an attack:
- pain in the left hand or little finger of the left hand, in the cervicothoracic spine, lower neck or lower jaw, scapula;
- pain localized in the abdomen and dyspepsia;
- suffocation and shortness of breath;
- shortness of breath with severe weakness and rapid increase in edema;
- dizziness with nausea, darkening of the eyes and a sharp decrease in blood pressure;
- dizziness with confusion, speech disturbances, nausea, vomiting and paresis of the arms and legs;
- discomfort in the chest area (without pain) with increased sweating and severe weakness.
In a number of clinical cases, a heart attack is represented by a combination of symptoms of several atypical forms (for example, cerebral and arrhythmic). Such manifestations of this life-threatening condition significantly complicate the detection of myocardial necrosis and aggravate the prognosis of the outcome of the emergency condition considered in this article.
How to recognize myocardial infarction
The symptoms of an upcoming attack are unambiguous and make it possible to identify the problem in 70% of all cases. According to clinical guidelines developed for doctors, myocardial infarction often occurs suddenly. But in some cases the disease develops gradually, over several days and weeks.
Pre-infarction period
If the patient has previously experienced angina attacks, then in the pre-infarction period they often change their character: they become more frequent, can change or expand the area of irradiation, occur with less load, and become more intense. In the pre-infarction period, not only angina pectoris can occur with any exertion, but also at night, at rest. The worst thing is long-term attacks of heart failure (10-15 minutes), accompanied by a strong reaction of the autonomic system, arrhythmias. This type of angina is called “unstable.” With improper treatment or the natural course of the disease, it is a harbinger of myocardial infarction.
In some cases, the pre-infarction period may be accompanied by nonspecific symptoms: fatigue, general weakness, etc. In this case, a heart attack can be suspected only after an ECG.
Table No. 1. Harbingers of the onset of an attack
| Symptom | Short description |
| Chest pain | An anginal attack - an attack of squeezing, pressing, burning pain - is one of the main signs of a typical form of myocardial infarction. The intensity of pain can vary from minor to unbearable. The most typical feeling is squeezing or pressure behind the sternum. The attack is not completely stopped with nitroglycerin or sometimes with repeated use of any other narcotic analgesics. Irradiation of pain to the left arm, left shoulder, throat, epigastrium, lower jaw, etc. may also be observed. Painful attacks come in waves and last from 20 minutes to several hours. |
| Excessive sweating, paleness | An anginal attack is often accompanied by agitation, anxiety and various autonomic disorders, including increased sweating |
If a person experiences one or more of the above symptoms, they should receive first aid immediately.
There are also atypical forms of myocardial infarction, which have their own symptoms.
- Astamatic. Usually observed in senile or elderly patients, often against the background of chronic heart failure. Painful attacks may be mild or absent altogether, and the only sign of a developing heart attack is an attack of cardiac asthma or pulmonary edema. In this case, the heart attack will develop as acute left ventricular failure.
- Abdominal. This form is characterized by pain in the upper abdomen and symptoms of dyspepsia - vomiting. nausea, flatulence, sometimes gastrointestinal paresis. This option is similar to the development of an acute gastrointestinal disease, therefore, if an “acute abdomen” is diagnosed, an ECG procedure must be performed.
- Arrhythmic. The pain syndrome may be smoothed out or completely absent. The possible development of a heart attack is indicated by heart rhythm disturbances present in the clinical picture.
- Cerebrovascular. This option is usually observed in elderly patients. It can manifest as fainting, dizziness, nausea, vomiting, sometimes signs of a transient cerebrovascular accident, and sometimes have the character of a severe stroke.
Emergency care before the ambulance arrives. What to do?
If you suspect a myocardial infarction, you should immediately call an ambulance and provide the dispatcher with the following information:
- about suspected myocardial infarction;
- describe the symptoms observed in the victim;
- ask for a team of cardiologists and resuscitators to arrive.
Before the arrival of specialists, it is necessary to immediately begin carrying out emergency assistance measures:
- Help the patient find a comfortable position: lay him on his back and place a cushion under the back of his head, or give him a semi-sitting position by placing a pillow or folded clothes, a blanket, etc. under his back.
- Unbutton and remove clothing or accessories (scarf, belt, tie, etc.) that interfere with free breathing, and ensure the most comfortable temperature conditions (for example, open a window in hot weather or cover with a blanket in the cold season).
- Explain to the victim that he must remain still and remain emotionally calm. You need to talk to a person in the state of an attack of myocardial infarction in an even, firm and calm tone, and you should not make sudden movements that could frighten him. If the patient has manifestations of motor agitation, then give him a sedative (tincture of valerian, motherwort, Valocardin, etc.).
- Measure blood pressure: if it is not higher than 130 mm Hg. Art., then give the patient a tablet of Nitroglycerin or another drug available under the tongue, the active component of which is organic nitrates (for example, Isoket, Nitrocor, Nitrogranulong, Izodinit in the form of sublingual tablets or spray). Before the doctors arrive, Nitroglycerin should be taken again 1-2 times (that is, 2-3 tablets can be given in total). If after taking the first dose of this drug the victim has a severe throbbing headache, then the subsequent dose should be halved. And if after taking Nitroglycerin there is a sharp decrease in blood pressure, then repeated use of this nitrate-containing drug should be discontinued. When using Nitroglycerin analogues (for example, medicine in the form of Izoket spray), each dose should be 0.4 mg. Before injecting the product, the first dose should be released into the air, as it may not be complete. After this, the patient must take a deep breath and hold his breath, then an injection is performed, the mouth is closed, and breathing for 30 seconds should be carried out only through the nose.
- To prevent blood clots, thin the blood and reduce the load on the heart muscle, give the patient up to 300 mg of crushed Aspirin.
- You can put a mustard plaster on the area where the pain is localized. Constantly monitor it so that the skin does not burn.
- Count the patient's pulse, and if he does not have a history of bronchial asthma, and the heart rate does not exceed 70 beats per minute, then give him 25-50 mg of Anetolol or a dose of any other beta-blocker (for example, Bisopropol, Propranolol, Nebivolol and etc.). This measure will reduce the risk of arrhythmia and sudden death, limit the area of necrosis of cardiac muscle tissue, protect the myocardium from toxic effects and increase its tolerance to stress.
Sometimes during an attack of myocardial infarction the patient faints. The following measures can help him in such situations:
- lay the patient on his back and place a cushion under his shoulders;
- remove dental structures from the mouth (if present);
- tilt the victim's head back or turn him to one side if the patient begins to vomit;
- ensure prevention of aspiration of vomit.
Remember! If a patient with signs of myocardial infarction has stopped his heart and breathing, or his breathing movements have become intermittent (agonal), then he should immediately begin performing cardiopulmonary resuscitation measures - chest compressions and artificial respiration.
Before resuscitation begins, a precordial blow is performed - 2 strong and short blows are applied to the sternum area (at the border of the middle and lower third) from a height of 20 - 30 cm. After their execution, the pulse is immediately felt. If it does not appear, then cardiopulmonary resuscitation (indirect cardiac massage and artificial respiration) is performed:
- pressing on the heart area with a frequency of 75 - 80 per minute;
- 2 breaths into the patient’s mouth after every 15 to 20 chest compressions.
The duration of such actions should be at least 10 minutes.
Principles of first aid
At the first signs of an attack, you need to call a medical team and begin providing assistance for myocardial infarction, which is performed according to certain algorithms.
First aid for myocardial infarction consists of maintaining or restoring the blood supply functions to the damaged heart muscle.
If a person is conscious, the algorithm of actions should be as follows:
- The patient should be seated so that the upper part of the body is much higher. This position will reduce the load on the heart muscle.
- Give the patient Valocordin or any other sedative. This can reduce heart contractions.
- If the attack began at home, provide free access to fresh air and free the victim from oppressive clothing and accessories. These actions must be performed quickly if the attack is accompanied by an acute manifestation of suffocation.
- Before doctors arrive, regularly record your blood pressure and pulse rate. These data will allow doctors to quickly navigate the stage of diagnosing the disease and provide emergency care;
- Give the patient 2 aspirin tablets and ask them to chew. This drug actively thins the blood, and chewing it accelerates the effect.
- If a person experiences severe pain, painkillers may be used.
If patients have deviations from normal blood pressure, pulse and respiration levels, the following action algorithm should be used:
- If blood pressure is low and the pulse is weak, it is better to place the patient so that the head is lower than the body.
- If the patient has severe shortness of breath, he should be seated with his legs elevated.
- Nitroglycerin cannot be used at low blood pressure, as this can lead to complete cardiac arrest.
If, based on obvious signs, you suspect a heart attack, you need to act in this order:
- Seek medical help as soon as possible;
- Ask people around you (passers-by, colleagues, relatives) to help, tell them in detail about the manifestations of the attack;
- Sit down, if possible, take a reclining position;
- Ask those around you for the necessary medications.
- Try to remain still.
Note!
When calling doctors, be sure to report suspicions of a heart attack so that the dispatcher can send a car equipped with the necessary medical resuscitation equipment.
These simple steps to eliminate the first symptoms of myocardial infarction at the prehospital stage will help you wait for doctors with minimal consequences for the body.
Critical situations
If first aid for myocardial infarction is provided correctly, doctors will carry out the necessary diagnostics and prescribe appropriate treatment.
But what to do if acute coronary syndrome is accompanied by loss of consciousness of the patient, cardiac arrest and respiratory arrest?
In case of acute myocardial infarction, it is important to restore the functioning of the heart muscle and bring the victim to consciousness before the ambulance arrives.
In this case, emergency resuscitation of the heart and lungs is necessary, which consists of artificial respiration and heart massage.
Note!
All emergency actions in case of ACS are performed when the victim is lying on a hard and flat surface, with his head thrown back.
With this algorithm of actions, it is important to follow a clear sequence:
- First of all, you need to hit the patient’s solar plexus area with the edge of your palm. This way you can restart a stopped heart muscle.
- If this technique does not help, emergency assistance is provided in the form of a standard massage to restore myocardial function. 15 intense pressures are performed in the chest area, then mouth-to-mouth breathing is restored. These emergency measures are carried out until the person regains consciousness or the entire pre-hospital period. In case of heart failure accompanied by coronary syndrome, these actions will help save the patient's life.
Note!
In case of heart attack syndromes, emergency care is carried out rhythmically so that the pressure imitates the heartbeat.
First aid for myocardial infarction. Algorithm of actions
Emergency care for a patient after the ambulance arrives is carried out in the following sequence:
- Relief of acute pain with the help of non-narcotic and narcotic analgesics (solutions of Analgin, Morphine hydrochloride, Omnopon, Promedol) in combination with a solution of Atropine sulfate. The drugs are administered intravenously for faster pain relief.
- Carrying out an ECG.
- If delivery of the patient to the intensive care unit is possible within the next 30 minutes, then the victim is immediately taken to the hospital.
- If such rapid transportation of the patient turns out to be difficult, then drugs to restore coronary circulation (Tenecteplase, Alteplase, etc.) are administered on site.
- The patient is transferred to the ambulance as gently as possible - a stretcher is used for this. During transportation, humidified oxygen is inhaled.
After the patient is delivered to the intensive care unit, neuroleptanalgesia is administered to ensure complete relief of pain. For this purpose, medications such as Talamonal or a combination of Droperidol and Fentanyl are used. If the desired analgesic effect is not achieved, the patient is placed under inhalation anesthesia, which is provided by a mixture of oxygen and nitrous oxide.
Further, to provide first aid to the patient, the following drugs are prescribed:
- organic nitrates: Sodium isosorbide, Nitroglycerin, Isoket or others;
- anticoagulants: Heparin, etc.;
- antiplatelet agents: Acetylsalicylic acid, Cardiomagnyl, etc.;
- beta-blockers: Propranolol, Inderal, Obzidan, Anaprilin;
- ACE inhibitors: Enalapril, Ramipril, etc.;
- sleeping pills and sedatives: Temazepam, Diazepam, Triazolam, etc.;
- antiarrhythmic drugs: Lidocaine, Amiadron, Novocainamide, etc.
The treatment plan is drawn up individually for each patient. If necessary, other medications may be added to it.
To restore coronary circulation to a patient with severe forms of heart attack, the following surgical operations can be performed:
- balloon angioplasty;
- coronary artery bypass grafting.
Emergency care for a patient
After the ambulance team has arrived, they provide emergency medical care for acute myocardial infarction. Algorithm of emergency care for acute myocardial infarction:
- To eliminate severe pain, use non-narcotic or narcotic analgesics, for example, a solution of Analgin, Morphine, Promedol in combination with Atropine. Medicinal solutions are injected into a vein to make the pain disappear faster;
- An ECG is performed to assess the functionality of the heart;
- Immediately hospitalize the victim;
- If it is not possible to quickly transport the patient to a hospital, then the patient is administered drugs to normalize blood circulation through the blood vessels of the myocardium. For this purpose, Tenecteplase, Alteplase, etc. are used;
- The patient is transferred on a stretcher to the car. On the way to the hospital, oxygen therapy (supply of humidified oxygen through a nasal catheter) is given.
In the intensive care unit, neuroleptanalgesia (combined internal anesthesia) is performed, which allows you to completely relieve pain. For this purpose, use Talamanol or a combination of Droperidol and Fentanyl. If this method does not work and the pain does not go away, then inhalation anesthesia is used.
The following medications are used during therapy:
- Organic nitrates : Isosorbide, Nitroglycerin, Isoket, etc.;
- Drugs that inhibit the activity of the blood coagulation system, preventing the formation of a blood clot, for example, Heparin;
- Antiplatelet agents : Acetylsalicylic acid, Cardiomagnyl;
- B-blockers: Propranolol, Inderal, Obzidan;
- inhibitors : Enalapril, Ramipril;
- Sedatives: Temazepam, Diazepam, Triazolam;
- Antiarrhythmic drugs : Lidocaine, Amiadron, Novocainamide.
The treatment regimen for each patient is drawn up separately by the attending physician. If necessary, treatment can be supplemented with other drugs. In severe cases, balloon angioplasty (changing the shape of the vessel at the site of compression) or coronary bypass surgery (restoring blood flow in the arteries of the heart by bypassing the site of narrowing using shunts) is performed to restore coronary circulation.
Actions of a patient during a heart attack
Patients with coronary artery disease who are at risk of developing a heart attack should know not only the first signs of this dangerous condition, but also the algorithm of actions at the onset of such an attack:
- remain calm and take a “reclining” or “sitting” position;
- inform others about the onset of an attack and the need to take medications;
- if possible, call an ambulance yourself, informing the dispatcher about the development of a heart attack;
- try to move as little as possible;
- if you have medications, take 2-3 crushed tablets of Aspirin, Valocardin and Nitroglycerin;
- Describe symptoms to ambulance workers.
Video: First aid for yourself during a heart attack
After admission to the intensive care unit, the patient must follow all the doctor’s recommendations regarding medication, gradual expansion of physical activity and diet.
The importance of first aid during a heart attack
In case of competent assistance, subsequent complications can be prevented, and sometimes, a life can be saved. If adequate measures are taken in a timely manner within half an hour after the occurrence of a heart attack, the likelihood of a positive outcome will increase significantly, and the risk of serious changes in the body, on the contrary, will decrease.
Actions of the medical team during a heart attack
First aid for complications of myocardial infarction
In the absence of breathing, pulse in the vessels of the neck and graying of the skin, it is necessary to call emergency medical assistance, if this has not been done before, and immediately begin resuscitation measures. According to new recommendations from the American Heart Association, they should be carried out in the following sequence:
- Indirect cardiac massage. Place the patient on a flat and hard surface (floor, asphalt, etc.). Place the base of one of your palms in the place where the ribs meet on the chest, place the second palm on top and apply rhythmic pressure with your body weight. In this case, it is necessary to ensure that the sternum drops sufficiently deep (preferably 5 cm). 100 such movements should be performed per minute. After 30 compressions, you should switch to artificial respiration.
- Artificial respiration. All measures must be done promptly: the patient throws back his head, pushes his jaw forward, opens his mouth and closes his nose, then completely clasps the patient’s lips with his lips and blows air into his mouth (in order to protect against infections, preferably through a handkerchief or mask). In this case, the chest of the person being resuscitated should rise. You need to take 2 such artificial breaths, and then return to cardiac massage.
- Resuscitation should be continued until the doctors arrive, without reducing the rhythm and observing the ratio of pressure on the sternum and inhalations - 30 to 2.
Read also: Rescue of a drowning person on water: rules
The criteria for the effectiveness of the described measures are the improvement of the patient’s skin color, the appearance of spontaneous breaths, and pulse. Resuscitation can be stopped only when the person begins to breathe on his own.
Resuscitators also recommend that if it is impossible to perform artificial respiration (lack of skills and protective equipment - scarves, masks), only perform rhythmic and intense artificial heart massage until the medical team arrives. It is worth noting that first aid for a heart attack, provided correctly and without delay, especially cardiopulmonary resuscitation, can significantly increase the patient’s chances of survival.
Poor nutrition, bad habits and constant habits are the three most important factors that can disrupt the heart function of even the healthiest person. is the disease that kills the most people worldwide every year (7.4 million in 2012), and myocardial infarction is its most severe complication.
First aid
To help the patient and prevent death, you need to know a certain algorithm of actions. If characteristic symptoms occur, you should immediately call an ambulance. In this case, it is important to report the presence of signs of a heart attack and ask to send a resuscitation team.
What can be done before the doctors arrive? As a rule, first aid for a heart attack comes down to the following manipulations:
- Lay or sit the patient down so that he is comfortable.
- Provide him with access to fresh air. To do this, you need to open the windows in the room, unfasten or remove his clothes and objects that limit his respiratory activity.
Calm the person down. Especially if he has attacks of fear and panic. At the same time, he is given sedatives (Valerian, Corvalol).- To relieve pain, you can give Nitroglycerin (prohibited for low blood pressure). It will not relieve the pain completely, but it will help you hold on until the ambulance arrives. In total, you are allowed to take up to 2-3 tablets of this drug.
- Measure blood pressure and pulse. If these indicators are normal, then painkillers or beta blockers (Atenolol) can be used. If blood pressure or pulse activity decreases, these drugs can cause cardiac arrest.
- To thin the blood, you should take Aspirin. The maximum single dose is no more than 300 mg.
- Warm heating pads are applied to the arms and legs, and mustard plasters are applied to the heart.
- If the patient has symptoms of cardiorespiratory arrest, chest compressions and artificial respiration should be performed.
It is important to take such measures within the first minutes after a heart attack. This significantly increases the patient’s chances of surviving and avoiding negative consequences.
The most common complications that occur are:
- Primary. They develop immediately after a heart attack. It can be:
- cardiogenic shock;
- fibrillation (cessation of activity) of the ventricles;
- pericarditis;
- hypotension (sharp decrease in blood pressure);
- rupture of the heart muscle. Such conditions lead to the death of the patient. This happens in more than half of the cases, even when the necessary revitalizing measures are carried out.
swelling of the lungs;
- thromboembolism;
aneurysm;
After carrying out the necessary manipulations, you should tell the doctors what exactly you did, as well as what medications and in what quantity you gave the patient.
What if this happened on the street?
It happens quite often when a person becomes ill outside the home, and in this case it is quite difficult to find the necessary medicine. If trouble occurs, then it is necessary to carefully check the victim’s pockets or bag; as a rule, people suffering from heart disease always carry such medications with them.
How to give medicine to a patient? The use of the above-described drugs occurs according to the following scheme: the first nitroglycerin tablet is placed under the person’s tongue, and after 6 minutes the second is given, provided that the pain has not decreased.
How to distinguish a heart attack from angina pectoris
The problem is relevant even for cardiologists. It is impossible to carry out differential diagnosis on your own. Both processes are determined only approximately.
Specific signs of necrosis of cardiac structures:
- Acute pain. The discomfort is extremely intense. It radiates to the shoulder blade, back in general, neck, jaw, forearm, moves all the way to the hand. The force is so great that the patient may lose consciousness.
There is also a more insidious option. When the discomfort is moderate or mild, but obsessive, lasts more than half an hour. You need to remember: with angina, the pain is always pronounced, but not unbearable, lasting up to 30 minutes maximum.
Read also First aid for road traffic accidents
In any case, the first action when persistent heart pain is detected should be to call an ambulance. You won’t be able to delimit states on your own.
- There is an effect of Nitroglycerin. But against the background of myocardial infarction it is incomplete, partial. The discomfort subsides, but does not go away. An attack of coronary insufficiency responds better to medications, so stable correction of the patient’s condition is possible. You need to listen carefully to how you feel.
- Severe arrhythmia. It occurs more often with necrosis of the heart muscle. Accompanied by typical disorders: freezing in the chest, turning over, tying a knot, missing blows. These are non-specific moments, so it is impossible to say exactly what caused it.
- Fainting conditions. Against the background of a heart attack, they are also more common.
- Severe shortness of breath. Inability to take in air, problems with the natural process. Panic and a feeling of fear are growing.
- Increased sweating. Almost never occurs during an attack. Against the background of necrosis, much more often. Speaks of a sharp drop in blood pressure and weakening of cardiac activity.
- Rate of progression. A heart attack is more aggressive and leads to health problems faster. In the fairer sex, it develops gradually, which is different from an attack of coronary insufficiency. In female patients, detection of pathology is easier.
In general, it is impossible to distinguish a heart attack from angina without special methods. And such differentiation is not of great importance at the prehospital stage.
In about 15% of emergency cases, there are no symptoms at all. The group at increased risk of developing a “silent” heart attack includes people over 50 years of age, patients with diabetes mellitus and arterial hypertension.
How to recognize a pathological condition?
Myocardial infarction is an acute manifestation of cardiac pathology known as coronary artery disease. It develops against the background of atherosclerotic lesions of the coronary vessels. In this case, complete or partial blockage of the heart arteries occurs.
As a result, blood circulation and nutrition of the heart muscle are disrupted. This condition leads to spasm and necrosis (death) of heart cells and their replacement with connective tissue. If the patient is not given immediate care, he may die.
General information about MI
What signs indicate the development of a heart attack? First of all, you should pay attention to the following symptoms:
- The occurrence of acute pain in the heart area. It has specific characteristics:
- appears abruptly;
- radiates to the left arm, shoulder blade, neck;
- lasts from several minutes to several hours;
- it cannot be removed with Nitroglycerin.
has an intense paroxysmal character;
With atypical manifestations, other signs may be added. For example, abdominal pain, attacks of nausea and vomiting, cough, dizziness and headache.
Most often, a heart attack occurs after the action of provoking factors. A heart attack can occur after physical overload, stress, emotional shock, overheating or hypothermia. It also develops as a result of alcohol or toxic (including drug) damage.
First aid to yourself
Algorithm of action for suspected necrosis of cardiac structures:
- Call an ambulance. Describe your own condition clearly, briefly and to the point. There is no need to embellish, let alone hide anything.
Brigades in Russia and the CIS countries are loaded to capacity, there are not enough doctors and even paramedics, so dispatchers are forced to rank situations by priority. The first to go are heart patients and children.
If you do not make clear the seriousness of the situation, there is a risk that you will have to wait for an ambulance for several hours. A heart attack does not tolerate such delays.
- Open a window or window. Acute necrosis of cardiac structures leads to the impossibility of adequate gas exchange.
The pulmonary artery and pulmonary vessels become stenotic (narrowed), hypoxia of all body tissues occurs due to a decrease in myocardial contractility.
If there is not enough oxygen in the atmospheric air, the situation will worsen. Cerebral ischemia and further progression of infarction are the most likely moments.
- Take a Nitroglycerin tablet, but only with your doctor's approval. The drug and its analogues partially help relieve pain.
It is not recommended to take Validol, Corvalol and phenobarbital-based pharmaceuticals as primary medications. They will not give a pronounced effect. Organic nitrates do not always act as desired.
Extensive heart attack is a contraindication to taking Nitroglycerin. Rapid development of arrhythmic disorders is possible. If there are no doctor’s instructions, then the best decision would be not to take anything until specialists arrive.
- Take a comfortable position. Horizontal orientation is associated with disruption of normal breathing. Asphyxia and other problems may occur. If you lose consciousness, vomit. Therefore, it is better to find a stable sitting position. The possibility of fainting is always taken into account.
- Remove constricting, tight clothing. Especially a collared shirt, T-shirt, etc. Compression of the carotid sinus, located in the neck, will lead to a reflex drop in heart rate. Given the current heart attack, this is almost guaranteed death.
- Calm down. An emergency condition is associated with the development of severe anxiety and fear. This is a so-called panic attack. At such moments, obsessive thoughts, mental and motor agitation arise.
You should call an ambulance if you have any suspicions. Signs of a heart attack in women are described here, and in men - here. False modesty costs lives. Neither heart attack nor angina can be treated at home.
Symptoms of myocardial infarction
The ability to orientate yourself in a timely manner and provide adequate support to the patient before the ambulance arrives greatly increases his chances of survival.
First aid for myocardial infarction should be provided immediately.
Algorithm of actions
- Immediately call an ambulance (in a conversation with the dispatcher, formulate the symptoms as clearly as possible, voice the suspicion of MI, so that a specialized cardiology or resuscitation team can respond to the call).
- Provide the patient with a semi-sitting position (the elevated position of the upper half of the body reduces the preload on the heart).
- Try to reassure the patient (emotional and physical stress increases the release of vasoconstrictors, which increases myocardial ischemia and increases its oxygen demand).
- Provide oxygen flow (open windows, doors, turn on air conditioning).
- Remove outer clothing and loosen all elements that compress the body (tie, belt, necklace, etc.).
- If possible, measure blood pressure and count pulse. For severe tachycardia, take 1 tablet of Anaprillin; for hypertension, take 1 tablet of Captopril.
- Give ASA (150-325 mg) or Clopidogrel (100 mg). The effect will occur faster if the tablets are chewed.
- Give 1 tablet sublingually. "Nitroglycerin." Repeat the dose every 5 minutes (but no more than 3 doses).
- Before the ambulance arrives, it is prohibited to take non-narcotic analgesics!
https://www.youtube.com/watch?v=He2ivwlDReo
If the patient suddenly loses consciousness, stops breathing and cardiac arrest occurs, it is necessary to perform cardiopulmonary resuscitation before the doctors arrive:
- position the patient lying on his back, tilt his head back, place a cushion under his neck, push out the lower jaw (prevention of obstruction of the airways with the tongue);
- check the pulse in the carotid artery;
- perform indirect cardiac massage and perform artificial respiration with a frequency of 30:2 if the procedure is performed by one person, or 15:1 if two people perform the procedure. Pressing should be done quickly (100 per minute), rhythmically and with sufficient force to ensure cardiac output;
- check every 2-3 minutes to see if a pulse appears.
The quality of first aid provided to a patient depends on many factors:
- knowledge of the person providing assistance, the algorithm of actions in case of a heart attack, the ability to perform resuscitation actions;
- time elapsed from the attack to the onset of actions;
- medication and instrumental support (tonometer, Nitroglycerin, Aspirin);
- the staffing of ambulance teams with the necessary equipment, medications, and personnel qualifications;
- distance from specialized cardiology departments.
There are also factors that aggravate the course of a heart attack, and thereby reduce the chances of success:
- age over 70 years;
- concomitant pathology (diabetes mellitus, obesity, kidney pathology, widespread atherosclerosis, hypercholesterolemia, hypertension);
- painless onset of ischemia or atypical clinical picture;
- extensive focus of necrosis (transmural MI) with cardiogenic shock;
- the occurrence of severe arrhythmias and cardiac conduction disorders.
A heart attack is a life-threatening condition that occurs as a result of an acute disruption of the blood supply to the heart muscle. This happens because an atherosclerotic plaque clogs one of the arteries. Blood supply stops and necrosis of heart tissue begins. The process develops in 20-30 minutes. If such a stage occurs and the person is not given help, this can lead to death.
Most often, a heart attack occurs in people suffering from organic lesions and heart disease, ischemia, atherosclerosis, and diabetes. Risk factors worsen with age. Symptoms of the condition vary slightly between men and women.
In men
Symptoms of a heart attack can be both typical and atypical, when the acute condition is confused with attacks of asthma, angina pectoris, or stroke. The correct diagnosis must be made by a doctor. Typical manifestations of a heart attack in men include:
- severe weakness;
- rapid heartbeat with signs of arrhythmia;
- chest pain, which can radiate to the left shoulder, collarbone, scapula;
- rapid and intermittent breathing;
- pallor of the face and body skin;
- cold clammy sweat;
- weakening and intermittency of the pulse;
- severe nausea or involuntary vomiting;
- a sharp drop in pressure;
- loss of consciousness, deep fainting.
Even if there are 2-3 signs of a heart attack, urgent medical attention is needed.
Among women
In women, the signs of a heart attack are somewhat different, so they are often confused with atypical ones and are not paid due attention. This can be fatal over time.
A female heart attack is characterized by the fact that pain and discomfort are localized mainly in the upper part of the body (jaw, neck, shoulders and upper back). Often the pain occurs in the epigastric region and is accompanied by sensations similar to severe heartburn. The condition is aggravated by weakness, sweating, and blood pressure may drop if it was normal or elevated before. If you seek help in time, you will be able to prevent the development of a heart attack and its consequences.
In addition to providing medications, first-aid care for myocardial infarction consists of a simple algorithm of actions. After calling the ambulance and waiting for the doctors, the following measures are carried out, the implementation of which can be carried out by others:
- Opening windows or turning on the air conditioner to ensure oxygen enters the enclosed space, which will improve blood flow and ensure normal physiological functioning of the body.
- It is important to help the patient sit down or lie down; support placed under the back of the head and upper back ensures elevation of the torso area, the legs are bent and the feet are placed on an elevation to facilitate blood flow and reduce the load on the circulatory system.
Effective first aid for myocardial infarction is a step-by-step action performed in strict sequence. It includes the following steps:
- Taking Aspirin (1-2 tablets) will thin the blood and dissolve a blood clot in the coronary artery; it is recommended to chew the tablets.
- Dosed intake of Nitroglycerin relieves pain due to rapid penetration into the body systems due to absorption.
Special first aid for myocardial infarction, provided before the arrival of the ambulance team, will normalize blood flow and neutralize the predicted dangerous consequences of an acute illness.
Myocardial infarction
A transferred acute myocardial infarction is accompanied by severe pain, difficulty breathing and cardiac arrest: emergency care provided when diagnosing it involves an algorithm of important steps. In case of acute heart disease, the functions of the heart should be restored; this is possible by performing artificial respiration and cardiac massage.
Calling a doctor is part of first aid at home for a heart attack. While waiting, you should try to distract the patient and move him to a sitting or lying position. In order to reduce the load on the circulatory system, it is necessary to position it so that the torso rises above the lower part of the body; for this, you can form a cushion from clothing and place it under your back. It is recommended to supplement the algorithm of actions for first aid for myocardial infarction by ensuring good ventilation of the room.
Nitroglycerin tablets (0.5 milligrams) dissolve, the capsule should be bitten without swallowing, which will make it possible to reduce the level of pain.
At the initial signs of panic behavior, it is important to provide the patient with sedatives, but it is recommended to limit their use. Prompt emergency care for diagnosed myocardial infarction allows taking Corvalol and Valocordin, which have a calming effect and normalize the heartbeat. These medications help relieve symptoms of anxiety and ease nervousness, reduce heart rate and stress on the heart.
Quickly provided first aid for myocardial infarction consists of mandatory intake of medications necessary to alleviate the condition, reduce pain and normalize blood flow, which neutralizes the likelihood of negative consequences.
Self-administration of first aid for a heart attack includes the need to take aspirin, which is necessary to thin the blood. Taking into account the patient’s weight and well-being, the required dose is 500 mg (at least a whole tablet).
Release forms of Nitroglycerin
At home or on the street, it is difficult to fully diagnose an attack, which is often confused with angina pectoris. It is necessary to be interested in the person’s well-being, and in case of emerging symptoms of acute myocardial infarction, provide psychological support. It is recommended to immediately call the emergency team without wasting precious time.
The qualified work of medical specialists will help preserve the vital functions of the body. Acute coronary syndrome, the symptoms of which include dizziness and chills, a sharp outflow of blood from the face and a lack of oxygen, requires the participation of others and control of the pulse rate. First aid provided for myocardial infarction before the ambulance arrives requires careful recognition of the symptoms:
- painful sensations;
- general weakness and fatigue;
- lack of oxygen when breathing.
Not many people have any idea what to do during an attack: the primary steps that must be taken are to identify the symptoms, reduce the level of pain and call a team of medical professionals.
Self-help for a heart attack before the ambulance arrives requires reducing nervousness and neutralizing a person’s panic state.
Increasing heart pain and lack of air when breathing, increasing weakness and shortness of breath are accompanied by uncontrolled changes in blood pressure and determine the required compliance with the standard of emergency care for myocardial infarction.
Myocardial infarction occurs when the artery that supplies oxygen to the heart is blocked. Due to lack of proper blood supply, the heart muscle is subject to certain damages. As a rule, myocardial infarction is accompanied by chest pain lasting more than 15 minutes, but a hidden course of this condition cannot be excluded, which, accordingly, excludes the manifestation of any of its symptoms.
- Call an ambulance. You should not endure pain and symptoms that indicate an approaching heart attack or its onset for more than five minutes. If you are unable to call an ambulance, contact the people around you. If there is a police or fire department vehicle nearby, contact them; they can also take you to the hospital. The same applies to providing first aid for myocardial infarction to other people.
- Chew and swallow aspirin (1 tablet).
- Take/give nitroglycerin to the patient. This can only be done if these tablets were previously prescribed to you by a doctor - the dosage in this case is determined according to his instructions. In no case should you take nitroglycerin intended for another person - in the absence of direct instructions to take this drug, it may simply become dangerous for you.
- Cardiopulmonary resuscitation (abbr. CPR). If you suspect the relevance of the condition in question in any of the people around you, and if the victim is unconscious for this reason, you must begin to take the appropriate measures provided for in this paragraph. In particular, first aid for myocardial infarction in the case of an unconscious victim requires, in the absence of the person providing it, SRL skills, performing manual massage of the chest area. It consists of continuously applied pressure on the chest (approximately twice per second). If you have the skills to provide such assistance and are confident in your own skills, either 30 pressures are applied to the chest area with alternating artificial respiration (“mouth to mouth”), or only pressure is performed on the specified area.
- Severe pain behind the sternum. A very unpleasant feeling occurs unexpectedly, in paroxysms, and the pain syndrome can “radiate” between the shoulder blades, to the left shoulder, arm, part of the neck. Lasts from thirty minutes to two hours.
- Paleness and profuse sweating. A person with myocardial infarction quickly turns pale and cold, sticky sweat appears all over the body.
- Fainting and borderline states. Almost always, especially in the first phase of an attack, a person may faint several times. Less often, he experiences an unreasonable feeling of fear, and sometimes vague auditory and visual hallucinations.
- Arrhythmia and heart failure. Nearly half of myocardial infarction survivors showed telltale signs of heart failure, ranging from shortness of breath and nonproductive cough to atrial fibrillation and brief sudden cardiac arrest.
- Low effectiveness of nitroglycerin. A person does not feel significant relief after taking nitroglycerin - drugs of this group, which dilate blood vessels, can only be used as an additional remedy, together with prescription narcotic analgesics, and only under certain conditions.
- Place the person in a chair with a backrest or in a reclining position so that the upper part of the body is located as high as possible - this will reduce the load on the heart.
- Calm the patient emotionally or with Valocordin to reduce the heart rate.
- Unbutton too tight and tight clothes, loosen all knots, tie, scarf, especially if signs of imminent suffocation begin to appear.
- Be sure to check your blood pressure and pulse rate - if they are normal, you can give nitroglycerin/aminophylline (if it drops sharply, this procedure can lead to cardiac arrest).
- Several aspirin tablets actively thin the blood - be sure to give them (if the person is not allergic) with a maximum dose of up to 300 milligrams. A faster effect of the drug is obtained by chewing it in the mouth.
- Has your heart stopped? Is breathing agonistic or absent? Does it take a long time for a person to regain consciousness? Cardiopulmonary resuscitation should be started immediately. In the absence of a defibrillator, perform artificial respiration, chest compressions, or in extreme situations, a precordial short strong blow to the sternum with a fist. The basic scheme is 15 pumping movements, two inhalations/exhalations, one launch-impact, all this should be done for a maximum of 10 minutes.
- Severe pain behind the sternum. A very unpleasant feeling occurs unexpectedly, in paroxysms, and the pain syndrome can “radiate” between the shoulder blades, to the left shoulder, arm, part of the neck. Lasts from thirty minutes to two hours.
- Paleness and profuse sweating. A person with myocardial infarction quickly turns pale and cold, sticky sweat appears all over the body.
- Fainting and borderline states. Almost always, especially in the first phase of an attack, a person may faint several times. Less often, he experiences an unreasonable feeling of fear, and sometimes vague auditory and visual hallucinations.
- Arrhythmia and heart failure. Nearly half of myocardial infarction survivors showed telltale signs of heart failure, ranging from shortness of breath and nonproductive cough to atrial fibrillation and brief sudden cardiac arrest.
- Low effectiveness of nitroglycerin. A person does not feel significant relief after taking nitroglycerin - drugs of this group, which dilate blood vessels, can only be used as an additional remedy, together with prescription narcotic analgesics, and only under certain conditions.
Helping another person
The situation is much more complicated with primary measures for a third-party patient. If the victim complains of severe chest pain, you should immediately call an ambulance. Tell about the condition, suggest the development of necrosis of the heart muscle.
Further:
- Help sit the person down. Laying is not recommended for the reasons already mentioned. Asphyxia due to pulmonary edema and/or vomiting. Possible death before specialists arrive. And beyond cardiac reasons.
- Give Nitroglycerin for mild pain. In general, it is better to refrain from using the drugs unless there is a clear indication from the treating cardiology specialist. The permissible dosage when prescribed by a doctor is 1 tablet. Additional use of aspirin is possible, again according to indications.
- Open the window, window. If the patient is at home or indoors. Move the patient to a warm place when the condition develops in the winter season. In summer there is no need. But place a cloth or clothing under the person so that there is no direct contact with the cold ground or asphalt.
- Calm the person down. Do not allow intense movement. Physical activities affect your heart rate. Excessive stimulation of cardiac structures leads to a greater aggravation of the ischemic process.
- If possible, measure your heart rate.
If the patient is unconscious
The algorithm is slightly different:
- Move the person to a safe place. For example, when the patient is close to the road or highway.
- Call out and gently shake your shoulder. Try to get out of syncope in this way.
- Check your pulse. Against the background of the current heart attack, vascular vibrations in the wrists and neck will be minimal.
- Assess the nature of breathing, its presence. You need to lean in and listen.
- Free your tongue. In a faint state, it can lodge in the throat and block the airways.
- The head is carefully turned to the side. In case of vomiting, so that food masses and gastric contents do not provoke aspiration and death from asphyxia.
In case of cardiac arrest
Direct massage is recommended.
Open palms are folded and placed on top of each other. Hands are placed on the chest, in the center, in the hollow area. Press rhythmically at a speed of 100-120 movements per minute.
The force should be sufficient to displace the chest 5 cm in depth.
Clinical first aid guidelines suggest that rib fractures are not a reason to stop massage.
It is better not to do artificial respiration. Without a well-developed skill, the method will be of no use, and valuable time will be lost.
Massage itself is a physically exhausting process. Every 2-3 minutes it is recommended to change with others. You can gain useful experience after completing the relevant courses.
Upon arrival of the team, resuscitation measures are stopped. It is necessary to inform the medical personnel about the condition, also if there have been changes in blood pressure, heart rate - vital indicators.
Primary diagnostic measures - assessment of cardiac activity and breathing - should take no more than 2-3 minutes.
No longer recommended, risks are too high, time is running out. If necessary, it is possible to accompany the person to the emergency department. Especially if it is an elderly relative or a mentally ill person. The issue is resolved on an individual basis.
Ministry of Health of the Astrakhan Region
GBUZ JSC "Center for Medical Prevention"
REMINDER FOR THE POPULATION
FIRST AID FOR MYOCARDIAL INFARCTION
MYOCARDIAL INFARCTION
– this is the death of a section of the heart muscle caused by its prolonged ischemia due to spasm or thrombosis of the coronary arteries. One of the characteristic signs of myocardial infarction is the fear of death.
SYMPTOMS OF MYOCARDIAL INFARCTION
· Prolonged intense squeezing-pressing pain in the left half of the chest, may
give to the arm, shoulder, neck, back, shoulder blade area, lower jaw and stomach.
· The pain continues even after taking nitroglycerin.
· Fear of death arises, the person turns pale, and cold sweat appears.
· Fainting condition.
The disease does not always manifest itself in such a classic picture. A person may only feel discomfort in the chest or interruptions in the functioning of the heart. In some cases there is no pain at all. In addition, there are atypical cases of myocardial infarction, when the disease is manifested by difficulty breathing with shortness of breath or abdominal pain, nausea, vomiting, and digestive disorders.
If these symptoms occur, you need to call EMERGENCY MEDICAL AID.
(preferably a specialized cardiology or resuscitation team)!
| 103 or 03 – from a landline phone 112 – from a mobile phone |
WHAT TO DO BEFORE THE ARRIVAL OF AMBULANCE MEDICAL AID?
1.
Avoid physical activity, do not walk, do not smoke, do not eat food until the doctor arrives.
2.
Remove or unfasten clothing that restricts breathing.
3.
Open a window or turn on the air conditioner to provide fresh air.
4.
Lie in bed with the head of the bed raised or sit down (preferably in a chair with armrests) so that the upper body is raised.
5.
Take half a tablet (0.25 g) of acetylsalicylic acid (aspirin) - chew the tablet, do not swallow, leave it to be absorbed under the tongue.
At the same time, place a nitroglycerin tablet (capsule, spray dose) under the tongue. Nitroglycerin can be given again at intervals of 15-20 minutes. Nitroglycerin is not recommended for use when myocardial infarction is accompanied by low blood pressure. 6.
In case of panic, you need to take a sedative - valerian or Corvalol.
If cardiac arrest is suspected ( lack of consciousness, breathing, carotid pulse, blood pressure)
resuscitation measures should be started immediately. To save a person you have 3-5 minutes, for this remember the algorithm of actions:
· To start a stopped heart from a height of 30-40 cm from the patient’s chest, a strong blow is applied to the chest with the edge of the palm clenched into a fist ( precordial
blow).
Then feel the pulse in the carotid artery. If it is not there, proceed to chest compressions and artificial respiration.
· Place a cushion made from available items under the patient’s neck. Throw the patient's head back as far as possible. If necessary, clean your mouth with a tissue.
· Approximately 15 chest compressions should be alternated with two full exhalations into the mouth or nose. Check your carotid pulse periodically.
· Rescue efforts should continue until the ambulance arrives. After the ambulance arrives, give the doctors the opportunity to do everything necessary.
REMEMBER
that myocardial infarction can be prevented!
To avoid the development of the disease, it is necessary to undergo a timely examination of the cardiovascular system and be observed by a cardiologist.
What you should absolutely not do
The following actions are prohibited:
- Engage in physical activity. In some cases, myocardial infarction manifests itself as bradycardia. The heart rate decreases.
Particularly proactive people begin to do squats and push-ups. This is absolutely impossible to do. Heart rate will increase due to reflex stimulation of cardiac activity, but at what cost?
Myocardial contractility decreases, blood flow weakens. The increased frequency of contractions will only make the situation worse. The risk of death will increase dramatically.
- Take medications. The issue of a possible emergency condition and self-care methods is discussed with a cardiologist. If he allows you to take Nitroglycerin, it is permissible to drink it. In other cases, the condition may worsen. The same applies to Aspirin and other medications.
- Wash with cold water. Low temperature exposure to facial tissue will lead to reflex vasoconstriction. Including coronary ones. This is the body's natural response to an intense stimulus. The nutrition of cardiac structures will weaken. Is it worth saying how the hearts will react to such a process? You can’t wash your face with hot or even warm water.
- Panic, nervous. A negative emotional background will lead to the release of large amounts of cortisol, adrenaline and other stress hormones. Including angiotensin, renin. They will lead to stenosis (narrowing) of blood vessels, coronary arteries. The nutrition of the heart and body tissues will weaken. This will increase the likelihood of death or, at a minimum, accelerate the progression of myocardial infarction.
- Eating. You cannot eat because you are likely to develop vomiting. When you lose consciousness, a reflex process occurs. This body response is the result of cerebral ischemia. Aspiration of gastric contents and death from asphyxia are possible.
- Try to cope on your own. It is necessary to call an ambulance. This is an axiom. Provided that the patient still plans to live. Because without hospitalization the chances tend to zero.
- If someone else is hurt, don’t shake the person. Trying to bring him to his senses, hitting him on the cheeks. Such methods are good for cinema, but are strictly contraindicated in real life. Injuries to the cervical spine, vomiting, and other dangerous situations are possible.
Read also Alcohol poisoning: symptoms, first aid, treatment
If a car is available, the patient is transported to the hospital on their own. This is only advisable if the institution is located nearby or there is a chance of quick transportation.
What do doctors do at first?
Emergency care for myocardial infarction is not a method of treatment, but a path to maintaining the minimum possible vital activity and slowing down the process.
The first thing paramedics or doctors do is assess the objective condition of a person. Sometimes it gets to the point of absurdity, and they try to find out the well-being of unconscious people, but this is rather an exception to the rule.
Blood pressure and heart rate are measured. Auscultation provides information about chest sounds.
The number one task for doctors is to partially stabilize the patient’s condition and take him to the hospital. The person is then placed in intensive care.
Impact measures are conservative. The following drugs are used:
- Epinephrine, Adrenaline. They artificially stimulate cardiac activity. Particularly relevant for critical drops in blood pressure and significant bradycardia of less than 50 beats per minute. In other cases, use is strictly contraindicated. The pathological process may worsen.
- Antispasmodics. Relieves excess muscle stiffness, partially restores blood flow, and eliminates pain.
- Beta blockers. To equalize heart rate. Specific names are determined by specialists. If the patient is accompanied by a relative, it is worth informing about the presence of cardiac or vascular diseases and talking about the prescribed therapy regimen. This will help you get your bearings.
- Calcium antagonists. To ensure normal myocardial contractility.
- Non-narcotic and narcotic, opioid painkillers. Analgesics are used if the patient is conscious to provide relief. Because it is extremely painful for a person to bear.
- Nitroglycerine. Only if there are no contraindications. It is usually prescribed at the pre-hospital stage by the ambulance specialists themselves.
Attention:
It is prohibited to use cardiac glycosides and antiarrhythmic medications. They will cause cardiac arrest and death. The likelihood of complications is high, so considerable experience and qualifications are required.
First aid for myocardial infarction provides a good prognosis for the course and outcome of the pathological process. In the absence of competent support, the chances of survival drop sharply.
Taking specialized courses is a good investment in the future. Including in the event of an emergency condition developing in the person himself or his loved ones.
What determines the success of providing first aid to a patient with myocardial infarction?
The quality of first aid provided to a patient depends on many factors:
- knowledge of the person providing assistance, the algorithm of actions in case of a heart attack, the ability to perform resuscitation actions;
- time elapsed from the attack to the onset of actions;
- medication and instrumental support (tonometer, Nitroglycerin, Aspirin);
- the staffing of ambulance teams with the necessary equipment, medications, and personnel qualifications;
- distance from specialized cardiology departments.
Possible complications of myocardial infarction
Experts divide the complications of a heart attack into early and late:
| Type of complications of myocardial infarction | When do they arise? | Types of complications |
| Early | In the first hours or days (in the first 3-4 days) after an acute attack |
|
| Late | Occurs against the background of increased motor activity of the patient 14–21 days after an acute attack |
|
Depending on the nature of the damage and disorders, complications of a heart attack are classified as follows:
| Type of complications | Nature of damage and violations |
| Mechanical |
|
| Electrical (or arrhythmic) | occur in almost 90% of patients and manifest themselves in different types of arrhythmias. |
| Ischemic |
|
| Thromboembolic |
|
| Inflammatory |
|
The most severe complications of myocardial infarction include:
- recurrent or prolonged course;
- pulmonary edema;
- areactive or true cardiogenic shock;
- clinical death;
- acute right ventricular failure;
- atrioventricular block at any location of the necrosis zone;
- acute cardiac aneurysm;
- thrombosis and thromboembolism in various organs;
- circulatory failure IIB and III degrees;
- ventricular paroxysmal tachycardia;
- gastrointestinal bleeding;
- a combination of two or more complications.
Potential Risks
In case of myocardial infarction, experts identify the following potential risks:
| Primary | Secondary |
|
|