How to improve blood circulation in the legs of older people.
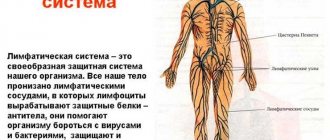
Thanks to good blood circulation in the legs, the tissues absorb nutrients and get rid of waste, which promotes health and strengthens the strength of the legs.
Foot circulation can be improved by following simple habits, taking herbs and other nutritional supplements, and making changes to your diet. Find out how to improve blood circulation in your legs. Method 1 of 4: Follow good habits.
Don't sit or stand for too long. It's important to move throughout the day to keep blood moving through your legs. Only if you sit or stand for a long time does the blood stagnate, which is harmful to your health. In case you find yourself in one position for an hour or more, make a few movements.
In case you work in an office and have to sit for a long time, get up and take breaks every hour and a half or so. Even just walking to the bathroom and back to your desk will keep your legs moving, which gets your blood flowing. You can also switch from a sitting desk to a standing desk, which allows you to stand rather than sit while you work.
Take a position that will promote blood circulation. Perhaps you cross your legs when you sit. This position cuts off the circulation in the legs, which prevents blood from flowing to the tissues of the legs. Get into the habit of sitting in a position that does not interfere with your blood circulation. Sit with your legs slightly apart and your feet flat on the floor.
Remember to stand up from time to time so you don't stay in this position for too long. You can also elevate your legs a little to promote blood circulation. Place your feet on a stool 15-30 cm high. Exercises. Attention! Only if your schedule allows you to do some exercises, your blood circulation will definitely improve.
Any exercise that involves your legs stimulates blood circulation. Try race walking, running, cycling, swimming, hiking and other exercises that you enjoy and that will get your legs moving. For maximum benefit, exercise daily. Even half an hour of walking will improve the health of your feet.
If you're looking for low-impact exercise, try relaxation exercises. There are many relaxing poses that engage the legs and stimulate the cardiovascular system. Wear comfortable shoes. High heels, pointy shoes, or other tight footwear can impede blood flow from the feet to the heart.
So, if you care about improving circulation in your feet, it is important to wear comfortable, low-heeled shoes with good cushioning. Wear sneakers or moccasins that allow your feet to breathe. Swap pointed shoes for shoes with round or almond toes. If you need extra height, opt for platforms rather than heels.
Wear compression stockings. Similar to tights, but specifically designed to stabilize leg tissue and stimulate circulation. You can buy them at the pharmacy or contact your doctor to order stockings that meet your individual needs. Stop using tobacco.
can lead to peripheral artery disease, a condition in which the arteries in the legs harden and can no longer pump blood. Only if you have poor circulation, it is extremely important to stop smoking and using other tobacco products to restore the health of your feet.
Method 2 of 4: Take herbs and supplements.
Try birch bark tea. it stimulates the cardiovascular system. You can drink it not only as a supplement, but also simply as tea, especially if you add a little ginger to it. Include a cup of this tea in your daily diet. take ginkgo supplements. Ginkgo tree has long been used for medicinal purposes, and there is evidence that it dilates blood vessels and improves circulation.
It is recommended to take 120-240 mg of ginkgo leaf extract per day. divide it into two or three servings. drink cayenne pepper tea. that this hot pepper helps dilate blood vessels and improves blood circulation. You can sprinkle it on food or add it to tea with honey.
Consuming cayenne pepper daily improves blood circulation over time. Take fish oil supplements. fat contains omega-3 fatty acids, which are essential for a healthy lipid profile. Having a high level of “Good” cholesterol, it increases blood circulation. Fish oils are sold in capsule form and are usually made from mackerel, tuna, cod liver, salmon or herring.
Method 3 of 4: Eat a healthy diet.
Eat eat less salt. causes your body to retain water and swell, which can affect venous pressure and lead to poor circulation. Try to halve your salt intake and avoid adding salt to food after cooking. Try to cook more at home rather than eat out in cafes and restaurants.
You never know how much salt you put in your food, and there's usually more than you think. Avoid salty snacks, fast foods, and microwaved foods. Drink plenty of water to flush salt out of your body. You need to drink about 2 liters of water per day to replenish its reserves in your body.
Maintain a healthy body weight. Part of keeping your legs and feet healthy and improving your circulation is maintaining a healthy body weight. Excess excess weight puts additional stress on the circulatory system. eat a balanced diet and consult your doctor to achieve a weight that is suitable for your body type.
Method 4 of 4: Medical assistance.
Talk to your doctor about improving your blood circulation. So, if lifestyle changes and healthy habits don't help, you may have a more serious health problem called peripheral artery disease. Talk to your doctor about whether you may have this and what treatment is available to you.
Peripheral artery disease occurs when plaque builds up in the arteries, preventing blood from flowing from the feet to the heart. This leads to leg pain and other symptoms of poor circulation. Peripheral artery disease is usually treated with medications to relieve leg pain and lower blood pressure and cholesterol levels. Also, peripheral arterial disease is sometimes treated by heart surgery.
Possible causes of poor circulation in the legs
Poor circulation in the legs can have various causes. The most common of them:
- Diseases of the peripheral arteries of the lower extremities (endarteritis and atherosclerosis), which lead to narrowing of blood vessels.
- Diabetes mellitus – this disease carries the risk of damaging blood vessels throughout the body, including the legs. The condition is aggravated by the fact that diabetes affects not only the arteries, but also the nerve fibers, which causes sensitivity in the legs to worsen.
- Varicose veins are dilation of veins caused by insufficient valves. Varicose veins cannot drain blood well from the lower extremities, and therefore stagnation develops in the legs.
- Thrombosis is a serious problem that can interfere with the flow (in arterial thrombosis) or drainage (in venous thrombosis) of blood from the lower extremities.
- Obesity – Excess weight impairs circulation in the legs.
Treatment of circulatory problems in the legs should begin with non-drug measures, including lifestyle changes, a balanced diet and exercise to improve circulation. Exercise is very important for good blood circulation in the legs. Any type of exercise increases blood circulation throughout the body, but walking in the fresh air is especially beneficial for the lower extremities. When walking, contraction of the leg muscles improves venous outflow and enhances the formation of collateral vessels.
Cardiologists risk losing their jobs—hypertension is now curable!
Swimming is also very beneficial for blood circulation in the legs and for improving overall health. Any moderate physical activity increases systemic blood circulation and strengthens the heart muscle. However, you should remember that you need to increase the intensity of exercise gradually.
A rational and balanced diet improves the rheological properties of the blood and the condition of the vascular walls, positively affecting blood circulation not only in the legs, but throughout the body. To this end, you need to eat enough vegetables and fruits, fish, whole grains and water, and also limit your intake of fatty foods of animal origin.
- Complete smoking cessation. Smoking has a very bad effect on blood vessels, contributing to the narrowing of their lumen, and also reduces the ability of the blood to carry oxygen and increases the risk of blood clots.
- Using hot water bottles to warm cold feet.
- Contrasting warm and cold baths.
- Tight clothing and socks should be avoided.
- You need to take care of your feet. This is especially important for people with diabetes. Wear suitable footwear and pay attention to any scrapes, cuts or injuries. When blood circulation is impaired, tissues recover more slowly and are more prone to infection.
- You cannot stand in one place for a long time or sit for a long time.
- For venous congestion in the legs caused by varicose veins or thrombophlebitis, wearing compression stockings may be helpful.
- Massage of the lower extremities, which can often improve blood circulation.
Drug treatment depends on the cause of the deterioration in circulation. In case of diabetes, it is very important to achieve its compensation and normalize blood sugar levels. For diseases of peripheral arteries and thrombosis, drugs that affect blood clotting are prescribed - antiplatelet agents (Aspirin, Clopidogrel) and anticoagulants (Warfarin, Xarelto, heparins).
If drug therapy and lifestyle modifications are ineffective, surgical interventions are possible for some diseases. For diseases of peripheral arteries, vascular bypass surgery, angioplasty or stenting, and removal of atherosclerotic plaque are performed. In case of arterial thrombosis, I remove the clot. For varicose veins of the lower extremities, sclerotherapy, laser surgery, and phlebectomy are possible.
Poor circulation in the lower extremities, as we said earlier, is just a symptom that occurs as a result of a pathology that occurs latently in the body. And so far the only sign of its progression is the problem with the legs.
Why does this condition arise?
- First of all, let's pay attention to lifestyle. This health-impairing factor depends entirely on us. We can say that it is easiest to eliminate such a reason if it is done on time. An unhealthy diet, eating fast food, smoking and uncontrolled excessive drinking of alcohol have a detrimental effect not only on the circulatory system, but also on the entire body as a whole.
- Physical inactivity is the scourge of the modern world. It is low mobility that leads to disruption of the entire functioning of the body. In this case, it will not be difficult to restore blood circulation to the legs. Swimming with light jogging, playing simple sports, walking in the fresh air and daily morning exercises will help cope with the problem.
- According to statistics, peripheral circulation disorders are most observed in the legs. This is caused by an increased level of “bad” cholesterol (low-density lipoproteins), which accumulate in the form of fatty deposits on the walls of blood vessels, causing a narrowing of their lumen.
- Diseases of the endocrine system: obesity, diabetes mellitus and diabetes insipidus. Systemic diseases of various origins, such as: hypertension with renal and liver failure and others.
- Taking certain types of medications for a long time. This could be the treatment of a chronic illness, which was not carried out very correctly, or the use of hormonal contraceptives, which were either not suitable for the patient or were taken uncontrolled.
These are the most common causes of microcirculation disorders in the legs.
Treatment of circulatory disorders in the lower extremities should be aimed primarily at eliminating the underlying disease in combination with an impact on local symptoms.
Causes of circulatory disorders of the lower extremities
Embolism of the arteries of the lower extremities, in which the collateral circulation is insufficiently developed, can lead to acute ischemia of the legs. This is a serious pathological condition that requires immediate surgical intervention, the purpose of which is to restore and improve normal blood flow in the affected area of the artery. Patients who have undergone surgical treatment need to take medications in the postoperative period to improve blood circulation in the vessels of the legs.
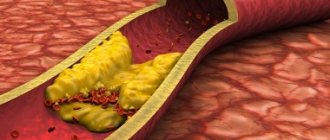
Chronic arterial insufficiency is observed with obliterating atherosclerosis of the vessels of the lower extremities. This disease is characterized by general metabolic disorders, in which there is complete or partial blockage of the artery lumen by cholesterol plaques. Atherosclerosis at the initial stage requires conservative therapy. Since the etiology of the disease is known, therapy is prescribed aimed at reducing the amount of cholesterol.
Groups of drugs used to treat acute arterial obstruction and improve microcirculation (in a compensated state, when there are enough collaterals): thrombolytics, anticoagulants, disaggregants, antispasmodics.
Table. Characteristics of medicinal substances for the treatment of acute arterial insufficiency of the lower limb vessels.
| Thrombolytics | They dissolve the formed blood clot directly in the lumen of the vessel, improve blood viscosity, and as a result, circulation in the arteries of the legs is restored. They have contraindications. |
|
| Indirect anticoagulants | They inhibit blood clotting processes by directly influencing coagulation factors (thrombin formation). In case of overdose, bleeding is possible. | |
| Able to increase blood flow in the lower extremities due to improved blood viscosity. They inhibit thrombus formation by blocking the synthesis of vitamin K-dependent blood clotting factors. They have a long-lasting effect. |
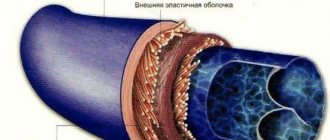
Obliterating atherosclerosis of the vessels of the lower extremities is a chronic vascular disease that develops due to lipid metabolism disorders, leading to the formation of atherosclerotic plaques, thickening of the walls of the arteries of the legs and a decrease in the vascular lumen. All these changes can lead to partial or complete cessation of blood flow.
At first, this pathology practically does not manifest itself in anything, but as this disease progresses, atherosclerotic plaques increasingly narrow the lumen of the vessels and can completely block it, leading to ischemia and even necrosis of the tissues of the lower extremities. This development of the disease can result in the development of gangrene and loss of a leg.
According to statistics, over the past 10 years there has been a steady increase in the number of patients with obliterating atherosclerosis of the lower extremities. This disease occurs in approximately 10% of the world's inhabitants. Most often the disease affects people (mostly men) over 70 years of age. From this article you will learn about the causes, signs, diagnosis and principles of treatment of this pathology in order to “be fully armed.” But, as you know, it is easier to prevent a disease than to treat it, and therefore in the article we will also touch on the prevention of the disease.
Signs
Other localizations of this pathology are much less common.
Atherosclerotic plaques attached to the walls grow with connective tissue, and platelets and calcium salts settle on them. Such changes lead to destruction and occlusion of arterial walls.
When palpating the affected artery, no pulsation is detected. As the disease progresses, areas of darkening may appear on the surface of the skin of the affected leg (incipient gangrene).
During obliterating atherosclerosis of the lower extremities, the following stages are distinguished:
- Stage I (initial manifestations of stenosis) – a feeling of goosebumps, pale skin, a feeling of coldness and chilliness, excessive sweating, rapid fatigue when walking;
- Stage II A (intermittent claudication) – a feeling of fatigue and stiffness in the calf muscles, squeezing pain when trying to walk about 200 m;
- Stage II B – pain and feeling of stiffness prevent you from walking 200 m;
- Stage III – squeezing pain in the calf muscles becomes more intense and appears even at rest;
- Stage IV – signs of trophic disorders, long-term non-healing ulcers and signs of gangrene appear on the surface of the leg.
In advanced stages of atherosclerosis of the lower extremities, the development of gangrene often leads to complete or partial loss of a limb. The lack of adequate surgical care in such situations can lead to the death of the patient.
Also, atherosclerosis of the lower extremities can be complicated by arterial thrombosis. This complication, in the absence of prompt medical attention, leads to the loss of a limb or, in the case of detachment of multiple blood clots, to embolism of other arteries. If a detached thrombus enters a coronary artery, the patient may develop myocardial infarction. If the blood clot migrates to the carotid artery, it is a stroke.
Diagnostics
After determining the stage of the disease, the patient is offered comprehensive treatment.
Treatment
The treatment tactics for obliterating atherosclerosis of the vessels of the lower extremities depends on the stage of development of the pathological process and may include conservative or surgical techniques.
To treat obliterating atherosclerosis of the vessels of the lower extremities, physiotherapeutic procedures (microcurrents, laser therapy), balneotherapy and hyperbaric oxygenation can be prescribed.
Indications for surgery may include:
- signs of gangrene;
- intense pain at rest;
- thrombosis;
- rapid progression or stages III-IV of atherosclerosis.
When performing such minimally invasive operations, angiography is used to control the manipulations being performed. These interventions can be performed in specialized hospitals. After the operation, the patient is under medical supervision for 24 hours, and the next day he can go home.
In addition to such reconstructive operations, additional auxiliary surgical techniques may be used:
- revascularizing osteotomy - stimulation of the growth of new small blood vessels by damaging the bone is performed;
- sympathectomy - the intersection of nerve endings that provoke spasm of the arteries, is carried out when repeated blockages of the arteries form.
In the event of the formation of large-scale non-healing trophic ulcers or when signs of gangrene of the limb appear, plastic surgery using flaps of healthy skin after removal of necrotic areas or amputation of part of the lower limb can be performed.
The prognosis for the treatment of obliterating atherosclerosis of the vessels of the lower extremities is favorable if the patient contacts an angiosurgeon early. During 10 years of development of this pathology, the development of thrombosis or gangrene is observed in 8% of patients.
Prevention
Obliterating atherosclerosis is the most common disease of the arteries of the lower extremities.
The disease can also affect the upper limbs and aorta, but most often the legs are its target.
Obliterating atherosclerosis is manifested by deterioration of blood circulation due to the accumulation of cholesterol and fats on the walls of blood vessels.
The resulting dense plaques interfere with the normal outflow of blood and lead to a decrease in the lumen of the arteries. In the absence of proper treatment, serious consequences are likely, including the development of gangrene.
This disease occurs mainly in elderly people over 60-65 years of age; in this age category, more than 5% of the population suffers from atherosclerosis obliterans.
But the disease sometimes develops at a young age: among 30-40 year olds, 0.3% of cases of the disease are observed. Males are more susceptible to atherosclerosis.
The disease does not develop on its own even in very elderly people. Its appearance is facilitated by certain risk factors that may have occurred in the past.
Smoking. The most important factor of the disease. According to statistics, more than 90% of people with atherosclerosis of the lower extremities are heavy smokers.
Excessive drinking of alcohol. For this reason, pathological processes in blood vessels are accelerated.
Abuse of fatty and fried foods. And, as a result, excess cholesterol in the body, which is deposited in the blood vessels.
Constant stress and increased nervousness. Because of them, blood circulation worsens.
Lack of movement, physical inactivity. All major processes in the body slow down, which also leads to atherosclerosis.
The presence of certain diseases. Ailments such as diabetes, obesity, rheumatism and hypertension increase the risk of atherosclerosis.
Often the disease proceeds unnoticed by the person himself, sometimes until a serious and threatening stage occurs.
But the time comes and the symptoms make themselves felt.
And they appear as follows:
- numbness of the feet;
- progressive lameness;
- high sensitivity of the feet to cold;
- constant feeling of coldness in the legs, chilliness;
- spasms of the lower extremities, mainly at night;
- difference in the temperature of the legs (the skin of the diseased leg is cooler than the healthy one);
- periodic pain while standing still;
- ulcers and other disorders that appear on the skin of the legs;
- embolism or acute thrombosis (in rare cases).
Causes
Circulatory disorders of the lower extremities are arterial and venous. The causes of venous circulation disorders are mainly varicose veins and thrombophlebitis.
The veins of the legs are divided into superficial and deep. They do not have the ability to contract because they do not have a muscle wall. In this case, the blood from the lower extremities must rise upward with force, since it is held at the bottom by gravity.
This is facilitated by the muscular system of the legs and the pressure of blood flow from the arteries. When the muscles contract, they work like pumps, pushing blood out of the lower veins and sending it to the upper ones. In a calm, relaxed state of the muscles, the upward movement of blood flow is carried out due to the pressure of blood from the arteries. It rises thanks to valves that are located in the connecting veins.
If the veins for some reason become less elastic, the valve apparatus atrophies and varicose veins occur. It is a sign of impaired venous circulation. Varicose veins in most cases are a hereditary disease.
Thrombophlebitis is also inherited, but is sometimes a complication of varicose veins. It is an inflammation of the walls of the veins due to the presence of blood clots in them. When blood clots partially block the gaps in the veins of the legs, they interfere with the normal process of blood flow in them. As a result, a violation of the venous circulation of the lower extremities is formed.
As for arterial circulatory disorders of the legs, its causes are usually:
- atherosclerosis of leg vessels;
- endarteritis;
- diabetic angiopathy.
With atherosclerosis, cholesterol, which forms fatty plaques, is deposited in the arteries of the legs. As a result, the lumen of the arteries narrows and interferes with the normal flow of blood through them.
Endarteritis is a systemic inflammatory disease, the etiology of which is still unclear. It affects the small arteries of the feet and legs, reducing their lumen and preventing normal arterial blood flow. Endarteritis is observed mainly in men under the age of 50 years.
Risk factors
Poor circulation of the lower extremities can be caused by:
- Sedentary lifestyle, sedentary/standing work;
- Increased levels of homocysteine (a sulfur-containing amino acid that is formed in the body during the processing of methionine);
- Alcohol abuse;
- Smoking;
- Obesity;
- Diabetes;
- High blood pressure;
- Lipid metabolism disorders;
- Stress;
- Mature age.
Causes of pathology
The main reason leading to impaired blood circulation in the lower extremities is a sedentary lifestyle. Most people, due to the nature of their work, are often in a sitting position, which leads to stagnation of blood in the veins. Pain appears in the legs, they begin to get tired quickly and become cold.
Many people, especially older people, constantly feel a little chilly, but after a short walk they feel warm. This is explained by the fact that even such a small physical activity increases blood circulation, relieving cold feet syndrome.
How to improve blood circulation in the legs? In this case, no special treatment is required, just a little change in your lifestyle is enough. If you start moving more, the illness can go away on its own, and simple morning exercises will help improve the general condition of the body.
Other reasons, and not so harmless ones, can lead to impaired blood circulation in the lower extremities. Such a pathological condition may be a sign of malfunction of an organ. That is why it can be difficult to understand what exactly contributed to the development of the disease and what treatment is required.
The following are the most common causes of circulatory problems in the legs:
- alcohol and smoking;
- age-related changes;
- high cholesterol levels in the blood;
- ischemia, atherosclerosis;
- diabetes;
- hypertension;
- overweight;
- varicose veins, thrombosis and arterial stenosis.
Products that improve blood circulation in the legs. Drug treatment
Drugs that improve blood circulation in the legs should only be prescribed by a doctor. After questioning and external examination of the patient, he is sent for examination. Based on the results obtained, the doctor prescribes the necessary medications to normalize blood circulation in the lower extremities. So how can you improve blood circulation in your legs? To do this, use the following means:
- Angioprotectors. They are necessary to improve microcirculation, as well as normalize vascular permeability, so that normal metabolic activity returns to the walls. These include “Curantil”, “Persantin”, “Trental”, “Flexital”, “Doxy-Chem”, “Pentoxifylline”, “Radomin”, “Vazonit”.
- Low molecular weight dextran drugs. Thanks to such drugs, additional blood volume flows from the intercellular space into the bloodstream. As a result, blood flow is significantly improved. The following medications belong to this category: “Reomacrodex” and “Reopoliglyukin”.
- Preparations containing prostaglandin E1 (“Vasaprostan”). Thanks to them, blood flow improves and microcirculation is normalized. These drugs also help to expand blood vessels and normalize blood pressure.
- Calcium channel blockers, which even affect the blood vessels of the brain. These include: “Kordafen”, “Kordaflex”, “Adalat”, “Stamlo”, “Norvax”, “Plendil”, “Foridon”, “Latsipil”.
- Antispasmodics of myotropic action. With the help of such medications, blood vessels dilate and blood begins to circulate freely. In addition, they relieve spasms well. Such medications are “Mydocalm”, “Cavinton”, “Eufillin”, “Halidor”.
How to stabilize blood circulation in the vessels of the legs
Discomfortable symptoms in the legs, such as systematic pain, lameness during sudden movements or exertion, and limb cramps are an indicator of poor blood circulation. Such precedents force people faced with a problem to look for a question to answer: what to do when poor blood circulation in the legs interferes with normal life, what actions to take first? The answer to these questions is clear: you need to visit a medical facility to identify the original source of the problem. The doctor, based on the patient’s complaints, studying the family history, conducting the necessary examinations of the body and standard laboratory tests, will be able to make a diagnosis, the variation of which determines the methodology of further treatment.
Methods for restoring blood circulation in the legs depend directly on the primary source of the disease and the neglect of the disease. If the disease is at an early stage, and there are no critical pathologies among the causes of the disease, it is often possible to restore blood flow without the use of drastic measures, by coordinating the patient’s lifestyle, using alternative therapy, special exercises and physiotherapeutic procedures. In more complex situations, radical treatment will be required, with the inclusion of medications in the complex of treatment measures. Situations with advanced cases may require mandatory surgical intervention, which may consist of either removing the blockage of a vessel or expanding the stenotic segment with a special expander, or amputating a limb, at least if it is impossible to stop the process of necrosis and rotting by medicinal methods.
Drug therapy
Making a specific diagnosis for the patient is helpful for prescribing measures for the treatment of blood circulation disorders in peripheral vessels. According to the regulations, the doctor initially prescribes drugs to the patient, the action of which is aimed at eliminating the provocateur of the disease. Often, the patient is prescribed a complex of drugs, both in tablet or injection form, and in the form of ointments or gels. The basis of complex treatment of the disease are drugs to improve blood circulation of the following drug groups:
- Antiplatelet agents, the action of which is aimed at normalizing blood circulation by stopping and preventing atherosclerotic processes.
- Anticoagulants that prevent thrombosis by inhibiting blood clotting.
For vein pathologies, vascular drugs are used to improve blood circulation in the legs from the category of phlebotropic and venotonic drugs. Frequently prescribed drugs in these categories include tablets such as Detralex, Venoruton and Antistax; ointments such as Troxevasin or Escin can be used for topical application, which, in addition to strengthening and toning the venous walls, have a powerful anti-inflammatory effect. In complex treatment, non-steroidal anti-inflammatory drugs, such as Indomethacin or Diclofenac, available both in injection forms and in tablets or ointments, can be used. Combinations of drugs, as well as their type, are determined by the treating doctor, depending on the diagnosis and medical indications, the complexity of the disease and disturbing symptoms.
Alternative medicine
Of no small importance in the comprehensive restoration of blood flow in the vessels of the lower extremities is given to methods of alternative medicine, time-tested and proven effective in practice. You can improve the condition of blood vessels at home by taking products prepared according to the following recipes:
- Horse chestnut flowers, weighing fifty grams, must be infused in a dark place with half a liter of vodka for fourteen days, shaking the container with the tincture every day. Take one teaspoon of the tincture three times a day before meals, first diluting it in a glass of water at room temperature. Treatment must be carried out in ten-day courses, with five-day breaks.
- Take three hundred grams of hazelnuts and prunes, five hundred grams of raisins and walnuts, grind all the ingredients in a blender or meat grinder. Fifty grams of honey are added to the finished mixture, the resulting medicine is taken one tablespoon before each meal.
- Decoctions of adonis or wild rosemary have a beneficial effect on blood circulation. To prepare the potion, you need to take a spoonful of the crushed plant, pour a glass of boiling water and simmer over low heat for half an hour, let the potion brew and strain. The resulting decoction must be stored in the refrigerator, take one spoon three times a day. The course of therapy should not exceed a month.
If blood flow in the region of the lower extremities is poor, baths are often used at home. Pine baths have the most effective effect on the vascular system; however, medicinal herbs such as oregano, calamus, chamomile, string, and nettle are also often used. The use of baths must be agreed upon with a doctor, since in case of certain cardiovascular diseases, steaming the legs is strictly prohibited. It is worth remembering that traditional medicine can only be effective in combination with drug therapy, or as a preventive measure for problems with blood circulation in the extremities for people at risk.
Massage, acupuncture
Therapeutic foot massage and acupuncture procedures are characterized by effective effects on circulatory disorders of various locations. To improve blood circulation in the extremities, a light massage helps well, gradually turning, after relaxing the muscles, into rolling and rubbing the problem segments of the leg, with periodic, moderate pressure, which will help strengthen the vascular lines. Massage problem areas for no more than fifteen minutes so that the procedure does not have the opposite effect. If you have no experience in performing massages, you can initially use the services of specialists, which will allow you to visually and tactilely feel how to correctly perform the procedure at home. As for acupuncture, at the present time it has gained particular popularity due to the active stimulation of the activity of blood vessels and nerve endings.
Acupuncture is a procedure that can only be performed by a specialist, and only after a comprehensive examination of the patient.
Therapeutic exercise and physical activity
Despite the rapid development of medicine in all directions, alternatives to human physical activity as a method of combating and preventing many diseases have not been invented. Physical activity of a person, exercises, and feasible exercises are integral areas of treatment and prevention of cardiovascular problems. The question of how to restore blood circulation in the legs is answered by a manual on physical therapy, which regulates the effectiveness of the following exercises for normalizing blood supply to the extremities:
- Take a lying position on your back. Perform leg movements based on the principle of simulating cycling.
- From a similar starting position, perform synchronous movements with your legs, according to the principle of crossing them, imitating “scissors”. To begin with, you can carry out movements by raising your legs at a right angle relative to the floor, gradually complicating the task by reducing the angle to a minimum.
- Lying on your back, raise your arms and legs up, vibrating them. Exercise helps to relax the limbs, helps clean vascular lines from deposits, and is an excellent prevention of thrombosis.
- Standing position: you need to perform raises on your toes, with parallel muscle tension. You must repeat at least 10 lifts at a time.
- From a standing position, keeping your feet shoulder-width apart, bend forward, trying to reach the floor with your fingertips. When bending, it is important that your legs do not bend at the knees.
- Starting position: sitting on the floor with your legs spread apart as far as stretching allows. Place your arms at chest level and bend forward, trying to reach the floor. Repeat the exercise 5 times, then take a break by repeating the bends.
The total charging time should not exceed half an hour to avoid overloading the body. In addition to specific exercises, jogging, swimming, fitness, dancing or other sports will be beneficial for health, and for people who cannot afford intense exercise, they can be replaced with easy, but regular and long walks.
Symptoms of circulatory disorders of the lower extremities
In rare cases, the disorder may be asymptomatic, but the most common symptom is intermittent claudication, i.e. discomfort and/or pain in the lower extremities that occurs when walking and disappears at rest. Sometimes there are cramps, heaviness or weakness in the legs.
The degree of circulatory impairment in the lower extremities is determined by the distance that a person can overcome. As the disease progresses, the symptoms become more pronounced - the pain intensifies (and it is localized from the thigh to the fingertips even in the absence of movement), disturbances in the trophism of the skin occur (they become dry, pale), and in more severe cases, trophic ulcers appear, the necrosis of soft tissues, gangrene occurs.
Pathological root causes of the development of the disease
Painful sensations in the legs are not only the fate of older people; problems in this category are increasingly observed in young people, and even in children. Many people often associate pain in the lower extremities with increased stress or simple fatigue, however, often the source of the problem has a more complex and dangerous etiology. Conventionally, the primary sources of the disease can be divided into three basic categories:
- Pathologies of peripheral segments of arteries.
- Stenosis of vascular branches in the lower extremities against the background of atherosclerotic formations in the blood vessels.
- Inflammation of the vascular membranes or spasms of the arterial tracts.
The causes of such pathological processes are often serious diseases, the most common of which are:
- Atherosclerosis of the obliterating type. The disease is characterized by the accumulation of harmful fats and cholesterol in the vessels of the legs, which provokes their fragmented or complete blockage with sclerotic formations. The disease most often manifests itself in mature people who lead an unhealthy lifestyle, regardless of gender.
- Autoimmune vascular disease, chronic, called thromboangiitis. Pathology is a common cause of deterioration in blood supply to the extremities as a result of spasm of one or more vessels of the hip region. Most often it is diagnosed in representatives of the stronger sex who abuse addictions, however, recently it is often diagnosed in women over thirty years of age.
- Diabetic vascular disease. It develops against the background of existing diabetes mellitus, dangerously rapidly progressing necrosis of the vascular membranes and tissues of the legs, which results in gangrene with the need for amputation of the limb.
- Thrombophlebitis, as a serious pathology of the veins, contributes to disruptions in the blood supply to the extremities and the outflow of fluid, which is accompanied by a decrease in the tone of the vascular walls.
Sometimes the cause of deterioration in blood flow is problems with the spine, as well as serious impairments in the functionality of the kidneys and heart.
The problem of deteriorating blood circulation in the lower extremities is one of the ailments that can be prevented by following simple principles of healthy living:
- Through physical activity and correct eating style, maintain weight criteria within normal limits.
- Give up bad habits, try to avoid psycho-emotional stress.
- Give preference to loose-fitting clothing and comfortable shoes.
- For people who work in an office and regularly sit or stand, it is important to learn to alternate activities by systematically changing positions.
- Contrast showers and foot baths, used regularly, will help stimulate the activity of the circulatory system.,
Ointment to improve blood circulation in the legs. Medicines
The treatment regimen largely depends on the severity of vascular damage, the duration of the disease and the stage at which it is at the time of treatment, as well as the presence of concomitant pathologies. What medications are used to treat the lower extremities when normal blood circulation in them is disrupted?
List of drugs:
- Antiplatelet drugs for the prevention of vascular blockage and their treatment, such as Aspirin, Reopoliglyukin.
- Vascular drugs with dilating action, for example, Vazonit, Vazaprostan, Trenal and others.
- Medicines that increase physical endurance - Pentoxifylline and Cilostazol, which improve blood circulation and make walking easier for the patient.
- Drugs that reduce the content of “bad” cholesterol in the blood.
- Anticoagulants that thin the blood, such as Warfarin, Heparin.
- Antispasmodics, for example, Drotaverine. Neutralize vascular spasm, reduce pain.
- Drugs that increase blood circulation in tissues, this can be Zincteral and others.
- Diabetics are prescribed fibrates to reduce the amount of triglycerides, such drugs as Bezafibrate, Clofibrate.
- To regulate cholesterol levels, statins are prescribed: Lovastatin, etc.
- An ointment made on the basis of antibacterial agents (Levomekol, Dimexide) treats trophic ulcers on the legs.
- Vitamin complexes.
- A nicotinic acid.
- Physical procedures, for example, electrophoresis and others as prescribed by the doctor.
Reasons for the development of the disorder
There are quite a lot of factors that are responsible for the development of pathology; at present, circulatory disorders in the arteries are usually divided into three main groups:
- peripheral parts are affected , that is, arteries and their further narrowing due to the formation of atherosclerotic plaques;
- artery walls become inflamed;
- arterial spasm is observed .
Such disturbances in the blood flow are often observed due to the following developing diseases:
- Obliterating atherosclerosis , which is caused by the accumulation of fat-like substances and cholesterol in the vessels. Based on this, sclerotic plaques are formed, which over time can lead to either partial or complete blockage of the passage of blood vessels. This disease can affect representatives of any gender and age category.
- The cause of the development of pathology can be an autoimmune vascular disease in a chronic form ( thromboangiitis ). At the same time, due to spasmodic vessels in the thigh area, blood cannot flow to the lower extremities in sufficient volume. Bad habits contribute to the development of this disease. The disease is often observed in young men, males.
- The most terrible complication is diabetic foot , which is the result of vascular damage from diabetes mellitus. If blood does not flow to the legs in the required volume, gangrene may begin to develop. In this case, the affected limbs are amputated.
- Violation of the venous circulation of the lower extremities causes thrombophlebitis and varicose veins . In this case, the blood outflow system is disrupted, and as a result, the walls of the blood vessels weaken.
Diagnostics
When making a diagnosis, the following factors are taken into account:
- Cause of the disease (varicose veins, atherosclerosis, thrombophlebitis, etc.);
- Depth of lesion;
- Type of violation (complete or partial blockage of the vessel);
- The degree of artery damage.
Depending on the prevailing symptoms, arterial insufficiency is usually divided into four stages:
- Stage I (full compensation): numbness, fatigue, tingling and chilliness of the feet that occur after physical activity;
- Stage II (insufficiency during functional loads): stage I symptoms, to which intermittent claudication is added;
- Stage III (failure at rest): continuous pain even at night;
- Stage IV (ulcerative-necrotic changes): ischemic pain is added (due to which a person constantly requires painkillers), the first signs of gangrene appear.
To clarify the diagnosis, the following are prescribed: ultrasound Dopplerography of blood vessels, angiography, capillaroscopy, thermometry, magnetic resonance angiography or MRI.
Diagnostics of blood supply to the brain
At the first signs of abnormal brain function, you should contact a specialized clinic for diagnosis and treatment. Healthy people who do not exhibit any symptoms indicating the disease also need to be examined once a year. This must be done in order to detect a problem in time, if there is one.
Diagnosis is carried out in various ways. The first is an MRI of the brain. This type of examination allows you to see the condition of the tissues and find out how affected parts of the brain are. This method is one of the most effective, because it allows you to see even nerve trunks and membranes. Neurosonography is prescribed for newborn children. Diagnosis is carried out through a fontanel that has not yet become overgrown.
There are many more types of examinations that a doctor may prescribe. He looks at the patient’s condition, his symptoms and, based on this, determines the type of diagnosis. After this, pills and other drugs are prescribed that can restore the blood supply to the brain.
To diagnose circulatory disorders in the legs, laboratory and instrumental studies are performed. Before making a diagnosis, the specialist determines whether the patient has any vascular diseases. For accurate diagnosis, the following laboratory research methods are used:
- general blood analysis;
- coagulograms;
- blood for sugar;
- lipid profiles.
Instrumental methods are also prescribed:
- angiography of the extremities;
- MRI;
- Doppler ultrasound.
Additional methods of prevention
If you notice symptoms of slow blood flow, you should consult a specialist who will tell you how to improve blood circulation in the body.
It is best to deal with the problem comprehensively. Proper nutrition and physical activity, massages, losing excess weight, quitting smoking and, if possible, minimizing stress are necessary.
If possible, unnecessary stress and overexertion should be avoided. If this fails, then you can resort to massage, which will perfectly relax the body as a whole and speed up blood flow. You can also do meditation or yoga to relieve stress.
A contrast shower promotes faster blood circulation and relaxation of the body. Quitting smoking and losing excess weight will reduce the strain on the cardiovascular system and also speed up blood circulation.
What are the symptoms of poor circulation?
Poor blood circulation is dangerous because it is often asymptomatic. At an early stage, poor circulation is almost invisible; it is often recognized when deterioration occurs. The following symptoms are common indicators of a weakened cardiovascular system.
Visible symptoms of poor circulation
You can literally see the following symptoms of poor circulation in yourself or your loved ones:
1. Ulcers on the legs. Ulcers and sore, inflamed skin (rashes that don't go away) on the legs are a symptom of poor circulation. People with poor circulation may notice dry red patches of varying sizes on their legs.
2. Edema. Poor blood circulation prevents the kidneys from functioning well, and as a result, swelling may be noticed. If your arms or legs begin to swell, fluid is accumulating in them due to slow blood flow. This happens because the circulatory system tries to reduce the load, resulting in fluid retention - edema.
3. Discolored skin. Without the right amount of oxygen pumped through the veins, a slight change in skin color occurs, also known as cyanosis. Your fingers and toes will look as if they've been bruised - bluer than usual.
4. Varicose veins. If the valves that work to pump blood are weakened, this causes blood to stagnate and pressure to rise in the veins. As a result, veins located close to the surface of the skin appear twisted and swollen. After standing for a long time, the veins in the legs may feel itchy. These veins most often appear near the legs and ankles.
5. Hair loss and weakened nails. This is another one of the most noticeable symptoms of poor circulation. When the body does not receive enough nutrients, this will certainly affect the growth of hair and nails. Hair may become dry and begin to thin and fall out in clumps. Your skin may become drier, itchy, and your nails may become weak and brittle.
Physical exercise
Many people work in sedentary jobs, which contribute to the development of blood circulation problems. Exercise can solve a difficult problem.
You need to get into the habit of doing exercises every day, lasting at least 30-45 minutes. You can engage in different types of activities on different days, alternating the load on different parts of the body. For example, you can devote one day to dancing, the second to swimming, and the third to jogging. If possible, you can visit the gym.
If your job is conducive to a sedentary lifestyle, then it is necessary to change your position at the workplace more often, and it is advisable to get up and walk around every half hour.
Risk group
Adverse symptoms, such as heaviness in the legs in the evening, after a long walk or after a normal working day, are not always a consequence of the presence of pathologies of complex etiology in the body. Poor circulation may be a consequence of less dangerous, but requiring attention, factors that medicine classifies as a risk group for the progression of problems with blood circulation in the peripheral parts of the body, including in the lower extremities:
- Lack of physical activity, prolonged static loads. The highest likelihood of blood flow deterioration is in people who work in office environments, regularly spending more than half the day in a sitting or standing position.
- Overweight. This factor is the primary source of many problems with the cardiovascular system, and not only. Against the background of obesity, the vessels of the lower extremities lose the ability to contract correctly under a thick layer of fat, against the background of excessive load on the extremities under significant weight.
- Genetic predisposition to developing diabetes.
- Abuse of bad habits, in particular alcohol and smoking, which negatively affect the condition and functionality of the vascular system.
- Hypertension or hypotension, the possibility of developing problems with blood pressure.
- High cholesterol criteria, disruption of lipid metabolic processes in the body.
Leg problems can also be a consequence of hormonal disorders, develop against the background of uncontrolled use of certain groups of drugs, and also worsen during critical changes in weather conditions, in weather-sensitive people.
Conclusion
Thus, there are many ways to help improve blood circulation in the lower extremities. Treatment will be successful if the person has the will, perseverance and desire to do so. To avoid such a pathological condition, preventive measures should be used.
The question of what to do if there is poor blood circulation in the legs is asked not only by phlebologists. They consult with friends, turn to the Internet. The main prescriptions should be made by a doctor, taking into account the causes of the disease and the clinical picture. By supplementing the course of treatment with folk remedies, you can speed up the restoration of blood circulation in the lower extremities and prevent changes in the rhythm of life. Just don’t forget - all additions must be agreed upon with your doctor.
Causes of poor circulation
The condition of the lower extremities is influenced by lifestyle. Addiction to bad habits - smoking, alcohol and drug addiction, as well as professional activities associated with low physical activity or the need to walk or stand all day - have a negative impact. But there are other factors that provoke poor circulation in the legs:
- excess weight caused by metabolic disorders or poor nutrition;
- pregnancy;
- hereditary factors;
- unfavorable emotional environment;
- bad ecology;
- age-related changes;
- regular use of certain medications, for example, hormonal drugs;
- diseases of various types that cause complications in the cardiovascular system.
Blood supply to the legs is also impaired in diabetes mellitus. Venous outflow worsens due to decreased vascular tone.
The reasons that first cause a disorder of microcirculation in small capillaries, and then blood circulation in large vessels, are divided into 3 groups:
- Inflammation of the walls of arteries and venules, causing spasm.
- Blockage of blood vessels due to atherosclerosis.
- Peripheral angiopathy as a complication of diabetes mellitus.
Prevention
To prevent disruption of the venous outflow of the lower extremities, you should adhere to a healthy lifestyle. Give up bad habits, stick to a rational diet, don’t overeat, but don’t starve, and don’t forget about physical activity. Acute infectious and chronic diseases should be treated in a timely manner, preventing the development of complications. To strengthen the immune system and the vascular system, use folk remedies and vitamin complexes during the epidemic season.
What to do when you discover the first symptoms of a blood supply disorder, everyone decides for themselves. But it is still better to seek help from official medicine. The sooner the disease begins to be treated, the faster it recedes.
Diabetes mellitus is often accompanied by leg diseases. Disorders associated with complete or partial blockage of the vessels of the lower extremities occur in 30-35% of patients. The older the patient is, the more likely they are to appear.
Ways to combat circulatory disorders
If you do not take any measures to combat circulatory disorders, then after a certain period of time the result will be disfigured legs with blue nodules and intertwined with swollen veins. There is also a high probability of damage to the deep internal veins. Unfortunately, pathological changes affecting peripheral vessels are chronic and do not go away without treatment.
Doctors involved in the treatment of blood vessels have at their disposal various means that improve blood circulation in the legs. With the help of medications and physiotherapeutic procedures, the pathological condition of the veins and arteries of the lower extremities is reduced or eliminated. If these methods turn out to be ineffective, then they resort to such a radical method as surgery with removal, cauterization or sclerosis of the affected area of the vessel. But such surgical intervention is quite painful, and in the end the cause of vein deformation is not completely eliminated.
To make a diagnosis, the following are carried out: visual examination, ultrasound (Dopplerography) of the lower extremities, capillaroscopy and angiography - contrast study of blood ducts, large and small, determination of the temperature of the affected area - thermometry. The patient is often referred for an MRI with contrast.
It is recommended to give up bad habits - smoking (or reduce the number of cigarettes smoked per day), alcohol, and recover from drug addiction. The following methods help improve blood circulation in the legs: restoring the balance between work and rest, physical therapy, treatment with pharmaceutical and folk remedies.
In the initial stages of the disease, ointments and gels—topical medications—are used to improve blood circulation in the extremities. They do not restore poor blood flow, but they help cope with unpleasant sensations - heaviness and “goosebumps” in the feet and calves. Ointments are divided into blood thinners, those that relieve inflammation of blood vessels and phlebotonics - they improve blood circulation by increasing the tone of the check valves of the veins.
The most popular and affordable drugs from each group:
- Heparin. Reduces blood clotting, eliminates swelling and pain.
- Indomethacin. The main properties are anti-inflammatory and analgesic, additional, like those of the 1st group.
- Troxevasin - thrombolytic effect, strengthens blood vessels.
The cheapest remedy for improving blood circulation in the extremities, which is preferred by older people, is Vishnevsky ointment. Liniment helps restore blood supply, stop inflammatory processes, and stop blood clots. The downside of the product is the unpleasant smell.
Antispasmodics are not drugs that improve blood circulation in the lower extremities, but they restore muscle contractility and restore blood supply, relieving pain. Nitric oxide, the active component of Nitroglycerin and Isosorbide dinitrate, instantly eliminates spasms. Injections with Magnesium Sulfate quickly relax. But you can use other antispasmodics on the recommendation of a doctor.
Vascular drugs for improving blood circulation in the legs include drugs from the PNS group. But they do not act selectively, not only on problem areas, but have an effect on all blood vessels of the body. The most commonly used:
- Alpha adrenergic blockers - Nicergoline, dilates arteries and increases the tone of veins, and Phentolamine, relaxes muscles, dilates blood vessels, has an anti-inflammatory effect.
- Calcium antagonists that normalize internal pressure in blood vessels and reduce the risk of thrombosis - Amlodipine, Nifedipine.
- Vasodilators, vasodilators, for example, Proxodol. This group also includes calcium antagonists.
- RAS inhibitors - Enalapril, Ramipril.
To increase the speed of blood flow, drugs are prescribed to restore peripheral circulation:
- Halidor is an antispasmodic with myotropic action;
- Vintoceptin - additional antioxidant properties;
- Wafarin is a blood thinner.
The range of medications for varicose veins is wide, so you should not treat the disease yourself - you should entrust the choice to a doctor. Not all tablets, ointments and injections are compatible with each other.
Before using pharmaceuticals, even if prescribed by a doctor, you need to read the instructions. Side effects can occur both with oral medications and with ointments and gels.
A complex of physical therapy (physical therapy), which helps to strengthen the weak blood flow of the lower extremities with varicose veins, is agreed upon with a specialist methodologist. In the initial stage of the disease, you can independently choose ways to improve blood circulation in the legs. Classes can be supplemented with exercises:
- Lying with your legs bent, breathe deeply, drawing in your stomach.
- Slowly roll from heel to toe, and then rise.
- Raise your legs while lying down, holding a pillow between them.
- Lying on your back, pull your feet towards you with sliding movements, bending your knees. At this time, the pelvis is raised.
One of the exercise therapy complexes, which is performed at the initial stage of varicose veins:
- starting position - lying on your back;
- the legs are lifted in turn, then bent, pressed to the chest, lowered;
- raise the lower limbs and rotate the feet;
- straighten and bend your toes.
Roll over onto your back and raise your straight legs as high as possible. They get to their feet and roll from heel to toe. Finish the session by walking with a high hip lift. Repeat exercises - 8-14 times, it is advisable to perform the complex in the morning and evening.
Emergency operations to restore blood flow to the legs are required only in case of acute thrombophlebitis - inflammation of the lumen of the great saphenous vein, which increases the risk of thrombosis. Planned operations are performed to eliminate trophic disorders in the vessels of the lower extremities, remove deformed vessels and prevent recurrence of varicose veins. In acute conditions, surgery is performed in an open manner.
The rest use methods: laser ablation, endoscopic vein dissection and the most common method - phlebectomy. The choice of surgical intervention is at the discretion of the doctor. The duration of rehabilitation is determined by the type of operation, stage of the disease, age and condition of the patient.
ethnoscience
Home remedies help slow down the development of the disease and keep it in remission for a long time. To improve blood flow in the legs using folk remedies, the following recipes are used:
- Ginger tea to stimulate blood flow. Brew 0.5 tsp. grated root with a glass of water, leave for 15 minutes, sweeten with honey. Drink a glass a day.
- Ginseng. Alcohol tincture is taken 20 drops 3 times a day, dissolved in 100 ml of water. Strengthens capillaries.
- Foot bath with horse chestnut. 150 g of dried flowers are steamed in a water bath, pour 5 liters of boiling water, and infuse. The duration of the procedure is 15-20 minutes, preferably done 40-60 minutes before bedtime.
- Cold and hot shower. The limbs are rinsed alternately with hot and ice water. It is recommended to carry out the procedure before increased loads.
- Foot baths with pine needles. Pine or spruce needles, 5 cups, add water and bring to a boil. Remove from heat and let stand for 15 minutes. Then dilute the concentrated decoction with 5 liters of water.
- Garlic compress. Grind the head without the husk, mix with butter - 1:2, apply in the form of a compress overnight.
There are many home treatment methods: rubbing walnut oil, horse chestnut powder ointment, nettle tea, calendula baths and others.
Folk remedies may not be combined with pharmaceuticals. If the therapeutic course is supplemented, the attending physician must be notified.