Autonomic dysfunction syndrome, what is it?
Autonomic dysfunction (AVD) is a syndrome characterized by functional disorders of the autonomic nervous system at the suprasegmental and segmental levels and the general condition of the patient. Currently, the complex of these autonomic symptoms is described by the term “somatoform autonomic dysfunction.” The validity of this diagnosis is still discussed in wide scientific circles.
Causes
The basic cause of such disorders is a violation of the nervous regulation of the autonomic nervous system, that is, the one that is responsible for the regulation and stability of the functioning of all internal organs and the entire organism as a whole. This is the part of the nervous system that a person cannot control - it does not obey consciousness. That is, considering VD to be a whim, spoiled behavior, or weakness is not only wrong, but even dangerous.
What disrupts the regulation of body activity at the level of nerve fibers? First of all, this is heredity - there are a huge number of families where all members have symptoms of autonomic dysfunction. Endocrine disorders and pathologies, including transient ones - during puberty, menopause, pregnancy - are also causes of the manifestation of VD.
Autonomic dysfunction is inevitable in those who lead a sedentary lifestyle, preferring an abundance of fatty foods and dishes with an excess of extractive substances. It is provoked by smoking, alcohol, frequent infectious diseases and chronic infection (carious teeth, tonsillitis, sinusitis), allergies, chronic fatigue syndrome, iatrogenic diseases, injuries, stroke.
Causes of the disorder
This syndrome often occurs as a result of the influence of mental or somatic disorders that a person already has. As a rule, autonomic disorders are a consequence of secondary dysfunction of the nervous, humoral and autonomic regulation of vascular wall tone in pathological conditions of various organs and systems.
Somatic pathologies include arterial hypertension, coronary heart disease, and diseases of the gastrointestinal tract. Mental disorders include depressive disorders and panic attacks.
Also, the causes of autonomic disorders include:
- Disrupted work and rest schedule;
- Excess body weight, obesity I, II and III degrees;
- Reduced physical activity during the day (sedentary lifestyle, which is especially typical for office workers);
- Spending long periods of time at the computer/TV/electronic gadgets;
- Alcohol abuse;
- Long history of smoking;
- Insomnia (insomnia), dyssomnia (sleep disorders);
- Chronic diseases in the stage of decompensation;
- Chronic infectious processes;
- Immunodeficiency conditions;
- Chronic stress, especially if it is present both at work and at home;
- Taking narcotic, psychostimulant or toxic drugs.
What is psychovegetative syndrome?
Psychovegetative syndrome or vegetative dystonia is a pathology that is accompanied by a violation of the autonomic functions of the body.
The disease is presented in the international classification of diseases. He is assigned a code according to ICD 10 - F45.3.
Reasons for violation
Neurosis is the main factor causing psychovegetative syndrome
Psychovegetative disorders are associated with the appearance of malfunctions in the functioning of different parts of the body. They often arise against the background of a discrepancy between a person’s physical development and the function of his endocrine system.
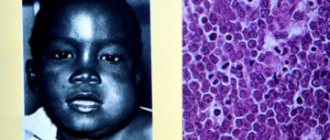
Most often, the pathology occurs in older children and adolescents. Rarely, the disease is diagnosed in men and women who have reached the age of forty.
The pathological process can be provoked by the influence of genetic factors and constitutional features of the structure of the human body. The influence of a disorder of the nervous system, which is organic in nature, cannot be ruled out. The syndrome is also caused by mental and somatic disorders.
Clinical signs of psychovegetative syndrome appear due to hormonal changes in the body. This factor explains the development of the disease in children and adolescents. Psychophysiological changes have no less influence on the development of pathology. Acute and chronic stress contribute to the deterioration of the general health of a person who is at risk.
The main factors causing the syndrome include the following diseases:
- Pathologies of the nervous system;
- Occupational diseases;
- Neuroses;
- Mental disorders;
- Psychosomatic disorders.
Any of these factors, if left without medical attention, will one day lead to the development of psychovegetative syndrome. The occurrence of complications that aggravate the course of the underlying disease cannot be ruled out.
Autonomic dystonia may well be caused by organic brain lesions. In this process, dysfunction of the peripheral nervous system is not the least important. Endocrine changes in the body top the list of main reasons that lead to the development of the syndrome. Therefore, adolescents and women going through menopause are at risk.
Doctors classify vegetative dystonia of a psychophysiological nature into a separate category. It is caused by frequent stress, excessive physical strain, neurotic disorders and overwork. These factors must affect the human body over a long period of time to lead to the syndrome.
Symptoms
Against the background of a general deterioration in well-being, which causes disruption of the body’s functioning due to autonomic dysfunction, patients experience specific symptoms. They enable doctors to suspect the course of this disease in a person.
As a rule, patients come to see a doctor with complaints of vegetative symptoms that do not allow one to determine a specific disease.
A person with such a diagnosis is disturbed by painful signs that usually appear in the presence of dysfunction of internal organs and systems. We are talking about the following symptoms of illness:
- Heart and blood vessels - tachycardia, rapid heartbeat, pain in the chest, increased or decreased blood pressure, lightheadedness and hot or cold flashes;
- Respiratory organs – the appearance of a feeling of a lump in the throat, lack of air, uneven breathing and shortness of breath;
- Nervous system – headaches, dizziness, trembling, tension in muscle tissue, sleep problems, paresthesia, chills and tremors;
- Digestive tract - dyspepsia, nausea, dry mouth, constipation, diarrhea, flatulence and problems with appetite;
- Genitourinary system – decreased libido, impotence, frequent urge to urinate.
With cerebrovascular and other disorders, general symptoms also occur that indicate a deteriorating state of health. Patients experience problems such as body weakness, motor restlessness, fidgetiness, muscle stiffness, inability to concentrate, memory loss and irritability. These are exactly the manifestations of vegetative dystonia. The symptoms of this syndrome are varied. Each patient has an individual range of painful symptoms with varying intensities.
Complications and consequences
Ignoring treatment of psychovegetative syndrome results in the development of frequent headaches
Experts have conducted a lot of research, trying to find out the causes of psychovegetative syndrome and the complications that it can cause. They concluded that ignoring treatment leads to the development of psychological and neurological disorders. The occurrence of cardiac problems cannot be ruled out.
The consequences of the syndrome, like vegetative-vascular dystonia (VSD), pose a threat to human health. Patients with psychovegetative syndrome are at risk of encountering the following complications:
- Decrease in the level of work of the heart muscle, the appearance of interruptions;
- Malfunctions of the urethra and frequent urge to go to the toilet;
- The appearance of symptoms of low or high blood pressure;
- Impaired function of the vascular system;
- Metabolic disturbances and a sharp decrease in body weight;
- The emergence of dependence on weather conditions;
- Disruption of the digestive system.
Complications of vegetative dystonia make its main symptoms, which made themselves felt at an early stage in the development of the disease process, more pronounced.
If the patient does not begin treatment for the disease, his condition will continue to worsen. Ignoring the problem results in the development of frequent headaches, anxiety attacks, neuroses, depression and increased psychological vulnerability. Because of the syndrome, a person becomes more irritable and apathetic.
Symptoms
Autonomic dysfunction syndrome has a polyetiological character. This explains the variability of symptoms. Symptoms of autonomic dysfunction are quite nonspecific. It is divided into 2 main groups. The first group of symptoms is characterized by the appearance of general complaints in the patient: a rise in body temperature to subfebrile levels, increased sweating, restlessness, tremor, a feeling of heartbeat.
The second group of symptoms is more specific and is characterized by complaints of dysfunction in one organ or one system.
Symptoms are often subjective and not confirmed by objective research:
- Headache, dizziness;
- Nausea;
- Bloating (flatulence);
- Dyspnea;
- Pain in the heart area;
- Vegetative crises;
- Neurogenic syncope;
- Orthostatic hypotension;
- In men - impotence;
- Angina;
- Decreased mood (hypotymia);
- Paresthesia of the upper and lower extremities (feeling of “pins and needles” crawling across the body);
- Cardiophobia (fear of death, fear of cardiac arrest);
- General weakness, decreased performance;
- Impaired urination (it may be difficult or, conversely, more frequent);
- Dissomnia disorders;
- Dysmenorrhea in women;
- Swelling of the face in the morning;
- Unpleasant sensations throughout the body.
Symptoms are combined into syndromes. Thus, the main clinical syndromes are:
- Cardialgic;
- Tachycardial;
- Asthenic;
- Astheno-neurotic;
- Hyperkinetic;
- Myocardial dystrophy syndrome;
- Respiratory distress syndrome.
The classification proposed by Nikitin and Savitsky is most widespread in clinical practice. It includes three syndromes - cardiac , hypertensive and hypotensive. This principle of dividing symptoms is based on the predominance of vagotonic or sympathicotonic manifestations.
Symptoms of somatoform disorders
There are 5 types of somatoform disorders: hypochondriacal, somatized, chronic somatoform pain disorder, undifferentiated somatoform disorder and somatoform dysfunction of the autonomic nervous system.
Hypochondriacal disorder
is manifested by expressed fears for the presence of a serious incurable disease, for example, cancer or progressive ischemic disease, which supposedly at any time can cause a heart attack and death of the patient. A patient's "presumptive diagnosis" depends on the symptoms present. The distinctive features of this type of somatoform disorder are numerous senestopathies, constant fears about one’s health and accompanying affective disorders - anxiety, sadness, hopelessness, despondency. Against this background, characteristic hypochondriacal depression often develops.
Patients with this somatoform disorder are very persistent in their desire to identify their supposedly incurable illness and find professional help. Prompted by anxiety and fear for their health, they again and again turn to various doctors, asking or demanding repeated examinations. Another characteristic feature of this type of somatoform disorder is the instability of ideas about the presence and severity of the disease. The “presumptive diagnosis” may change: today a patient with hypochondriacal somatoform disorder is more worried about coronary disease, in a month – about a possible stroke or prostate cancer. The level of fear also changes: today the patient believes that the end is near and is completely immersed in hypochondriacal experiences; tomorrow he hopes that he will “hold out for a while.”
Somatization disorder
– a type of somatoform disorder in which intrapsychic conflicts are expressed at the level of the body, in the form of somatic symptoms. It differs from hypochondriacal disorder in the emotional perception and interpretation of pathological manifestations. A patient with hypochondriacal somatoform disorder fears for his health, worries about imminent death or severe suffering. A patient with somatization disorder is convinced that his pain is caused by a physical illness, and the task of doctors is to identify this illness and provide appropriate help.
Patients with this somatoform disorder react extremely negatively to specialist attempts to point out the psychological nature of their symptoms. They deny the presence of a psychological problem and often conflict with doctors. Complaints in this somatoform disorder are varied, atypical for a somatic disease, but quite constant compared to hypochondriacal disorder. Somatization disorder is accompanied by a persistent decrease in mood, depression or increased anxiety is possible.
Somatoform dysfunction of the autonomic nervous system
– somatoform disorder accompanied by the occurrence of vegetative symptoms. Caused by disruption of the activity of organs controlled by the autonomic nervous system. Complaints are variable and nonspecific. Possible pain in the heart, tachycardia, urination problems, shortness of breath, sweating, gastrointestinal disturbances, fever to subfebrile levels, fluctuations in blood pressure and other pathological manifestations.
As with other somatoform disorders, patients associate their symptoms with some kind of physical illness, but persistent fear of an incurable disease (as with hypochondriacal disorder) or conflict and belief in the purely somatic nature of symptoms (as with somatization disorder) are less pronounced. As in other cases, there is a lack of recognition of the psychological nature of the somatoform disorder, but the reaction to the doctor’s message about the absence of physical disorders more often proceeds according to the asthenic type.
Chronic somatoform pain disorder
manifests itself as constant pain. The pain in this somatoform disorder is debilitating, painful, occurs for no apparent reason, and is localized in the same place, usually in the area of the heart or stomach. The nature of the pain remains virtually unchanged over time, and there are no autonomic or neurological disorders.
Undifferentiated somatoform disorder
– a disorder in which patients present numerous complaints characteristic of the group of somatoform disorders, but these complaints do not fit into the clinical picture of the types of disease listed above.
Stages and forms
There are various forms (according to A.M. Vein):
- Constitutional nature;
- Against the background of hormonal changes;
- Psychophysiological nature;
- Against the background of somatic diseases;
- Against the background of occupational diseases;
- For nervousness and mental disorders.
Also, autonomic disorders are often divided into generalized, systemic and local forms. Local forms of autonomic dysfunction are characterized by damage to the peripheral nervous system, and generalized forms are characterized by impaired functioning of suprasegmental autonomic structures.
Autonomic dysfunction syndrome is also characterized by the presence of degrees of severity:
- Lightweight;
- Moderate severity;
- Heavy.
The severity is determined by the severity of tachycardia, the level of blood pressure (hypertension or hypotension), the severity of pain, as well as the frequency of vegetative crises.
Symptoms of the disease
Autonomic disorders differ in 3 directions, which is caused by weakening or strengthening of the activity of the sympathetic and parasympathetic systems.
Manifestations of pathology are as follows:
1. Activation of the sympathetic system. Symptoms affect cardiac activity. Cardiovascular dystonia occurs, which is expressed in increased heart rate and surges in blood pressure. The patient experiences discomfort, nervousness and headache. Cases of presyncope are common. A person is afraid of dying suddenly, loses peace and sleep.
2. Excessive activity of the parasympathetic nervous system. As the heart rate decreases, the patient experiences weakness and dizziness. The limbs become cold and lose sensitivity. Insufficient blood flow causes disturbances in the functioning of internal organs. The patient suffers from diarrhea and constipation. In some cases, involuntary urination and defecation occur.
3. Variable activity of nervous subsystems. Lack of coordination in their activities leads to the fact that an attack of dystonia is of a mixed nature. It can begin with symptoms that are inherent in the first direction, and end with manifestations characteristic of the second.
In cases where the disease affects the respiratory system, the patient experiences attacks of suffocation. He experiences shortness of breath and fear of suffocation due to lack of air. As a rule, painkillers do not help relieve pain during an attack.
Disturbances in the functioning of the autonomic system begin to appear in early childhood. Children with this diagnosis are prone to colds. They are passive, get tired quickly, complain of weakness and headache. As a rule, with age, such symptoms disappear or become less pronounced. If this does not happen, then you need to consult a doctor.
The course of the disease depending on age
Autonomic dysfunction syndrome is quite widespread: it occurs in more than 30% of patients who seek medical help. In children, adolescents and young adults, the incidence of this pathology is up to 30%. This is explained by hormonal changes that occur in a young body. In the older age group, the root causes of the development of autonomic disorders are considered to be chronic diseases (pancreatitis, gastric and duodenal ulcers), infectious processes, smoking and physical inactivity.
Also, the educational load, huge information flows and a sedentary lifestyle have a significant impact on the incidence of students.
Diagnostics
Diagnosis of autonomic dysfunction syndrome has significant difficulties associated with the lack of a clearly defined etiology of the disease and objective research methods. A patient seeking medical help should be carefully examined to identify the primary causes of certain symptoms. As a rule, the diagnosis of “autonomic dysfunction” is established by excluding cardiovascular diseases, pathologies of the respiratory and other systems.
Diagnostics is based on the following data:
- The patient’s complaints, the dynamics of their development;
- History of the disease (when the symptoms appeared, how they began, how they changed, their dynamics);
- Compounded hereditary history (presence of cardiovascular diseases or diabetes mellitus in parents under the age of 55 years);
- Determination of blood pressure (at rest and during functional tests) and heart rate;
- Electrocardiography and echocardiography to exclude pathology of the cardiovascular system;
- General and biochemical blood test to exclude pathologies of other organs;
- General urine analysis;
- Chest X-ray and spirometry for pronounced symptoms from the respiratory system;
- Bicycle ergometry allows you to adequately assess your heart rhythm.
Of particular importance is differential diagnosis with other diseases.
Diagnosis and treatment
Patients can go from doctor to doctor for months with similar complaints. They usually start with general practitioners, then it is the turn of a cardiologist, gastroenterologist, surgeon, until finally they reach a neurologist or psychoneurologist, whose competence this condition includes.
Data from the anamnesis, functional and instrumental studies (usually all of them have been completed by this time: ECG, CT, EEG, 24-hour monitoring, FGDS, laboratory tests) clearly indicate the absence of organic pathology, which becomes the reason for differential diagnosis with neuropsychiatric diseases and the formulation diagnosis of autonomic dysfunction.
Treatment should begin immediately and be as complete as possible. You should not hope that normalizing your diet, daily routine and quitting smoking will instantly solve the problem - the nervous system has been weakened for years, and it needs to be thoroughly treated.
Undoubtedly, maintaining a healthy lifestyle (optimal nutrition, proper rest, giving up bad habits, playing sports) is the most important factor in treatment.
Medicines will help stabilize the body’s functioning and support it at first. Daytime tranquilizers, nootropics, sleeping pills, cardiac, antidepressants, and vascular drugs are used. Taking adaptogens, vitamins, physiotherapy, massage, and a swimming pool are effective.
Treatment methods
Treatment tactics for autonomic dysfunction syndrome depend on symptoms and concomitant diseases. In most cases, therapy is complex and based on the clinical picture of the disease.
Drugs
An obligatory component of treatment is the impact on autonomic disorders with their subsequent correction.
- Angiotensin-converting enzyme inhibitors (enalapril) and sartans are used for hyperactivation of the sympathoadrenal system in tachycardial and cardialgic syndromes;
- Beta blockers;
- The use of melatonin-type drugs (melaxen, circadin) is justified by the fact that autonomic dysfunction syndrome is often accompanied by a disruption of normal circadian rhythms;
- Antiasthenic drugs with a vegetative stabilizing effect (enerion, ladasten);
- Vitamin therapy: B vitamins;
- Nootropic drugs with antiparoxysmal effects (phenibut, phenotropil);
- Antiasthenic drugs with adaptagen properties;
- Psychotropic drugs with anxiolytic effect (tenoten, atarax);
- Antidepressants are prescribed for severe VSD. In addition to antidepressant, they also have anti-anxiety, analgesic, stimulating, sedative and anti-anxiety effects.
Physiotherapy
Physiotherapy is the use of physical factors for therapeutic purposes.
Among the methods of physiotherapy used to treat vegetative-vascular dystonia, the following are actively used:
Electrotherapy is a method of physiotherapy that involves the use of electrical energy, magnetic and electric fields. This category includes galvanization and electrophoresis.
- Galvanization stimulates metabolic and trophic processes, improves lymph and blood circulation in tissues;
- Medicinal electrophoresis is used to achieve a calming effect in patients with severe cardialgia, hypertensive syndrome and rhythm disturbances. For different symptoms, the use of different concentrations of medicinal substances is indicated;
- Electrosleep has found wide application in the hypotensive form of autonomic dysfunction. These procedures are carried out daily, and the course is no more than 20 procedures;
- Aeroion therapy involves the use of aeronizers for both individual and collective use. In the process of air ionization, positively and negatively charged air ions are formed. The effect of aeroion therapy leads to a decrease in blood pressure and heart rate, improved sleep, a decrease in headaches and weakness;
- Acupuncture;
- Massotherapy;
- Water procedures (especially using hardening elements);
- Sun and air baths.
Treatment at home
Since autonomic dysfunction syndrome is characterized by rather disparate symptoms, treatment should also have an integrated approach. In addition to drug therapy, herbal adaptogens are widely used - ginseng, eleutherococcus, Chinese lemongrass.
Non-drug treatment of autonomic disorders includes the following methods:
- Maintaining a healthy lifestyle;
- Getting rid of bad habits (smoking, drinking alcohol);
- Night sleep at least 8 hours a day;
- Dosed physical activity;
- Balanced diet;
- Psychocorrection for mental disorders.
Pharmacotherapy
There is no single standard for how to treat vegetative-vascular dystonia. Most neurologists are of the opinion that taking medications only aggravates the situation - a person needs to radically reconsider his lifestyle. If you find and eliminate the provoking factors, you will be able to cure VSD without pharmaceutical drugs.
However, in order to make the patient feel better, symptomatic therapy is carried out. So, with high blood pressure, antihypertensive drugs are prescribed. Or, on the contrary, if a person is prone to hypotension, tonic medications are recommended. Sedatives help eliminate nervous excitability, preferably using plant materials - valerian, hawthorn, or motherwort, lemon balm.
Most often, not a single doctor will tell you how to cure VSD once and for all. In severe cases of pathology, they resort to the help of anxiolytics, antidepressants, and psychocorrectors. In order to improve blood circulation in the brain and in the area of internal organs, courses of medications such as those that expand and accelerate blood flow can be prescribed.
All medications are prescribed for VSD on an individual basis, after careful analysis of information from diagnostic procedures and exclusion of other causes of deterioration in well-being. Whether it is possible to cure VSD forever, the doctor explains to the patient in a personal conversation, after the basic treatment measures have been completed.
Possible complications and consequences
Often, with autonomic dysfunction, paroxysmal conditions may develop that require immediate medical attention. This indicates the importance of a correct diagnosis and timely initiation of therapy to avoid the development of such phenomena. Paroxysmal states include vegetative crises and panic attacks. The clinical picture is represented by the following symptoms:
- Increased sweating;
- Rapid heartbeat (more than 90 beats per minute);
- Shortness of breath, difficulty breathing;
- Tremor of the limbs;
- Suffocation;
- A sudden fear of death;
- Feeling of heat or, conversely, cold.
During the interictal period, symptoms become more “mild” in nature.
side of the respiratory system, difficulty breathing and shortness of breath are observed. Dyspeptic symptoms and abdominal pain from the gastrointestinal tract. Also characteristic is a number of nonspecific symptoms that appear when the thermoregulatory, sweating and vestibular systems are disrupted. As a rule, the development of serious complications occurs when there are errors in the diagnosis of diseases and, as a consequence, the lack of adequate and timely treatment of the underlying disease.
Pain in the heart area
Psychogenic cardialgia is pain in the heart area due to dysfunction of the ANS, which can occur at any age. At the same time, the electrocardiogram, the results of ultrasound of the heart and other studies are normal.
With psychogenic cardialgia, the pain is stabbing, radiating to the shoulder blade, left arm, and right half of the chest. It is caused by excitement, overwork, and may be associated with changes in weather. The pain is not associated with physical activity. When palpated, painful sensations are revealed in the area of the pectoral muscle, between the ribs, on the left shoulder and forearm along the nerve.
Pain may be accompanied by:
- Rapid heartbeat;
- Arrhythmia;
- Irregularities in blood pressure;
- Shortness of breath without exertion;
- Attacks of sweating;
- Panic attacks that appear at night.
Psychogenic cardialgia disappears after taking sedatives. But if ANS dysfunction is not treated, chest pain reappears during emotional stress.
Preventive measures
Prevention of autonomic dysfunction is of particular importance in preventing the development of complications and is based on the following principles:
- Physical activity in accordance with the functional capabilities of the body;
- Rational balanced nutrition;
- Psychotherapy;
- Maintaining sleep and wakefulness;
- Minimizing stress in a person’s life;
- Treatment of chronic diseases;
- Observation by a general practitioner, modern detection and treatment of diseases;
- Vitamin therapy;
- Fighting excess weight;
- Sanitation of foci of chronic infections;
- To give up smoking;
- Refusal of alcohol abuse.
Source: nervy-expert.ru
Help for patients with somatoform disorders involves a complex of therapeutic interventions aimed at relieving clinical manifestations and including, along with psychotherapy, drug treatment with psychopharmacological and restorative drugs, physiotherapy, and exercise therapy. When treating somatoform disorders, the anxiety-depressive symptoms accompanying the above disorder, personal characteristics, and the presence of highly valuable ideas are taken into account. For this purpose, it is necessary to use a complex of drugs with a pronounced antidepressant effect. In the treatment of somatoform disorders, it is also possible to use beta-blockers (propanolol, Trazicor, Obzidan, etc.). The selection of psychopharmacotherapy and the choice of medication or their complex is carried out strictly individually, taking into account the variety of clinical manifestations, individual tolerance of drugs, with a gradual selection of the optimal therapeutic dose for a given patient.
List of medications used and their dosage
1. Diazepam - at the beginning of therapy, parenteral administration of the drug at a dose of 20-80 mg/s is necessary. in 3-4 doses during the first ten days, followed by transfer to oral administration of 20-40 mg/s. in 3-4 doses over 7-10 days.
2. Amitriptyline - at a dose of 50-150 mg/s. for 30 days in 3-4 doses. It is used to relieve somatoform and anxiety-depressive symptoms.
3. Chlorprothixene - 30—
100 mg per day for 10-20 days in 3 divided doses.
4. Imipramine - 50-150 mg/s. in 2 doses in the first half of the day. It is used to relieve depressive symptoms accompanied by motor and ideational retardation (adynamic, apathetic component), and algic disorders.
5. Fluoxetine – 20-60 mg/s. 4-6 weeks in the first half of the day in 1-2 doses in 30% of cases. Unlike amitriptyline and melipramine, it does not cause difficulty urinating, does not have a cardiotoxic effect, is easy to use, and is used once a day.
6. Fluvoxamine 100-150 mg per day for up to 30 days of use. It is used to relieve somatoform and anxiety-depressive disorders.
7. Trifluperazine 5 mg/s. in 2 doses. It is used to eliminate overvalued ideas and psychopathological personal reactions.
8. Risperidone - oral solution 30 ml 2-6 mg/s. in 1-2 doses. It is used to eliminate overvalued ideas, psychopathological personal reactions, and affective disorders.
9. Carbamazepine - 200-400 mg/s. in 2 doses.
10. Trihexyphenidyl - used to prevent adverse extrapyramidal disorders, 2 mg 3 times a day (daily dose 6 mg).
List of essential medications: 1. *Diazepam 0.010 g, tablet, 0.5% - 2 ml, amp. 2. *Amitriptyline 0.025, 0.01, tab., 1% – 2 ml, amp. 3. Chlorprothixene 50 mg, tablet, dragee 4. *Fluoxetine 0.02 g, caps. 5. *Imipramine 0.025 g, tablet, 1.25% - 2.0 ml, amp. 7. *Fluvoxamine 0.05 g, tab. 8. *Carbamazepine 0.1, 0.2 g, table.
List of additional medications: 1. *Trifluoperazine 0.005 g, table. 2. *Risperidone oral solution, 30 ml, vial. 3. *Trigexyfinidyl 0.002 g, table.
Source: diseases.medelement.com
Symptoms of autonomic dysfunction
The symptoms are so varied that before a correct diagnosis is made, the patient may mistakenly turn to different specialists for a long time.
The main manifestations of a disorder of the autonomic nervous system vary depending on the type of dysfunction, but the main ones can be identified:
- tachycardia, pain in the heart, feeling of heart failure;
- the patient feels a lack of air, spontaneous attacks of shortness of breath appear;
- jumps in venous and blood pressure;
- impaired blood circulation in tissues (especially in the extremities);
— periodic fluctuations in body temperature are observed (from 35°C to 38°C);
— possible disturbances in the gastrointestinal tract (diarrhea, constipation, vomiting, belching);
- a state of general weakness, lethargy, decreased performance, irritability, dizziness, frequent mood swings, sleep disturbance, anxiety, periodic startlings during sleep.
Disorders of the autonomic nervous system
Disturbances in the autonomic innervation of organs and tissues can occur due to damage in various parts of the autonomic nervous system.
Damage to the hypothalamus
The highest integration and organizational center of all autonomic functions is the hypothalamus. Although it does not have pinpoint, clearly defined centers, it has been established that stimulation of the anterior hypothalamus causes autonomic reactions associated with activation of the parasympathetic nervous system (decreased blood pressure, bradycardia, decreased breathing, etc.).
Irritation of the posterior hypothalamus leads to an increase in the tone of the sympathetic nervous system and the appearance of corresponding autonomic reactions - increased blood pressure, tachycardia, increased breathing (Fig. 135).
The hypothalamus is not only the center of the autonomic nervous system, but also functions as an endocrine organ. Currently, 7 releasing factors of the hypothalamus have been identified that regulate the activity of the pituitary gland. These are factors that stimulate the pituitary gland to release ACTH, growth hormone, thyrotropin, follicle-stimulating hormone, luteinizing hormone, as well as a factor that inhibits the pituitary gland to release melanocyte-stimulating hormone. If we also take into account that the hormones oxytocin and vasopressin (antidiuretic hormone) are formed in the neurosecretory nuclei of the anterior hypothalamus and then deposited in the posterior lobe of the pituitary gland, the hypothalamic-pituitary gland system should be considered as a single endocrine complex. Therefore, pathological processes resulting from damage to various parts of the hypothalamus and pituitary gland must be analyzed from the point of view of disruption of the activity of this most important endocrine apparatus.
With lesions (trauma, tumor, hemorrhage, etc.) in the area of the autonomic nuclei of the hypothalamus, various autonomic disorders occur depending on the location of the damage.
Damage to the nuclei of the anterior hypothalamus causes disturbances in carbohydrate metabolism. Activation of the transition of glycogen to sugar develops, an increase in blood sugar levels and a condition such as a transient form of diabetes mellitus. Damage to the supraoptic nucleus of the anterior hypothalamus is accompanied by disruption of the hypothalamic-pituitary connections with the posterior pituitary gland. The secretion of antidiuretic hormone decreases. As a result, an increase in urine output occurs - polyuria. When the body is dehydrated, the neurosecretion of these hypothalamic nuclei increases. This causes an increase in the secretion of ACTH and aldosterone. The reabsorption of water in the tubules increases. Urination decreases.
Destruction of the posterior and middle hypothalamus inhibits the secretion of corticosteroids.
Electrical stimulation of the nuclei of the posterior hypothalamus (implantation of electrodes) increased the secretion of corticosteroids. Irritation of the posterior areas of the gray tuberosity and mamillary bodies also caused the secretion of corticosteroids and lymphopenia.
Damage to the cells of the nuclei of the middle hypothalamus causes a disorder of the autonomic innervation of the salivary glands of a parasympathetic nature and is accompanied by increased salivation. The middle hypothalamus also contains areas whose damage affects heat regulation.
Damage to the area of the ventromedial nuclei leads to disruption of fat metabolism. Severe obesity occurs due to polyphagia and inhibition of fat oxidation processes. Damage to the nuclei of the posterior hypothalamus, according to some data, causes inhibition of the synthesis of blood proteins. Of particular importance is the effect of damage to this part of the hypothalamus (lateral hypothalamic nucleus and tuberomammillary nuclei) on mineral metabolism. Damage to these, as well as the nuclei of the middle part of the hypothalamus (ventromedial, dorsomedial; infundibular nuclei, etc.) causes a significant change in mineral metabolism.
Increased sodium excretion in urine. This effect is realized through a decrease in the effect of neurosecrets from the above sections of the hypothalamus on the cells of the anterior pituitary gland. There is inhibition of the secretion of adrenocorticotropic hormone from the pituitary gland and aldosterone from the adrenal cortex, which is known to delay the release of sodium from the body.
The hypothalamus can influence the activity of the gastrointestinal tract. For example, irritation of the anterior part of the hypothalamus causes increased intestinal motility, and irritation of the posterior part of the hypothalamus causes its inhibition. It was noted that lesions of the hypothalamus at the level of the gray tuberosity caused gastric hemorrhages, peptic ulcers and gastric perforation in monkeys.
The separation of the hypothalamus from the pituitary gland causes atrophy of the thyroid gland. In turn, removal of the thyroid gland inhibits neurosecretion of the nuclei of the anterior hypothalamus.
Thus, there is feedback in the form of mutual regulation of the functions of the thyroid gland and hypothalamus.
Destruction of the parasympathetic (lateral) nuclei of the hypothalamus in rats leads to early abortion, and at the end of pregnancy causes premature birth. Stimulation or destruction of the sympathetic (ventromedial) nuclei in cats and rats did not affect the course of pregnancy.
The destruction of the ventromedial nuclei significantly affects the ovarian-menstrual cycle. Animals stop estrus, the weight of the uterus increases, and the corpus luteum in the ovary disappears. These changes are accompanied by obesity.
Damage to sympathetic innervation
Experimentally, in several steps, you can remove all nodes of the sympathetic chain and paravertebral nodes in a cat and study the vital functions of such an animal. This operation is called complete desympathization. Let us recall that removal of the sympathetic chain, i.e., all nodes bordering the spinal column, disrupts the vasomotor and trophic innervation of many organs. As a result, there is a loss of many functions, among which the influence of desympatization on blood circulation, metabolism, the activity of smooth muscle organs, etc. is of particular importance. The effect of desympathization on blood circulation is reflected in the loss of the vasoconstrictor effect on the arterioles of many areas of the body with sympathetic innervation. Arterioles dilate and blood pressure drops. Turning off the sympathetic innervation of the heart (Pavlov's amplifier nerve and other nerves) leads to a weakening and slowing of heart contractions. These effects, however, can be compensated for by a reflex from the baroreceptors of the blood vessels caused by a drop in blood pressure. The weakening of baroreceptor irritation caused by a drop in blood pressure reduces the flow of impulses along sensory fibers to the center of the cardiac branches of the vagus nerve.
A decrease in reflex stimulation of the cardiac centers of the vagus nerve causes a decrease in their tonic excitation. This causes a decrease in the tonic influence of the vagus nerve on the heart, the heart leaves its influence (the “escape” phenomenon) and tachycardia develops.
The effect of desympatization on smooth muscle organs is expressed in the loss of the effect of sympathetic innervation on the function of a particular organ. For example, removal of the superior cervical sympathetic ganglion in a rabbit or cat is accompanied by constriction of the pupil (loss of the pupil-dilating influence of the sympathetic nerve) and dilation of the arteries of the ear due to loss of the vasoconstrictive influence of the sympathetic nerve.
The loss of influence of the sympathetic nervous system on the gastrointestinal tract is accompanied by activation of the motor function of the stomach and especially the intestines, since sympathetic innervation inhibits the movements of the stomach and intestines.
Sympathetic innervation of the smooth muscle sphincters of the bladder and anus ensures the relaxation of these sphincters, and the loss of sympathetic innervation contributes to their spastic contraction. The same is the relationship of sympathetic innervation to the sphincter of Oddi, which regulates the flow of bile from the gallbladder.
Desympathization causes inhibition of oxidative processes, a drop in the animal’s body temperature, hypoglycemia, lymphopenia and neutrophilic leukocytosis. There is a decrease in calcium content and an increase in potassium content in the blood.
It is clear that during phenomena of irritation of the sympathetic nervous system, all of the indicated changes in metabolism and functions of smooth muscle organs occur in the direction opposite to that described.
Damage to parasympathetic innervation
Parasympathetic innervation disorders can occur due to:
- 1) increased excitability and excitation of the parasympathetic division of the autonomic nervous system;
- 2) inhibition or loss of parasympathetic innervation of organs.
Perversions of the functions of the parasympathetic system are also possible. These are called amphatonia or dystonia.
Increased excitability and stimulation of the parasympathetic nervous system . Increased excitability of the parasympathetic nervous system can occur against the background of hereditary constitutional influences in the form of so-called vagotonia. As an example of such a condition, we can point out the thymic-lymphatic condition - an enlargement of the thymus gland and lymph nodes, in which even weak irritations of the vagus nerve, for example, electric current or mechanical (a blow to the epigastric region), can cause instant death from cardiac arrest (vagal death ). This condition is often an expression of general autonomic neurosis, in which, simultaneously with an increase in the excitability of the parasympathetic part of the autonomic nervous system, the excitability of its sympathetic part increases.
Irritation of the parasympathetic (vagus) nerves can occur due to:
- a) irritation of the vagal center in the medulla oblongata mechanically with increased intracranial pressure (brain trauma and tumors);
- b) irritation of the endings of the vagus nerve in the heart and other organs, for example, by bile acids in obstructive jaundice.
This results in bradycardia, increased peristalsis (diarrhea) and other manifestations of irritation of the vagus nerve.
The excitability of the parasympathetic department of the autonomic system increases under the influence of substances that enhance (potentiate) the action of the mediator of the parasympathetic nervous system - acetylcholine. These include potassium ions, vitamin B1, drugs from the pancreas (vagotonin), choline, some infectious agents: influenza viruses, bacteria of the enteric typhoid group, some allergens.
Increased excitability and excitation of the parasympathetic nervous system and specifically the vagus nerve can occur under the influence of substances that depress (inhibit) cholinesterase. These include many organophosphorus compounds (tetraethylfluerophosphate, tetraethylpyrophosphate and many other compounds of this series). Substances of this type are also known as “nerve poisons”, used by the imperialists as means of chemical warfare. Poisoning with these substances causes the accumulation of acetylcholine in the body and death from an excess of this substance. The accumulation of acetylcholine in the body is also a cause of poisoning with tetraethyl lead (a detonator in internal combustion engines), as well as manganese.
Depression or loss of parasympathetic innervation . Inhibition or loss of parasympathetic innervation occurs experimentally in animals after removal of most of the pancreas. In such animals, the negative chronotropic and inotropic influence of the vagus on the heart is sharply weakened. The synthesis of the parasympathetic nervous system mediator, acetylcholine, sharply decreases.
Transection of one, and especially two, vagus nerves in the neck in animals (dogs, rabbits) and in humans is a very difficult operation. Vagotomized animals usually die within a few days to several months after surgery. Bilateral vagotomy causes death much earlier.
It is known that in the trunks of the vagus nerves there are up to 300 different nerve fibers each. Transection of the vagus nerve causes the following phenomena:
- 1) disorders of respiratory movements due to interruption of the reflex paths from the lungs to the respiratory center (Hering and Breuer reflexes). Breathing movements become rare and deep;
- 2) paralysis of the muscle that closes the entrance to the larynx during swallowing. This causes food to be refluxed into the larynx and lungs, contributing to the development of aspiration pneumonia;
- 3) hyperemia and pulmonary edema due to paralysis of the vasoconstrictor nerves in the lungs. It also contributes to the development of pneumonia (“vagal pneumonia”);
- 4) digestive disorders due to inhibition of the secretion of gastric and pancreatic juice.
The longest survival times for vagotomized animals were obtained by I. P. Pavlov when they were specially fed through a gastric fistula with easily digestible food. Disturbances in the parasympathetic innervation of the heart are also caused by bacterial toxins (botulinum, diphtheria) and antigens of bacteria of the enteric typhoid group.
Disorders of the sacral narassympaticus (S2-S4) of the pelvic nerve occur with injuries or tumors of this part of the spinal cord or pelvic nerve. Disorders of urination (emptying the bladder), defecation, and genital functions occur.
Autonomic neuroses
These very common disorders of autonomic innervation most often extend to both parts of the autonomic nervous system. They consist of a sharp and prolonged increase in the excitability of the autonomic nervous system. This is expressed in disorders of the frequency and rhythm of the heart, disturbances in the tone of blood vessels (“vascular dystonia”, “vascular crises”), increased sweating or, conversely, dryness. skin, phenomena of white or red dermographism, digestive disorders (dyspepsia, diarrhea, constipation), etc. The previous division of autonomic neuroses into “sympathicotonia” and “vagotonia” has now been abandoned, since disorders usually occur in both parts of the autonomic nervous system.
Emotional disturbance. Emotional stress
Emotional disorders develop when the hypothalamus, limbic system and neocortex are damaged.
Thus, when the posterior nuclei of the hypothalamus are damaged, lethargy, apathy, decreased initiative, and loss of interest in the environment develop. Bilateral removal of the amygdala nuclei in an experiment reduces emotional reactions in animals, making them tame and obedient.
The phenomena of unmotivated excitement, anger, rage or euphoria are united under the concept of “emotional stress”. In persons with pathology of the anterior parts of the hypothalamus, phenomena of excitement occur with euphoria, unmotivated transitions to irritability and anger.
Removal of the orbital cortex in cats and monkeys caused increased irritability and aggressive behavior. There is evidence that the substrate of rage in cats is located in the ventromedial nuclei of the hypothalamus.
Emotional disorders also occur due to damage to the frontal lobes of the brain. For example, various feelings: fear, joy, grief and many others in people who have undergone operations on these lobes lose their strength and vitality. The ability for imagination and creativity is significantly reduced. The free ones become careless. Their behavior is governed by the “pleasure-displeasure” principle.
With tumors of the medial parts of the frontal lobes, lethargy and apathy develop; Memory for current events is often impaired.
Extensive brain damage, such as necrosis, among other disorders, leads to emotional disorders in the form of stereotypical, unfocused outbursts of rage that occur in response to any external stimuli. These reactions are to some extent reminiscent of the so-called false anger (increased aggressiveness) in decorticated animals.
Diagnosis of autonomic dysfunction
To make a diagnosis, it is necessary to exclude organic pathology.
Anamnesis is being collected. An ECG is measured with daily recording of an electrocardiogram. Rheovasography can also be used. The gastrointestinal tract is examined using gastroscopy. A study of the nervous system is being carried out. This is done using electroencephalography and computed tomography. Taking into account the data obtained and the overall clinical picture, the doctor can diagnose a disorder of the autonomic nervous system.