Inflammation of the perineum is manifested by redness, swelling, and pain.
Sometimes a rash or discharge appears.
The reasons may vary.
Basically, inflammation in the perineal area occurs as a result of infectious, allergic or dermatological diseases.
It can also be the result of systemic hormonal disorders, such as diabetes.
Inflammation of the perineum due to chafing
The perineum is the area between the anus and genitals.
The skin often chafes in this area.
Then an inflammatory process of traumatic origin develops.
At least in the initial stage, it is aseptic: that is, it is not associated with the colonization of the problem area of the skin by microorganisms.
Any trauma to the skin leads to inflammation.
And the stronger the damage, the stronger the inflammatory process and it lasts longer.
Any scratch on the skin leads to redness and swelling in this area.
After any surgical operations, inflammation of damaged tissues continues for several days, and this in no way indicates the addition of infectious complications.
The inflammatory process is a normal reaction of the body to any damaging factors.
It helps prevent infection and normal tissue regeneration.
Chafing is skin damage that occurs as a result of prolonged exposure to a weak mechanical factor.
If the friction is short-lived, it usually does not lead to injury.
But with prolonged rubbing of the skin, its top layer is damaged.
Initially, a person may not feel any symptoms.
But then the skin in the rubbed area becomes inflamed.
It swells, turns red, and becomes too sensitive.
Factors that increase the risk of chafing:
- tight underwear
- sweating (wet skin softens, so it gets damaged faster)
- high mobility (when a person walks for a long time, the number of rubbing movements increases)
The resulting pain usually causes the person to stop moving, change underwear, or perform other actions that prevent further trauma to the skin.
But sometimes this doesn't happen.
It is not always possible for a person to stop further rubbing immediately.
Because the friction zone is in an area that is hidden from the eyes of others.
When you are in a public place, far from home, it can be problematic to do anything.
In such conditions, friction continues, and damage to the skin of the perineal area can be quite significant.
The resulting inflammation can last from a day to several days.
It usually goes away on its own, without any treatment.
But the patient’s task is to prevent infection.
Any mechanical damage to the skin, even superficial, is a risk factor for the development of infection.
Bacteria and fungi can get into the wound.
For normal healing of damage and prevention of complications it is necessary:
- If possible, keep the problem area open for air access (minimal clothing, loose underwear)
- eliminate further mechanical impact
- regularly carry out hygiene of the inflamed perineum, immediately drying the skin in this area
- avoid excessive sweating during this period to avoid skin maceration
If there is significant damage and inflammation of the skin of the perineum, you can do sitz baths with antiseptics.
It is acceptable to use chlorhexidine or potassium permanganate solution.
You must also understand that if the skin of the perineum falls into similar conditions in which it was rubbed, the problem will repeat.
Therefore, it is worth eliminating risk factors if possible (change underwear, wear less clothes so as not to sweat).
Cuts, tears and seams
Natural resolution does not always go smoothly: often the fetus is too large, and the woman’s pelvis is not adapted to such expansion. In order not to injure the baby or cause unnecessary pain to the mother, the obstetrician makes an incision, widening the exit so that the head fits through without problems.
The incision is made to avoid rupture, since smooth tissue is easier to stitch than a lacerated wound, it heals faster and there is less risk of bleeding. This area is then sutured with non-absorbable threads. Essentially, this is a mini-surgery. Answering the question about how long the perineum hurts after childbirth, we can say that if you had such stitches, you will feel pain in the vaginal area for 3-4 weeks after childbirth.
Internal sutures will also cause you discomfort if ruptures occur during the birth process and the doctor has to stitch up mini-wounds on the cervix or in the womb. Such scars heal quickly, and the threads are then completely absorbed by the body or come out piece by piece through the vulva. Such stitches bring less trouble to the woman and after childbirth the pain between her legs is much less. In terms of intensity and time - up to 21 days.
Inflammation of the perineum due to diaper rash
Diaper rash is the result of prolonged exposure to moisture on the skin.
Under its action, the epidermis - the upper stratum corneum - softens.
It may peel off.
When high humidity of the skin of the perineum is maintained for a long time, inflammation begins.
Initially, it occurs without an infectious factor.
In the future, opportunistic bacteria or fungi that live on the skin may join.
There are quite a lot of them in the perineal area, since nearby is the intestine, populated by microorganisms.
Risk factors for diaper rash:
- hot climate
- warm clothes for the weather
- obesity
- increased sweating
- fever, thyrotoxicosis or other pathological conditions that provoke increased sweating
High humidity can also be caused by factors other than sweat.
For example, it is observed with urinary incontinence.
To avoid worsening the clinical manifestations of diaper rash and prevent infection of the perineal area, it is worth taking the necessary measures in time.
Usually, to eliminate the inflammatory process, it is enough to provide air access to the perineum.
As soon as the constant moisture of the skin leaves, it dries and regenerates.
This happens quite quickly, within 2-3 days.
However, when the process becomes more severe, when erosions, spots, papules appear, and exudate is released, the use of antiseptics and antibiotics may be required.
If the symptoms are severe, increase during treatment, or do not disappear for a long time, you should see a doctor.
Situations in which you should consult a doctor
You should contact your gynecologist if the following symptoms are observed:
- An increase in temperature in the absence of any external factors.
- Discharge of large amounts of pus.
- The appearance of unpleasant discharge that has a yellow-green color and a putrid odor.
- Increased swelling, edema.
- Seam divergence.
Self-medication and the slightest delay in such a situation can lead to dangerous consequences.
We looked at what it means when the perineum hurts after childbirth.
How did it go, what was the treatment? what helped and in general what did the doctors tell you why this happens?
I have a similar situation with my girlfriends, they didn’t immediately put ice on it for the 3rd day, the swelling hasn’t gone down, the ointment doesn’t help ;(
Inflammation of the perineum with streptoderma
Streptoderma is an inflammation of the skin caused by streptococci.
The peculiarity of these bacteria is that they can infect even those areas of the skin that do not have hair.
The most common form of superficial streptoderma remains streptococcal impetigo.
The primary element of inflammation is phlyctena in the perineal area.
This is an element of the rash that looks like a bubble with purulent contents.
It is surrounded by a rim of hyperemia.
The bladder cover is tense.
It opens up fairly quickly.
Yellow crusts appear at this place.
With a large number of conflicts, one large crust may form on a limited area of skin.
All crusts usually go away after 5 days.
Phlyctenas are characterized by peripheral growth.
That is, after they appear on the skin of the perineum, they can increase in size.
From the perineum, a person with unwashed hands can spread streptoderma to any other areas of the skin, most often to the torso, face, and limbs.
With severe inflammation, large conflicts appear in the perineum.
They can have a diameter of up to 2 cm.
This form of streptoderma is called bullous impetigo.
There is also dry streptoderma in the perineal area.
In this case, conflicts do not form.
Only red spots appear that grow along the periphery and are accompanied by itching.
Superficial streptoderma can be treated.
Local forms of antibiotics are usually sufficient.
Ointments with erythromycin help well.
Systemic antibiotic therapy is sometimes required.
Streptococcal skin infections can be severe but are easy to treat.
Because streptococci are highly sensitive to most antibiotics.
Including the oldest penicillin drugs.
If there is no adequate timely treatment, superficial streptoderma can become deep.
Its most common form is ecthyma vulgaris.
It is a deep ulcerative inflammation of the skin of the perineum.
Clinical signs are approximately the same.
Conflicts appear on the skin.
However, after opening them, deep ulcers form.
Such damage heals within 1 month.
Scars remain in their place.
What to do if you don't pass
If the swelling remains persistent and has not gone away a week after birth, or if there is a sudden appearance of unilateral swelling with redness and pain in the leg, you should consult a doctor. The examination begins with a therapist if there are complaints of pain in the lumbar region or heart area. If there is visible dilation of the veins and heaviness in the legs, they turn to a phlebologist, and in his absence, to a surgeon.
To find out the cause, the following is prescribed:
- blood tests - general, biochemistry;
- Ultrasound of vessels of the lower extremities with duplex scanning;
- Analysis of urine;
- ECG;
- X-ray of the foot and leg bones, spine.
For in-depth examination of blood vessels, rheovasography and lymphangiography are used. Ultrasound of the pelvic organs helps to examine the condition of the uterus, and the kidneys and liver are scanned with ultrasound when examining the abdominal cavity. If you suspect a decrease in thyroid function or other hormonal disorders, you need to consult an endocrinologist and analyze the level of hormones in the blood.
To reduce swelling and heaviness in the legs due to venous stagnation, it is recommended to wear compression hosiery and a support bandage during physical activity. Such medical products prevent excessive accumulation of blood in the surface layers of tissues and accelerate the restoration of blood circulation.
They must be removed at night and during rest periods. When sitting or lying down, it helps to activate the outflow of venous blood and lymph by raising the legs to an elevated position.
Women also need to wear shoes with heels no higher than 4 cm, use orthopedic insoles if necessary, limit carrying weights, and maintain body weight within normal limits.
Inflammation of the perineum due to STDs
Inflammatory processes in the perineal area can be observed with some sexually transmitted infections.
However, such symptoms are not typical for STDs; in most patients with sexually transmitted infections, the perineum does not become inflamed.
This syndrome is possible with:
- herpes
- syphilis
- gonorrhea
- trichomoniasis
- chlamydia
With STDs, inflammation of the perineum is more common in women than in male patients.
It is usually observed with severe inflammation in the vagina.
Gonococcal, chlamydial or trichomonas colpitis may be accompanied by copious discharge.
They flow into the perineal area.
Inflammation begins in this area.
Red spots, papules, and erosions appear here.
There may be discharge with an unpleasant odor.
With syphilis, elements of a secondary period rash may appear in the perineal area.
But they are also detected in other parts of the body.
Treatment of complicated irritations
Complicated diaper rash, characterized by skin damage.
Diaper rash of the second and third degrees differs:
- extensive area of lesions;
- the addition of an infection (viruses, bacteria, fungi);
- the appearance of weeping wounds and ulcers;
- increased pain syndrome;
- the appearance of signs of intoxication.
To cope with this, ointments, antiseptics and herbal lotions alone are not enough.
If, despite the measures taken, the pathology does not go away and the symptoms increase, you should visit a doctor. A dermatologist will select the optimal set of therapeutic measures and medications.
Before prescribing therapy, the doctor will assess the degree of skin damage and the general condition of the patient, and will also take a fragment of the epithelium and discharge from the affected area for analysis to determine the infectious pathogen.
In severe and complicated cases, in addition to ointments and external antiseptics, the following are prescribed:
- antibacterial (or antiviral, antimycotic) tablets;
- antihistamines;
- immunostimulants (or immunomodulators);
- non-steroidal anti-inflammatory drugs;
- drugs that relieve pain.
In some cases, hormonal treatment is indicated.
It is very important to start therapy on time so that the disease does not worsen. In the later stages, it is extremely dangerous to self-medicate. The consequences can be the most severe - treatment will have to be continued in a hospital, where doctors will have to fight not only for the health of the patient’s skin in the groin area, but often for his life.
Inflammation of the perineum due to herpes
Herpes infection quite often causes inflammation of the perineal area.
When infected, the pathogen invades the skin of the anogenital zone.
A few days after infection, a blistering rash appears.
Its elements are located on the pubis, scrotum, penis, labia, and perineum.
Classic herpetic eruptions are vesicles (bubbles with a clear liquid that becomes cloudy after a few days).
However, atypical forms also occur.
Then the rash can be represented by spots, papules, or blisters with hemorrhagic (bloody) contents.
Herpetic infection has a chronic, relapsing course.
Once infected, a person becomes a carrier of the herpes virus forever.
Sometimes the case is limited to only one acute infection, which lasts about 2 weeks.
But in 80%, the first relapse occurs within the first year after infection.
The rash appears in old places.
If initially it was localized in the perineum, then with subsequent relapses the bubbles will be there.
The severity of relapses is always lower than that of the primary infection.
But it correlates with the severity of symptoms and the duration of the disease at the first infection.
In addition, if when you first encountered the virus, herpes lasted longer and more severely, relapses are highly likely to occur more often.
Inflammation of the perineum due to skin fungus
An ideal habitat is created for fungi in the perineum.
There are folds there, they are warm and humid.
Sweat, sebum, and exfoliated cells often accumulate.
They are a nutrient substrate for fungi.
Most often, three types of fungal infections are detected in this area:
- dermatophytosis
- candidiasis
- pityriasis versicolor
Dermatophytosis is contracted from another person.
The feet are primarily affected initially.
Inflammation of the perineum in men of fungal etiology is observed more often than in women.
They bring the infection into the intimate area from their own feet, with unwashed hands.
If the fungi find these living conditions acceptable for themselves, the inflammatory process begins here.
Flaky spots appear.
They often follow the shape of folds.
Itching is often felt.
In addition, pityriasis versicolor may appear in the perineal area.
Like many other diseases, this pathology occurs when the skin humidity is high.
Usually it does not cause significant discomfort.
Round spots appear that peel off only when scratched, and almost never itch.
The disease occurs without subjective symptoms.
Stains bother a person only as an aesthetic defect.
The fungi that cause pityriasis versicolor are saprophytes of human skin.
They do not pose a significant health threat.
However, without treatment, the pathology can last for years.
Often the spots merge, and the area of inflammation of the perineum can be very extensive.
Inflammation of the perineum due to candidiasis
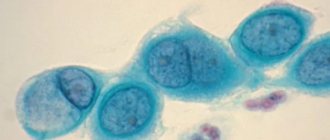
Candida belongs to the normal human microflora.
This is a fungus that is found in almost all people.
It lives in the mouth, intestines, genitals and skin.
As a rule, its growth is restrained by other representatives of the biocenosis.
But sometimes candida provokes inflammation of the skin of the perineum.
This requires predisposing factors.
These could be:
- decreased immunity
- hypothermia
- lack of proper hygiene of the intimate area
- sweating
- antibiotic therapy (antibiotics kill bacteria that compete with fungal flora)
- topical or systemic use of corticosteroids
Severe fungal processes occur against the background of immunodeficiencies and diabetes.
The main symptoms of perineal candidiasis:
- skin redness
- itching
- papules
- pustules
- cracks
- erosion
- white deposits
What tests should I take for perineal inflammation?
For successful treatment, it is important to find out why the perineum is inflamed.
Only after this can you begin treatment.
Basic tests to be taken:
- skin scraping and microscopic examination of the sample
- PCR for fungi
- PCR for sexually transmitted infections
- skin culture for infections
- blood for allergies
According to indications, studies can be carried out to determine the predisposing factors of inflammatory processes.
For example, blood is donated for sugar testing or an immunogram is done.
Typically, these tests are performed for long-term or severe inflammation of the perineum.