Hypertension is a common disease in modern society. It develops terrible illnesses, such as stroke and heart attack, and mercilessly claims the lives of millions of people. Previously, it was believed that the pathology affects older people, but recently the trend has changed dramatically; high blood pressure is found in the younger population. Unfortunately, hypertension cannot be fully treated, and it is completely impossible to get rid of it. However, this is not a reason to completely refuse medical care. Timely treatment can relieve severe symptoms and slow down the development of other diseases.
Content
- 1 Epidemiology
- 2 Etiology 2.1 Genetic predisposition
- 2.2 Other factors
- 4.1 Risk stratification 4.1.1 Risk factors 4.1.1.1 Basic
- 7.1 Lifestyle interventions
Causes
The essence of the development of hypertension is the absence of normal reactions (vasodilatation) after eliminating stressful situations. Such conditions are typical for the following persons:
- Abuse of salty foods - salt consumption in excess of the norm (15 g per day) leads to fluid retention, increased stress on the heart, which can cause spasm of arterial vessels;
- Drinkers and smokers;
- Persons whose work involves constant night shifts, emergency situations, intense physical and intellectual activity, severe stressful situations, and frequent negative emotions;
- Patients with chronic kidney diseases, thyroid diseases, diabetes mellitus;
- People whose relatives had hypertension, suffered a stroke or myocardial infarction.
Hypertension can be caused by eating junk food and smoking.
Pressure surges are most common in older people, but problems with blood pressure in the presence of certain factors can also occur in young people.
35% of middle-aged men have hypertension, and in the older generation (over 60 years old), pressure surges are recorded in almost every second man. In women, due to hormonal characteristics, hypertension is observed less frequently than in the stronger sex, however, with the onset of menopause, the chances of developing arterial hypertension in both sexes are equal.
The occurrence of hypertension is promoted by low physical activity, excess weight, frequent overeating - all that is called an unhealthy lifestyle. By eliminating such factors, a person himself can prevent the development of hypertension without drug treatment. But if the disease is started, hypertension will develop into other stages, which are fraught with the onset of a hypertensive crisis and premature death.
Etiology
Genetic predisposition
Twin studies suggest that heredity plays a major role in the etiology of hypertension[3].
Approximately 50% [4], [5], [6] of patients have a hereditary predisposition to EG, caused by mutations in the genes of angiotensinogen, angiotensin II receptors, angiotensin-converting enzyme, renin, aldosterone synthetase, β-subunit of amiloride-sensitive sodium channels of the renal epithelium, etc.
Other factors
- Obesity increases the risk of hypertension fivefold. More than 85% of cases of hypertension occur in patients with a body mass index of more than 25[7].
- Smoking: reduces endothelium-dependent vasodilation, increases the activity of the sympathetic nervous system, and is a risk factor for the development of coronary heart disease.
- Excessive consumption of table salt: excess sodium increases the volume of circulating blood, causes swelling of the walls of arterioles, and increases the sensitivity of the vascular wall to vasoconstrictor factors.
- Insufficient intake of calcium and magnesium, trace elements and vitamins from water and food.
- Alcohol abuse.
- Low physical activity, physical inactivity.
- Psycho-emotional stressful situations[8].
- Replication of pathogenic microorganisms, especially increasing under various stress conditions, associated with isolated systolic hypertension and systolic-diastolic hypertension, replication of cytomegalovirus. This was observed in Russia, then in the mid-Atlantic states of the United States, Kazakh, and Chinese populations, although in US populations as a whole the data have not yet been sufficiently studied. This is due to the fact that increased expression of angiotensin II and renin in the blood and tissues, certainly observed as a result of exposure to cytomegalovirus, does not always lead to the development of arterial hypertension, since, for example, people of the African race on average have very high levels of angiotensin II and renin, they do have more severe hypertension, but in Cuba, Puerto Rico and especially Africa, the prevalence of hypertension is usually much lower than among US whites.[9][10][11]
- The occurrence of arterial hypertension depends on the person’s age. At a young age, mainly secondary hypertension - due to smoking, alcoholism, drugs, vertebrobasilar insufficiency, congenital anomalies of blood vessels, kidneys, adrenal glands, pituitary gland. In middle age - due to excess body weight, neuropsychic stress or past diseases with damage to the heart, blood vessels, and kidneys. And after the age of 40, this is almost always the result of sclerotic vascular lesions;
- Gestational hypertension is hypertension that some women develop during pregnancy. It usually resolves after delivery, but sometimes the disease can be prolonged, and women who have had hypertension in pregnancy, as well as preeclampsia and eclampsia, which are also accompanied by hypertension, are more likely to develop hypertension in subsequent years[12].
- Among Africans[13] living in industrial societies, essential hypertension is four times more common than among whites, develops more quickly and leads to greater mortality, and the prevalence, but not severity, of essential hypertension in them decreases with a decrease in overt or covert racism[5 ][14][15][16].
Treatment of severe hypertension with non-drug methods
If hypertension has become severe, then, as a rule, non-drug treatment of arterial hypertension alone is not enough to normalize blood pressure. But, nevertheless, they are also necessary, otherwise drug treatment will also not be fully effective.
Treatment of severe arterial hypertension is as follows:
- Limiting table salt.
- Complete abstinence from drinking alcohol.
- Moderate physical activity.
- Weight loss if the patient is overweight.
- Auto-training – relaxation, meditation.
Now it’s worth taking a closer look at each of the listed methods. In severe cases of hypertension, and in general, all hypertensive patients are advised to reduce their daily intake of table salt to 4-6 grams. As practice shows, the amount of table salt consumed directly affects the level of lower (diastolic) pressure.
If you limit your salt intake, you can achieve a reduction in systolic pressure by approximately 5.4 mmHg, and diastolic pressure by 6.5 mmHg. In this case, you need to monitor the amount of salt not only in its pure form, but also in all products that the patient consumes throughout the day.
As for alcohol, it is generally undesirable for any form of arterial hypertension, especially for severe ones. Any alcohol has an uncontrollable effect on blood vessels and blood pressure, so you should completely avoid it, even wine and beer.
Physical activity with very high blood pressure is contraindicated. But this does not mean that the patient must remain in bed, on the contrary. You need to move, but only without overexertion. Preference is given to aerobics, swimming, race walking or jogging.
Both the set of exercises and the feasible sport are selected individually. Such activities have a beneficial effect on the respiratory system and strengthen the cardiovascular system. In addition, during sports, the patient gets rid of extra pounds. And weight loss is a mandatory part of a comprehensive treatment program for arterial hypertension.
If a person with hypertension, who is additionally obese or simply overweight, loses at least one kilogram, systolic and diastolic pressure decrease by 1.6 and 1.3 mmHg, respectively.
It is known that in case of hypertension any stress and experiences are strictly contraindicated, even if they are associated with positive emotions. Therefore, autogenic training with a trainer or independently is recommended to all patients.
The main thing is that the patient remains calm and monitors his mental balance; this is very important with high blood pressure.
Classification
- Classification of hypertension in clinical recommendations 2020 ACC/AHA Hypertension Guidelines:
- Normal blood pressure: SBP less than 120 mmHg. Art.; DBP is less than 80 mm Hg. Art.
- High blood pressure: SBP 120-129 mm Hg. Art.; DBP is less than 80 mm Hg. Art.
- AH I degree: SBP 130-139 mm Hg. Art.; DBP 80-89 mm Hg. Art.
- AH II degree: SBP 140-159 mm Hg. Art.; DBP 90-99 mm Hg. Art.
- Stage III hypertension: SBP >160 mm Hg. Art.; DBP >100 mmHg Art.
- by risk factors:
- short
- average
- high
- very tall
- by HD stage: I, II, III
Risk stratification
| Category AD | ||||
| FR, POM or AKS | High normal | 1st degree hypertension | 2nd degree hypertension | 3rd degree hypertension |
| No | Minor risk | Low risk | Moderate risk | High risk |
| 1-2 FR | Low risk | Moderate risk | Moderate risk | Very high risk |
| 3 FR or POM | High risk | High risk | High risk | Very high risk |
| AKS or SD | Very high risk | Very high risk | Very high risk | Very high risk |
RF - risk factors contributing to the development of the disease
POM - target organ damage ACS - associated clinical conditions DM - diabetes mellitus
Slight risk: < 1% Low risk: 1-3% Moderate risk: 4-5% High risk: 6-9% Very high risk: 10% and >
Risk factors
Basic
- Old age: men over 55 and women over 65
- Smoking
- Dyslipidemia: total blood cholesterol TC > 6.5 mmol/l (250 mg/dl) or LDL cholesterol > 4.0 mmol/l (155 mg/dl) or HDL cholesterol < 1.0 mmol/l (40 mg/dl) ) for men and <1.2 mmol/L (48 mg/dL) for women.
- Genetic predisposition: family history of early cardiovascular disease
- Abdominal obesity: waist circumference >102 cm for men and >88 cm for women
- CRP >1 mg/dl
Additional
- Impaired glucose tolerance
- Low physical activity
- Increased fibrinogen
Target organ damage
- Left ventricular hypertrophy
- Proteinuria (>300 mg/day) and/or a slight increase in plasma creatinine concentration (1.2-2 mg/dL) or microalbuminuria
- Signs of atherosclerotic lesions of the carotid, iliac and femoral arteries, aorta
- Generalized or focal narrowing of the retinal arteries
Associated clinical conditions
- Ischemic stroke
- Hemorrhagic stroke
- Transient cerebrovascular accident
- Myocardial infarction
- Angina pectoris
- Coronary artery revascularization
- Congestive heart failure
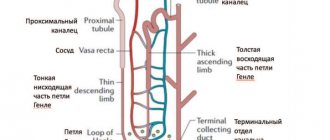
- Diabetic nephropathy
- Renal failure (plasma creatinine levels greater than 2 mg/dL)
- Dissecting aneurysm
- Severe hypertensive retinopathy
- Hemorrhages or exudates
- Papilledema
Hypertension: what is it?
To begin with, you should familiarize yourself with the general information. Today, hypertension is one of the most common cardiovascular diseases. What it is?
This disease is accompanied by a persistent increase in blood pressure in the vessels of the systemic circulation. Normally, young people have blood pressure levels of 120/70-75 mmHg. Art. Blood pressure increases as the body grows and ages. For example, for a forty-year-old patient these figures are approximately 130/80, and for patients over 50 years old - 135/85.
If a person's blood pressure exceeds 140/90 mm Hg. Art., then it is advisable to talk about hypertension (hypertension). Of course, we are talking about a persistent change in indicators, and not about a short-term increase in pressure due to, for example, stress or taking certain medications.
Clinical picture
Arterial hypertension is characterized by a long asymptomatic course. Typically, symptoms of the disease appear during hypertensive crises (headache, dizziness and other neurological disorders, chest pain, shortness of breath, feeling of fear). A more pronounced clinical picture is observed when lesions in target organs are identified:
- Heart damage: signs of coronary heart disease and progressive heart failure;
- Brain damage: progressive neurological disorders, hypertensive encephalopathy, visual impairment;
- Kidney damage: signs of renal failure;
- Peripheral vascular disease: intermittent claudication.
Stages
If you already have hypertension, it will not be possible to completely cure it - this is said by doctors and scientists who have been struggling for years to find a quick and simple treatment for hypertensive patients. The disease causes irreversible changes and complications that cannot be eliminated. But the sooner the patient seeks help, the greater the chance of stopping the development of the disease and minimizing the risk of complications.
Doctors consider systolic pressure above 139 and diastolic pressure above 89 mmHg to be elevated. Art.
The World Health Organization distinguishes several degrees of hypertension:
- 1st degree is also called borderline. It is observed in patients whose blood pressure ranges from 140/90 to 160/100. These indicators may not be recorded constantly, but may occur from time to time.
- Grade 2 – moderate hypertension. It is characterized by blood pressure indicators ranging from 160/100 to 180/110. In this case, the blood pressure is almost constantly elevated (increased levels are recorded several times a week or daily).
- Stage 3 , or severe hypertension. Her blood pressure is 180/110 mm Hg. Art. and higher.
If a patient is diagnosed with stage 3 hypertension, the risk of stroke, heart attack and other complications is many times higher.
Doctors also distinguish 3 stages of the development of arterial hypertension:
- Transistor. Increased pressure occurs from time to time, but no associated symptoms occur. A comprehensive examination of a person does not reveal any disturbances in the functioning of other organs. At this stage, hypertension can be cured if its cause is determined as accurately as possible. But the difficulty is that, without any complaints, a person does not control his blood pressure and does not seek an appointment until deterioration becomes noticeable.
- Stable. In this case, an increase in blood pressure is recorded regularly, and an examination of the heart reveals an increase in the size of the left ventricle. Retinal vasospasm often occurs. No other organic pathologies are found in such patients.
- Sclerotic. At this stage, significant deterioration in health is observed, associated with impaired cerebral circulation, disturbances in the functioning of the heart (signs of heart failure, coronary heart disease, myocardial infarction, etc.). This is the most dangerous stage, which is fraught with serious complications and can lead to death.
Diagnostics
Diagnosis of hypertension is based on blood pressure measurements. To establish a diagnosis of hypertension, it is necessary to take at least three independent measurements at different meetings with a health care worker using only a mercury tonometer according to the method of N. S. Korotkov, in which elevated blood pressure values are obtained. To diagnose secondary forms of hypertension, as well as to determine damage to internal organs, additional examinations are carried out: a general blood test, a general urinalysis, specific blood and urine tests, ultrasound of the heart and internal organs, an ECG, and various tests.
Holter blood pressure monitoring is a research method that involves putting an automated tonometer on the patient, recording blood pressure for 24 hours, at an interval specified by the program, usually from 30-60 minutes during the day to 60-120 minutes at night. As a result, several dozen results are obtained per day. Based on these data, one can judge the average pressure during the day, the average pressure during the night, and the average pressure during the day. In addition to the blood pressure numbers themselves, it is possible to obtain data that does not directly support the diagnosis of hypertension. For example, the presence or absence of hypertension can be judged by the speed and magnitude of the decrease in blood pressure at night or the speed of its rise in the morning.
Drug treatment
Drugs for the treatment of hypertension must be taken constantly - only in this case will they ensure stabilization of indicators and protect other organs from negative consequences. The treatment regimen with dosages is selected by the attending physician. It is not always possible to do this the first time: depending on individual characteristics, half a tablet may be enough for one patient, while another needs 2-3 times more.
The patient should not independently make changes to the treatment protocol after experiencing a positive effect. In this case, he runs the risk of worsening his condition and developing immunity to the prescribed drug.
The standard treatment for severe hypertension involves reducing levels by no more than 15%, even if the pressure is extremely high. A sharp drop can cause more harm to the body. Therefore, if there is a strong increase, doctors recommend not to self-medicate, but to call a doctor or an ambulance: they will choose the appropriate drug and lower blood pressure gently and gradually.
Treatment
The main goal of treating patients with hypertension is to minimize the risk of developing cardiovascular and other complications and death from them. To achieve this goal, it is necessary not only to reduce blood pressure to a normal level, but also to correct all risk factors: smoking, dyslipidemia, hyperglycemia, obesity, and treatment of concomitant diseases - diabetes mellitus and others. Treatment must be ongoing over many years. The disappearance of unpleasant sensations does not provide grounds to stop treatment.
Lifestyle interventions
- reducing alcohol consumption
- to give up smoking
- normalization of body weight
- increased physical activity
- normalization of sleep, work and rest patterns
- reducing the consumption of table salt, including salt from bakery and food products, to 5 g/day
- increasing the consumption of plant foods, reducing the consumption of animal fats, increasing the amount of potassium, calcium contained in dairy products, vegetables, fruits, grains in the diet, and calcium should be supplied along with vitamin D, and magnesium, which, like calcium, is contained in hard water, in mineral magnesium waters, which is the main component of green chlorophyll, green algae, etc.
Drug therapy
Currently, seven classes of antihypertensive drugs are recommended for the treatment of hypertension in Russia (see more details in Arterial hypertension#Treatment):
- diuretics (diuretics),
- α (only for concomitant diseases, where they are indicated) and β-blockers,
- calcium antagonists (in this case, additional dietary intake of magnesium can also be considered as taking a kind of calcium antagonist),
- ACE inhibitors,
- angiotensin II receptor antagonists,
- imidazoline receptor agonists.
The selection of a drug or combination of drugs should be carried out by a doctor.
How to treat hypertension?
The goal of treating hypertensive disease is to reduce mortality rates from cardiovascular disease. Long-term arterial hypertension leads to target organ damage. Even a slight increase in blood pressure increases the risk of developing diseases, because 60% of cardiovascular complications are observed in patients with a moderate increase in blood pressure.
Basic principles of treatment:
- when prescribing antihypertensive therapy, it is necessary to achieve the full target level of blood pressure, that is, normalization of blood pressure, reducing it to a level below 140/90 mm Hg, and in young people and in people with concomitant diabetes mellitus - to 130/80 mm Hg. Art. and below.
- treatment should be started as early as possible and carried out continuously; the concept of a course of antihypertensive therapy is unacceptable;
- The treatment regimen should be simple, preferably 1 tablet per day (this increases the number of patients actually being treated rather than avoiding treatment);
- preference should be given to long-acting antihypertensive drugs with a minimum-maximum ratio > 60%, since this prevents significant fluctuations in blood pressure during the day, and also reduces the number of prescribed tablets;
- all persons with high blood pressure are subject to simultaneous drug and non-drug treatment - lifestyle modification;
- in elderly patients with isolated systolic arterial hypertension, treatment is carried out in the same way as with systolic and diastolic arterial hypertension.
Drug treatment includes antihypertensive drugs. General classification):
- neurotropic drugs: stimulants (agonists) of central α2-adrenergic receptors - clonidine, estulic;
- stimulants (agonists) of central imidazoline receptors - physiotens (moxonidine);
- c-adrenergic blockers - prazosin (Advertusen, Pratsiol), doxazosin (Cardura), terazosin (Hitrin).
- cardio-selective β-blockers [metoprolol succinate (Betaloc-ZOK), azoprol retard, bisoprolol (Concor)];
First-line antihypertensive drugs are:
- diuretics;
- β-adrenergic receptor blockers;
- calcium antagonists;
- ACE inhibitors;
- angiotensin II antagonists.
Second line drugs:
- rauwolfia alkaloids;
- central α2-agonists (clonidine, guanabenz, guanfacine, methyldopa);
- direct-acting vasodilators (hydralazine, monoxidil).
see also
Arterial hypertension
| Diseases of the cardiovascular system (I00—I99) | |
| Arterial hypertension |
|
| Cardiac ischemia |
|
| Cerebrovascular diseases |
|
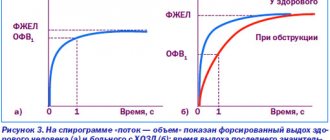
| Pulmonary pathology |
|
| Pericardium |
|
| Endocardium/Heart valves |
|
| Myocardium |
|
| Conduction system of the heart |
|
| Other heart diseases |
|
| Arteries, arterioles, capillaries |
|
| Veins, lymphatic vessels, lymph nodes |
|
Treatment of severe hypertension with non-drug methods
If hypertension has become severe, then, as a rule, non-drug treatment methods alone are not enough to normalize blood pressure. But, nevertheless, they are also necessary, otherwise drug treatment will also not be fully effective.
Treatment of severe arterial hypertension is as follows:
- Limiting table salt.
- Complete abstinence from drinking alcohol.
- Moderate physical activity.
- Weight loss if the patient is overweight.
- Auto-training – relaxation, meditation.
Now it’s worth taking a closer look at each of the listed methods. In severe cases of hypertension, and in general, all hypertensive patients are advised to reduce their daily intake of table salt to 4-6 grams. As practice shows, the amount of table salt consumed directly affects the level of lower (diastolic) pressure.
If you limit your salt intake, you can achieve a reduction in systolic pressure by approximately 5.4 mmHg, and diastolic pressure by 6.5 mmHg. In this case, you need to monitor the amount of salt not only in its pure form, but also in all products that the patient consumes throughout the day.
As for alcohol, it is generally undesirable for any form of arterial hypertension, especially for severe ones. Any alcohol has an uncontrollable effect on blood vessels and blood pressure, so you should completely avoid it, even wine and beer.
Physical activity with very high blood pressure is contraindicated. But this does not mean that the patient must remain in bed, on the contrary. You need to move, but only without overexertion. Preference is given to aerobics, swimming, race walking or jogging.
Both the set of exercises and the feasible sport are selected individually. Such activities have a beneficial effect on the respiratory system and strengthen the cardiovascular system. In addition, during sports, the patient gets rid of extra pounds. And weight loss is a mandatory part of a comprehensive treatment program for arterial hypertension.
If a person with hypertension, who is additionally obese or simply overweight, loses at least one kilogram, systolic and diastolic pressure decrease by 1.6 and 1.3 mmHg, respectively.
It is known that in case of hypertension any stress and experiences are strictly contraindicated, even if they are associated with positive emotions. Therefore, autogenic training with a trainer or independently is recommended to all patients.
The main thing is that the patient remains calm and monitors his mental balance; this is very important with high blood pressure.