Obliterating atherosclerosis of the vessels of the lower extremities Obliterating atherosclerosis of the vessels of the lower extremities is a chronic vascular disease that develops due to lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of the walls of the arteries of the legs and a decrease in the vascular lumen.
All these changes can lead to partial or complete cessation of blood flow. At first, this pathology practically does not manifest itself in anything, but as this disease progresses, atherosclerotic plaques increasingly narrow the lumen of the vessels and can completely block it, leading to ischemia and even necrosis of the tissues of the lower extremities. This development of the disease can result in the development of gangrene and loss of a leg.
What it is?
Obliterating atherosclerosis is one of the forms of atherosclerosis. With this disease, cholesterol plaques form on the walls of the arteries, they disrupt normal blood flow, causing vasoconstriction (stenosis) or its complete blockage, called occlusion or obliteration, therefore they speak of occlusive-stenotic damage to the arteries of the legs.
According to statistics, the prerogative of having pathology belongs to men over 40 years of age. Obliterating atherosclerosis of the lower extremities occurs in 10% of the total population of the Earth, and this number is constantly growing.
Classification of atherosclerosis
Based on the nature of vascular damage, stenosis and occlusion are distinguished. In the first case, there is a pathological narrowing of the diameter of the arteries, causing circulatory problems.
Occlusion is a complete blockage of the lumen. Taking into account the localization of obliteration, atherosclerosis of the femoral-popliteal, aorto-iliac, popliteal-tibial region or multi-storey lesions of the vessels of the legs are distinguished.
Classification of the disease according to the prevalence of the stenotic process:
- segmental occlusion;
- widespread vascular damage;
- occlusion of several arteries;
- obliteration of one or more vessels with preservation of blood circulation in the deep artery;
- blockage of an entire segment.
Atherosclerotic plaques can be stable or unstable. Their condition depends on their size, shape and structure. Stable deposits are rich in collagen, characterized by slow growth, and the disease progresses over several years. Unstable ones consist predominantly of lipids, are easily subject to erosion, decay, and can cause occlusion, even if there are no signs of stenosis.
Causes
The main cause of atherosclerosis is smoking. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Additional factors that provoke atherosclerosis of the arteries of the lower extremities and lead to an earlier onset and severe course of the disease:
- increased cholesterol levels due to frequent consumption of foods rich in animal fats;
- high blood pressure;
- excess weight;
- hereditary predisposition;
- diabetes;
- lack of sufficient physical activity;
- frequent stress.
Frostbite or prolonged cooling of the legs suffered at a young age of frostbite can also be a risk factor.
Risk factors
The main reason for the development of the disease is disturbances in cholesterol metabolism. They are caused by a number of reasons, both directly dependent on a person and those over which he is unable to influence. Risk factors for the development of atherosclerosis are as follows:
- Floor. The gender factor plays a very important role in the development of the disease. In most cases, atherosclerosis affects men over the age of forty. Among women, the disease is much less common. Females become more susceptible to atherosclerosis after menopause. This is due to a decrease in estrogen levels and an increase in cholesterol levels.
- Age. As mentioned earlier, the older a person is, the greater the risk of getting sick. Atherosclerosis is most common among older people over the age of sixty. The reason for this is changes in metabolic processes that occur as the body ages.
- Heredity. Atherosclerosis cannot be inherited. But members of the same family or clan may have high cholesterol levels. In some cases, this occurs due to changes in genes that are inherited. In addition, a similar situation is observed due to the same living conditions and eating habits, which a person gets used to in childhood.
- Nutrition. The main reason for the development of the disease is poor nutrition. A person should eat food in proportion to energy expenditure. In addition, food contains important chemical compounds necessary for the normal functioning of the body.
- Bad habits. Frequent smoking leads to changes in the walls of blood vessels. This factor contributes to the further occurrence of atherosclerosis. A slight increase in cholesterol in the blood of a smoker increases the chances of developing the disease (the risk of developing the disease in such people is nine times higher).
- Stress. During stressful situations, the human body produces glucose and fats. Such a measure was justified at that stage of development when a person fought for survival every day. Additional release of glucose and fat ensured normal muscle functionality under conditions of increased stress.
This body response to stress continues today. But modern people rarely overuse muscle mass, so the produced substances accumulate in the body and trigger the atherosclerotic process. - Obesity. Accompanied by a violation of the metabolism of fats and carbohydrates, and therefore cholesterol levels increase. Excessive weight often leads to diabetes, which makes the situation even worse.
The more factors simultaneously influence the human body, the higher the chance of developing atherosclerosis.
Development mechanism
Most often, atherosclerosis of the vessels of the lower extremities manifests itself in old age and is caused by disorders of lipoprotein metabolism in the body. The development mechanism goes through the following stages.
- Cholesterol and triglycerides that enter the body (which are absorbed into the intestinal walls) are captured by special transport proteins - chylomicrons and transported into the bloodstream.
- The liver processes the resulting substances and synthesizes special fatty complexes - VLDL (very low density cholesterol).
- In the blood, VLDL molecules are affected by the enzyme lipoprotein lipase. In the first stage of the chemical reaction, VLDL is transformed into intermediate-density lipoproteins (or IDL), and then in the second stage of the reaction, IDL is transformed into LDL (low-density cholesterol). LDL is the so-called “bad” cholesterol and it is the one that is more atherogenic (i.e., capable of provoking atherosclerosis).
- Fatty fractions enter the liver for further processing. Here, high-density cholesterol (HDL) is formed from lipoproteins (LDL and LPPP), which has the opposite effect and is able to cleanse the walls of blood vessels from cholesterol deposits. This is the so-called “good” cholesterol. Part of the fatty alcohol is processed into digestive bile acids, which are necessary for normal food processing and are sent to the intestines.
- At this stage, the liver cells may fail (genetically or due to old age), as a result of which, instead of HDL at the output, low-density fat fractions remain unchanged and enter the bloodstream.
Mutated or otherwise altered lipoproteins are no less, and perhaps more atherogenic. For example, oxidized under the influence of H2O2 (hydrogen peroxide).
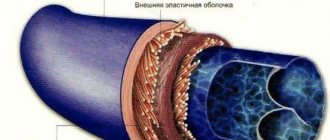
- Low-density fat fractions (LDL) settle on the walls of the arteries of the lower extremities. Prolonged presence of foreign substances in the lumen of blood vessels promotes inflammation. However, neither macrophages nor leukocytes can cope with cholesterol fractions. If the process is delayed, layers of fatty alcohol - plaques - form. These deposits are very dense and interfere with normal blood flow.
- Deposits of “bad” cholesterol are encapsulated, and when the capsule is ruptured or damaged, blood clots form. Blood clots have an additional occlusive effect and further clog the arteries.
- Gradually, the cholesterol fractions, together with blood clots, take on a rigid structure due to the deposition of calcium-containing salts. The walls of the arteries lose their normal extensibility and become fragile, resulting in possible ruptures. In addition to this, persistent ischemia and necrosis of nearby tissues is formed due to hypoxia and lack of nutrients.
[adsen]
Stages
During obliterating atherosclerosis of the lower extremities, the following stages are distinguished:
- Stage I (initial manifestations of stenosis) – a feeling of goosebumps, pale skin, a feeling of coldness and chilliness, excessive sweating, rapid fatigue when walking;
- Stage II A (intermittent claudication) – a feeling of fatigue and stiffness in the calf muscles, squeezing pain when trying to walk about 200 m;
- Stage II B – pain and feeling of stiffness prevent you from walking 200 m;
- Stage III – squeezing pain in the calf muscles becomes more intense and appears even at rest;
- Stage IV – signs of trophic disorders, long-term non-healing ulcers and signs of gangrene appear on the surface of the leg.
In advanced stages of atherosclerosis of the lower extremities, the development of gangrene often leads to complete or partial loss of a limb. The lack of adequate surgical care in such situations can lead to the death of the patient.
According to prevalence, obliterating atherosclerosis is divided into stages:
- Segmental obliteration - only one limb fragment falls out of the microcirculation area;
- Widespread occlusion (2nd degree) – block of the superficial femoral artery;
- Blockage of the popliteal and femoral artery with impaired patency of the bifurcation area;
- Complete blockade of microcirculation in the popliteal and femoral arteries – 4th degree. In case of pathology, blood supply is maintained through the system of deep femoral arteries;
- Damage to the deep femoral artery with damage to the femoral-popliteal region. Grade 5 is characterized by severe hypoxia of the lower extremities and necrosis, trophic ulcers and gangrene. The severe condition of a bedridden patient is difficult to correct, so treatment is only symptomatic.
Types of occlusive-stenotic lesions in atherosclerosis are represented by 3 types:
- Damage to the distal part of the tibial and popliteal arteries, in which the blood supply to the lower leg is preserved;
- Occlusion of blood vessels of the leg. Patency of the tibial and popliteal arteries is preserved;
- Occlusion of all vessels of the thigh and leg while maintaining patency of individual branches of the arteries.
Surgery
Surgery is indicated for patients with grade III and IV obliterating atherosclerosis. According to indications, the following types of reconstructive operations are used:
- angioplasty and stenting;
- bypass;
- laser atherectomy;
- cryoplasty;
- balloon angioplasty.
During bypass operations, an autovenous graft (great venous vein) is used as a plastic material. If it is not possible to use autologous material, homografts and allografts from living donor tissue are used. Alloprostheses made of polytetrafluoroethylene or dacron can be used.
For stenting, metal, balloon-expandable (heparin-coated) and self-expanding stents are used. Endovascular methods save patients from surgery.
Using a laser, atherosclerotic plaque is removed, which narrows the lumen of the vessel. The operation is indicated when bypass surgery is not possible in order to reduce the risk of embolic complications.
Contraindications to surgery are myocardial infarction and strokes that the patient has suffered within the previous three months. Surgery is not performed in patients with stage 3 heart failure.
Postoperative period
After surgery, the wounds are drained within 24 hours. The doctor observes the pulsation of the transplanted graft and peripheral vessels. This is done by palpation or using Doppler ultrasound scanning. In case of graft thrombosis, urgent surgical intervention is indicated, which is aimed at eliminating the cause of the thrombosis.
During the day, the patient should be in the intensive care unit, where he will be provided with control of hemodynamics, hemoglobin levels and hematocrit. Patients are prescribed antiplatelet agents, anticoagulants (Heparin) under the control of blood clotting. After discharge, continuous use of Aspirin is prescribed.
Symptoms
Symptoms of OASNK in the initial stages are usually quite vague or absent altogether. Therefore, the disease is considered insidious and unpredictable. It is this damage to the arteries that tends to develop gradually, and the severity of clinical signs will directly depend on the stage of development of the disease.
The first signs of obliterating atherosclerosis of the lower extremities (second stage of the disease):
- feet begin to constantly freeze;
- legs often go numb;
- swelling of the legs occurs;
- if the disease affects one leg, then it is always colder than the healthy one;
- Pain in the legs appears after a long walk.
These manifestations appear in the second stage. At this stage of development of atherosclerosis, a person can walk 1000–1500 meters without pain.
People often do not attach importance to symptoms such as freezing, periodic numbness, pain when walking long distances. But in vain! After all, by starting treatment at the second stage of the pathology, you can 100% prevent complications.
Symptoms that appear at stage 3:
- nails grow slower than before;
- hair begins to fall out on the legs;
- pain can occur spontaneously both day and night;
- pain appears after walking short distances (250–900 m).
When a person has stage 4 of obliterating atherosclerosis of the legs, he cannot walk 50 meters without pain. For such patients, even going shopping, and sometimes just going out into the yard, becomes an impossible task, as going up and down the steps turns into torture. Often patients with stage 4 disease can only move around the house. And as complications develop, they stop getting up at all.
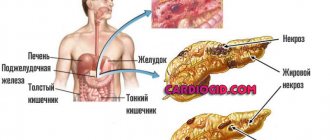
At this stage, treatment of the disease, obliterating atherosclerosis of the lower extremities, often becomes powerless; it can only briefly alleviate the symptoms and prevent further increases in complications, such as:
- darkening of the skin on the legs;
- ulcers;
- gangrene (this complication requires amputation of the limb).
Why is atherosclerosis dangerous?
With atherosclerosis, the lumen of blood vessels decreases, blood supply is disrupted, and tissue nutrition deteriorates. If the diagnosis is made too late, necrosis of individual areas may develop. If the patient has gangrene, urgent amputation of the limb is required. If this is not done, the patient may die from sepsis and infectious-toxic shock.
As a result of tissue ischemia, acute infarction or stroke develops, which causes death in 30% of cases of death due to atherosclerosis.
Important! Atherosclerosis is rarely an isolated disease. Most often it is of a secondary nature and is a complication of other pathologies and disorders in the functioning of blood vessels. Such patients are often diagnosed with coronary heart disease, heart failure, diabetes mellitus, narrowing of the spinal canal and other dangerous diseases with a high risk of mortality.
What happens in blood vessels during atherosclerosis
Mortality statistics after amputation of the lower extremities with atherosclerotic vascular lesions
| Period after amputation | Mortality rate (percentage of total patients) |
| First year | ≤ 20 % |
| 5 years | 40-70 % |
| 10 years | ≥ 95 % |
Early diagnosis of the disease is of great importance in a favorable prognosis for life and health. If atherosclerosis has been identified at the initial stage, there is a high probability of a positive result of drug correction and limb preservation, so you should consult a doctor when the first symptoms appear. Unfortunately, more than half of the cases of the disease are practically asymptomatic, but there are certain signs that should alert the patient and become a reason to consult a specialist.
Stages of atherosclerosis
Features of the flow
All symptoms of the disease develop gradually, but in rare cases, obliterating atherosclerosis of the vessels of the lower extremities manifests itself in the form of arterial thrombosis. Then, at the site of arterial stenosis, a blood clot appears, which instantly and tightly blocks the lumen of the artery. Such a pathology develops unexpectedly for the patient; he feels a sharp deterioration in health, the skin of the leg turns pale and becomes cold. In this case, a quick visit to a vascular surgeon (counting the time to irreversible events by the clock) allows the person to save his leg.
With a concomitant disease—diabetes mellitus—the course of obliterating atherosclerosis has its own characteristics. The history of such pathologies is not uncommon, and the disease develops so rapidly (from several hours to several days) that in a short time it leads to necrosis or gangrene in the lower extremities. Unfortunately, doctors often resort to leg amputation in such situations - this is the only thing that can save a person’s life.
Typical symptoms depending on the location of the lesion
Atherosclerotic lesions of the extremities have typical symptoms, which can help a specialist determine the affected area and simplify the diagnosis of the disease.
| Narrowing area | Symptoms |
| Aorta and iliac artery | Pain in the gluteal muscles and upper thigh. Problems with potency in men (impotence is diagnosed in 25% of cases) |
| Superficial femoral artery | Painful sensations and burning sensations in the upper and lower legs |
| Posterior tibial artery | Pain and lameness in the lower extremities |
| Popliteal artery | Pain in the upper legs |
When examining and palpating the affected areas, the doctor may notice a lack of pulsation in the ankles, behind the knees, and in the area of the femoral arteries. The patient is required to be prescribed a set of diagnostic measures, which may include:
- Ultrasound diagnostics;
- Doppler ultrasound of peripheral arteries;
- determination of the ankle-brachial index when measuring pressure;
- other procedures.
Diagnostics of atherosclerosis
Important! A vascular surgeon treats atherosclerosis. If there is no specialist in the hospital or clinic, if signs of pathology appear, you can contact a regular surgeon or therapist, who will collect anamnesis, clarify complaints and refer the patient for consultation to specialized doctors.
Diagnosis of the disease
The diagnosis of “obliterating atherosclerosis of the vessels of the lower extremities” is made based on the following data:
- Characteristic complaints of the patient (pain syndrome, intermittent claudication).
- On examination, signs of atrophy of the soft tissues of the limb are noted.
- Rheovasography of the extremities shows a pronounced decrease in the index on the legs and feet.
- Reducing the level of pulsation in the arteries of the feet, legs, popliteal and femoral arteries. If the area of the aortic bifurcation is affected, there may be a lack of pulsation in both femoral arteries (Leriche syndrome).
- Thermometry, thermography – reducing tissue temperature and the level of infrared radiation.
- Ultrasound of the vessels of the legs (Dopplerography) indicates a violation of the blood supply to the peripheral parts.
- Arteriography (a study that involves injecting a contrast agent into the arteries of the legs) shows the area of narrowing of the artery of the limb.
- Tests with functional load - decreased load tolerance, rapid fatigue and the appearance (or intensification) of ischemic pain.
Diagnostics
Diagnosis of atherosclerosis of the lower extremities is necessary to determine the degree of the disease, differentiate it from other pathologies and choose tactics to cure the patient.
The diagnostic program is compiled from a general examination, laboratory and instrumental research methods.
During a general examination, the doctor determines:
- Color and condition of the skin of the legs (pale skin, red-cyanotic, or bluish-black, which indicates the presence and stage of atherosclerosis of the lower extremities).
- Skin temperature of the lower extremities (cold legs are a sign of poor circulation).
- The degree of pulsation of the arteries and the presence of noise by auscultation (weak pulsation of the arteries and the presence of systolic noise indicate arteriosclerosis).
- Functional tests. Moshkovich test for assessing the plantar symptom: the patient, lying down, raises his legs up without bending them at the knees (2-3 minutes), then stands up. Normally, in a healthy person, when lying down, the skin turns pale; after taking a vertical position, after 8–10 seconds it acquires a natural pink tint. In a patient suffering from atherosclerosis, the skin remains pale or acquires a marbled tint.
Laboratory methods for diagnosing atherosclerosis of the lower extremities:
- Lipidogram (biochemical blood test) . The level of total cholesterol and ego fractions (LDL and HDL), and the atherogenicity coefficient (the ratio of “good” and “bad” cholesterol) are determined.
- Coagulogram . The blood coagulation system is assessed.
Instrumental methods for studying atherosclerosis of the lower extremities:
- Angioscanning of leg vessels with Doppler sonography . A non-invasive ultrasound method allows you to assess the condition of small vessels and characterize blood flow (vasoconstriction/dilation, presence of blood clots, plaques in vessels, aneurysms, speed and direction of blood flow).
- Measuring the ankle-brachial index using volumetric sphygmography . Determines the ratio of systolic blood pressure between the upper and lower extremities.
- Magnetic resonance angiography allows you to evaluate the anatomical and functional data of blood vessels by obtaining a three-dimensional image.
- Multislice computed tomography of the extremities . An invasive method using x-ray contrast agents. It makes it possible to assess the condition of the walls of arteries and veins, to identify their pathology and features.
Treatment of obliterating atherosclerosis
Conservative treatment of patients with obliterating atherosclerosis of the arteries of the lower extremities is carried out in the following cases:
- at the stage of chronic arterial circulatory failure in the extremities according to the classification of A. V. Pokrovsky - Fontane;
- with severe concomitant pathology: coronary disease, cerebral vascular damage, chronic diseases of the lungs, liver, kidneys, diabetes mellitus;
- multiple (multi-story) occlusions and stenoses of the main arteries;
- lesions of the distal vascular bed.
It assumes:
- sedative therapy (seduxen, elenium);
- desensitizing therapy (diphenhydramine, pipolfen);
- pain relief (analgesics, intra-arterial agents, blockades of 1% novocaine solutions, paravertebral blockades at the L2 - L3 level, epigastric blockades);
- exclusion of vascular risk factors (smoking, alcohol, excessive cooling, nervous stress, physical inactivity, diabetes mellitus);
- improving the rheological properties of blood, i.e. reducing its viscosity (plasma substitutes - dextrans, defibrinogenic enzymes - acrod, pentoxifylline, trental, vasonite, agapuria);
- elimination of vascular spasm (antispasmodics - no-shpa, halidor, xanthinol nicotinate; gangioblockers - hexonium, dicaine);
- normalization of the blood coagulation system (anticoagulants);
- inhibition of platelet adhesive-aggregation activity (acetylsalicylic acid, ticlide);
- restoration of oxidant-antioxidant balance - protection of cell membranes (antioxidants - vitamins A, E, C, probucol);
- activation of metabolic processes in tissues (vitamins, nicotinic acid, complamin, solcoseryl, bradykinin inhibitors - prodectin, parmidine);
- elimination of immune disorders (immunomodulation, immunosorption, ultraviolet radiation of blood);
- normalization of lipid metabolism. It includes diet therapy, the prescription of lipid-lowering drugs, the use of extracorporeal methods for correcting the composition and properties of circulating blood, partial jejunoileobypass surgery, and gene therapy.
Diet therapy for obliterating atherosclerosis is based on limiting the energy value of food intake to 2000 kcal per day with a decrease in the proportion of fat (up to 30% or less) and cholesterol (less than 300 mg). It is justified to prescribe antiatherogenic nutritional supplements to patients, such as polyunsaturated fatty acids, fish oil, eikonol (a nutritional supplement obtained from certain types of fish).
If there is no normalization of lipid metabolism parameters during diet therapy, without stopping it, drug treatment is carried out. Currently, five groups of lipid-lowering drugs are used for the treatment and prevention of atherosclerosis:
- enterosorbents - cholestyramine, which are sequestrants of bile acids;
- statins - lovastatin (Mevacor), simvastatin (Zocor), privastatin (Lipostat), fluvastatin (Leskol)
- fibrates - mofibrate, otofibrate;
The effectiveness of conservative therapy is assessed by factors affecting lipid metabolism, primarily by the level of total cholesterol and LDL cholesterol.
Normal triglyceride levels are 150 mg/dL. Extracorporeal methods for correcting the composition and properties of circulating blood: plasmapheresis; selective immunosorption, including on sorbents with monoclonal antibodies to LDL (especially effective in the treatment of patients with severe hetero- and homozygous hypercholesterolemia); hemosorption. These methods make it possible to obtain a persistent hypolipidemic effect, which consists in reducing the level of LDL in the blood and increasing the content of HDL, reducing the atherogenic coefficient. This slows down the progression of atherosclerotic arterial occlusion. However, if conservative correction of hyperlipidemia is unsuccessful, there is a tendency for the process to progress, especially in early atherosclerosis, significant clinical manifestations of atherosclerosis in patients with its generalized form, which is usually observed in people with familial hypercholesterolemia, when the cholesterol level exceeds 7.5 mmol/l, In cases of severe xanthomatosis, a partial jejunoileal shunt operation (Buchwald operation) can be performed.
The essence of this surgical intervention is to exclude the distal third of the small intestine from digestion and anastomose the proximal 2/3 of the small intestine with the dome of the cecum. The colon has the ability to synthesize and secrete several types of lipids and their apoproteins, influence hepatic synthesis and secretion of lipids through absorption and enterohepatic circulation of bile acids (BAs) and cholesterol. A decrease in the length of the functioning part of the small intestine leads to impaired absorption of FAs and acceleration of their excretion, an increase in the synthesis of fatty acids in the liver, increasing the oxidation of cholesterol, a decrease in the intestinal synthesis of cholesterol, chylomicrons, VLDL, a decrease in lipid absorption and subsequent inhibition of the synthesis of atherogenic lipoproteins in the liver. A side effect of Buchwald's operation is the frequent development of diarrhea, impaired absorption of vitamin B12 and folic acid.
Two main methods of gene therapy for obliterating atherosclerosis have been developed. The essence of the first of them is to introduce a gene encoding a normal protein - a receptor for LDL, with the help of a retrovirus, into a culture of hepatocyte cells of the patient, and then, through a catheter installed in the portal vein, to deliver a suspension of such cells to the patient's liver. After their engraftment, the donor's normal receptors begin to function. The disadvantage of the method is the need for the patient to take significant doses of statins and a gradual decrease in the function of the introduced genes.
The second (direct) method is performed on a patient without prior manipulation of target cells, while the gene is complexed with a carrier (vector) and directly introduced into the patient, but locally - into the cardiovascular system to avoid dissemination of the gene in the body. Direct administration is carried out using a viral infection, chemical or physical method,
In the complex of conservative treatment of patients with atherosclerosis, especially with stages III - IV of chronic arterial insufficiency of the extremities, it is advisable to include drugs with a complex mechanism of action; 1) tanakan - stimulates the production of relaxation factor by the vascular endothelium. The drug has a vasodilating effect on small arterioles, reduces capillary permeability, reduces platelet and red blood cell aggregation, protects cell membranes by suppressing lipid peroxidation reactions, improves the absorption of glucose and oxygen by tissues; 2) prostaglandins and their synthetic derivatives (vasoprostan). They influence all stages of the development of ischemic syndrome in the limb, have a vasodilating effect, suppress platelet aggregation, improve microcirculation, and normalize metabolic processes in ischemic tissues.
Patients with obliterating atherosclerosis of the vessels of the lower extremities are prescribed physiotherapeutic, balneological and sanatorium-resort treatment (magnetic therapy with pulsed and direct currents with effects on the lumbar sympathetic ganglia and lower extremities, interference currents on the lower extremities and lumbar spine, massage of the lower extremities, reflex-segmental massage of the spine , radon, hydrogen sulfide baths, acupuncture, hyperbarotherapy).
One of the most modern methods of physiotherapeutic treatment of patients with obliterating atherosclerosis of the vessels of the lower extremities is electrical stimulation of the spinal cord. It is performed if it is impossible to perform reconstructive operations on the arteries due to the prevalence of occlusive lesions with systolic pressure at the ankle level less than 50 mm Hg. Art. The essence of the method is the percutaneous introduction of a quadripolar electrode into the epidural space of the lumbar spine, extending its apex to the T12 level and positioning it in the midline. During the first week, electrical stimulation of the spinal cord is carried out with a pulse frequency of 70 - 120 Hz from an external source. If a positive clinical result is obtained, the generator is implanted into the subcutaneous tissue of the anterior abdominal wall and programmed for continuous or intermittent operation. Electrical stimulation is carried out for a long time (months).
For obliterating atherosclerosis of the vessels of the lower extremities, training walking is also used (kinesitherapy, muscle training, walking through a walking throuth). Kinesitherapy aims to increase the distance of pain-free walking. The essence of the method is as follows: if hypoxic pain appears in the calf muscles when the patient overcomes a certain distance, he temporarily slows down his step. A few minutes after this, the patient is again able to perform movements without pain. The mechanism of the beneficial effect of training walking in occlusive-stenotic lesions of the arteries of the extremities is explained by an improvement in the utilization of oxygen by myocytes, an increase in the activity of their mitochondrial enzymes and anaerobic energy production, the transformation of white muscle fibers into red ones, stimulation of collateral circulation, and an increase in the ischemic pain threshold.
For the surgical treatment of patients with obliterating atherosclerosis of the main arteries of the lower extremities, arterial reconstructive and palliative operations are used. Reconstructive methods for restoring arterial blood flow include: endarterectomy, bypass surgery, prosthetics, X-ray endovascular reconstruction (see “Treatment of Leriche syndrome”). An indispensable condition for their implementation is good patency of the distal vascular bed.
Endarterectomy (thrombendarterectomy), as a rule, is used in patients with short (segmental) single occlusions of the main arteries 7-10 cm long. The essence of the operation is to remove the atheromatically changed intima along with the blood clots located next to it. Endarterectomy can be open, semi-closed, closed, eversion, as well as using mechanical and physical methods.
In open endarterectomy, the isolated artery is dissected longitudinally above the location of the plaque. Then, under visual control, the altered intima is peeled off from the underlying layers of the wall to the level of transition to visually unaffected areas and is cut off. The edges of the intima adjacent to the manipulation zone are fixed to the artery wall with atraumatic sutures, which is a reliable way to prevent it from wrapping and blocking the lumen of the arteries. To prevent narrowing of the endarterectomized artery, an autovenous patch is sewn into the incision.
The semi-closed endarterectomy method involves: 1) exposure of the affected segment of the arteries along its entire length; 2) dissection of arteries (longitudinal, transverse) in the projection of the distal end of the occlusion; 3) circular separation in this place of the atheromatically changed intima from the muscular membrane; 4) transverse intersection of the selected segment and passing along it in the proximal direction a special instrument - a disobliterator, mainly a ring (ring stripper), exfoliating the altered ingima; 5) opening the lumen of the artery above the area of the proximal end of the occlusion and removing the detached cylinder of the affected intima through it; 6) suturing the artery wall, if necessary with an autovenous patch.
Endarterectomy with the closed method is carried out in the same way as the semi-open one, but without isolating the artery along its entire length.
When using the eversion endarterectomy method, the artery is transversely dissected below the location of the plaque. Next, the layer of its wall, consisting of the muscular layer and adventitia, peels off from the affected intima and contracts (turns out) in the proximal direction along the upper border of the plaque. At this level, the resulting cylinder of altered intima is cut off. The inverted muscularis propria and adventitia return to their original position. The patency of the vessel is restored by applying a circular suture. It is also possible to perform reverse eversion thromboendarterectomy.
Bypass operations for obliterating atherosclerosis are performed for extended and multi-storey occlusive-stenotic lesions of the main arteries of the lower extremities. A segment of the great saphenous vein isolated from its bed, reversed and anastomosed with the artery above and below the obstacle is most often used as bypasses. Less commonly used are the human umbilical cord vein, homoarterial grafts, synthetic prostheses made of polytetrafluoroethylene, and the great saphenous vein without isolating it from the bed. The essence of the latter method is that the vein is not isolated from the subcutaneous tissue and is not reversed, but is intersected above and below the site of occlusion. Before forming an arteriovenous anastomosis, the venous valves are destroyed using valvulotomes of various designs. The presence of tributary veins capable of acting as arteriovenous fistulas after arterial blood flow is started through it is established on the basis of data from angiography, Dopplerography, palpation, etc., followed by their ligation.
The success of the shunt operation is determined, in addition to the condition of the peripheral bed, and the diameter of the shunt used, which must exceed 4-5 mm.
In case of severe damage to the arteries of the leg, obstruction of the plantar arch, in addition to the usual femoral-popliteal (tibial) autovenous shunting, additionally c. After leaf anastomosis, an arteriovenous fistula is formed, which leads to the discharge of part of the blood directly into the vein, increases the speed of blood flow through the vein and thereby reduces the likelihood of thrombosis. During surgery, a side-to-side anastomosis is first performed with the receiving artery, then a fistula is created by anastomosing the distal end of the shunt with the adjacent popliteal or tibial vein. The diameter should be 2-4 mm, i.e. 40 - 60% of the shunt diameter.
Prosthetics of the main arteries of the lower extremities for atherosclerosis is used extremely rarely.
If it is not possible to restore blood flow through the main arteries, primarily due to occlusion of the distal vascular bed, plastic surgery of the deep femoral artery is performed. At the same time, quite frequent damage to both the deep femoral artery and the popliteal and leg arteries, poor development of collaterals between them lead to unsatisfactory results of the operation.
In case of occlusion of the distal vascular bed or poor condition of the deep femoral artery, palliative surgical interventions are performed aimed at enhancing collateral circulation in the limb. These include lumbar sympathectomy, revascularizing osteotrephination, methods of P. F. Bytka, G. A. Ilizarov, microsurgical transplantation of the greater omentum to ischemic tissue of the extremities.
Lumbar sympathectomy for obliterating atherosclerosis involves extra-, transperitoneal removal of the II - III lumbar sympathetic ganglia on the affected side (Diez operation). The main mechanism of action of the operation is to eliminate the influence of the sympathetic nervous system.
When using revascularizing osteotrephination for obliterating atherosclerosis, 6-9 burr holes with a diameter of 4-6 mm are made on the medial surface of the tibia at biologically active points (as in acupuncture) in the area of a well-developed subcutaneous network of collaterals without damaging the bone marrow. In the postoperative period, subthreshold irritation at biologically active points caused by trepanation stimulates the opening of reserve collaterals. At the same time, through burr holes, unconventional intervascular connections are formed between the arteries of muscle tissue and the bone marrow. In addition, the content of bone marrow mediators—myelopeptides, which have analgesic, trophic and angioprotective properties—increases in the general bloodstream (G. A. Ilizarov, F. N. Zusmanovich, 1983).
The essence of P.F. Bytok’s method is the introduction of autologous blood through certain points on the foot and lower leg into their soft tissues (Fig. 42). Treatment is carried out for 30 days. The tissues are infiltrated twice - on the lower leg on the 1st and 14th days, on the foot on the 7th and 21st days. One session consumes 60 - 80 ml of blood for the foot, 150 - 180 ml for the lower leg. The clinical effect of the operation becomes noticeable after 2-3 months. after completion of the course of treatment and is associated with the formation of well-vascularized connective tissue in the extravasation area.
G. A. Ilizarov’s method (longitudinal compactectomy according to G. A. Illizarov) involves the formation of a longitudinal bone flake 10-16 cm long from the anterior internal surface of the tibia. 2-3 distraction wires are passed through it and attached to the Ilizarov apparatus applied to the bone. From the 8th to 9th postoperative day, the bone flake is removed daily from the tibia by 0.5 mm. The procedure is performed for 31-36 days, until the gap between the tibia and its fragments is 15-20 mm. After this, fixation of the flake continues for 45–60 days, which depends on the degree of maturity of the connective tissue. According to G. A. Illizarov, when the flake is distracted, regional stimulation of the vascular network occurs under the influence of tensile stress. At the same time, the main vessels expand, the number and caliber of small vessels of muscles, fascia and bones increase; at the site of hematoma formation, well-supplied connective tissue develops; due to increased blood supply, regenerative processes in the limb are activated.
During microsurgical transplantation of the greater omentum onto ischemic tissues of the extremities, the greater omentum is placed subfascially on the thigh, moving to the popliteal region and lower leg. The feeding vessel of the graft, usually the right gastroepiploic artery, is implanted into the common femoral artery, and the vein into the femoral vein.
The disadvantage of these methods of surgical treatment of obliterating atherosclerosis, which occurs with occlusion of the entire distal vascular bed of the lower extremities, is the long period of time required for the development of collateral circulation - from 1 to 3 months. This limits the use of such operations in the treatment of patients with critical limb ischemia of stages III - IV, who need a rapid increase in blood circulation in the limb. In such cases, arterilization of the venous system of the foot is carried out: arterilization of the superficial venous network with preliminary destruction of its valves - arterilization into the sources of the great saphenous vein, and in case of occlusion of the superficial veins - into the deep venous system. Arterilization into the origins of the great saphenous vein on the foot involves performing a bypass (reversed autovein, vein in situ, prosthesis) between the patent segment of the popliteal artery or the distal segment of the superficial femoral artery and the origins of the great saphenous vein on the foot. The arterilization of the deep venous network is based on the inclusion of the posterior tibial vein into the bloodstream using a similar technique.
If it is impossible to perform reconstructive surgery in patients with thrombotic occlusions of the arteries of the lower extremities or abdominal aorta due to atherosclerosis, systemic or local thrombolysis with well-known thrombolytic drugs (streptokinase, decase) can be used.
The greatest effect from its use is achieved: 1) with a period of occlusion not exceeding 12 months. in patients with damage to the abdominal aorta and iliac arteries, 6 months. - with the appearance of the femoral and popliteal arteries, 1 month. - renal arteries; 2) with the extent of occlusion up to 13 cm, 3) with a satisfactory condition of the distal vascular bed (the arteries of the lower leg are patent).
Systemic lysis is carried out according to the traditional scheme, local involves the introduction of a thrombolytic in a lower dosage through a catheter directly into the body of the thrombus, antegrade or retrograde, which is accompanied by activation, in contrast to systemic lysis, only of plasminogen, which is part of the structure of the thrombus.
There are several methods of local thrombolysis: 1) continuous infusion with an initial administration of a large dose, and then a maintenance dose; 2) administration of a thrombolytic drug through a catheter with multiple holes along the entire length of the occluding thrombus (pulsatile spray technique); 3) administration of a thrombolytic in a large dose while pulling the catheter along the length of the thrombus. The maximum duration of thrombolytic therapy does not exceed 48 hours. Its effectiveness is monitored angiographically or using ultrasonography.
In the postoperative period, patients continue complex conservative treatment aimed at preventing purulent and thrombotic complications of the operation. Subsequently, they must annually undergo 1-2 courses of inpatient therapy for the disease, and while on outpatient treatment, constantly take antiplatelet agents, indirect anticoagulants and other pathogenetically based drugs.
Treatment of atherosclerosis of the lower extremities
The choice of treatment method for atherosclerosis of the lower extremities is determined by the attending physician depending on the stage of the disease, its duration and the presence of concomitant diseases.
The first stage is the first call to change your lifestyle and give up destructive habits.
Further, an integrated approach to the treatment of atherosclerosis of the lower extremities is used, which includes conservative and surgical treatment methods.
Drug treatment involves the use of the following groups of drugs:
- Lipid-lowering drugs . They reduce the concentration of cholesterol and other lipids in the blood and prevent the progression of atherosclerosis. These include: Atorvastatin, Simvastatin, Rosuvastatin, Traikor, fish oil preparations.
- Antispasmodics (Drotaverine, Papaverine). Reduce the level of pain.
- Preparations that improve microcirculation (Pentoxifylline, Nicotinic acid).
- Antiplatelet drugs and anticoagulants (Acetylsalicylic acid, Heparin, Warfarin). Improves the rheological properties of blood and reduces the risk of thrombosis.
- Vasodilators (Vazonit, Vazoprostan).
- Ointments for atherosclerosis of the vessels of the lower extremities are prescribed based on antibiotics with anti-inflammatory properties, for better skin regeneration and wound healing. These include: Oflocain, Levomekol, Argosulfan, Dimexide, Ichthyol ointment.
- Vitamin preparations.
Taking vitamin supplements
Physiotherapeutic methods
Physiotherapeutic treatment is an important component of the treatment program, aimed at improving blood circulation in ischemic areas, stimulating and developing collateral pathways, reducing pain, and optimizing blood rheology.
The following treatment methods are prescribed:
- Diadynamic therapy is an electrotherapeutic method that activates peripheral blood circulation, reduces swelling of the extremities, weakens the inflammatory process and has an analgesic effect. The duration of the procedure is 10 - 15 minutes, the number is 10 - 12 times, repeated after 3 -4 weeks.
- Laser therapy is a radiation method that helps saturate tissues with oxygen, relieves inflammation and swelling, and reduces vascular spasm. If used in conjunction with transcutaneous electrical stimulation, it helps restore neuromuscular regulation of the affected limbs. The course of procedures is 10-15 times, which must be carried out 3-4 times a year.
- Amplipulse therapy is an electrotherapeutic method of alternating currents. It has a pronounced analgesic effect, relieves vascular spasm, and increases the delivery of nutrients to affected tissues. A course of 10 - 12 procedures that must be repeated several times a year.
- Magnetotherapy is a method of physiotherapy that produces a therapeutic effect by applying an alternating electromagnetic field to the body. Also a simple and effective method, which has anti-thrombotic and anti-inflammatory effects, promotes the regeneration of the skin of the legs. The course of treatment is 10-15 procedures.
Effective methods of treating obliterating atherosclerosis are balneotherapy, mud, hydrogen sulfide, carbon dioxide baths, which are used in sanatorium and resort conditions.
It should be noted that the choice of procedure, duration and course of treatment is determined only by the attending physician.
Surgery
The surgical method of treatment is used when drug therapy is ineffective and the process enters the third or fourth stage.
The following surgical treatment methods are used:
- Endovascular techniques (stenting, angioplasty) are performed through percutaneous access, under the control of an X-ray machine. Less invasive operations can also be performed on an outpatient basis and do not require general anesthesia.
- Bypass surgery . This method involves the use of a synthetic vessel, or autograft (the patient's vein) to create an artificial blood path, bypassing the affected artery.
- Thrombendarterectomy is an operation aimed at removing atherosclerotic plaques and clearing clogged arteries.
- Skin plastic surgery . Used at stage 4, with extensive skin damage from atherosclerotic ulcers on the leg, and the ineffectiveness of drug treatments.
- Amputation . It is carried out in case of critical circulatory disorders, gangrene, or inability to save a limb using other methods of therapy. This operation prevents the risk of blood poisoning and multiple organ failure. Subsequently, prosthetics of the affected limb are provided, the patient is trained in everyday self-care, and returning to work.
Surgical intervention
Traditional methods
Traditional medicine methods are used both for prevention and in conjunction with drug therapy to treat the disease.
Folk remedies help reduce pain, have an anti-inflammatory and healing effect, as well as cleanse blood vessels.
It should be noted that treatment with traditional methods is carried out only after consultation with the attending physician and requires systematic use.
Recipes for cooking:
- Tincture.
To prepare you need:
- 100 grams of dried rose hips and hawthorn;
- 50 grams of immortelle herb;
- 80 grams of lingonberry leaves.
Pour boiled water over all ingredients, leave until cool and strain. Take 3 tablespoons 3 times a day, before meals.
The course is 1 month, after a 7-day break, repeat the course.
- Alcohol tincture of garlic.
You will need:
- 50 grams of garlic;
- 200 ml vodka.
Crush the garlic, pour in vodka. Leave for 7 days in a warm place, then keep in the refrigerator. Take 10-15 drops 3 times a day before meals.
Repeat the course after 8 weeks.
Alcohol tincture of garlic
- Alcohol tincture of horse chestnut.
The following ingredients are required for preparation:
- Horse chestnut fruits (2-4 pcs.);
- Vodka 200 ml.
Pour the fruits with vodka in a glass container and leave for two weeks in a cool place. After this, strain the tincture through cheesecloth and add 100 ml of cold boiled water. Take 10 drops 3 times a day before meals.
The course is 14 days, must be repeated after a 2-week break.
- Herbal tincture.
You will need:
- 50 grams of lemon balm;
- 50 grams of fennel;
- 50 grams of adonis;
- 200 ml boiled water.
Mix the herbs and pour boiling water over them. Leave until cool. Strain. Divide into three equal parts and take throughout the day.
Three week course.
- Tincture of dill seeds.
For preparation you will need:
- 1 tablespoon of dill;
- 200 ml boiling water.
Crush the dill seeds and add boiled water. Leave until cool and strain. Divide into 4 parts and take throughout the day, before meals.
The course of application is 1 month.
Folk recipes for topical use for obliterating atherosclerosis:
| Name | Components | Cooking diagram | Mode of application |
| Herbal decoction | 1 hour l. daisies, | Mix all ingredients and add 1 glass of boiled water. Leave until cool and strain through cheesecloth. | Use for compresses 2-3 times a day. |
| 1 hour l. St. John's wort, | |||
| 1 hour l. sage, | |||
| 1 hour l. plantain. | |||
| Ointment | 100 grams of dioscorea root, 200 grams of melted interior fat. | Grind the root of dioscorea and mix with interior fat. | Rub into affected limbs 2 times a day. |
| Oil mixture | 100 ml sea buckthorn oil, 100 ml olive oil. | Mix the oils and store in a cool place. | Rub into the skin of your feet 2 times a day. The course is three weeks. |
| Nettle bath | An armful of fresh nettles. | Place nettle leaves in a bath and fill with boiled water. Let it brew for 3-40 minutes. | Take baths for half an hour every other day. |
Also, for atherosclerosis of the lower extremities, hirudotherapy and bee venom treatment are effective.
These methods have an anesthetic and anti-inflammatory effect, improve blood clotting.
Prevention
Lost health due to atherosclerosis is the result of your attitude towards yourself at random, therefore, already having such a disease, you must at least now be more attentive to yourself and be sure to carry out prevention. In case of OASNK, it is necessary to choose spacious, comfortable shoes to avoid calluses, bruises, avoid any injuries to the legs, and when sitting, do not cross your legs over each other, because At the same time, the vessels are pinched and the blood supply to the affected leg is disrupted. It is necessary to take walks every day; it is very good for your legs. This also includes proper nutrition with the exception of animal fats, salt, smoked meats, fried, red meat, full-fat milk, and cream.
It is necessary to normalize weight and control blood pressure - the numbers should not exceed 140/85. Reducing blood lipids will protect you from myocardial infarction; eliminating physical inactivity from your daily routine and introducing moderate physical activity will also be useful. Quitting smoking is mandatory (this alone reduces the mortality rate from 54% to 18%). It is better to avoid alcohol in any dose.
It is necessary to promptly treat any chronic diseases, control blood sugar levels, avoid stress, regularly visit a doctor for examinations, and systematically conduct courses of conservative treatment. The prognosis is determined by the presence of other forms of atherosclerosis in the vicinity: cerebral, coronary - which, of course, do not improve health.