Schmorl's hernia is considered a fairly common disease in which the lesion is localized on the spine, provokes various symptoms and can lead to the development of severe complications.
The disease affects patients of different ages, can occur in acute and chronic forms, and often significantly worsens the condition of patients. Various methods are used for treatment to not only eliminate the symptoms, but also prevent the progression of the pathology.
What is Schmorl's hernia?
Schmorl's hernia is a degenerative-dystrophic disease of the spinal column, in which protrusion of the cartilage tissue of the intervertebral disc occurs in the vertical plane. In this case, there is an increase in pressure on neighboring vertebrae and disruption of their structure with long-term persistence of symptoms without special treatment.
The difference between this type of hernia and the classic form is considered to be the nature of the protrusion. With a normal intervertebral hernia, it occurs in the horizontal plane, which leads to displacement of the vertebrae as a result of gradual destruction of the disc.
Experts note that Schmorl's hernia is a hereditary disease, but often develops in elderly patients.
Preventive measures
A central Schmorl hernia can destroy the intervertebral disc, which provokes the development of more serious pathologies. To prevent this from happening, it is better to follow these preventive measures:
- monitor your weight;
- try not to lift things that are too heavy;
- It is better to quit smoking, as it contributes to the deterioration of the elasticity of cartilage;
- Healthy food.
Schmorl's hernias, which everyone already knows, are not considered a fatal disease. But they can make life significantly more difficult. Therefore, you should definitely know how to treat Schmorl’s hernia correctly. Be healthy!
Places of occurrence of hernia
Schmorl's hernia on the spine can be localized in its various parts.
Symptoms and the risk of complications largely depend on the location of the lesion.
Lumbar
In the area of the lumbar spine, such a hernia occurs quite often. This is due to the increased load on this particular department, as well as the presence of other degenerative diseases in this area.
Pathology provokes various symptoms depending on the individual characteristics of the patient.
At the initial stages, it does not manifest itself in any way, but as the condition progresses, the following signs appear:
- Pain in the lumbar region, aggravated by heavy loads or when the patient remains in one position for a long time. People whose professional activities involve constant sitting or standing are more likely to suffer from severe forms of the pathological condition. This is due to the increased load on the lumbar spine.
- Discomfort or pain in the lower extremities. In this case, patients may note that the pain begins in the spine and gradually reaches the calf muscles.
- Numbness of the legs, goosebumps, changes in the condition of the skin. These symptoms appear only with prolonged progression of the condition.
- Fatigue and weakness of the leg muscles. If the patient exercises intensely, he may notice a decrease in endurance.
- Disorders of the pelvic organs occur in advanced stages, when not only the vertebrae are affected, but also the nerve endings responsible for the innervation of the organs.
Depending on the presence or absence of other complications, patients may experience associated manifestations.
Thoracic region
Localization of the hernia in the thoracic spine is most common. There is no exact data on the reasons that could explain this, but the lesion can form not only in old age. It is often found in adolescents. At the initial stages, the condition is not disturbed, which is due to the minimal size of the hernia.
As the condition progresses, the vertebra deteriorates and its pressure on the spinal cord increases. It is at this stage that neurological disorders develop, accompanied by severe pain during exercise and being in one position for a long period of time. Patients report numbness in their hands, muscle pain and fatigue.
Schmorl's hernia
Against the background of damage to the spinal cord in the area of the thoracic spinal column, disruption of the functioning of the organs of the chest and abdominal cavity is possible. Patients may develop various complications. The most pronounced disorder is pain, which is localized in the area of the hernia.
Cervical region
Localization of the lesion in the cervical spine is not so common. The condition is considered dangerous because it increases the risk of blocking the artery supplying the brain and causing the patient's death.
Patients with this type of hernia experience frequent headaches and dizziness. However, the symptoms are not eliminated with conventional analgesics. Patients report a decrease in mental performance, memory loss and concentration.
The condition gets worse in the absence of therapy. Patients may develop a stroke, as well as oxygen starvation of tissues as a result of a decrease in the volume of incoming blood.
Clinical picture
The symptoms of this disease are very scarce, because the nucleus pulposus of the intervertebral disc affects only the vertebral body, without affecting the spinal cord or spinal nerves. Most often, a Schmorl's hernia is detected on an x-ray. We can only talk about indirect symptoms:
- Feeling of stiffness in the back.
- Pain in the muscles that make up the frame of the spine.
- Limitation of spinal mobility.
Muscle pain and limited mobility occur due to excessive and prolonged tension of the dorsal muscles, which thus protect the damaged area of the spine from possible injuries and stress.
Types by location
A Schmorl hernia in the spine can affect different parts of the disc and vertebra. Depending on this, doctors distinguish several types.
| Type of hernia | Peculiarities |
| Central | It is localized in the central part of the intervertebral disc, progresses rather slowly, and exerts uniform pressure on neighboring discs. |
| Front | It is quite difficult to diagnose, since the lesion is localized in the anterior part of the intervertebral disc and is difficult to see on x-ray. |
| Lateral | One of the common types of hernia, which affects the side of the disc, resulting in uneven pressure on the vertebrae. |
| Rear | A common type of hernia, accompanied by degenerative-dystrophic disorders in the posterior part of the intervertebral disc. |
Depending on the location of the lesion, the symptoms of the disease and the rate of its progression differ.
Types of hernias
There are several main types of Schmorl's hernia, based on its location and size:
1 Multiple hernias .
This pathology is characterized by the penetration of cartilage into bone tissue in several areas of the spine. An x-ray shows how multiple Schmorl hernias form a certain pattern, while the cartilage takes on a diamond shape and encircles the affected disc on both sides. Hernias detected in childhood can sometimes heal on their own once the child reaches adulthood. A diagnosed multiple hernia, in most cases, indicates Scheuermann's pathology (a degenerative disease in adolescents that provokes the development of lumbar hypolordosis and thoracic kyphosis). As a result of the disease, the motor function of the spine is impaired.
In the early stages of the disease, symptoms may be completely absent. The first signs of a hernia are back pain, which may subside in a horizontal position, excessive fatigue and weakness. The patient experiences a gradual smoothing of the thoracic and lumbar curvature of the spine and stooping.
2 Small hernias . They are formed due to a congenital defect in the structure of the intervertebral discs; they may not change in size for several years.
3 Intracorporeal hernias. This type of hernia is characterized by destruction of the end plate; the hernial formation is located inside the vertebral body. The bone tissue around the hernia becomes denser, changes its structure, and an area of osteosclerosis forms.
4 Central hernias. Formed in the body of the joint between the vertebrae. A central hernia develops without visible symptoms and is diagnosed only during radiography. A hernia detected in time can be easily treated without surgery, with the help of therapeutic exercises and training on simulators. Without starting treatment in time, the disease can develop into an intervertebral hernia.
5 Anterior hernia. It is localized in the anterior part of the spine, often between the second and third lumbar vertebrae or in the cervical region. The main symptoms of a hernia are pain, which can intensify with any physical activity. The patient has a disturbance in the musculoskeletal system of the body, and local lordosis straightens.
6 Deep hernias. This type of hernia develops in people prone to osteoporosis or in those who suffer from a chronic form of the disease. Cartilage tissue penetrates deep into the body of the spine and dense cartilaginous plexuses develop there. A deep Schmorl's hernia requires immediate treatment; the patient must completely avoid any physical activity, including bed rest.
7 Posterior hernia. The pathology is formed in the posterior part of the spine due to the insertion of the detached posterior ligament of the vertebral body into the vertebra.
8 Cartilaginous hernia. The body of the hernial formation consists of cartilage. Some experts do not distinguish cartilaginous hernia as a separate type, citing the fact that it is a synonym for the general term “Schmorl’s hernia.”
9 Hernia of the end plates. They are formed in adolescence due to the specific structure of the vertebral plates or the rapid growth of the child.
The disease process itself is characterized by the penetration of cartilaginous plates into the spongy structure of the spine. 10 Single hernias. A hernia of this type is quite common; at a young age it tends to occur in the thoracic spine, and in older people - in the lumbosacral spine.
In the first stages of development of the pathology, the symptoms are invisible, the person can lead a normal lifestyle. When the disease begins to progress, cartilaginous nodes appear in other parts of the spine, impaired mobility and curvature of the column are observed. 11 Hernia of the caudal plate. With a Schmorl's hernia of the lower endplate, hyaline cartilage is pressed into the vertebral structure. Over time, due to physical activity, the nucleus pulposus of the intervertebral disc can also be depressed. A hernia of the caudal plate is dangerous because it constantly increases in size due to the fluid of the nucleus pulposus.
By method of defeat
Depending on the method of damage to the intervertebral disc, several types of pathological conditions are distinguished. Based on the number of foci, single and multiple hernias are distinguished. The former are not so common, are not accompanied by pronounced manifestations and can be asymptomatic for a long period of time.
Multiple hernias or nodules are quite common; they affect several vertebrae at once, which complicates the course of the pathology and leads to rapid progression with the development of severe complications.
Doctors distinguish several types of the disease:
- A small hernia is asymptomatic for a long time.
- Intracorporeal is localized in the central part of the intervertebral disc.
- The deep one affects the vertebrae quite severely, which leads to compression and the development of severe symptoms.
- An endplate herniation can disrupt the alignment of the vertebrae and impair brain function as it affects the thinnest areas of the vertebra.
- A caudal hernia also affects the thinnest areas of the vertebra, which are quickly destroyed, leading to a significant deterioration of the condition and the development of severe complications.
Depending on the location and method of damage to the vertebrae and discs, the symptoms differ somewhat.
Symptoms of the disease
Most often, small Schmorl hernias in the vertebral bodies do not manifest themselves in any way. However, the patient may experience increased fatigue in the lumbar region, decreased back flexibility, and a feeling of discomfort. Therefore, in most cases the disease is detected by chance during an X-ray examination of the spine associated with the diagnosis of other diseases.
Schmorl's nodes in the spine may be accompanied by local pain. Most often they occur during exercise and go away during a period of rest. When palpated, slight pain and even muscle spasm may also be observed in the area of the affected vertebra.
Clinical symptoms of the disease are absent or very scarce for the following reasons:
- the disease does not lead to the development of aseptic inflammation;
- does not cause muscle spasms;
We recommend that you familiarize yourself with the methods of removing intervertebral hernia on our website.
Muscle spasm in the lower back
- does not compress blood vessels and nerve roots.
Very rarely, Schmorl's hernia can cause pain in the lower extremities and lower back, occurring under the influence of physical activity. The progression of the pathological process can lead to complete collapse of the intervertebral disc into a herniation, which significantly impairs the function of the lumbar vertebrae.
Important! A hernia significantly weakens the spine, and a vertebral fracture may occur at its location.
A possible fracture can occur due to:
- strong blow;
- significant lateral load on the spine;
- compression of the spine along the axis.
Causes
Schmorl's hernia occurs not only as a result of the patient's hereditary predisposition to such a lesion on the spine.
There are other reasons, predisposing factors that can provoke a pathological condition:
- Poor nutrition with insufficient content in foods of components that are necessary for the health of cartilage tissue.
- Excess weight, which increases pressure on the intervertebral discs.
- Intensive growth in adolescence, when bone tissue develops somewhat more slowly, which leads to the formation of voids in the vertebral body. This cause is considered the most common when pathology occurs in patients under 18 years of age.
- Degenerative-dystrophic changes in cartilage tissue as a result of age-related physiological processes in the body of patients.
- Severe injuries of the spinal column, which may result in deformation of the discs and vertebrae.
- Severe and prolonged calcium deficiency in the patient’s body, which leads to increased porosity of bone tissue. The disease develops especially often in women during menopause, when, as a result of a decrease in estrogen levels, intense leaching of calcium from the bones is observed.
- Professional sports that involve heavy lifting and intense loads that increase pressure on the spinal column. Pathology can develop in patients who, due to their professional activities, lift heavy objects every day.
- Other diseases of cartilage and bone tissue, such as osteoarthritis. In this case, damage to the spine is observed, increasing the risk of developing severe complications.
Various predisposing factors can provoke the disease, the degree of its neglect and the rate of progression depend on this.
How dangerous is the disease?
Even multiple Schmorl's hernias, if detected and treated in a timely manner, are not dangerous. If the symptoms are ignored, the disease provokes further complications, the final result of which is a compression fracture of the spine. In adolescents, untreated Schmorl's nodes cause the formation of incorrect posture. Scoliosis negatively affects the functioning of the respiratory and digestive systems.
If the disease is advanced, it can develop into spondyloarthrosis.
A deep and advanced disease develops into spondyloarthrosis, causing usurative processes that provoke purulent inflammation and destruction of spinal tissue. Degeneration of discs and plates leads to the appearance of osteophytes. Progressive usuration can cause damage to the vertebral cartilage, which may result in the central nervous system being affected.
Stages of hernia development
The development of the pathological condition occurs over different periods of time, depending on the number of lesions, as well as the degree of tissue damage. However, any form of the disease occurs in 3 stages. The only difference is the time required for the disease to transition from one stage to another.
At stage 1, there is no symptomatology. The presence of the disease can only be determined if routine preventive diagnostics of the patient is carried out.
If you study the images, you can see that the fibrous ring of the intervertebral disc is somewhat damaged, but it is not completely torn, which explains the absence of symptoms. The condition of patients at this stage does not worsen, only a slight decrease in performance is possible.
At stage 2, the first symptoms appear, which is associated with further damage to the fibrous ring and progression of the disease. Depending on the location of the lesion, the pain is concentrated mainly in the cervical, thoracic or lumbar region.
Somewhat later, numbness of the limbs, weakening of muscles and poor circulation occur. Usually at this stage the patient consults a doctor to get help.
At stage 3, complications from internal organs appear, performance decreases significantly, and a change in the patient’s posture is observed.
When the focus is localized in the cervical spine, headaches become intense and are quite difficult to relieve with analgesics. At this stage, complications appear that aggravate the condition and can lead to irreversible changes.
Prevention
Schmorl's hernia can occur in almost every person and lead to serious complications, so it is important to prevent the disease. As recommendations for prevention, doctors advise:
- give adequate physical activity;
- do not work with weights with a weak lumbar girdle;
- follow the principles of healthy eating;
- if necessary, use an orthopedic mattress;
- control body weight;
- avoid physical inactivity;
- to refuse from bad habits.
Diagnostics
Schmorl's hernia on the spine is diagnosed quite simply, but doctors always use several methods to assess the general condition of the patient:
- A general and biochemical blood test helps to assess the patient’s general condition and see signs of inflammation, if any. It is considered an important diagnostic step and examines blood from a vein.
- Examination and questioning of the patient is considered an important stage of diagnosis. In this case, the doctor not only listens to the patient’s complaints, but also evaluates the skin, posture and possible negative changes that manifest themselves in the form of external signs. Based on the survey and examination data, an additional examination is prescribed.
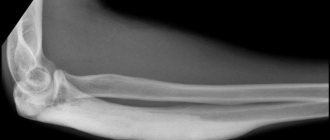
- X-ray of the spinal column in different projections is considered the most effective diagnostic method. Because it helps to identify the degree of tissue damage and the number of lesions in the spine. After studying the images, the doctor prescribes additional research and treatment.
- Magnetic resonance imaging of the spinal column is used as an additional diagnostic method. It is prescribed when radiography does not allow one to accurately determine the degree of tissue damage.
After receiving the diagnostic results, the specialist prescribes appropriate treatment depending on the symptoms and the presence of complications.
Features of treatment
Treatment of Schmorl's hernia in the lumbar region in the absence of symptoms should be aimed at preventing the progression of this disease. Hernia therapy should be carried out taking into account a number of factors, such as the patient’s gender and age, characteristics of his professional activity, the presence of concomitant diseases and the severity of the process.
Treatment of Schmorl's hernia has the following goals:
- elimination of pain syndrome;
- restoration and normalization of spine flexibility;
- prevention of possible complications;
- elimination or reduction of muscle spasms;
- improved blood circulation in the back muscles;
- improvement of metabolic processes in bone tissue.
The video explains how to treat Schmorl's hernia
Most often, when treating Schmorl's hernia, conservative therapy is used, which helps strengthen the musculoskeletal skeleton and involves the following:
- Rational and balanced nutrition. This includes fish, soy and dairy products, as well as those containing large amounts of protein.
Advice! Patients suffering from Schmorl's hernia are advised to reduce their salt intake, as it can be deposited in joints and bones.
- The patient must monitor his weight, since obesity puts additional stress on the spine.
- Therapeutic massage can relieve fatigue and back pain, minimizing muscle spasms, helping to normalize blood circulation and strengthen the back muscles.
Additionally, we recommend reading about how to treat a lumbar disc herniation at home in addition to this article.
Lumbar massage
↓ Be sure to study the recommended material on the topic ↓
What should not be done in case of lumbar disc herniation?
- If the patient has severe pain, he is prescribed painkillers.
- Physiotherapy. This is a very effective method that allows you to strengthen your back muscles, improving the flexibility of the spinal column.
- Spinal traction. Helps improve blood circulation in tissues, while increasing intervertebral clearance.
- Swimming. It is an excellent way to strengthen the muscles of the spine and back.
Advice! The patient should avoid jumping into water and lifting heavy objects.
Surgical treatment
For Schmorl's hernia, surgical treatment is not performed. Only conservative therapy is indicated, involving a complex of physiotherapeutic measures. The operation is performed when there is a complication when an intervertebral hernia or fracture occurs. When conservative therapy proves futile, surgery is performed.
Schmorl's hernia on x-ray
Treatment methods
Drug and non-drug treatment methods are used to treat patients. Typically, the doctor selects medications and additional methods that enhance the effectiveness of treatment and reduce the risk of complications.
Drug therapy
To alleviate the condition, anti-inflammatory, painkillers and drugs to eliminate tissue swelling are prescribed.
The most effective means:
- Spasmalgon is an antispasmodic medication that helps to significantly improve the condition and relieve spasms of the smooth muscles of the musculoskeletal system. The product eliminates pain and is used during exacerbation of the condition. The dosage is determined individually and ranges from 2-4 tablets per day. Treatment lasts 5-7 days.
- Ketorol is an analgesic and anti-inflammatory medication that is actively used to eliminate pain and stop the progression of the disease. The drug is taken for 5-7 days, 1-3 tablets per day. If necessary, the course can be extended, but only as prescribed by a doctor.
- Ibuprofen has pronounced anti-inflammatory and analgesic properties. It is taken 2-4 tablets per day for 5 days. For pathologies of the digestive tract, you should take the medication with caution.
- L-lysine not only helps relieve pain, but also has anti-edematous properties, which helps prevent the progression of the disease. The solution is administered intravenously using a dropper, after adding 5-10 ml to 200 ml of sodium chloride. Treatment lasts 10 days with daily manipulation.
- Actovegin improves tissue nutrition and blood circulation in the affected area. The drug is taken in courses of 2-3 weeks, the daily dosage is 3-6 tablets. The drug significantly improves the patient's condition.
- Neurorubin is prescribed to improve the condition of tissues; it contains B vitamins. The drug is administered intramuscularly at a dose of 3 ml per day for 10 days. If necessary, repeated courses are prescribed every 3-6 months.
- Teraflex contains substances that improve the condition of cartilage tissue. It helps increase the elasticity of the fibrous ring of the disc, stimulates the production of components responsible for the restoration of cartilage, and prevents its rapid destruction. Take 1 tablet 2 times per day, treatment lasts at least 6 weeks
Other drugs are also used if the patient's condition worsens, but in most cases, if therapy is started in a timely manner, more potent drugs are not required.
Physiotherapy
Schmorl's hernia on the spine can be treated using physiotherapy methods, which help to significantly improve the condition of the tissues and stop the progression of the disease. They cannot completely cure the disease, but they reduce the risk of complications.
Electrophoresis is considered the most effective method of physiotherapy. The method involves attaching special sensors to the skin in the spinal area, which deliver low-frequency electrical impulses to the tissues.
These impulses stimulate blood circulation and promote tissue repair. To obtain a therapeutic effect, you need to undergo at least 10 procedures every 3 days.
Massage
Massage is an effective and important stage of rehabilitation after completing a course of drug therapy. The procedure should only be carried out by a specialist. They last at least 30 minutes and are carried out once every 2-3 days. The minimum course duration is 15 sessions.
The method helps improve the condition of tissues, improves blood circulation and stops the progression of the pathological process. Against the backdrop of these changes, improvement is noted.
Exercise therapy
Therapeutic exercise is used in the recovery stage after acute symptoms have been eliminated with the help of medications. A set of exercises is selected for each patient individually, depending on the condition, location of the lesion and the presence of associated abnormalities.
Exercises are performed at least 3 times a week. At the initial stages, they are allowed to be performed for no more than 10 minutes. As the condition improves, the training time increases and gradually reaches 30 minutes. The first few lessons are best done under the guidance of an instructor, who will point out possible mistakes and explain safety precautions.
Surgery
Surgery usually involves replacing the affected vertebra with a titanium implant. It is performed under general anesthesia and involves a long period of rehabilitation, which includes medication, physiotherapy and exercise therapy.
The operation is indicated in the case of complete destruction of a vertebra, damage to several vertebrae at the same time, as well as pinching of the spinal cord, which disrupts the functioning of internal organs. The method of intervention and features of anesthesia for each patient are determined individually.
Other methods
Additional treatments include acupuncture. This method is not used very often, but is considered very effective provided that it is carried out by a specialist.
The procedure involves inserting special needles into biologically active points on the patient’s back. When they are stimulated, tissue restoration processes are accelerated. The session lasts up to 1 hour and is carried out 2-3 times a week for a month. If necessary, the course is extended to 2 months.
Surgery
When conservative methods of treating Schmorl's hernia do not produce results, and the patient's condition constantly worsens, doctors resort to surgical treatment. Indications may include not only acute pain, but also disruption of the normal functioning of internal organs and compression of the spinal cord.
Depending on the complexity of the hernia formation, the doctor performs surgical manipulation. This may be the introduction of a sclerosing substance using an injection or the removal of part of the vertebral body, fixing adjacent vertebrae.
Possible complications
If left untreated, patients develop complications.
The most common of them:
- Impaired patient mobility.
- Pathologies of internal organs.
- Disorders of the functioning of the pelvic organs.
- Rachiocampsis.
- Displacement of vertebral discs.
- Complete destruction of the bone tissue of the spine.
- Pinched nerve endings.
The most severe complication is the patient's loss of ability to move.
Schmorl's hernia is a common disease, localized on the spine, and can cause serious complications. To prevent the progression of pathologies, it is necessary to visit a doctor in a timely manner and undergo a course of therapy.
Etiology of disease formation
The figure shows the localization of Schmorl's hernia in the vertebra.
Schmorl's nodes in children are formed due to degenerative changes in the spine, during a period of sharp elongation in height. Scheuermann-Mau disease often leads to the occurrence of pathology. With Schmorl's hernia, the causes may be as follows:
- excessively increased activity of the patient;
- spinal injury, accompanied by damage to the integrity of thin hyaline cartilage;
- congenital diseases of the spine;
- sports and work injuries;
- imperfection of end plates;
- Vitamin D deficiency is another factor that makes bones and vertebrae weak and prone to wear and tear;
- sedentary work;
- oncological pathologies with metastases;
- lag in the development of the back muscle corset;
- age-related changes leading to weakening of bone tissue.
When spondyloarthrosis is diagnosed, Schmorl's hernia can also appear. This disease begins to form due to the destruction of the vertebral bodies in the presence of osteomyelitis and bone tuberculosis. If there is a predisposition to the occurrence of pathology, then pregnancy, scoliosis and impaired blood supply can cause the formation of a degenerative process.
Predisposing factors
A Schmorl's node can form due to the following diseases:
- Microfracture of the closing septum of the cartilage resulting from a spinal injury (the lumbar region most often suffers).
- Degenerative-dystrophic processes in osteochondrosis of the spinal column lead to deformation and destruction of the vertebrae.
- Osteoporosis, osteopenia are progressive chronic diseases associated with calcium deficiency that contribute to fragility and the formation of cavities in bone tissue.
- Kyphosis of the thoracic region and lordosis of the lumbar region.
- Heavy physical activity associated with lifting loads. Athletes involved in weightlifting are at risk.
- Hereditary disorders in the structure of spongy bone.
- The period of breastfeeding and childbearing is associated with hormonal and physiological changes in a woman’s body.
In adolescence, a Schmorl's hernia can appear as a result of the rapid growth of muscle tissue, which contributes to high compression on the slowly developing vertebrae. This condition in medicine is called acceleration.
Causes
Schmorl's hernia is diagnosed at any age, but more often it is found in children. This is due to a large percentage of the genetic etiology of this disease, as well as to the disproportionate growth of spinal column tissue.
The main causes of vertical hernia:
- Loss of cartilage tissue density, characterized by its softening. Disturbance of mineral metabolism in the bone, which manifests itself as cavities in bone formation.
- Disruption of metabolic processes in the spine, which can result from a deficiency of vitamins and microelements, as well as diseases based on metabolic failure, inflammatory processes, and infections.
In young children, Schmorl's nodules can form due to a genetic predisposition. The disease can be transmitted from generation to generation and be multiple in nature, affecting several vertebrae. This phenomenon is explained by the weakness of cartilage tissue, which is hereditary.
The period of active growth of a child is associated with different rates of division of bone and cartilage cells. Usually the bone tissue “lags behind” and does not have time to grow in the enlarging vertebrae, due to which a cavity is formed. The void is filled with cartilaginous formation and a Schmorl's hernia is formed. Not every child can have a pathological process. The presence of an endplate defect at the genetic level or of an acquired nature is an important condition for the onset of the disease.
In adults, the disease often forms in the lumbar spine. Initial deformation of the vertebra is provoked by heavy lifting or mechanical damage. In addition, a decrease in bone density after metabolic and inflammatory diseases may be to blame.
What it is?
A Schmorl's hernia (Schmorl's node) is a hernia that penetrates into the cavity of the upper or lower vertebra. According to the anatomical structure, between the two vertebrae there is a cartilaginous disc, which is designed to soften shocks during movement.
The disc consists of elastic cartilage tissue, which is particularly dense at the edges of the disc. This structure is necessary to “hold” the jelly-like core, due to which the shock-absorbing ability is achieved. If, under the influence of provoking factors, the structure of the cartilage changes and becomes weak, the core of the disc “comes out” and forms a cartilaginous knot.
For a vertical hernia to form, two prerequisites must be present. One of them is a weak cartilage shell, which in this case manifests itself in defects of the endplate at the junction with the vertebrae. The second condition is the formation of voids in the bone tissue on the lower or upper part of the vertebra. If the two factors are present, cartilage tissue fills the space in the bone and forms a nodule, which is named after the German scientist who first described the disease.