General information
Lymphedema, or elephantiasis, “elephantiasis”, elephantiasis - all these terms describe a condition in which swelling increases in the area of the extremities, most often the lower ones, thereby threatening a person’s motor activity . The disease causes chronic blockage of the lymphatic drainage pathways, which ultimately leads to the accumulation of toxins. Because of this, bacteria, harmful substances, and elements of leukocytes are not removed from the body, but continue to remain in the soft tissues.
Note! According to statistics, obstructed lymphatic drainage is diagnosed in every tenth person on the planet. At the same time, 10 million people have lymphedema caused by a chronic infection entering the body.
The risk group is primarily people suffering from peripheral vascular diseases. Up to 7% of them already have lymphedema, and this figure is growing steadily. The disease is difficult to treat. The success of the latter is determined not only by the correctness of the selected therapy, but also by the patient’s lifestyle.
How is the treatment carried out?
When dealing with lymphedema, it is recommended to follow some rules of behavior: if the patient has stage 3 or 4 of the disease, the success of therapy depends on minimizing external pressure on various parts of the body. It is not recommended to wear thick or very tight clothing. Injury should be avoided where possible. At the first signs of inflammation - redness, fever or chills - it is better to consult a doctor immediately.
Primary lymphedema
If lymphedema is caused by hereditary causes, complex therapy will be needed. Treatment includes:
- lymphatic drainage through tissue massage;
- drug therapy;
- hardware pneumocompression and compression therapy using special bandages or long-term compression stockings;
- gymnastics;
- caring for the skin of your feet (or hands) to prevent ulcers or injuries and subsequent infection;
- surgical intervention.
Drainage helps relieve blockages in lymph nodes
Manual lymphatic drainage, which is useful against primary lymphedema, is a form of massage. The goal of this treatment is to relieve blockage of the lymphatic vessels. The massage therapist applies pressure to the skin with their fingertips in the direction of the lymphatic vessels to release blocked lymph.
Treatment with certain medications may be helpful against primary lymphedema. Diuretics (diuretics) are useful in the initial stages of the disease; however, it is important that the patient does not take them in the long term. If skin inflammation recurs, long-term treatment with antibiotics may be required.
Benzopyrones (including Coumarin and flavonoids) are a group of drugs that have been successful in treating lymphedema. Benzopyrones help reduce excess fluid, reduce swelling, reduce skin temperature and reduce secondary infections.
It has been found that retinoids can effectively treat chronic skin changes caused by stage 3 and 4 lymphedema. These treatments are believed to reduce skin keratinization, inflammatory and fibrotic changes.
Ammonium lactate acts as a humectant when applied to the skin. In addition, the drug can reduce the likelihood of infectious skin diseases by 50%. In lotions, ammonium lactate is used to reduce eczema and itching.
Surgical treatment consists of creating bypass pathways for lymph drainage.
Secondary lymphedema
If the patient has secondary lymphedema, treatment is aimed at the underlying disease; for example, if lymphostasis is caused by a malignant tumor, complex therapy is required. Untested methods of alternative medicine are not used in the treatment of cancer. As a rule, chemotherapy and radiation are prescribed; treatment with cytokines or monoclonal antibodies.
Causes
Most often, the disease manifests itself as a result of disturbances in the functioning of the lymphatic system. They disrupt the normal flow of lymphatic fluid and, as a result, cause the development of edema. This fluid contains fats and proteins, which should normally be cleared in the lymph nodes and then travel further along the lymphatic pathways. However, when pathology occurs, the lymph flow is delayed.
If the disorders that provoke the obstructed outflow are congenital, for example, a person is diagnosed with underdevelopment, valvular incompetence or aplasia of peripheral lymphatic vessels, he is diagnosed with primary lymphedema . In this case, the disease appears already in childhood or adolescence, mainly in girls. In boys, the disease is diagnosed 4 times less often. In this case, both the lower and upper extremities can swell in everyone.
Also in medical practice, secondary or acquired lymphedema . It is characterized by changes in lymphatic drainage due to acquired blockage in the lymph nodes or destruction of lymphatic channels.
This happens for a number of reasons, including:
- Excess weight and cellulite.
- Surgical operations on the extremities, especially those affecting the lymphatic system.
- Serious injuries.
- Infectious diseases, for example, erysipelas, in which streptococci easily enter the body and provoke inflammation of the lymphatic vessels and thickening of their walls. As a result, lymph circulation deteriorates and clogged pathways appear.
- The entry of parasites into the body - pinworms, toxocara, roundworms.
- Decreased immunity, for example, due to a chronic severe illness or vitamin deficiency in the off-season.
- Chronic eczema.
- Long-term effects on the skin of negative factors - excessively low temperature, ultraviolet radiation when visiting a solarium.
- Working in hazardous work without proper protective equipment.
- Tumors of the lymphatic system or surrounding tissues, in which their metastases reach the lymph nodes. Sometimes lymphedema occurs after removal of these tumors as a result of disruption of lymph flow.
- Syphilis, especially untreated or neglected.
- Burns.
- Systemic autoimmune diseases, such as lupus erythematosus.
Varicose veins, thrombophlebitis, phlebitis and other diseases of the venous system.- The bite of mosquitoes carrying the nematode Wucheria bancrofti, which provokes filariasis and, as a result, lymphedema.
- Hodgkin's lymphoma.
- Cervical cancer, breast cancer, melanoma.
- Chronic heart failure.
- Portal hypertension.
- The procedure of lipectomy is the removal of fat from the thighs.
- Excision of scar tissue.
- Burns disease is osteochondropathy of the elbow.
- Streptococcal lymphangitis.
- The influence of ionizing radiation when a person lives in an area with high background radiation or undergoes radiation therapy.
Along with the reasons described above, congenital hyperproduction of tissue fluid can provoke the development of lymphedema .
The latter is the progenitor of lymphatic fluid and, concurrently, a factor influencing the increase in its quantity in the channel. Due to the fact that the lymphatic vessels cannot withstand the increased load, some of the lymph is retained in certain areas, accumulates and provokes swelling.
Types of surgical treatment
There are primary and secondary lymphostasis. Primary appears during puberty due to insufficiency of lymphatic vessels, which leads to stagnation of lymph. Secondary – the result of diseases of the lymphatic system.
- infections (including parasitic ones);
- injuries accompanied by damage to blood vessels and nodes;
- tumors of the lymphatic system;
- scars and other consequences of removal or irradiation of lymph nodes.
- Reversible lymphostasis of the legs is mild swelling, with an increase in the volume of the limb, without the proliferation of connective tissue. Treatment is carried out using massage, pressotherapy, compression hosiery and medications prescribed by the vascular surgeon;
- Irreversible edema is swelling with hardening of the skin and proliferation of connective tissue. Skin tension causes pain. In this case, an immediate visit to a doctor is required, who will prescribe the correct treatment regimen, a course of massage, and bandaging;
- The third stage is characterized by the formation of elephantiasis, fibrosis and cystosis. The limb becomes deformed, movement becomes difficult due to the development of osteoarthritis and heaviness in the legs.
Liposuction. Removal of fibrotic subcutaneous tissue by aspiration. Indicated for moderate proliferation of connective tissue.
Island dermatofasciolipectomy. Excision of affected areas of skin with fibrous tissue, fascia and subcutaneous fat. Several liposuctions are performed before insular dermatofasciolipectomy. The postoperative wound is closed with flaps of skin preserved in the operation area or taken from other areas of the patient’s skin.
Creation of lymphovenous anastomoses. These are bypass operations to connect lymph vessels with veins to improve lymph outflow. They are used for secondary lymphostasis, which develops mainly during radiation therapy of lymph nodes or after mastectomy. In case of primary lymphostasis, lymphovenous anastomoses have no effect. The essence of the operation is to connect the vessels of the lymphatic channel with the nearest vein by creating thin microanastomoses.
Tunneling. Creation of passages in tissues affected by lymphostasis to drain accumulated lymph beyond the boundaries of the affected area. The diverted lymph is absorbed into intact lymph vessels, which leads to the removal of edema.
Temporary tunnels are special prostheses or spiral drainage. To create permanent tunnels, spirals made of special inert material or sections of saphenous veins are used.
Tunneling is indicated in advanced cases of lymphedema, when it is not possible to apply other methods mentioned above. The tunneling effect is temporary.
For primary lymphostasis, a tissue lymphoid complex transplant is used. The essence of the operation is that a flap of skin with fasciola and healthy lymphatic vessels and nodes is transplanted onto the affected area. This ensures the outflow of lymph through intact nodes and vessels that serve as drainage.
After surgery, additional drug treatment is carried out. Every patient with lymphostasis should be observed by an angiosurgeon. The need for maintenance therapy usually continues throughout life.
Symptoms of lymphedema
Signs of the disease are determined by the type of lymphedema, meanwhile, doctors identify some symptoms that are common to all types of pathologies. This:
- Dense swelling. Initially, it is the result of stagnation of lymph in the affected area. After its prolonged exposure to surrounding tissues, areas of connective tissue appear that undergo fibrotic changes at the site of localization of the edema, thereby thickening the swelling.
- Discomfort, pain in the limbs. As a rule, they precede the development of edema. Unpleasant sensations decrease when a person changes body position, adopting one that improves lymph flow. This happens until the swelling increases, then the circulation of lymphatic fluid does not improve when changing positions and edema develops. Also at this stage, seizures may occur.
- Deformation of the affected limb. It occurs due to the accumulation of lymph in the same area.
- Changes in the structure of the skin. Swelling causes the skin to stretch, causing it to thicken and become pale and shiny. In some areas, the skin resembles the skin of an orange - it is covered with enlarged, large pores.
- A feeling of heaviness and fullness in the affected limb.
- Impaired mobility of the affected limb.
- Weakness, loss of strength.
Important! A simple test can help distinguish swelling due to lymphedema from other pathologies. When pressing on the affected, swollen area, dimples do not appear on the skin.
Signs and symptoms
The main symptom associated with lymphedema is swelling or puffiness in various parts of the body due to the accumulation of protein-rich fluid in the soft tissue layers under the epidermis (lymphedema).
Swelling often occurs in one or both legs, but can also appear on the torso, face, genitals and arms. When lymphedema develops in the legs, swelling is usually most noticeable in the foot and ankle.
In some cases, swelling can cause tightness, discomfort, and unusual tingling sensations in the affected areas. The affected area does not heal well even after minor trauma (such as a cut or insect bite).
Types and stages
Primary lymphedema, which is the result of disturbances in the lymphatic system, is divided into three types:
Melroy's disease. It accounts for up to 25% of all diagnoses. This is a familial disease that usually appears at birth or in the first year of a child's life. It mainly affects women, and most often it affects the lower extremities. The swelling is painless and in most cases is bilateral.- Mezha's disease, or lymphedema precox. The pathology can manifest itself after birth and up to the age of 35, although this mainly occurs during puberty. In 70% of cases, the left lower limb is affected; cases of bilateral damage are rare. Due to the fact that women are more likely to suffer from this type of lymphedema, it was concluded that it is related to the level of estrogen in the blood.
- Lymphedema of Tart. A disease whose symptoms begin after patients reach 35 years of age. Doctors believe that its cause is a defect in the lymphatic valves, as a result of which they cannot fully perform their functions. The defect can be congenital or acquired due to infection, trauma, tumor development, excess weight, or iatrogenicity.
Depending on the severity of clinical manifestations, 3 stages of lymphedema are distinguished:
- Initial – characterized by weak expression or no signs at all. Patients usually attribute minor swelling that appears during this period to changes in the weather. The heaviness in their limbs may increase in the evening, but, as a rule, it completely disappears after slight physical activity. This gives them a reason to forget about their condition, while prolonged ignoring of the signs causes the situation to worsen and the pathology to move to the next stage.
- Second. It is characterized by severe symptoms when body weight increases, loading the lower limbs, and the skin becomes rough and inelastic.
- Third. It is characterized by a severe course and the development of irreversible processes. At this stage, trophic ulcers may appear. The body is weakened, which entails sepsis, tissue necrosis or muscle atrophy. Motor ability is lost.
Scrotal lymphedema
In addition to lymphedema of the lower extremities, scrotal lymphedema may also form. Scrotal lymphedema is a dangerous male disease that is diagnosed in only 8% of the male population.
The reasons for the progression of this subtype of the disease may be problems with the kidneys and disturbances in the outflow of lymph.
The symptoms of the pathology are as follows:
- edema formation;
- redness of the skin on the genitals;
- itching and burning.
Lymphedema of the scrotum, in the absence of correct treatment, can lead to serious consequences, including amputation of the genital organ. With this subtype of pathology, folk remedies are not applicable.
Diagnostics
At the second and third stages of lymphedema, making a diagnosis does not cause difficulties, while at the initial stage it is complicated. The primary form of the disease resembles lipedema, post-thrombophlebic syndrome, and kidney disease.
Note! Making an accurate diagnosis is delayed due to vague symptoms and the need to use expensive equipment. Meanwhile, during the initial examination, the doctor collects an anamnesis, examines the affected limb, refers for blood and urine tests and, if necessary, for consultation with related specialists.
Additionally, the following are used for diagnostics:
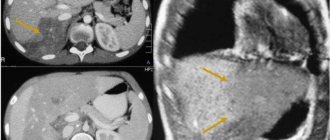
- Ultrasound to determine the volume and area of the lesion.
- Lymphangiography is an x-ray examination of the lymphatic system with the introduction of a contrast agent.
- Computed tomography to exclude or confirm a malignant course.
- Magnetic resonance imaging - it is used to assess obstructive processes in the secondary form of the disease or detect a cancerous tumor.
- Fluorescent microlymphography - allows you to identify microlymphatic abnormalities.
- Lymphoscintigraphy - gives a general assessment of the lymphatic system.
- Biopsy – performed to confirm the diagnosis, particularly in the presence of chronic ulcers.
Etiology
The following reasons may contribute to the development of lymphedema:
- chronic venous insufficiency;
- inflammation of blood vessels;
- vascular obstruction;
- infection.
There are primary and secondary types of the disease. The primary form can be diagnosed in children or be congenital. The secondary form can be provoked by the above factors and the following additional reasons:
- obesity;
- diseases that cause metabolic disorders;
- thoracic surgery, breast removal (mastectomy).
Treatment of lymphedema
Timely diagnosis is not the key to successful treatment, since the pathology has not yet been completely cured. At the same time, well-chosen therapy can alleviate the patient’s condition, as well as prevent or delay disability . Most often, treatment for lymphedema includes:
- taking medications that stimulate blood circulation;
- diuretics;
- phlebatropics;
- use of anti-inflammatory drugs;
- treatment with local ointments.
In extreme cases, doctors resort to surgical intervention, when the skin or subcutaneous tissue is excised to reduce the volume of the leg, plastic surgery is performed to improve the outflow of lymph, microsurgery is used to improve the condition of the lymph nodes, and an anastomosis is performed between the veins and lymphatic vessels.
Important! Lifestyle plays a huge role in the treatment of lymphedema. Avoiding salt and excessive fluid intake, as well as switching to plant-based foods and animal proteins help alleviate the situation. Additionally, patients are recommended to resort to the use of elastic stockings and socks, and undergo pneumopressotherapy (lymphatic drainage).
Treatment options
Conservative therapy
At the very beginning of the disease, medications perfectly stop negative changes, returning the person to the opportunity to lead a normal lifestyle.
For lymphedema, treatment is carried out with the following drugs:
- anti-inflammatory and antibiotics to suppress foci of infection;
- diuretics to relieve swelling;
- fortified food supplements to strengthen the walls of veins and canals.
Additionally, exercise therapy is prescribed. A special therapeutic set of exercises is designed to enhance natural lymph drainage, increase tone, improve metabolism and enhance the contractility of blood vessels and channels.
Eating wisely reduces symptoms. Necessary:
- limit salt and hot spices;
- reduce the amount of water and liquid foods;
- If you have extra pounds, reduce calories, remove all fatty and sweet foods.
A nutritious protein diet is part of rehabilitation and helps prevent recurrence of lymphedema.
It is useful to wear compression hosiery, which compresses the limbs and narrows the intercellular space. As a result, excess fluid is pushed out of the limbs and eliminated from the body. Doctors often recommend doing exercise therapy in just such stockings or socks.
Physiotherapy
For lymphedema, different types of physical therapy are used:
- electrophoresis;
- magnetic therapy;
- ultraviolet irradiation.
All procedures are aimed at combating muscle atrophy, improving blood circulation and lymph outflow.
Surgery
At the extreme stage, surgery becomes the only available way to:
- reduce pain syndrome;
- try to avoid disability.
There are several surgical options for treating lymphedema:
- removal of subcutaneous tissue and free areas of skin to reduce the volume of the leg;
- plastic surgery aimed at restoring lymph circulation in the extremities;
- microsurgery of blood vessels and lymph nodes;
- anastomosis.
Depending on the type of operation chosen, rehabilitation is prescribed and the length of hospital stay is determined.
Folk remedies
Allergic reactions are also rare. Natural components are easily taken and then eliminated even by a weakened body, but do not cure the disease.
The most popular recipes recommended by doctors:
- Boil 1 tablespoon of string leaves in a glass of water for 10 minutes and add to the foot bath. The procedure should be repeated twice a day for 20 days. The series has a powerful antimicrobial effect.
- 4 tbsp. l. 0.5 l of medicinal chamomile is poured. boiling water and leave in a water bath for half an hour. The course of administration is similar to the previous prescription.
- To increase hemoglobin levels, it is useful to consume 1 tbsp on an empty stomach. spoon of buckwheat flour for 14 days. You can buy ready-made flour in the store or make it yourself by grinding the cereal in a blender or coffee grinder.
- Diuretic tea is great for edema. To prepare the mixture, take rose hips, bearberry and currant leaves in equal parts. For a glass of tea take 2 tbsp. collection and pour boiling water. To preserve vitamins, it is better to cover the cup and wrap it in a towel for 30 minutes. Drink the drink on an empty stomach in the morning. The duration of admission is not limited.
Prognosis and possible complications
The doctor makes predictions depending on the form of the disease and the general health of the patient. With primary lymphedema, the chances of cure are minimal, although there is no talk of death. In case of secondary symptoms, patients are helped by well-chosen therapy, thanks to which they often successfully return to their previous life. Doctors are able to stop further blockage of the lymphatic vessels, but they are not able to turn back time.
The following complications are possible with lymphedema:
- development of infectious inflammation - trophic ulcers, eczema, erysipelas, fungal skin lesions;
- pathologies of the lymphatic system – lymphadenitis, lymphangitis;
- degeneration of damaged tissue – lymphangioscarcoma.
What is lymphedema?
Lymphedema is a pathological condition accompanied by increasing swelling of the soft tissues of the affected area
What is lymphedema? This is visible and palpable swelling of a part of the body that occurs as a result of stagnation of lymphatic fluid.
In the International Classification of Diseases, 10th revision (ICD-10), lymphedema is designated by codes I89.0, I97.2, Q82.0.
Lymph is a pale yellow fluid containing blood plasma and some white blood cells: lymphocytes. Lymph flows through the lymphatic vessels and enters the lymph nodes, where it is “filtered.”
The normal function of lymphatic vessels is to return proteins, lipids and water from the intercellular space to the intravascular space; 40-50% of whey proteins are transported through this pathway every day. Intercellular fluid helps nourish tissues. About 90% of the fluid returns to the bloodstream through the venous capillaries. The remaining 10% consists of high molecular weight proteins that are too large to easily pass through the venous capillary walls. Therefore, proteins travel through numerous filtering lymph nodes on their way to the venous circulation.
The swelling characteristic of lymphedema occurs when the movement of lymph in the lymphatic system is disrupted: chronic lymphatic stagnation retains fluid in the intercellular tissue, which leads to the development of edema. The damaged part of the body may change greatly in size. Swelling of the legs and arms is often the result of surgery in which lymph nodes were removed.
Lymphedema occurs very rarely; women are affected approximately 9 times more often than men. Lymphedema usually develops in young people between the ages of 15 and 20. Only about 17% of cases of lymphedema occur after age 35.
Symptoms
Regardless of the cause, any lymphedema is characterized by the following symptoms: the part of the body affected by lymphedema becomes swollen and noticeably increases in size. Pain does not usually occur with lymphedema of the lower or upper extremities.
In the early stages, the disease may be asymptomatic. This is why preventive screenings are so important. Timely detection of the disease helps prevent the development of complications of varying severity.
Lymphedema can sometimes have very different symptoms depending on the underlying cause. Based on clinical symptoms, it is possible to distinguish primary lymphedema (hereditary) from secondary (acquired).
Primary lymphedema often spreads to both sides of the toes and feet. Another typical manifestation of primary lymphedema of the upper and lower extremities is Stemmer's sign: the fingers take on a square shape when pressure is applied to their surface. Primary lymphedema subsequently spreads to the legs. The entire leg may change shape. Damaged skin is also susceptible to infection.
Secondary lymphedema has other symptoms. The disease spreads from the shoulder towards the arm or leg. Secondary lymphedema usually occurs on only one side of the body. The consequences may be the same as with the primary form.
Causes
The main reason for the development of pathology is blockage of the lymph nodes
Lymphedema of the upper as well as lower extremities can have many different causes. In most cases, blockage of the lymph nodes results in increased lymphatic pressure. Due to increased pressure in the vessels, lymph from the lymphatic channels enters the surrounding tissues. In rare cases, lymphedema is caused by changes in the composition of the lymph. Other causes include damage to genetic information or general diseases associated with stagnation of venous blood.
Primary lymphedema develops without obvious causes or due to a malformation (congenital abnormality) of the lymphatic system. Depending on the cause, primary lymphedema may be present at birth or develop throughout life.
Primary hereditary lymphedema is caused by an inherited developmental disorder. As a result, the patient has too few lymphatic vessels or they are severely deformed and are therefore unable to perform their function. The primary form often affects the legs on both sides and worsens during menstruation in women.
The main types of primary lymphedema:
- hereditary lymphedema type I (Nonne-Milroy syndrome): a congenital abnormality of the lymphatic system that causes congenital lymphedema;
- hereditary lymphedema type II (Meige syndrome): usually develops only during puberty. Girls suffer from the disease much more often than boys. Other symptoms include dwarfism, overweight and mental retardation.
Primary lymphedema, for which no cause can be identified, occurs primarily as a result of changes in the lymphatic vessels. The disease develops between the ages of 15 and 20 years. In 50% of cases, lymphedema is limited to one leg. Women are more likely to suffer from the disease than men.
Lymphedema that is caused by various acquired causes (for example, diseases, injuries) is called secondary. The main risk factors for the development of secondary lymphedema:
- injuries or sprains of the arm, leg, chest, as well as scars of various origins;
- removal of a breast tumor (after mastectomy);
- obesity: the increased risk of secondary lymphedema after breast cancer removal increases by 40-60% in obesity.
Not only the condition after removal of breast cancer is considered as a cause of secondary lymphedema. Various forms of cancer may also play a role in the development of lymphedema: Hodgkin's disease or some leukemias.
Other causes of secondary lymphedema:
- stagnation of venous blood;
- inflammation of the lymphatic vessels (so-called lymphangitis);
- chronic heart failure;
- portal hypertension;
- peripheral vascular surgery;
- lipectomy (removal of excess fat tissue);
- burns;
- insect bites;
- external pressure;
- Herpes simplex infection can cause lymphangitis and resultant lymphedema;
- parasitic diseases (filariasis, etc.).
Complications
If treated promptly, lymphedema does not cause complications.
Untreated lymphedema often leads to various complications: in addition to swelling of the soft tissues, channels open in the skin, allowing bacteria to penetrate into the subcutaneous space. If the disease progresses rapidly, serious skin damage can occur. If swelling occurs in the scrotum, it can increase significantly in size. Scrotal lymphedema can lead to erectile dysfunction.
In later stages, lymphedema causes severe inflammation and irritation of the skin. Blisters, scabs and eczema form on the affected areas. In addition, metabolic disorders often occur in the tissue of the affected limb. In the worst case, erosions or ulcers of varying severity may occur.
Complications of lymphedema also include hyperkeratosis, erysipelas, lymphangiosarcoma, relapses of lymphangitis, and deep vein thrombosis. Some patients may develop protein deficiency. Complications after surgery are common and include bruising, skin necrosis, and worsening swelling of the foot or hand.
Prevention
You can prevent the development of the disease by choosing comfortable underwear and shoes that do not restrict movement. However, it is not recommended to walk barefoot in public places, for example, on city beaches . It is also worth observing the rules of personal hygiene, regularly undergoing examinations by a doctor, and if any signs of illness occur, immediately contact him for advice.
Lymphedema is a serious disease that is difficult to correct, but thanks to proper treatment it slows down its progression. It is important to simply identify it in a timely manner and listen to the recommendations of a specialist.
Lotin Alexander, doctor, medical columnist
8, total, today
( 44 votes, average: 4.68 out of 5)
Reduced platelets in the blood of adults: what does this mean?
Hemophilia: causes, signs, treatment
Related Posts
Treatment with traditional methods
Treatment for lymphedema should only begin after visiting a qualified specialist and undergoing appropriate tests.
The main course of treatment, on the recommendation of a doctor, can be supplemented with folk remedies. At an early stage of the disease, this gives excellent results. However, in order to use any treatment methods, you need to know the reasons that triggered the progression of the pathology. Otherwise, even folk remedies in the form of decoctions and lotions can only worsen the situation.
Folk remedies for the treatment of lymphostasis:
- herbal decoctions;
- lotions;
- compresses.
Folk remedies for the treatment of illness can only be used in tandem with a course of treatment prescribed by a doctor. All recipes are selected strictly individually, since not always what helped one person will help another just as effectively.
Classification of lymphedema
There are two types of lymphedema:
- Primary (congenital) lymphedema, caused by congenital pathology of the lymphatic vessels, usually develops in childhood and adolescence (80% of patients are girls under the age of 18). More often it affects the lower extremities symmetrically, less often the upper extremities. In 6% of cases, hereditary lymphedema is observed (Nonne-Milroy syndrome, Meige syndrome). In other patients, primary lymphedema develops due to congenital aplasia or hypoplasia of the lymphatic vessels. Compensated primary lymphedema often progresses rapidly after pregnancy, trauma, or soft tissue infection.
- Secondary (acquired) lymphedema is caused by an infectious process (most often erysipelas), trauma, burn, surgery associated with the removal or damage of lymph nodes. It is most acutely expressed if the obstruction of lymph outflow is combined with a violation of venous outflow (during irradiation or extirpation of the inguinal and axillary lymph nodes). Secondary lymphedema is observed more often than primary lymphedema.
Complication of lymphedema
Due to lymphedema, tissue nutrition may be disrupted. The skin begins to crack, ulcers form, and lymphatic fistulas appear between the fingers. Lymphedema can be complicated by erysipelas. If the disease lasts for a long time, lymphangiosarcoma may occur.
Treatment of lymphedema
If there are no changes in the soft tissues, conservative treatment may be used. The patient must adhere to a special diet, perform physical therapy, and may need physiotherapeutic and balneological procedures. To reduce the volume of the affected limb, you need to wear a special bandage, variable hardware pneumocompression, and lymphatic drainage.
With the help of comprehensive treatment, the progression of lymphedema can be stopped.
In severe cases, surgery is used; for this, the lymphatic vessels can be stained; if this is done in advance, the lymphatic drainage can be brought back to normal. After long-term treatment, you can reduce skin swelling and improve subcutaneous tissue.
Lymphostasis of the lower extremities in children
The cause of lymphostasis of the lower extremities in children is most often a congenital pathology of the structure of the lymphatic system (underdevelopment of the valve apparatus, increased extensibility and thinning of the walls of the lymphatic vessels). Inadequately formed lymphatic vessels are not able to fully function and drain lymph from the subcutaneous tissue and muscles of the lower extremities.
At an early age, children usually have an improperly developed lymphatic system that still copes with its functions. However, as the child grows and develops and his physical activity increases, mild lymphedema begins to appear. They are most pronounced towards the end of the day, and disappear in the morning, after a night's sleep.
With the onset of puberty, hormonal changes occur in the body, against the background of which the condition of improperly formed lymphatic vessels worsens even more. As a result, lymphatic edema of the lower extremities quickly increases and becomes permanent. If treatment is not started, the child develops elephantiasis and long-term non-healing trophic ulcers appear.
Stages of the disease
Symptoms of lymphostasis of the lower extremities are directly related to the degree of its progression. So, there are 3 stages: first, second and third.
- Initial stage (reversible, lymphedema). This is mild swelling, which occurs more often in the evening or after physical activity, the cause is overwork. It completely disappears in the morning after a full rest and appears again by the end of the day. Localization area: ankle joint, base of toes. Swelling does not manifest itself as pain; the skin at the site of swelling becomes pale and folds form upon palpation.
- Second stage (irreversible, fibroedema). At grade 2, the signs are completely different, which is due to rapid progression. Unlike the 1st degree, the affected area rises higher, the skin does not form folds and swelling accompanies the patient 24/7. Rest doesn't help. Pain begins at the site of swelling. The skin changes color, becoming darker, turning blue. The skin in the area of edema weakens and any mechanical damage leads to the formation of wounds and ulcers. Fatigue of the limbs, even during normal standing, leads to convulsive conditions.
- The last stage (elephantiasis, elephantiasis, elephantism). The most severe form of lymphostasis with pronounced symptoms. Elephantiasis is named because of the significant enlargement of the legs and changes in the nature of the skin - dark color, roughness. Significant functional impairments of the legs are observed - due to the large volumes in the knee joint, they no longer bend. In addition to local symptoms, other manifestations may be observed: a general weakened state of the body, constant headaches, a white coating on the surface of the tongue, joint pain, and difficulty concentrating.
In the clinical course of lymphostasis of the lower extremities, three stages are distinguished:
- Transient mild swelling.
- Irreversible swelling (fibredema).
- Elephantiasis (fibrosis, cysts).