General information
Balantidium (from the Greek “bag”) was first described by the Swedish scientist Malmsten in 1857. This ciliate (the largest among human parasitic protozoa) was discovered by Malmsten while studying the feces of patients suffering from diarrhea. Malmsten described in detail the complaints of patients and the clinical picture of the disease.
In the 80s of the 19th century, balantidia were discovered in the intestines of pigs (further studies showed that the level of infection of pigs with balantidia reaches 80%).
The ability of balantidia to cause disease in humans was proven in 1901 by N.S. Soloviev. He also established that this type of ciliate belongs to interstitial parasites, and identified the disease as a separate nosological unit.
Balantidiasis is detected quite rarely in the form of sporadic cases, but the infection rate in rural areas can be 4-5% of the total population. In most cases, the disease is detected in persons who come into contact with pigs, the natural carriers of this type of ciliate. In foci of infection, the spread of the disease in some cases occurs through contact with patients with balantidiasis.
Forms
Depending on the clinical picture, balantidiasis is divided into:
- An acute form, reminiscent of enterocolitis or colitis in symptoms.
- The chronic form, in which intoxication is mild, and exacerbation is replaced by remission without any symptoms. It occurs more often than the acute form.
Also highlighted:
- latent balantidiasis, in which the pathogen exists in the intestines for a long time without showing pathogenic properties (carriage);
- forms of balantidiasis combined with other intestinal diseases (amoebiasis, shigellosis, etc. may be observed).
According to the severity, the disease can occur in mild, moderate and severe form.
The most common are moderate and severe forms.
Balantidiasis
Balantidiasis (synonym for ciliate dysentery) is a protozoal disease characterized by ulcerative lesions of the large intestine with disruption of its function.
The causative agent is Balantidium coli from the class of ciliates (Fig.).
The main source of infection is pigs. Infection with balantidiasis occurs through consumption of food and water infected with balantidia cysts, as well as through dirty hands and various household items. More often people who work in pig farms, slaughterhouses and sausage production get sick. Sporadic cases of balantidiasis are found everywhere.
When the pathogen penetrates the walls of the colon, crater-shaped ulcers are formed.
Clinical picture (symptoms and signs). In most cases, the disease occurs with minor periodic disorders of intestinal activity. Sometimes these phenomena increase and give a picture of chronic relapsing colitis. Severe forms of acute balantidiasis in their clinical course resemble bacterial dysentery: frequent liquid mucopurulent, then bloody stools, tenesmus, pain along the colon, loss of appetite, nausea, general weakness, cachexia. The temperature is often within normal limits.
Complications: peritonitis, intestinal bleeding.
The diagnosis of balantidiasis is made on the basis of the clinical picture and sigmoidoscopy data (see). Absolute proof of balantidiasis is the detection of pathogens in freshly excreted feces.
The prognosis in mild cases is favorable; in severe cases, death is possible.
Treatment is the same as for amoebiasis.
Prevention. Timely identification and treatment of patients with balantidiasis, strict adherence to the rules of personal hygiene. Carrying out measures to prevent environmental pollution from human and pig excrement. Pig farms require cleaning of pigsties and composting of excrement.
Balantidia: 1 - vegetative form; 2 - cyst
Balantidiasis (balantidiasis; synonymous with ciliate dysentery) is an ulcerative lesion of the large intestine with disruption of its function as a result of penetration and reproduction of the parasitic ciliate Balantidium coli in the intestinal tissues.
The body shape of the ciliate (Fig. 1, a) is irregular oval; length 50-80 microns, sometimes more; width 35 - 60 microns. The movement is carried out by cilia (4-6 microns), covering the entire body. At the anterior end there is a mouth opening - a cytostome. In the cytoplasm there are many vacuoles containing food inclusions: red blood cells, leukocytes, starch grains, fungi, bacteria, etc. In the middle part of the body there is a bean-shaped nucleus - macronucleus; a small nucleus, the micronucleus, is adjacent to its middle part. In the intestines and tissues of humans, Balantidium coli reproduces by transverse fission; sometimes conjugation is observed. Cyst formation occurs in the intestines. Cysts (Fig. 1, b) are round, dia. 50-70 microns. Balantidium coli is well cultivated on media proposed for the cultivation of dysenteric amoeba.
Rice. 1. Balantidium coli: a - vegetative form with swallowed red blood cells; b - cyst; 1 - cytostome; 2 - vacuoles filled with food inclusions; 3 - macronucleus; 4 - micronucleus; 5 - contractile vacuole; 6 - cytopig; 7— cyst shell.
Epidemiology. The main source of infection is pigs. However, a person who secretes ciliates can infect others. Wild rats and dogs play a minor role. Under favorable conditions, cysts persist in feces for several weeks and can enter the human digestive tract along with contaminated food, water, vegetables, and also through contaminated hands. Flies can also transmit balantidia cysts.
Sporadic cases of balantidiasis have been reported in almost all countries. Epidemic outbreaks of balantidiasis are extremely rare.
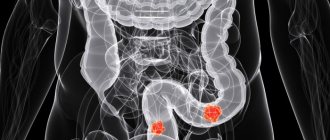
Pathological anatomy. When Balantidium coli penetrates the walls of the colon, ulcers are formed with uneven, sometimes undermined edges of different sizes and shapes, diameter. up to 3-4 cm. The cecum and ascending colon are most often affected (Fig. 2 and 3). Invaded ciliates destroy the intestinal mucosa, penetrate the submucosa and spread throughout it. Significant destruction of intestinal tissue sometimes leads to perforation.
The clinical picture of balantidiasis is varied and uncharacteristic. A large number of diseases occur with minor periodic intestinal disorders. In some cases, these phenomena increase and give a picture of chronic relapsing colitis, which occurs over a number of years and leads to cachexia.
Severe forms of acute balantidiasis resemble bacterial dysentery: liquid mucopurulent, then bloody stools up to 15-20 times a day, diffuse pain throughout the abdomen or along the large intestine, loss of appetite, nausea, tenesmus, general weakness. The temperature is often within normal limits, sometimes there is an irregular type of fever with chills. In rare cases, perforation of the colon may occur, leading to general peritonitis. With insufficient or improper treatment, after symptoms subside, relapses may occur, occurring as primary acute balantidiasis. Asymptomatic carriage of Balantidium coli is also observed.
The diagnosis in each case must be confirmed by findings of balantidia. It is necessary to take into account the temporary absence (up to 2 weeks) of parasites in the feces of patients with balantidiasis and their detection in carriers who have intestinal disorders of other etiologies.
Forecast. Mild and moderate forms of balantidiasis do not pose a danger if detected and treated in a timely manner. In severe cases, the prognosis is often unfavorable. Mortality 7-29%. Timely identification of patients and treatment reduce mortality to zero.
Treatment. Terramycin or biomycin 0.1-0.4 g 4 times a day for two five-day cycles with a break of 5 days; monomycin per os at 125,000-150,000 units according to the same regimen. Aminarsone is less effective (0.25 g 3 times a day for two five-day cycles). General strengthening therapy. Severe advanced cases of the disease are difficult to treat. Treatment of balantidine carriers is mandatory.
Prevention is the same as for other intestinal infections: measures to prevent contamination of the environment with feces of people and pigs. Pig farms require rational management of pigs, cleaning of pigsties, and composting of feces. Particular attention should be paid to the timely identification and treatment of carriers and patients with balantidiasis.
Reasons for development
The causative agent of balantidiasis is the ciliate Balantidium coli (phylum Protozoa, subphylum Ciliophora, class Ciliata). Balantidium is characterized by 2 stages of its life cycle - cystic and vegetative.
The vegetative stage is distinguished by the irregularly oval or ovoid shape of the body of the parasite, which reaches a length of 30 to 150 microns and a width of 30 to 100 microns. Numerous cilia allow the vegetative forms of balantidia to actively move (they can rotate around their axis).
At the narrowed end of the body of this ciliate there is a cellular mouth (cytostome) - a vertical slit perpendicular to the body, through which the parasite absorbs the remains of undigested food (especially starch grains), red blood cells, fungi and bacteria.
In the cytoplasm of the balantidium there are digestive and pulsating excretory vacuoles, a large nucleolus (micronucleus) and a nucleus (macronucleus), which in living ciliates can be visible even without staining as a bean-shaped light bubble (when stained according to Heidenhain, it becomes black). In the external environment, the vegetative form exists for 3 to 5 hours.
Round balantidium cysts are distinguished by a thick shell, and their size reaches 50 - 60 microns. In Lugol's solution, the cysts acquire a uniform brown-yellow color. In the external environment they are viable for 3-4 weeks.
Balantidia are low pathogenic for pigs in whose intestines they live (infection of pigs ranges from 21% to 100% depending on the region). Balantidia have also been identified in rats, mice, wild boars and monkeys, which, being carriers of parasites, release ciliate cysts into the environment along with feces.
Balantidium cysts that enter the human mouth along with contaminated food or water move to the large intestine, where they enter the vegetative stage and then multiply by division.
Since cysts are rarely formed in the human body and their number is insignificant, and it is almost impossible to become infected with the vegetative form, infection with balantidiasis through contact with a patient is extremely rare.
Causes of balantidiasis
The etiological agent of balantidiasis is the ciliated ciliate Balantidium coli. Balantidia are the largest representatives of intestinal protozoa that parasitize the human body. Their life cycle goes through 2 stages - cystic and vegetative. Balantidia cysts have a diameter of about 50 microns, a round shape and can remain viable outside the host body for 3-4 weeks. The length of the vegetative forms of parasites is 30-150 microns, width - 30-100 microns; the surface is covered with cilia, thanks to which movement is carried out. In the external environment, vegetative forms are less stable - they die after 3-5 hours.
Other Infectious diseases: Bacterial meningitis Bartonellosis
The main reservoir of balantidiasis pathogens are pigs, among which the invasion reaches 60-80%; Less commonly, humans are the source of protozoal infection. The mechanism of infection with balantidiasis is fecal-oral. Transmission of balantidia (usually cystic forms) occurs through dirty hands, contaminated water, fruits, and vegetables. More often, workers of pig farms, slaughterhouses, and meat shops fall ill with balantidiasis. In the human digestive tract, cysts form vegetative forms that parasitize the tissues of the cecum, sigmoid and rectum. At the site of their penetration into the mucous membrane of the colon, areas of hyperemia and edema are formed, which are subsequently transformed into erosions and ulcers. Defects of the mucous membrane have a crater-like shape, uneven edges, and a bottom covered with necrotic masses. Ulcerative-destructive changes in the intestine, the absorption of toxic substances, as well as the nutrition of parasites at the expense of their host form the basis of the pathogenesis of balantidiasis and determine its clinical manifestations.
Pathogenesis
The causative agent of balantidiasis enters the human body through the fecal-oral route - unwashed hands, fruits and vegetables, water contaminated with cysts leads to the parasite entering the digestive tract. After passing through the stomach and small intestine, the cysts begin their development (this period may be accompanied by symptoms characteristic of poisoning).
Vegetative forms formed in the upper part of the large intestine parasitize in most cases the tissues of the cecum, sigmoid and rectum.
During their life processes, balantidia secrete hyaluronidase, an enzyme that provokes the dissolution of the mucous membrane of the large intestine. In places where the mucous membrane is damaged, the parasite penetrates into the tissue, causing redness and swelling of the mucous membrane.
Balantidia penetrating into the submucosal layer activate the body's immune response, causing an accumulation of lymphocytes, histiocytic cells and segmented neutrophils in the lesion, which causes swelling.
Subsequently, erosions with uneven edges and crater-shaped ulcers form at the site of introduction of ciliates. Epithelial cells react to damage to the mucosa with increased proliferative growth (divide intensively), but the necrotic process also affects these cells.
Necrotic masses are gradually rejected, leaving a cavity communicating with the intestinal lumen.
The edges of the resulting ulcers are thickened and jagged, the uneven dark bottom is covered with a purulent-bloody coating. The area of ulcerative lesions can reach several centimeters.
Perforation of ulcers and the development of diffuse peritonitis are possible.
Although the localization of ulcers in most cases is in the bends of the intestine, cases of damage are known:
- appendix, as a result of which a purulent process developed and subsequent necrosis of the appendix;
- small intestine;
- liver tissue;
- heart muscle.
Balantidiasis is accompanied by symptoms of general poisoning, which arise as a result of the release of toxins during the life of balantidia.
Prevention
The intestinal parasite Balantidia is common on all continents, but the danger of becoming infected with it is especially great in countries with a hot, humid climate. Therefore, when going on a trip, you should remember about safety:
- drink only boiled or bottled water;
- do not swim in ponds and lakes with standing water.
Prevention of balantidiasis among farmers and people in contact with animals consists of identifying sources of infection (patients) and immediate treatment. It is important to remember to observe the rules of personal hygiene - thoroughly washing your hands after working with animals, processing fruits and vegetables before using them for food.
Symptoms
Both acute and chronic forms of balantidiasis can occur as follows:
- dysentery, in which foul-smelling, bloody-mucous diarrhea is observed;
- colitis, in which semi-liquid stool contains an admixture of mucus, but almost always no blood.
The incubation period is 5-30 days (in most cases about 2 weeks).
Acute balantidiasis is accompanied by:
- general intoxication (weakness, headache, loss of appetite);
- fever;
- abdominal pain (spasms and soreness of the large intestine are observed);
- diarrhea;
- flatulence;
- admixture of mucus and blood in the stool;
- enlarged liver.
There may be a false urge to defecate.
The performed sigmoidoscopy allows us to identify the presence of a focal infiltrative-ulcerative process.
In severe forms of acute balantidiasis, against the background of high temperature, the following is observed:
- defecation about 20 times a day;
- sudden weight loss;
- pronounced intoxication, which is manifested by chills, nausea, vomiting and headache.
Symptoms of peritoneal irritation may be present.
Sigmoidoscopy can detect extensive ulcerative lesions.
Chronic balantidiasis occurs at normal temperature and mild signs of intoxication. Defecation occurs 2-3 times a day, the stool is liquid. There is pain when palpated, mainly in the area of the cecum and ascending colon.
Sigmoidoscopy reveals typical ulcerative changes.
Balantidiasis, even in its acute form, can occur without an increase in body temperature, and complications are quite rare.
Symptoms of the disease
Sometimes a disease such as balantidia can last asymptomatically. The person does not know about his illness, while in fact he is a carrier of cysts. Problems in the body's functioning caused by protozoa can be reminiscent of other diseases. The most common signs are:
- Diarrhea, stool may be yellowish-green in color and contain blood and mucus;
- Problems with the central nervous system – disturbances of taste and smell, severe headaches;
- Vomiting or nausea, heartburn;
- Frequent abdominal pain;
- Increase in temperature for no apparent reason;
- Weakness, problems with appetite;
- In the most severe cases - convulsions and even coma.
In balantidiasis, the symptoms can be explained by the fact that the parasites begin to have a strong negative impact on the body's functions. The intestinal mucosa is damaged, which leads to the appearance of quite deep ulcers. The waste products of balantidia are characterized by a strong carcinogenic effect, which gradually poisons the body, and the carrier of the parasites is deprived of a considerable dose of nutrients supplied to it.
When carrying out studies, both food particles and some blood components, such as erythrocytes and leukocytes, were often found in the cytoplasm of balantidia.
The products obtained as a result of the metabolism of balantidium coli can penetrate into the liver or portal vein, due to which the accumulation of adipose tissue begins, and granular formations occur in the cell cytoplasm. With such changes, there is a disturbance in carbohydrate metabolism, problems with protein synthesis, and minerals are no longer processed properly.
The disease often occurs in a more complex form - then the ulcers begin to perforate, peritonitis, liver abscess, pneumonia can begin, and other inflammatory diseases are not excluded. Both adults and children can suffer from the disease.
In a child, the course of the disease most often occurs in an acute form, while transitions to a state of chronic relapse are constantly observed . But this is quite rare - the course of the disease mainly depends on the immune system and the general condition of the body.
The course of the disease is divided into different forms:
- Subclinical, which is characterized by a course without any special symptoms, but vitamin deficiency and ulcerative lesions are noted.
- An acute form, its severity can vary, and severe intoxication with very noticeable symptoms is not uncommon. Such an illness can last about a couple of months without weakening its course.
- Chronic form in a recurrent form - exacerbations occur after approximately 3 or 4 months and can last from a week to a month. The course of the disease can be described as mild. If left untreated, the disease can gradually last for several years.
- Continuous course - with this form, one can observe the gradual development of signs of the disease with noticeable manifestations of toxic effects and problems with the functioning of the excretory system.
Balantidium is a disease in which the course may depend on the general condition of the body before infection. For example, if a person with reduced immunity is infected, against the background of balantidiasis he often develops anemia, weight quickly decreases, intoxication progresses, and water-salt metabolism is disrupted.
It is worth noting that the life cycle of balantidia also has certain features among similar ones. Despite the fact that in their structure, the forms in which the parasite exists, and the methods of infection, balantidia are similar to other parasites, they are not able to disperse throughout the body along with the bloodstream. Their activity occurs exclusively in the intestines.
The disease can be determined based on a comprehensive study of symptoms, the results of tests performed in the laboratory, as well as the patient’s condition. With this disease, a clinical blood test shows an increased level of eosinophils, which reaches a level that allows us to make unambiguous assumptions about the patient’s condition.
If a child is sick, problems such as an enlarged spleen and liver may be noted; at elevated temperatures, arrhythmia and tachycardia may also begin, and blood pressure rises (but not to a critical level).
Diagnostics
The diagnosis is made based on:
- epidemiological data, which include occupational factors (workers of pig-breeding enterprises, etc.);
- analysis of patient complaints (putrefactive diarrhea, specific abdominal pain);
- intestinal endoscopy, which allows to identify erosions and ulcers;
- data from laboratory tests that make it possible to detect vegetative forms of balantidia in the patient’s feces;
- cultural research data.
Laboratory diagnosis of balantidiasis may include blood tests that reveal mild anemia, eosinophilia, a moderate increase in ESR, and decreased amounts of protein and albumin.
To diagnose balantidiasis, the following is examined:
- changes in the intestinal wall using sigmoidoscopy or colonoscopy;
- freshly excreted (no later than 20 minutes after defecation) feces;
- scrapings from affected areas of the intestine.
Laboratory diagnostic methods for balantidiasis include:
- Study of a native smear (unpainted material that has retained its natural color and structure). Allows, using a low magnification microscope, to detect fairly quickly moving vegetative forms of balantidia. For a detailed examination of ciliates, excess liquid is sucked out of the preparation and the smear is examined at high magnification.
- Examination of smears in Heidenhain-stained preparations. The main features of balantidia, clearly visible at low microscope magnification, include the characteristic oval shape of ciliates and the presence of a dark-colored bean-shaped macronucleus (vegetative nucleus) inside the cytoplasm.
- Cultivation of balantidia in Rice medium.
Since balantidia are isolated in periods, if the result is negative, the study is repeated several times.
Balantidia are more often detected in smears prepared from scrapings taken during sigmoidoscopy of affected areas of the intestine than during examination of stool.
During carriage, only single cysts of the parasite are detected.
Treatment
Balantidiasis is successfully treated with antibiotics in relatively low doses.
For treatment it is recommended:
- Monomycin, which is prescribed 4 times a day in the form of injections of 250 units. It is necessary to conduct two courses with an interval of a week.
- Oxytetracycline, used 4 times a day for a week in the form of tablets of 0.25 g (effective for mild forms of the disease).
- Metronidazole (Trichopol), which is used 3 times a day, 0.5 g.
Additionally prescribed:
- detoxification drugs;
- antiamoebic drugs (yatren), which are effective for ulcerative colitis;
- immunomodulators.
In hospital settings, for severe forms of the disease, hemotherapy is used.
In case of complications (peritonitis, perforation of an ulcer, intestinal bleeding, clinical development of acute appendicitis), surgical intervention is indicated.
After the course of treatment, a control analysis is carried out.
Treatment of balantidiasis
If the diagnosis of balantidiasis is confirmed, the patient is hospitalized in the infectious diseases department. Treatment is carried out using Ampicillin, Quiniophone, Oxytetracycline, Monomycin and other antibiotics that eliminate the etiology of the disease. Among antiprotozoal drugs, the doctor may prescribe Tinidazole and Metronidazole. The treatment course lasts 5 days. There may be 2-3 such courses.
As an addition to systemic drug treatment, the following are used:
- special diet with vitamin therapy;
- detoxification measures;
- hemotherapy;
- enemas based on norsulfazole.
In case of development of intestinal complications and acute appendicitis, emergency surgical intervention is indicated. Carriers of balantidia should also undergo appropriate treatment. If the intestinal wall does not contain ulcers, and stool examination for the presence of balantidia gives a negative result, there is no colitic syndrome, we can talk about curing balantidiasis and discharge the patient from the infectious diseases department of the hospital.