This article describes the etiology, symptoms, diagnosis, treatment, prevention of venous insufficiency of the lower extremities. Blood outflow from the lower extremities is carried out through deep and superficial veins. The vessels of the right and left lower limbs are connected by special connecting or communicating veins.
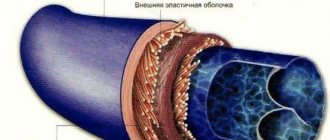
Veins have valves that help overcome the force of gravity: by closing, they prevent blood from being dumped down. When the valves malfunction, venous blood stagnates in the vessels of the lower extremities , and, as a rule, the pressure on the vascular walls increases and they expand.
As a result of this, the valve apparatus is subject to significant disturbances: the valve leaflets cannot completely close the lumen of the vein, venous blood is mixed down and cannot move up or moves only slightly. This is called venous insufficiency.
This disease is common. About 40% of the population suffers from circulatory failure.
Often people turn to specialists for help late, when the disease is in its final stages. And this poses a great danger. People are little aware of the symptoms of dangerous diseases and the manifestations that arise are considered the results of overwork during a day of work
And when characteristic dilated veins appear on the legs, they are often confused with varicose veins. Venous insufficiency can manifest itself in both the legs and the brain.
Pathogenesis
The pathogenesis of the development of acute and chronic venous insufficiency is unique. When there is a long-term obstruction of the outflow of blood through the vessels (the reasons for poor circulation may be different), an optimal environment is created for increasing the pressure in the lumen of the vein.
Due to the expansion of the veins, insufficiency of the valve apparatus develops. Each vein in the human body contains valve flaps whose job is to regulate blood circulation. If for some reason the valves do not close tightly, then the blood will begin not only to move upward (back to the heart), but also to flow down to the limbs. This will be the first symptom of the development of venous insufficiency - a feeling of constant heaviness and fullness in the legs.
If treatment is not carried out in a timely manner, the pressure in the veins will gradually only increase and the walls of the vessels will lose their elasticity. Their permeability will increase. Regional edema of the lower extremities will develop. Later, trophic disturbances will occur. They develop due to compression of the tissues that surround the venous vessels and disruption of their normal nutrition.
Complications of the disease
thrombophlebitis
Venous insufficiency is the initial stage to the formation of varicose veins, thrombophlebitis, trophic ulcers, and bleeding.
All of these diseases are chronic illnesses and are practically untreatable.
The prognosis for the quality of life of a patient with the development of these diseases is not reassuring , so one should try to prevent such complications and strive to identify VNNK at the initial stage.
Forms
- acute venous insufficiency (AVI). It develops quite sharply, due to the occlusion of the deep veins of the legs. Accordingly, the outflow of blood from them is immediately disrupted. This syndrome develops in people of advanced and working age. Its development is provoked by several reasons: acute forms of thrombosis, as well as injuries resulting in ligation of veins located in deep tissues. The pathological process affects only the deep veins; it does not extend to the superficial ones. Symptoms of AHF appear almost immediately - a person develops swelling of the legs, and the skin acquires a bluish tint. A distinctive sign of the presence of AVI is that the pattern of veins on the skin is clearly visible. A person feels severe pain in the direction of the great vessels. You can relieve pain with a regular cold compress. Its effect is due to the fact that cold helps reduce the volume of blood in the vessels;
- chronic venous insufficiency (CVI). The pathology is localized only in venous vessels located subcutaneously. It does not apply to deep ones. Only at first glance it may seem easy and harmless, but in fact, due to constant poor circulation, pathological changes develop in the trophism of the ankle joint. This form of deficiency has several stages. Not the first stage, pigment spots appear on the skin at the site of blood flow disturbance. If the patient does not seek help from a doctor in a timely manner, then gradually they become several times larger and grow into soft tissues. As a result, trophic ulcers occur (they are difficult to cure conservatively). At the last stage of CVI, blood clots form, pyoderma and other vascular abnormalities develop.
Chronic venous insufficiency
Diagnosis of the disease
It is possible to diagnose chronic venous insufficiency using ultrasound methods - Doppler ultrasound and duplex ultrasound scanning.
Doppler ultrasound allows you to study the flow of blood flow in a particular patient due to the ability of waves to change frequencies when interacting with the object being studied. In addition, with the help of this manipulation it is possible to determine the pressure in the vessels due to the reflection of ultrasonic waves from red blood cells.
Duplex ultrasound scanning is a research method that also makes it possible to determine the presence of pathologies regarding the flow of blood, as well as to objectively assess the condition of the veins.
To determine the cause of CVI, radiopaque diagnostic methods, such as venography, are used. Phlebography is carried out in the following way: a contrast agent is injected into the vein being examined, after which it is examined using radiography.
Causes
Venous insufficiency most often develops in the following conditions:
- postthrombophlebitic syndrome;
- varicose veins;
- congenital vascular pathologies;
- phlebothrombosis;
- limb injuries.
Negative factors that significantly increase the likelihood of progression of venous insufficiency of the lower extremities:
- drugs that contain hormones;
- genetic predisposition;
- female. In a woman’s body, the level of estrogen is quite high, so they are more likely to experience AVI and CVI. Also, during pregnancy and childbirth, the load on the venous vessels increases (venous insufficiency of both the legs and the brain may develop);
- obesity;
- weak motor activity;
- age. CVI is most likely to develop in older people, since their body has been affected by adverse factors for a longer period of time;
- static loads;
- chronic constipation;
- lifting weights (constant).
Additional recommendations
Any disease is easier to prevent than to treat.
Therefore, during conservative treatment, it is worth paying attention to lifestyle, nutrition, bad habits and gymnastics, avoiding a surgical solution to this problem.
Doctors recommend morning and evening walks at an easy pace for an even, gentle load on the veins of the lower extremities, which naturally increases their tone.
Light morning exercises are practiced for the same purpose. You should normalize your daily routine, give up alcohol and smoking, which negatively affect vascular tone. It is not recommended to abuse fried and salty foods.
At-risk groups
Lymphovenous insufficiency develops in people during the most active period of their life - from 20 to 50 years. But only a few patients seek help from qualified doctors as soon as they begin to feel the first symptoms of the disease. There are some groups of people in whom pathology develops most often:
- athletes;
- people who have a genetic tendency to CVI;
- overweight people;
- pregnant women.
Classification
Classification of CVI
The most common classification of chronic venous insufficiency is the following:
- degree 0. In this case, there are no pronounced symptoms of the disease. The patient does not notice any changes. Functionality preserved;
- degree 1. This degree is characterized by the appearance of the first symptoms indicating the presence of a pathological process in the body. The patient feels pain in the lower extremities, a feeling of heaviness and fullness. Soon pronounced, persistent swelling and cramps appear (more pronounced at night);
- degree 2. Swelling does not disappear. On examination, eczema, hyperpigmentation, lipodermatosclerosis are noted;
- degree 3. Trophic ulcers form on the surface of the extremities. This condition is the most dangerous for the patient's health.
There is also an international classification of WHI and CVI - the CEAP system.
Classification of venous insufficiency according to CEAP
According to the clinical picture:
- 0 – there are no visual signs of a person having pathology of the venous vessels;
- 1 – telangiectasia;
- 2 – varicose veins on the legs are visually noted;
- 3 – persistent swelling appears;
- 4 – changes appear on the skin;
- 5 – changes on the skin in the presence of an already healed ulcer;
- 6 - changes on the skin in the presence of a fresh ulcer.
Etiological classification is important, since the treatment of venous pathology largely depends on the causes that provoked chronic circulatory failure.
Etiological classification:
- EC – genetic predisposition;
- ER – unknown cause;
- ES – deficiency develops in a person due to injury, thrombosis, etc.
Anatomical classification according to the CEAP system makes it possible to display the level of the lesion, segment (deep, superficial or communicating), as well as the localization of the pathological process (inferior vena cava or great saphenous vein).
Classification of CVI according to the CEAP system, taking into account pathophysiological aspects:
- chronic insufficiency of venous circulation with reflux symptoms;
- CVI with manifestations of obstruction;
- Combined CVI (combination of reflux and obstruction).
The classification of acute and chronic circulatory failure is used in medical institutions by phlebologists to determine the stage of the disease, as well as its severity. This is necessary to prescribe appropriate effective treatment.
The mechanism of pathology development
The disease develops gradually and, depending on the measures taken to treat the pathology, the following stages and changes in the body occur:
- with a gradual loss of vascular elasticity, venous fluid stagnates during insufficient physical activity;
- the more the venules stretch and thin out, the larger the lumen appears inside the vessels. As a result, the functioning of the valves is disrupted, they allow blood flow back;
- through thinned vascular walls, blood plasma enters the adjacent tissues, which causes swelling of the legs;
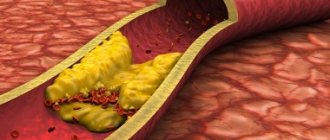
- in prolonged stagnant blood locations, thickening of the biofluid occurs, the appearance of metabolites, inflammatory processes, and the formation of free radicals;
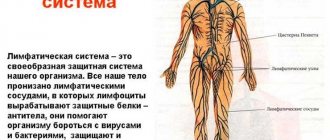
- pressure on the vascular walls increases, as a result of which lymphatic fluid cannot enter the venules and drain excess from the lymph nodes. The process disrupts the overall metabolism in the body;
- stagnation, pressure, decay products in the venous blood, plasma effusions cause disruption of the skin and the formation of trophic ulcers.
It is important to diagnose the disease at an early stage in order to prescribe adequate treatment. CVI in an advanced stage is not amenable to drug therapy.
Symptoms
Symptoms of AHF appear quickly, as blockage of blood vessels occurs very quickly. Due to the impossibility of blood flow from the lower extremities, edema occurs. Along the course of the vessels, the patient notes the occurrence of severe pain, which does not go away when changing position or at rest. The skin takes on a bluish tint and a pattern of veins appears on it. This form of the disease is easier to treat. First aid is applying a cold compress and taking painkillers. Further treatment will be prescribed only by a phlebologist.
Symptoms of the chronic form of the disease can vary. Therefore, the clinical picture of chronic circulatory failure may differ slightly in different people. In the first stages of development of the pathological process, either one or a complex of symptoms appears:
Symptoms of CVI
- most often a person begins to worry about heaviness in the legs, which increases significantly after a long stay in a standing position;
- formation of edema in the lower extremities;
- night cramps;
- hypopigmentation or hyperpigmentation of the skin;
- the skin loses its elasticity and becomes dry;
- in later stages, trophic ulcers form on the surface of the skin;
- Due to the deposition of a large amount of blood in the legs, a person experiences dizziness and fainting.
If you have at least one of the above symptoms, it is recommended to immediately seek emergency medical help at a medical facility. There, based on the data from the initial examination and diagnosis, the doctor will determine the severity of the disease (using an approved classification) and will also prescribe an appropriate course of treatment.
Treatment
Acute venous insufficiency is eliminated in several stages. During the active phase of the disease, it is necessary to apply a cold compress to the location of the pathological process. The cooled cloth is applied for two minutes, after which it is placed in a container with ice and water to cool. It is recommended to repeat these steps for an hour. After the inflammation is relieved, the second stage begins - improving blood circulation. You can use ointments that contain substances that slow down blood clotting.
CVI is much more difficult to treat than acute. When determining the correct tactics for treating chronic circulatory failure, it should be clearly understood that this pathological condition is a systemic process. The main goal of all therapeutic measures is to restore normal blood circulation in the venous system of the lower extremities, as well as to prevent the development of possible relapses.
- Treatment of the disease is carried out in several courses. It all depends on the severity of the symptoms and the severity of the pathology;
- treatment of venous insufficiency is selected strictly individually;
- drug therapy is combined with other methods of treating circulatory failure.
The greatest importance in the treatment of CVI is the use of synthetic drugs (phlebotropic drugs are prescribed), as well as elastic compression. Topical medications are also prescribed.
Surgical treatment is carried out to remove pathological venous discharge, as well as to remove areas of varicose veins.
Surgical treatment of CVI
Operative techniques
Surgical treatment of venous insufficiency of the lower extremities takes place in cases where conservative methods no longer help and the disease progresses. Clear indications for surgery are:
- the presence of trophic disorders;
- relapses of varicothrombophlebitis;
- pathological venous reflux.
It is not advisable to use surgical treatment in cases where the patient has posttrophic syndrome. All operations performed for CVI can be divided into 2 groups:
- Disconnection operations.
- Phlebectomy.
With surgical separation, pathological reflux is removed from a certain area of the deep veins. In such cases, an incision is made in the inguinal fold. Thus, the surgeon is able to reach the great saphenous vein. All estuarine tributaries must be bandaged during manipulation. The intersection of the small saphenous vein is carried out through an incision at the site of the sapheno-popliteal anastomosis. Crossing of perforating veins can occur in two ways:
- with a small (up to 1 cm long) incision - this operation is performed if venous insufficiency does not have serious problems, but trophic changes are noticed;
- subfascial - the operation involves the use of endoscopic technology, and occurs in cases where the incision can provoke the appearance of a trophic wound, purulent-necrotic complications.
Phlebectomy
Phlebectomy - surgical interventions involve the complete removal of some veins. Venous trunks are usually removed using plastic or metal special probes (this is the so-called Babcock operation).
Short stripping is a surgical option in which a large vein is removed along the entire thigh and in the upper part of the lower leg. Long stripping, which involves the complete removal of a large vein, is performed only when, during an ultrasound, the doctor notices insufficiency of the venous valves along the entire vein.
It is possible to get rid of varicose veins thanks to the so-called Narata operation. Removal is carried out through small punctures in the skin, and the main work of the vascular surgeon is performed using a miniflextractor (special tool). In this case, no stitches are required. The likelihood of postoperative complications is significantly reduced.
Chronic cerebrovascular insufficiency
This disease deserves special mention, since it can develop in absolutely any person and is a rather serious pathology. Chronic venous insufficiency of the brain can occur even with singing, physical stress, squeezing the neck with a too-tight collar, etc. As a rule, patients do not complain about the deterioration of their general condition for a long time. This is explained by the fact that the brain has an amazing compensatory mechanism and a developed circulatory system. Therefore, even serious difficulties in the outflow of blood do not appear for a long time. This is the greatest danger of this condition.
Causes:
- asphyxia;
- scoliosis;
- cessation of nasal breathing;
- traumatic brain injuries;
- neck and spine injuries;
- brain tumors;
- asthma;
- thrombosis and thrombophlebitis in the brain;
- venous and arteriovenous hypertension.
Symptoms:
- regular headaches;
- dizziness;
- apathy;
- memory loss;
- muscle weakness;
- numbness is felt in the limbs;
- the appearance of darkness in the eyes;
- mental disorders of varying severity.
Symptoms of CVI of the brain are similar to the symptoms of many diseases of the cardiovascular system, so it is important to conduct a thorough differential diagnosis. If blood circulation in the brain is disrupted for a long time, irreversible changes may occur in it that are dangerous to the health and life of the patient.