DEAD FRUIT EGG AND NON-HYSTICAL MOLE
DEATH FETAL EGG AND NON-HYSTICAL MOLE - a condition in which the fertilized egg dies, but continues to remain in the uterine cavity for a long time, sometimes several months. It is more often observed in repeatedly pregnant women with a history of induced abortions.
Clinic
Main symptoms: bloody discharge and cramping pain often appear, which then stop. There may be a long absence of these symptoms. Subjective signs of pregnancy disappear. The size of the uterus is less than the expected period of pregnancy, its consistency is denser than during pregnancy. At a certain point, the pregnant woman does not feel fetal movements. Often the fertilized egg is ejected from the uterus during the period corresponding to the due date. If the fetus dies in the first months of pregnancy, it is resorbed; if the pregnancy is terminated in the later stages, it undergoes maceration, mummification, and petrification. The fetus decreases in size, acquiring a spherical or flattened shape, and becomes locked in an amniotic hematoma. During short periods of pregnancy, blood permeates the fertilized egg, and the contents of the uterus turn into a bloody mole, which is then leached and acquires a yellowish-clay tint, forming a fleshy mole.
Diagnostics
Based on the cessation of uterine enlargement.
Treatment
Only bleeding requires emptying the uterus. When an infection occurs, medications are prescribed to accelerate the onset of miscarriage.
Taking into account the dangers that threaten a woman in connection with the presence of a retained fertilized egg and depending on infection if the death of the fertilized egg is established, the uterine cavity should be emptied with the prescription of drugs that stimulate uterine contractions and provoke a miscarriage.
Pregnancy after hydatidiform mole
If a woman has no complications, then doctors allow her to become pregnant six months after the operation and monitoring of hCG levels in the blood.
Pregnancy after a hydatidiform mole is no different from others, but before planning begins, you need to put your hormonal levels in order and cure STDs, if any. This will reduce the risk of reappearance of a pathologically altered embryo.
Complications after removal of surgery
For several months, the doctor is required to monitor the patient’s blood counts and track the dynamics of the decrease in hCG after surgery. If the hormone remains at the same level or increases, then this is a reason to write the woman a referral to a gynecologist-oncologist.
In some antenatal clinics, every pregnant woman with a hydatidiform mole is registered with an oncologist until the level of human chorionic gonadotropin returns to normal.
Such precautions are due to the fact that chorionic villi, growing in the form of vesicles, can become a malignant tumor. If the hCG level remains unchanged or increases, the patient is prescribed a course of chemotherapy.
It must be remembered that with the right approach from medical specialists, hydatidiform mole can be 100% curable.
Tags: pregnancy
- Endometrioid ovarian cyst - treatment and pregnancy
- Glaucoma - causes, symptoms and treatment, disease prevention
- Scoliosis - causes, symptoms by degree, treatment,…
- Urticaria in adults: photos, symptoms and treatment,…
- Atrial fibrillation - causes, symptoms and...
- Causes of shortness of breath: symptoms of diseases, what to do for...
Dead ovum and non-hydatidiform mole (O02.0)
Pathological ovum
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
With changes and additions WHO 1990-2018.
Processing and translation of changes © mkb-10.com
Dead fertilized egg causes
A failed miscarriage is a condition in which an ultrasound examination reveals the presence of an empty fertilized egg - anembryony. A living embryo is not visible inside such a fertilized egg - it either developed incorrectly or lost its viability in very early stages of development, but the pregnant woman’s body did not respond to this in time, as a result of which a spontaneous miscarriage did not take place. It is possible to reliably determine the stopped development of the embryo no earlier than the sixth week of pregnancy, since before this period the heartbeat may not be heard even with its normal development.
It is only a matter of time before the frozen fertilized egg begins to be expelled from the body. If such an embryo is detected, it is better for a woman to cleanse (curettage) the uterus rather than wait for bleeding to begin. The curettage procedure is performed by an obstetrician-gynecologist in a hospital setting. The duration of cleaning is several minutes, it is performed under general anesthesia. Carrying out a thorough curettage of the uterus leads to its contraction, helps prevent bleeding and significantly reduces the risk of infection of the uterus after a miscarriage. After cleaning, a woman may be prescribed antibiotics for preventive purposes.
Causes of hydatidiform mole
The occurrence of hydatidiform mole has a rather complex mechanism, which implies the presence of several factors that contribute to the appearance of an abnormal product of conception. All causes can be roughly divided into primary and secondary.
Some are general in nature and can be observed in a large number of women, but are not a guarantee that all these women will be pregnant with hydatidiform moles.
Secondary causes are a kind of trigger mechanism, the appearance of which is due to primary factors. They are guaranteed to cause an abnormal development of the embryo.
Primary causes
- Serious disruptions in the functioning of the endocrine system. Typically, a woman has very low estrogen levels.
- Infectious diseases. For example, at the time of conception, the expectant mother had a serious exacerbation of some type of STD.
- Patient's age. The incidence of hydatidiform mole increases in women over 37 years of age.
Secondary causes
- Fertilization of an egg that does not have a nucleus. As a result, the product of conception has a karyotype of 46XY. The production of such eggs is activated in women over 35 years of age, when the childbearing period is nearing completion.
- Fertilization of the egg occurred without pathologies, but then the maternal genes were lost, and the paternal ones were duplicated. This product of conception has a karyotype of 46XX.
- Fertilization of an egg by two sperm at once. In this case, the maternal chromosomes are in the minority and the zygote karyotype looks like 69XXY or 69XXX.
Establishing diagnosis
Diagnosis of a non-developing pregnancy is carried out on the basis of both the clinic and additional research methods.
During a gynecological examination, attention is drawn to the discrepancy between the size of the uterus and the duration of pregnancy, and the dense consistency of the uterus. The cervical canal is closed. Minor bleeding may occur.
The fetal heartbeat cannot be heard.
The following results of additional research methods are diagnostically important:
- on ultrasound there is no embryo when the size of the fertilized egg is more than 25 mm;
- Fetal CTE is more than 7 mm.
The presence of these signs allows you to make a 100% reliable diagnosis.
If there is a suspicion of a non-developing pregnancy in the absence of reliable signs, a repeat ultrasound is prescribed a week after the initial ultrasound. If the doctor doubts the diagnosis during a repeat ultrasound, the woman is referred to a more specialized institution to confirm or refute the diagnosis.
Important ! The absence of a fetal heartbeat in early stages of pregnancy is not a sufficient criterion for diagnosing a non-developing pregnancy and is not applied in isolation from the above criteria.
General blood and urine tests, a biochemical blood test, an ECG are prescribed; if indicated, a bacteriological analysis of a vaginal smear, a hemostasiogram for non-developing pregnancy for more than 4 weeks.
Studies of thyroid hormones and ultrasound of the thyroid gland are carried out. According to indications, consultations with a therapist, geneticist, and endocrinologist are prescribed.
Differential diagnosis is carried out with dysfunctional uterine bleeding, benign and malignant neoplasms of the uterine cavity (including leiomyoma), endometrial hyperplasia.
ATTENTION! A pregnancy test is useless at this stage. It can be positive when the child is already dead.
Treatment of the disease - what to do?
A pathologically altered product of conception is not subject to any other treatment other than its removal by surgical curettage or vacuum aspiration.
Moreover, the longer the patient delays visiting the clinic, the more she risks losing her uterus due to heavy bleeding when trying to separate the membranes that have grown into the uterine wall.
Vacuum aspiration
Indicated for those patients whose hydatidiform mole was diagnosed at a short period of time (up to 4 weeks). The pregnant woman is given oxytocin and anesthesia intravenously. Then the doctor begins the procedure of dilating the cervical canal, which is accompanied by severe bleeding.
When the cervix is prepared, you can begin vacuum aspiration of the uterine body cavity using a 12 mm diameter tip for the device. With the other hand, the specialist massages the uterus abdominally, through the abdominal wall.
- After aspiration, curettage of the uterine body cavity is carried out - this is necessary in order to completely eliminate all particles of the hydatidiform mole.
Surgical curettage
Almost always used in cases where the pregnancy is more than 4 weeks.
This method of treating hydatidiform mole is more preferable than just vacuum aspiration as it allows you to get rid of the product of conception and avoid complications in the form of relapse of the pathological process.
When curettage after a hydatidiform mole, the cervix also needs to be dilated, but if vacuum aspiration can be performed without general anesthesia, the surgical treatment method involves the introduction of general anesthesia.
After treatment of the uterine cavity, the contents are removed using a curette (the procedure is called “curettage”).
As a rule, doctors use a combination of these two methods: vacuum aspiration is performed in conjunction with curettage and subsequent curettage.
Implications for mother and child
In most cases, the disease does not pose a risk to a woman’s life. Miscarriage usually occurs before the 8th week of pregnancy.
The exception is intense bleeding during abortion and infection.
If the fertilized egg is expelled by the uterus on its own, parts of the egg may remain in its cavity, which further contribute to the occurrence of an infectious process. Infection can also occur in utero.
The fetus dies with this pathology. A dead egg is resolved in different ways. Depending on the accompanying circumstances (gestational age, presence of infection), the embryo can:
- dissolve;
- when the fetus becomes saturated with blood, it transforms into a non-vesical (blood) mole;
- mummify or petrify (petrify).
It is worth noting that the death of a fetus, especially in the later stages, often becomes a psychological trauma for a woman. Patients are recommended to consult a psychologist.
Pathological anatomy
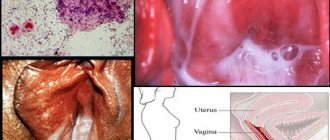
Rice.
1. Macroscopic specimen of the uterus during a hydatidiform mole: the uterine cavity is opened, the grape-shaped masses of a hydatidiform mole are visible. Macroscopically with P. z. in the uterus and extremely rarely in the fallopian tubes, chorionic villi are found, which have the appearance of a grape-shaped mass (Fig. 1), consisting of many different-sized bubbles (diameter from less than 1 mm to more than 1 cm) with transparent contents. Usually the fetus (or embryo) in the uterine cavity with P. z. absent, although sometimes with partial P. z. a developed fetus is discovered.
Microscopically, edema and often mucus-like transformation of the stroma are noted in the chorionic villi; there are no blood vessels, or their number is insignificant; hyperplasia of the chorionic epithelium is observed. Hydropic changes in the stroma of chorionic villi can sometimes occur in the absence of P. z., for example, after spontaneous abortion. In the edematous villi of the chorion during a hydatidiform mole, one can find large, predominantly round-shaped cells with foamy cytoplasm - Kashchenko-Hofbauer cells (see Placenta). Cytotrophoblast cells have high mitotic activity, their nuclei are of different sizes and color intensity, which also occurs in the syncytium of the villi. In the cytoplasm of the syncytium, the number of vacuoles of various sizes is increased. Histochemically, a significant amount of lipids and glycoprotein grains are found in the cytoplasm of chorionic epithelial cells; alkaline phosphatase is detected on the surface of syncytium cells. Electron microscopic examination reveals a large amount of osmiophilic lipids and ribonucleoprotein grains in the syncytium, as well as a smaller number of mitochondria, which often have an irregular shape, compared to the norm.
With destructive P. z. chorionic villi penetrate deep into the myometrium, destroying the walls of blood vessels and affecting the entire thickness of the uterus. Microscopically, numerous proliferating trophoblast cells of various sizes and shapes are detected; the coloring of the nuclei and cytoplasm has different intensities.
With P. z. often (in 25-60% of cases) multiple, usually small, thecal lutein cysts develop in the ovaries (see Ovaries), which have a smooth inner surface and a yellowish color; they are usually thin-walled with transparent contents. The appearance of thecallutein cysts in P. z. is associated with hyperstimulation of theca lutein cells by human chorionic gonadotropin (see), produced in large quantities by proliferating trophoblast. After removal, expulsion or birth of P. z. Theca lutein cysts undergo reverse development.