| Rosuvastatin | |
| Rosuvastatin | |
| Chemical compound | |
| IUPAC | (3 R ,5 S ,6 E )-7-[4-(4-fluorophenyl)-2-( N -methylmethanesulfonamido)-6-(propan-2-yl)pyrimidin-5-yl]-3,5- dihydroxyhept-6-enoic acid |
| Gross formula | C₂₂H₂₈FN₃O₆S |
| Molar mass | 481,539 |
| CAS | 287714-41-4 |
| PubChem | 446157 |
| DrugBank | DB01098 |
| Classification | |
| Pharmacol. group | statins |
| ATX | C10AA07 |
| ICD-10 | 78.078.0, 78.178.1, 78.278.2, 10., 15., 21.921.9, 24.924.9, 25.925.9, 64., 70., 100100., 81.281.2[1] |
| Dosage forms | |
| film-coated tablets | |
| Other names | |
| Akorta, Crestor®, Mertenil®, Rozart, Rozistark®, Rosuvastatin calcium, Rosuvastatin Canon, Rosuvastatin-SZ, Rosucard, Rozulip®, Roxera®, Tevastor® | |
| Rosuvastatin at Wikimedia Commons | |
Rosuvastatin
is a fourth-generation lipid-lowering drug from the group of statins. Developed by the Japanese pharmaceutical company Shionogi (English)Russian, sold since 2003.
pharmachologic effect
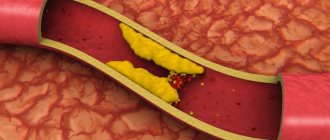
Rosuvastatin is a selective and competitive inhibitor of HMG-CoA reductase, which converts 3-hydroxy-3-methylglutaryl coenzyme A into mevalonic acid, which is a precursor of sterols, including cholesterol. Rosuvastatin increases the number of hepatic LDL-C (low-density lipoprotein cholesterol) receptors on the cell surface, increasing the uptake and catabolism of LDL-C, and inhibits the synthesis of VLDL-C in the liver, therefore reducing the total number of VLDL-C (very low-density lipoprotein cholesterol) particles. and LDL-C. Increases the content of HDL cholesterol (high density lipoprotein cholesterol). Reduces the size of atherosclerotic plaque and increases the lumen of blood vessels. Reduces the level of C-reactive protein.
Concomitant effects of the drug
Statins must be taken long-term. They are well tolerated by patients, but treatment continues for at least 3–4 years. Sometimes the patient develops disorders in the muscular system, and pain occurs when walking. A dangerous complication is complete tissue destruction and the development of renal failure.
Side effects of statins pose a threat to the patient's life if he takes the following drugs:
- antibiotics;
- fibrates;
- Verapamil;
- Amiodarone.
The medicine becomes dangerous for older people, those suffering from concomitant chronic diseases, and people who abuse alcohol. Large amounts of alcohol increase the activity of liver enzymes.
Side effects are an alarming signal, and the patient should urgently consult a doctor. Patients who drink alcohol may experience:
- headache;
- rash;
- bloating;
- insomnia.
You need to take medications correctly; it is recommended to take the tablet with water, if the instructions do not say anything about this. Tea, juice, mineral water can change the effect of the drug, strengthen or weaken it.
Drug interactions
The following drugs may cause negative interactions when combined with rosuvastatin and should be discussed with your doctor[3]:
- Anticoagulants: Warfarin (Marevan, Warfarex) - increases the risk of bleeding;
- H2-antihistamines: Cimetidine (Belomet, Histodil®, Primamet®, Simesan) - increases the risk of a decrease in endogenous steroid hormones;
- Immunosuppressants: Cyclosporine (Consupren, Orgasporin, Panimune Bioral, Sandimmune®, Ecoral®) - increases the risk of developing rhabdomyolysis and acute renal failure;
- Antifungals: Ketoconazole (Livarol®, Nizoral®, Mycozoral®, Sebozol®, Perhotal) - increases the risk of developing rhabdomyolysis and acute renal failure;
- Additional lipid-lowering agents: Clofibrate (Atromid-S), Fenofibrate (Tricor), Gemfibrozil (Lopid) - increases the risk of side effects;
- Nicotinic acid preparations: Niacin, Niaspan, Niacor, Enduracin - increases the risk of developing rhabdomyolysis and acute renal failure;
- HIV protease inhibitors: Atazanavir (Reyataz), Ritonavir (Rinvir, Norvir), Lopinavir, Ritonavir (Kaletra) - increases the risk of rhabdomyolysis and acute renal failure;
- Diuretics: Spironolactone (Veroshpiron, Spirix®, Aldactone, Veroshpilactone, Uractone) - increases the risk of a decrease in endogenous steroid hormones.
- Alcohol consumption should be reduced while taking rosuvastatin to reduce the risk of liver damage[4].
- Antacids (aluminum and magnesium hydroxides) such as Mylanta and Maalox should not be taken within two hours of taking rosuvastatin[4].
- Cardiac glycosides: Digoxin (Novodigal) - the concentration of digoxin increases.
Instructions for use of Rosuvastatin, dosage
The tablets are taken orally, swallowed whole, without crushing or chewing, with water, regardless of meals. The daily dose of the drug is taken 1 time.
Before starting therapy and during treatment, compliance with a standard cholesterol-lowering diet is required. Depending on the therapeutic goals and response to treatment, as well as taking into account current recommendations for target lipid levels, the doctor selects the dose of Rosuvastatin individually.
The recommended initial dose is 5 or 10 mg of rosuvastatin 1 time/day. When determining the initial dose, it is necessary to take into account the individual level of cholesterol levels, the possible risk of cardiovascular complications and assess the likelihood of developing adverse reactions. After 4 weeks, the doctor may increase the dose of the drug if necessary.
Increasing the dose to 40 mg should be carried out only in cases of severe hypercholesterolemia and a high risk of cardiovascular complications (especially in patients with hereditary hypercholesterolemia), if the desired result was not achieved when using a dose of 20 mg, and also if it is possible to provide medical supervision for the condition of such a patient.
Patients receiving rosuvastatin at a dose of 40 mg should be observed by a specialist especially carefully. It is not recommended to prescribe a dose of 40 mg to patients who have not previously consulted a doctor.
It is necessary to monitor lipid metabolism after 2–4 weeks of treatment with Rosuvastatin and/or when increasing its dose. Depending on these indicators, the dose should be adjusted if necessary.
- It is not recommended to prescribe a higher dose than 40 mg - this is not justified due to increased side effects.
The sudden onset of muscle pain/weakness or spasms, especially when accompanied by fever and malaise, requires medical attention. In such cases, it is necessary to determine the activity of creatine phosphokinase. If symptoms disappear and values return to normal, re-prescribing Rosuvastatin in lower doses can be considered under close monitoring of the patient's condition. In the absence of symptoms, routine monitoring of creatine phosphokinase activity is not advisable.
Side effects
According to the instructions for use, the appointment of Rosuvastatin may be accompanied by the following side effects:
- dizziness, headache (often).
- allergic reactions (including angioedema) are rare.
- rashes, itching, urticaria (uncommon side effects).
- rhabdomyolysis and myopathy (rare), muscle pain (common).
- constipation, abdominal pain, nausea (often), pancreatitis (rarely).
- tubular proteinuria.
- asthenia (often).
If patients have a glucose concentration of 5.6–6.9 mmol/l, the likelihood of developing type 2 diabetes increases.
Contraindications
It is contraindicated to prescribe Rosuvastatin in the following cases:
- liver disease in the active stage, including a persistent increase in the level of transaminases of unknown origin, as well as any increase in transaminases with a level 3 times or more exceeding the upper limit of normal;
- severe renal impairment with creatinine clearance ≤30 ml/min;
- simultaneous use of cyclosporine;
- during pregnancy and breastfeeding;
- increased sensitivity of the immune system to rosuvastatin or any other component;
- the drug is not prescribed to patients who do not use highly effective and efficient methods of contraception;
- myopathy;
- a dose of 40 mg/day is contraindicated in patients with an increased risk of developing rhabdomyolysis or myopathy;
- age up to 18 years.
Overdose
There is no specific treatment for an overdose of rosuvastatin, so treatment is symptomatic. It is necessary to monitor liver function and the activity of the enzyme creatinine phosphokinase.
FDA
In March 2012, the FDA updated its guidance for statins to include case reports of memory loss, liver damage, high blood sugar, development of type 2 diabetes, and muscle damage[5]. The new guidance states:
- The FDA has determined that liver damage associated with statin use is rare but can occur.
- Case reports of memory loss, forgetfulness, and periods of confusion have been noted with all statins and in all age groups. These experiences are rare, but sufferers often report a "fuzzy" feeling in their thinking.
- Slight increases in the risk of high blood sugar and type 2 diabetes have been reported with the use of statins.
- Some drugs interact with statins in ways that increase the risk of muscle damage (myopathy), manifested by unexplained muscle weakness and pain.
Rosuvastatin and Atorvastatin - what is the difference?
These are representatives of different generations of drugs - the fourth and third, respectively.
Later synthesis of the drug ensures the appearance of new qualities in it that improve the effect or tolerability. Its cost has increased accordingly. Important distinctive characteristics of these medications, produced only in tablets, are outlined in the table. comparison table
| Rosuvastatin (instructions) | Atorvastatin (instructions) |
| Generation LS | |
| IV | III |
| Participation of the liver in the transformation | |
| 10% | 90-95% |
| Half-life (the longer, the less often you need to take it) | |
| 19 hours | 7-9 hours |
| Metabolite activity | |
| No | Yes |
| Initial dosage (mg) | |
| 5 | 10 |
| Average dose (mg) | |
| 10 | 40 |
| Maximum dose (mg) | |
| 20 | 80 |
| Start of action | |
| 5-7 days | 7-12 days |
| 90-100% effect | |
| In 3-4 weeks | At 4-5 weeks of admission |
| Reduced levels of free fats (TG) | |
| No (water soluble) | Yes (fat soluble) |
| Side effects | |
| Rare | 1% or more, depending on the condition of the liver |
| Country of issue | |
| UK, Russia | Israel, Russia |
| Number of analogues | |
| 12 | 4 |
Participation of the liver - conversion of the drug by the liver is not required for the onset of action, which is the difference between Rosuvastatin and Atorvastatin. The result is a faster onset of action, less functional load on the liver cells, greater safety in using the drug, and its preferential excretion through the intestines (about 10% with bile). Lack of fat solubility does not imply participation in the breakdown of TG (triglycerides or free fats).
Links
- Annual Report and Form 20-F, Information 2004 (PDF) (unavailable link - history
). AstraZeneca PLC (2005). Archived from the original on May 13, 2005. - Annual Report and Form 20-F, 2003 (PDF). AstraZeneca PLC (2004). Retrieved March 20, 2005. Archived May 13, 2005.
- Highlights of Prescribing Information (PDF). AstraZeneca PLC (2008). Retrieved March 11, 2009. Archived December 17, 2012.
- McTaggart F, Buckett L, Davidson R, Holdgate G, McCormick A, Schneck D, Smith G, Warwick M (2001). "Preclinical and clinical pharmacology of Rosuvastatin, a new 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor." Am J Cardiol 87
(5A):28B–32B. DOI:10.1016/S0002-9149(01)01454-0. PMID 11256847. - Rosuvastatin bound to proteins in the PDB
- Rosuvastatin (Crestor) Information (unavailable link - history
). eMedicineHealth (October 16, 2005). Archived from the original on July 15, 2006. - US National Library of Medicine: Drug Information Portal - Rosuvastatin
- Extended instructions for use of the drug "Rosuvastin"
Use during pregnancy
The feasibility of using the drug in the treatment of acute coronary syndrome has been proven by a number of clinical studies. However, the instructions for use indicate the impossibility of treating pregnant women.
In some cases, statins are used as prophylaxis for the development of preeclampsia. The action of the drug disrupts the biological synthesis of cholesterol in the fetus and causes developmental defects. Taking it causes the greatest harm in the first trimester of pregnancy. The toxicity of the drug is manifested by damage to the kidneys and muscles in pregnant women. Other factors also have an impact:
- uncontrolled dosage;
- surgical interventions;
- concomitant drug therapy.
If a pregnant woman is at risk, a diet containing sea fish is recommended; Cardiomagnyl or Cardioaspirin are prescribed if treatment is necessary. If pregnancy is diagnosed, statins should be stopped. However, there is evidence that when taken prophylactically, cerebral blood flow increases in patients with atherosclerotic disorders.
Links[ | ]
- Annual Report and Form 20-F, Information 2004 (unspecified)
(PDF) (link unavailable). AstraZeneca PLC (2005). Retrieved October 11, 2012. Archived May 13, 2005. - Annual Report and Form 20-F, 2003 (unspecified)
(PDF). AstraZeneca PLC (2004). Retrieved March 20, 2005. Archived May 13, 2005. - Highlights of Prescribing Information (unspecified)
(PDF) (unavailable link). AstraZeneca PLC (2008). Retrieved March 11, 2009. Archived December 17, 2012. - McTaggart F., Buckett L., Davidson R., Holdgate G., McCormick A., Schneck D., Smith G., Warwick M.
Preclinical and clinical pharmacology of Rosuvastatin, a new 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor (English) // Am J Cardiol (English) Russian. : journal. - 2001. - Vol. 87, no. 5A. — P. 28B—32B. - doi:10.1016/S0002-9149(01)01454-0. - PMID 11256847. - Rosuvastatin bound to proteins in the PDB
- Rosuvastatin (Crestor) Information (unspecified)
(unavailable link). eMedicineHealth (October 16, 2005). Retrieved October 11, 2012. Archived July 15, 2006. - US National Library of Medicine: Drug Information Portal - Rosuvastatin
- Extended instructions for use of the drug "Rosuvastin"
Precautionary measures
The question may arise: how to take Rosuvastatin correctly without fear of worsening your health if you have to undergo long-term treatment? First of all, it is necessary to control the consumption of grapefruit juice, since more than 1 liter of drink per day leads to an increase in the concentration of the drug in the blood.
During the period of acute liver inflammation, treatment with statins should be carried out under the supervision of a physician, since transaminase activity increases, and the value of ALT and AST is several times higher than normal. Patients suffering from diffuse myalgia may feel uncomfortable. After taking statins, they experience muscle weakness and lethargy.
The use of statins in women of reproductive age leads to increased serum glucose and unexplained muscle pain. If symptoms of diabetes develop, you should consult a doctor. The use of statins and antihypertensive drugs does not cause the appearance of undesirable clinical signs indicating their interaction.
Cholesterol-lowering drugs prescribed by a doctor maintain normal lipid balance. Atherosclerosis does not develop in a few days. The first signs of this process appear at 35 years of age. Therefore, you should always monitor your cholesterol levels, even at an age when there are no and cannot be problems with the heart and blood vessels.
How to take statins for cholesterol in the morning or evening
Statins are drugs that reduce the body's production of cholesterol.
They are prescribed for the prevention of cardiovascular complications of atherosclerosis: coronary artery disease, coronary heart disease, myocardial infarction, stroke.
For maximum effectiveness, it is important to follow the rules for taking medications. So, when is it better to take statins in the morning or in the evening, should you coordinate the time of taking with food or not?
Pharmacology of statins
Before answering the question of how and when is the best time to take statins, you need to understand their mechanism of action. Another name of the group, HMG-CoA reductase inhibitors, very well reflects their principle of action.
These drugs have the ability to block one of the enzymes, without which cholesterol synthesis is impossible. Contrary to its bad reputation, this sterol is essential for the body.
It is an essential component of all cell membranes, the main raw material for the synthesis of vitamin D and steroid hormones.
The body has to find backup sources of cholesterol. For example, the breakdown of low-density lipoproteins LDL is one of the main factors in the development of atherosclerosis. In addition to lowering cholesterol, taking statins increases the level of high-density lipoprotein HDL, improves the condition of the vascular wall, and prevents thrombus formation.
When is the best time to take statins: morning or evening?
If you have ever searched the Internet for answers to the question of how best to take statins, you have come across different opinions on this matter. The instructions for the medications contain a clear answer to the question of how to take statins in the morning or evening.
The maximum amount of cholesterol is synthesized at night. At this point, the concentration of statin in the blood should still be high. Then the drug will block the largest number of cholesterol formation reactions, which means it will more effectively reduce its concentration.
Each drug has a different half-life:
Accordingly, it is necessary to take statins that have a short elimination period (lovastatin, simvastatin, fluvastatin) in the evening. Otherwise, by the time cholesterol is actively synthesized, trace amounts of the drug will remain in the blood.
Atorvastatin and rosuvastatin are eliminated rather slowly and can be taken at any time of the day. Pitavastatin occupies an intermediate position. The instructions recommend taking the tablet before bed, but this is not a necessary condition.
How to take statins before or after meals
Food does not have a significant effect on the absorption and cholesterol-lowering effectiveness of almost all statins. The exception is the drug lovastatin, which must be taken with dinner. And although most pills may not be taken with food, it is very important what you eat.
The effectiveness of statins is very easy to negate. It is enough to consume a large amount of foods containing cholesterol, sugar, saturated fats, trans fats. The drugs do not affect the absorption of dietary sterol in any way.
If cholesterol intake is not reduced, the body compensates for the lack of synthesis through food. Naturally, the sterol level does not decrease. You should also limit your alcohol consumption and quit smoking.
The first one damages the liver, the drug load on which is increased, the second one damages the blood vessels.
If you have started taking 1st-3rd generation statins, you should not drink grapefruit juice. It contains natural components that block the transport enzyme necessary to remove the drug from the body. The concentration of the drug in the blood increases, and so does the risk of side effects. For example, drinking just one glass of juice a day increases the AUC of atorvastatin by 37%.
Other admission rules
There are a few more simple rules that will make medications as effective as possible:
- Statins must be taken as a whole, which increases the absorption of the drug. This does not apply to tablets that have scoring marks. Their composition is selected in such a way that it allows fractional doses of the medicine;
- Take the tablet with a few sips of water. There is no need to use tea, coffee, milk, juice or other drinks for these purposes;
- If you are taking HMG-CoA reductase inhibitors that do not have a daily schedule, choose a specific dosage time. Violation of the regime is undesirable. If the schedule is followed, the concentration of the drug in the blood is stable, which allows you to effectively reduce cholesterol. This does not happen if she is constantly jumping;
- If you miss a pill, but there are more than 12 hours left until the next one, take it as quickly as possible. Wait for the standard time if you remember the medicine too late. There is no need to increase the dose of the drug.
Literature
- Ann Pietrangelo. Why Should You Take Statins at Night? 2017
- Jacqueline H. Kostick, PharmD. Statins: Morning vs Evening Dosing? 2007
- Kama Awad, Maria-Corina Serban, Peter Penson. Effects of morning vs evening statin administration on lipid profile: A systematic review and meta-analysis, 2017
Last updated: January 21, 2020
Source: https://sosudy.info/kogda-prinimat-statiny-utrom-ili-vecherom
Side effects
Side effects on the body are classified according to the frequency of clinical studies:
- Quite often or very often, more than 1 case in 10 patients,
- Often this is 1 case in 100 patients,
- Not often this is 1 case in 1000 patients,
- Rarely 1 case per 10,000 patients,
- Very rare or isolated cases 1 case over 10,000 patients taking the drug Rosuvastatin canon:
| body systems and organs | negative reactions of the body | repetition rate |
| nervous system organs | · headache, | often |
| · dizziness, | ||
| asthenic syndrome, | quite rare | |
| memory loss, | ||
| · polyneuropathy. | #rowspan# | |
| human skeleton and muscle fiber tissue | myalgia disease, | often |
| pathology rhabdomyolysis, | occasionally | |
| myopathy disease, | isolated cases | |
| · pathology arthralgia. | ||
| digestive organs | · dyspeptic abnormalities, | often enough |
| · severe diarrhea, | often | |
| · constipation, | very rarely | |
| diseases in liver cells, | ||
| · growth of transminase index, | rarely | |
| manifestation of jaundice, | ||
| · pathology pancreatitis. | ||
| urinary system | · proteinuria, | rarely |
| swelling of the periphery, | ||
| · pathology hematuria. | ||
| endocrine system | · type 2 diabetes mellitus. | not rare |
| blood flow system | pathology thrombocytopenia | quite rare |
| allergy | skin rashes that cause severe itching, | often |
| · urticaria, | ||
| pathology erythema, | rarely | |
| Quincke's edema | ||
| respiratory system | · coughing, | often enough |
| sore throat, | ||
| shortness of breath. | ||
| common adverse reactions in the human body | · fatigue of the whole body, | not very often |
| · sexual dysfunction, | rarely | |
| · depressive state, | ||
| #rowspan# | · excess weight, | very rarely |
| · insomnia at night, | frequency was not tracked | |
| · nightmares in sleep. | ||
| renal organ failure | ||
| Interstitial lung pathology |
Nightmares in sleep side effect of medication