The liver is one of the most important organs of all mammals, including humans. This gland, located in the abdominal cavity, is both a biological filter responsible for purifying the blood of toxins and poisons, and a laboratory for the production of enzymes necessary for normal digestion and absorption of food. Therefore, the health of the entire body largely depends on the health of the liver. Medicine pays the closest attention to the prevention and treatment of its diseases. In recent years, relatively recently discovered types of viral hepatitis B and C, the viruses of which cause serious chronic liver diseases, have become widespread throughout the world.
What is hepatitis and how do its different types differ?
Viral hepatitis is the most common infectious liver disease; its contagiousness (the ability to be transmitted through contact between people) directly depends on the types of viruses.
There are many known viruses of this disease, which are usually called by the letters of the Latin alphabet: A, B, C, D, E. In Russia, cases of infection with hepatitis A, B and C viruses, transmitted in different ways, are more common. The most common and highly contagious of these is virus A, or jaundice. Its causative agent has been known to mankind for a very long time, while the causative agents of viruses B and C were discovered by scientists only in the second half of the last century.
What are the main differences between different types of hepatitis from each other and how are they transmitted from person to person:
- Hepatitis A (jaundice) is a disease belonging to the group of intestinal infections, transmitted by the fecal-oral route - through dirty water, shared utensils, and when visiting a shared toilet. This type of virus is the most contagious among the three listed, but at the same time, hepatitis A is the most favorable in terms of prognosis. Usually people become infected with it due to a lack of clean drinking water or due to poor personal hygiene. The disease proceeds without complications, recovery occurs in 100% of cases, and after it a lifelong immunity to this type of virus is developed. In the case of vaccination, which is used to prevent epidemic outbreaks of jaundice, immunity in vaccinated people remains for 10 years.
- Viruses B and C are the types most often transmitted by blood. Therefore, the risk of infection is highest in people who frequently undergo blood transfusions or work with it. This also includes drug addicts with injection addiction. Another route of infection is infection of the fetus from a sick mother during pregnancy or childbirth. When asked what kind of hepatitis is transmitted through bed, experts answer that the sexual route of infection is possible through contact with a partner infected with types of virus B or C. Based on this, we can conclude that those who are promiscuous are also in the group risk.
The last two types of hepatitis virus, in addition to the method of infection, have much in common. For example, similar signs of illness: weakness, lethargy, elevated body temperature, abdominal pain, bitterness in the mouth, nausea and indigestion, yellowing of the sclera of the eyes.
After infection, hepatitis B and C can remain latent for a long time (from several months to 1-2 years), that is, not manifest themselves in any way, which makes its timely detection very difficult.
For this reason, these pathologies tend to take a chronic course; it is very difficult to recover from such diseases, and if detected at a late stage of development, it is impossible. At the same time, they can cause serious diseases of the liver and other organs, the development of which leads to death.
But there are also significant differences between them. The main difference between hepatitis B and C is the possibility of vaccination against the first type. There is currently no vaccine against hepatitis C.
Treatment of chronic hepatitis
In case of exacerbation of chronic hepatitis, bed rest must be observed. Vaccination, sun exposure, thermal procedures, and hypothermia are contraindicated.
Treatment of autoimmune hepatitis
The leading role in the treatment of autoimmune hepatitis belongs to immunosuppressive therapy. It is carried out with prednisolone or methylprednisolone.
Immunosuppressive therapy is contraindicated in severe liver failure, severe portal hypertension with edematous-ascitic syndrome, and chronic infections.
If side effects develop after taking prednisolone or the effectiveness of glucocorticoids is insufficient, azathioprine is prescribed.
Treatment of chronic alcoholic hepatitis
The effect of treatment for alcoholic hepatitis can only be obtained if you completely stop drinking alcohol.
It is necessary to follow a nutritious, protein-rich diet.
A mandatory component of drug treatment for alcoholic hepatitis is taking ursodeoxycholic acid for several months.
Diagnosis of diseases
Each of the mentioned types of viral hepatitis has its own differences in diagnosis.
Hepatitis A is determined using various diagnostic techniques, which include:
- Urinalysis - the level of a substance such as bilirubin sharply increases in it. It is also present in the urine of a healthy person, but in much smaller quantities than in a patient.
- A general blood test, which is taken from a finger, indicates infection with jaundice by a reduced level of hemoglobin and leukocytes in the patient’s blood.
- A biochemical analysis of blood from a vein for type A hepatitis demonstrates a difference in the composition of the blood of sick and healthy people in terms of the level of specific liver enzymes - the level of alanine transaminase (ALT) and aspartate aminotransferase (AST) increases in the patient’s blood. In some cases, hepatitis A occurs without external symptoms, then an increase in ALT becomes the main sign indicating the disease. There is also an increase in alkaline phosphatase and bilirubin levels.
- Coagulogram is a test for coagulation, or blood clotting. If the level of this indicator is below normal, this may also indicate the presence of the hepatitis A virus in the body.
The main way to determine whether a person is infected with hepatitis B or C or not is to test blood samples taken from a vein.
This analysis consists of identifying different types of markers - specific types of proteins that appear in the blood as a result of the protective reaction of the body’s immune system in response to the virus entering its environment. As the virus adapts, the body produces different types of markers, the differences between which allow specialists to find out at what stage of development the disease is.
For hepatitis type B, the following markers are typical:
- HBsAg – detected in the first six months after infection, subsequently not detected;
- HBeAg is characteristic of the active phase of virus reproduction. It is detected between one and a half and five months from the moment of infection;
- anti-HBsAg - appears as a result of the development of immunity after vaccination or a previous illness. Determined after six months;
- HBcoreAg – present in the blood in the first five months after infection;
- anti-HBeAg – if detected in the fourth month from the moment of infection, it is an indicator of recovery;
- anti-HBcoreAg – determined in the fifth month of the disease and persists for a long time after recovery;
- HBcoreIgM – an indicator of the acute stage, characteristic for the period from the 2nd to the 8th month;
- HBcoreIgG – its detection indicates that the disease has become chronic.
Hepatitis C is indicated by the presence in the blood of:
- anti-HCV total – these antibodies are present in both the acute and chronic stages of the pathology. They appear two months after infection and persist for up to eight years;
- anti-HCVcoreIgG - appears around the eleventh week from the moment the virus enters the blood and persists constantly as the pathology becomes chronic;
- NS3 – characteristic of the onset of the development of pathology and is evidence of its acute stage;
- NS4/5 - appears in the later stages as an indication of deep liver damage.
If antibodies to virus B or C are detected in the blood of the subject, this may mean the following:
- He is currently infected with one of the viruses.
- The course of treatment is successfully completed, but after it the antibodies remain in the blood for some time - from several months to a year.
- The body managed to cope with the disease on its own - such a development of the situation is in principle possible, although extremely rare.
- There are also cases of the so-called false positive reaction, when antibodies are detected in the blood of a healthy person.
Among the methods that allow one hundred percent accuracy to determine the presence of a virus and the type of pathogen is PCR - polymerase chain reaction. With its help, ribonucleic acid (RNA) is detected - a gene element unique to this virus.
Pathogenesis of diseases
Moving in the blood plasma, hepatitis A and B go unnoticed. The immune system begins to react when the liver is inflamed and multiplied viruses enter the capillaries through damaged liver cell walls.
Once in the cell, hepatitis A and B use the cell's resources for their reproduction. Gradually, the hepatocyte is “overpopulated” with hepatitis A and B viruses and ceases to fulfill its main duties. Viruses that have filled the cell membrane with their protein begin to attract the attention of white blood cells - lymphocytes.
Then the liver cells are attacked from two sides: from the inside by viruses, and from the outside by the body’s own immune system, which tries to prevent danger.
What happens next? During this period, hepatitis A and B progress almost identically. A destroyed hepatocyte “releases” many copied viruses that are looking for new cells and new food. Some of them are destroyed by the immune system. But if there are too many viruses and the immune system is weak, then serious changes in the body will begin.
The consequences of the destruction of hepatocytes for other organs and systems are different. Here are some of them:
liver dysfunction; an increase in bilirubin in the blood (which causes the sclera of the eyes and skin to become yellow); the spleen enlarges; slight degenerative changes are observed in the heart muscle; kidneys are damaged.
But the most important violation is the death of liver cells. After 6 months of gradual destruction, the chronic course of the disease begins. With chronic hepatitis, the proliferation of harmful viruses periodically increases and then subsides. The affected areas become overgrown with scar tissue, and the liver begins to “fail.”
ATTENTION!
Many of our readers actively use a well-known technique based on natural ingredients, discovered by Elena Malysheva, to treat and cleanse the liver. We recommend that you check it out.
After this, the following disorders often begin in the body:
Lack of vitamins and basic elements of cell structure. Liver cells play a major role in metabolism.
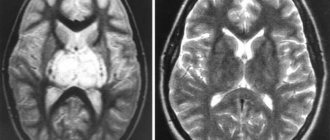
Accumulation of toxins throughout the body. As a result, hepatic encephalopathy begins. Weakness, drowsiness, anxiety, and then confusion sets in. The hepatitis B virus leads to hallucinations if a person also drinks alcohol. The patient's body stops processing fats and fat-soluble vitamins. Cholesterol accumulation. Bile produced by the liver also removes excess cholesterol from the body. Frequent bleeding. Hepatocytes form a protein used in the process of blood clotting. If it is not there, death is possible due to sudden pulmonary hemorrhage.
As you can see, the liver regulates many important life processes. Millions of chemical reactions occur simultaneously in it. Therefore, the damage caused by hepatitis A and B can be very severe.
In most cases, if the B strain virus has developed into a chronic form, after 45 years the person is diagnosed with cirrhosis.
In this regard, hepatitis B is considered very dangerous. Whereas type A is rather unpleasant and painful, but not particularly life-threatening. This virus is not chronic. It takes from 2 weeks to 2 or 3 months to heal. Of course, the process of cell restoration is long, but the liver can be completely renewed; no scars or other irreversible consequences remain.
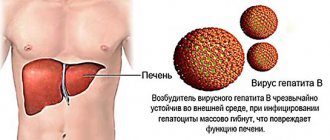
Hepatitis B
As already mentioned, the main thing that distinguishes hepatitis B (B) from C, besides the fact that it is caused by a different type of virus, is the possibility of vaccination and a better prognosis in terms of treatment and recovery.
And also the hepatitis B virus, in comparison with C, is characterized by:
- higher resistance to environmental factors - high and low temperatures, the use of disinfectants;
- lack of tendency to mutate - it has no subspecies;
- increased risk of infection;
- an indirect effect on the liver, which is autoimmune in nature, in which liver cells suffer less from the virus itself than from attacks by the immune system trying to destroy it;
- high probability of recovery - with a timely course of treatment in infected adults, recovery occurs in 90-95 percent of cases;
- development of lifelong immunity to infection in everyone who has suffered it.
At the same time, it cannot be said that infection with hepatitis B is less dangerous than infection with the C virus.
In the acute phase, option B can cause very serious complications, including:
- Hepatic encephalopathy is a disease caused by the liver losing its ability to cleanse the blood of toxic substances produced by the body and negatively affecting brain activity.
- The risk of developing massive internal bleeding due to blood clotting disorders.
However, such complications are quite rare. Compared to hepatitis C, the disease caused by the type B virus has a more pronounced symptomatic manifestation, due to which it is diagnosed in the early stages and less often becomes chronic.
What is it and what is the difference between hepatitis B and C
Differences between B and C are caused by the structure of the pathogens and include:
- Method of action on the liver. The type C virus is distinguished by its ability to independently destroy organ cells. B accumulates in gland cells - hepatocytes, causing an autoimmune reaction. This reaction is the destruction of liver cells by the immune system in order to reach the pathogen.
- Modification of an agent in the body. Virus B has a stable structure and is one of the DNA-containing pathogens. But C constantly mutates - 11 genotypes of the disease are known. This indicator affects the likelihood of developing chronic viral hepatitis.
Infections differ, which causes differences in the course of diseases caused by different pathogens.
Hepatitis C
Experts believe that hepatitis C is a more serious threat than hepatitis B.
These two types of viruses differ in the following parameters:
- virus C is less resistant to the external environment - it lends itself to boiling and other methods of disinfection, and also dies quickly at low temperatures;
- C viruses, characterized by a high ability to mutate, more easily avoid attacks by the immune system;
- the risk of becoming infected with hepatitis C is slightly lower than that of hepatitis B, since infection requires a more intense concentration of the pathological agent;
- virus C acts directly on liver cells, which leads to more destructive consequences;
- There are significantly fewer cases of recovery from type C infection - the number of recovered people is about a quarter of the total number of cases;
- In case of recovery, immunity is developed only against the variant with which the person was infected; his body is powerless against other variations of the virus.
This high mutation ability of the virus is the main reason why a vaccine against hepatitis C still does not exist. The problem remains unsolved, despite the fact that all virologists in the world are working to create a vaccine against this deadly disease.
What happens after the hepatitis virus enters the body?
Viruses travel through the bloodstream to the liver. Liver cells have a receptor protein called CD81, which the virus binds to and penetrates into the cell. Then the destructive work begins, characteristic of all viruses. The virus integrates its RNA into the genetic apparatus of the cell. And already here, as on a matrix, exact copies of the virus begin to be “printed” one after another, overgrowing a new membrane inside the cell.
This continues until the cell itself dies due to disorders incompatible with life caused by the virus, or is destroyed by the body’s own immune system. After cell death and destruction, newborn viruses enter the extracellular space and infect other, not yet affected cells. The process repeats again.
Differences in routes of infection
In terms of transmission routes, the hepatitis B virus is not much different from C.
Both of these viruses are most often transmitted as follows:
- through blood - during transfusion, injections of several people with the same syringe, when using non-sterile dental and pedicure and manicure instruments. In this case, not only the patient or client of the beauty salon can become infected, but also the doctor himself or the master providing the service;
- through vaginal discharge from woman to man - during sexual intercourse without a condom;
- through sperm from a man to a woman - infection is possible both during sexual contact not protected by a condom, and when using it;
- from mother to child - during pregnancy and childbirth.
At the same time, the risks of transmission of viruses B and C during sexual contact are somewhat different: for B they are higher than for C. A clear definition of the sexual route of transmission of the hepatitis C virus was recorded in approximately 5% of cases, the cause of about 10% of infections remained unclear.
Also, virus B can be transmitted through sweat, saliva and feces, while in C this method of infection has not yet been observed. It is not transmitted through everyday contact: through shared items, dishes, or skin contact.
Prevention of viral hepatitis
To protect yourself from hepatitis infection, you must follow simple prevention rules. You should not drink unboiled water, always wash fruits and vegetables, and do not neglect heat treatment of products. This way you can prevent hepatitis A infection.
In general, contact with other people's body fluids should be avoided. To protect against hepatitis B and C – primarily with blood. Blood in microscopic quantities can remain on razors, toothbrushes, and nail scissors. You should not share these items with other people. Piercings and tattoos should not be done with non-sterile equipment. It is necessary to take precautions during sexual intercourse.
(Visited 4,739 times, 1 visits today)
How is the treatment different?
When treating hepatitis A, gentle therapy is used using agents designed to protect the liver. These include the following drugs: Flamin, Berberine, Alahol, Cholenzym, Phosphogliv.
Since hepatitis A and E are not very different either in terms of the properties of the viruses or in terms of the method of transmission, their treatment method is also the same. But in Russia, the E virus is extremely rare - it is usually brought by tourists from countries with a hot climate and a lack of clean water resources.
The following are used to treat hepatitis B and C:
- Hepaprotectors - drugs that protect liver cells - Essentiale, Darsil, Karsil, Alahol.
- Immunomodulators that strengthen the immune status - Interferon.
- Antiviral drugs – Anaferon, Remantadine, Aflubin.
- Enzymes that facilitate the digestive process - Pancreatin, Mezim.
The hepatitis B virus has common features with the D virus and sometimes accompanies it. Treatment methods for these varieties are also common.
For viral hepatitis, therapy is aimed both at directly combating pathological agents and at generally strengthening the body in order to increase its resistance to infection and facilitate liver functioning. Therefore, taking vitamins and following a diet is of great importance.
Hepatitis E
Viral hepatitis E is caused by an RNA virus similar to rotaviruses. Methods for cloning it have been developed, and a test system has been created to confirm the diagnosis. The source of infection is patients with viral hepatitis E from the end of the incubation period and during the acute period of the disease.
The main route of spread is water; epidemic outbreaks have been described in countries with hot climates. The course resembles viral hepatitis A with a predominantly mild course and recovery. A distinctive feature of viral hepatitis E is its course in pregnant women: frequent spontaneous termination of pregnancy and rapidly increasing signs of acute liver failure with a mortality rate of up to 25% and higher.
Preventive actions
It is a well-known rule that it is easier to prevent any disease than to cure it. This is especially true for infectious diseases, including all forms of viral hepatitis.
To avoid infection, you need to:
- observe the rules of personal hygiene - wash your hands after visiting the toilet and before eating, use only personal utensils and towels;
- drink boiled or bottled water;
- do not engage in casual intimate relationships;
- do not use drugs;
- for therapeutic injections, use only disposable syringes, stored in sealed packaging until use;
- visit only those manicure and pedicure salons and dental offices whose staff carefully monitors compliance with safety rules, carefully sterilizing all instruments;
- When working with blood products or under conditions in which the blood of another person may come into contact with the skin, use protective measures - disposable latex gloves and gauze masks.
In addition, to protect against infection with hepatitis A and B, it is recommended to undergo preventive vaccination. By following these simple rules, you can be guaranteed to protect yourself from the danger of infection.
Signs of viral hepatitis
Regardless of the form of the disease, viral hepatitis has similar general symptoms:
- Dyspeptic disorders (nausea, vomiting, belching, bitterness in the mouth, loss of appetite);
- General malaise (sometimes the onset of viral hepatitis resembles the flu - there is an increase in body temperature, headache, body aches);
- Pain in the right hypochondrium (long-lasting, paroxysmal, aching, dull, radiating to the right shoulder blade or shoulder);
- Jaundice – yellowing of the skin and mucous membranes (but there are also anicteric forms of hepatitis);
- Darkening of urine, discoloration of feces;
- Skin itching.
The most unfavorable outcome of acute hepatitis is chronicity of the disease. Chronic viral hepatitis is dangerous because it gradually leads to the development of cirrhosis and liver cancer.
Epidemic hepatitis
In childhood, an exacerbation of another modification of extensive liver damage is possible - epidemic hepatitis, most often progressing in 1 - 5 years (less often in 5 - 10 years). This is the second name for “Botkin’s disease,” which is characterized by a mild form and final healing with properly selected conservative therapy. At first there is an anicteric period, but then the symptoms of the disease are as follows:
- disturbed temperature conditions;
- yellowing of the skin, sclera;
- rapid pulse;
- prostration;
- changes in the color of urine and feces;
- hemorrhagic symptoms;
- nervous breakdown.
A symptom of epidemic hepatitis is a violation of the temperature regime
These are signs of increased activity of a pathogenic infection, after which it is necessary to undergo a full diagnosis, focusing on biochemistry. There are no structural changes in the liver if a mild form of the disease is present. If epidemic hepatitis is detected, immediate hospitalization, quarantine and long-term drug therapy followed by rehabilitation are required. This is one of the forms of enteral hepatitis.
Cholestatic hepatitis
Most liver lesions tend to be chronic; cholestatic hepatitis is an option. The pathological process is accompanied by impaired outflow of bile and intoxication of the organic resource. The reason is obstruction of the bile ducts with subsequent congestion.
Symptoms:
We recommend reading:
Hepatitis E
- liver enlargement;
- yellowing of the skin;
- change in color of stool and urine;
- changes in laboratory testing;
- allergic reactions.
Cholestatic hepatitis occurs for a long time in an asymptomatic form, is diagnosed accidentally during a routine examination, and requires symptomatic and corrective therapy.
Fulminant hepatitis
If fulminant hepatitis progresses, the disease is infectious in nature. The main causative agent is HBV superinfection (HDV, HCV, HAV), other blood-borne infections that rapidly destroy liver tissue. The symptoms of the disease are as follows:
- reducing the size of the body's filter;
- laxity and softness of the parenchyma structure;
- disappearance of clearly defined edges of the organ;
- pain in the right hypochondrium;
- liver odor from the mouth.
Fulminant hepatitis in the absence of timely treatment is accompanied by foci of necrosis of the liver parenchyma. Therefore, systematic use of Interferon is indicated, and the ultimate goal is to prolong the period of remission (the disease is not curable).
In modern society, an epidemic of viral hepatitis prevails, so every person should know what measures to prevent this chronic disease, which can lead to disability and death of the body.
Cytomegalovirus hepatitis
This form of the disease progresses with increased activity of cytomegalovirus infection, which penetrates the body from the outside. The diagnosis is characterized by first an anicteric, and then an icteric period with obvious symptoms of the affected liver. This:
- yellowing of the sclera, skin;
- enlarged liver, spleen;
- change in color of stool, urine;
- allergic reactions;
- skin itching;
Hepatic bad breath is a symptom of fulminant hepatitis
- changes in laboratory parameters of blood and urine;
- symptoms of intoxication.
Cytomegalovirus hepatitis is difficult to treat and causes irreversible changes in the structure of the liver parenchyma for patients of all ages. The pathogenic infection goes through several stages of modification and remains in the body forever, producing an immune response and specific blood antibodies. CMV hepatitis is treated with the drug Ganciclovir; lifelong use is possible.
Congenital hepatitis
Acquired and congenital hepatitis are known by morphological characteristics. If the disease progresses in adulthood while the virus is active, then we are talking about an acquired diagnosis throughout life. When irreversible changes in the structure of the liver parenchyma predominate in the prenatal period, a congenital form of the disease occurs. The etiology is obvious: toxoplasmosis during pregnancy, hereditary metabolic diseases, taking illicit medications with subsequent mutations at the gene level.
A diagnosis of “Congenital hepatitis” can be made in the first days of a patient’s life; the symptoms are identical to the acquired form of the disease, but the prognosis for the future is not encouraging. It is almost impossible to achieve a complete recovery; the pathological process spreads to other organs and systems of the newborn body.
Treatment with medications
For the treatment of chronic hepatitis B, it is recommended:
Pegasys is recommended for the treatment of chronic hepatitis B
- Peginterferon alfa-2a (Pegasys). The drug is specially created to combat hepatitis B. Stops the reproduction of the virus and supports the immune system. Produced in the form of injections.
- Peginterferon alfa-2b (Intron A). A classic drug for the treatment of hepatitis B. Available in the form of injections. Recommended for children.
- Lamivudine, Telbivudine. They are analogues of nucleosides. They also effectively fight the HIV virus. With long-term use, the patient may develop drug resistance.
- Antiviral drug Adefovir.
- Tenofovir, a nucleotide analogue.
All of the above drugs are prescribed only by the attending physician. The dosage depends on age, general condition of the body, and severity of the disease.
Medicines for the treatment of hepatitis C:
- Ribavirin. A classic medicine to combat hepatitis C. Approved for children. Available in the form of injections and tablets.
- Telaprevir. It is a protease inhibitor, fights the virus, blocking its reproduction.
- Boceprevir.