Causes
At the moment, there is no consensus among pulmonologists as to whether hamartoma is a denovo tumor or whether it arises as a result of dysembryogenesis and further tumor degeneration. Some experts consider hamartoma to be a malformation of the lungs, which is formed as a result of a violation of the anlage and formation of bronchopulmonary structures at the stage of embryogenesis. The connective tissue, cartilaginous and smooth muscle elements of the neoplasm are formed from germinal tissue - mesenchyme. Sometimes epithelial structures are involved secondarily from the surrounding lung tissue in the process of tumor growth or from the mesodermal and endodermal bronchial primordia.
Predisposing factors contributing to the development of neoplasms include genetic predisposition, gene mutations, and prolonged exposure of the body of future parents to teratogenic and mutagenic agents.
Not to be confused with hematoma.
Large hamartoma from the spleen. The hamartoma is the dark round object on the left that dominates the image. This is a cross section; the growth is about 9 cm in diameter, whereas the entire spleen is about 11 cm in diameter.
Medical genetics, Pathology
A hamartoma is a primarily benign, focal malformation that resembles a neoplasm of the tissue of its origin. While traditionally considered a developmental malformation, many hamartians have clonal chromosomal aberrations that are acquired through somatic mutations and on this basis are now considered neoplastic. It grows at the same rate as surrounding tissue. It consists of tissue elements usually found in this place, but they grow in a disorganized manner. Hamarths occur in many different parts of the body, and are most often asymptomatic, non-palpable (undetected until they are found by chance during imaging studies obtained for another reason).
Additionally, the definition of a hamartoma versus a benign tumor is often unclear, as the lesions may be clonal. Lesions such as adenomas, cyst developments, hemangiomas, lymphangiomas and rhabdomyomas within the kidneys, lungs, or pancreas are interpreted by some experts as hamartomas while others consider them to be true neoplasms. Additionally, although hamartus shows benign histology, there is a risk of some rare but life-threatening clinical problems such as those in neurofibromatosis type I and tuberous sclerosis.
It is distinct from choristoma, a closely related form of heterotopia. The two can be differentiated as follows: a hamartoma is an excess of normal tissue in a normal situation (such as a mole on the skin), while a choristoma is an excess of tissue in an abnormal situation (such as pancreatic tissue in the duodenum).
Forecast
In most cases, the prognosis of the disease is favorable if a person promptly seeks help from a specialist and decides to undergo surgery. An unfavorable prognosis develops due to the pathological growth of the tumor, which compresses the lung tissue.
After timely surgery and rehabilitation, the person returns to a full life, but his condition is monitored using periodic radiography. Advanced forms of the disease require complete resection of the lung or transplantation of the entire organ.
Relapse of the disease is observed in only 1% of patients with a similar problem. Usually surgery resolves the issue forever. It is important to exclude the development of oncology, since tumor growth can be triggered by the chaotic division of cancer cells.
Hamartoma is a benign tumor, but in the absence of surgical intervention it can provoke acute respiratory failure and death. The neoplasm is formed during embryonic development, so it is impossible to influence and prevent its occurrence.
Symptoms
The clinical picture of pulmonary hamartoma depends on the size of the tumor, its location in the relatively large bronchi, diaphragm and chest wall. Based on the severity of symptoms of the tumor process, three stages of the disease are distinguished:
Stage I, caused by an asymptomatic course;
Stage II, characterized by scant clinical symptoms;
Stage III is characterized by the development of severe symptoms, which is due to the impressive size of the tumor and compression of surrounding tissues.
Most often, hamartomas are characterized by a long-term and asymptomatic course. The tumor is discovered accidentally during a chest x-ray or during an autopsy. With peripheral localization and small size of the tumor, the development of clinical symptoms may not be observed.
After the hamartoma reaches an impressive size, compression occurs on the tissues of the lung, bronchi, diaphragm and chest wall. The patient experiences shortness of breath, pain in the chest on the affected side, which most often appears at the height of a deep breath and is accompanied by a cough, and with severe physical exertion - hemoptysis. When a hamartoma compresses a large bronchus, a clinical picture occurs that is characteristic of a central lung tumor.
With endobronchial localization of the hamartoma, local obstruction of the bronchial tube occurs, which is accompanied by hypoventilation and segmental atelectasis of the corresponding part of the lung and the occurrence of obstructive pneumonia. In this case, the clinical picture of hamartoma may be accompanied by the appearance of symptoms of a chronic infectious process in the lungs.
With multiple pulmonary hamartoma, Carney's triad may occur, combined with gastric leiomyoblastoma and extra-adrenal paraganglioma, or Cowden syndrome, characterized by multiple benign formations of internal organs and a high potential for developing cancer of the breast and thyroid glands, digestive tract and genitourinary system.
Treatment
If a laboratory-confirmed hamartoma with a diameter of less than 2.5 cm is characterized by the absence of compression of adjacent tissue structures, then a specialist should observe the dynamics of the disease for several months. Further selection of therapy depends on changes in the size of the shadow on the radiograph.
Pathology can only be eliminated surgically. The peripheral tumor is removed by enucleation, segmental or marginal resection of the organ. The pulmonary lobe is excised in case of prolonged compression of blood vessels, parenchyma, bronchi, or complicated course of the disease.
To remove an endobronchial hamartoma, bronchotomy with removal of the node, fenestrated or circular resection of the bronchus with further suturing, and plastic surgery of the tumor are used.
To exclude peripheral or endobronchial cancer, urgently resort to postoperative histological examination of the defect. If the disease is not advanced, then minimally invasive cryodestruction, electrocoagulation, and laser evaporation are possible.
Diagnosis of lung tumors in Israel
The Ichilov Complex clinic provides not only an integrated approach, but also rational planning of all procedures so that the patient spends as little time as possible waiting. Typically, diagnostic measures take only 3 days.
First day – consultation with the medical director and leading oncologist
The first day is usually scheduled for a consultation with the medical director and the leading oncologist. At this stage, additional diagnostic measures are planned based on the patient’s condition and available medical documentation.
Day two – diagnostic procedures
Diagnosis of lung tumors in Israel includes a wide range of studies.
- X-ray allows us to draw preliminary conclusions about the presence of a tumor in the lungs.
- Computed tomography is used for a more detailed study of neoplasia.
- PET-CT is used to look for metastases.
- Bronchoscopy allows you to take a sample of the tumor for histological examination (CT-guided biopsy can also be used for this).
- Blood tests for specific biomarkers can be used to determine the prospects for using targeted therapy.
Third day – consultation
The final stage of diagnosis is a discussion of the result at a council consisting of specialists who will treat the patient. A collegial approach allows you to avoid mistakes and take a balanced approach to prescribing a treatment regimen. The patient is present at the consultation and takes part in the discussion, so at this stage he is fully informed about what the upcoming treatment will be and the full cost of the clinic’s services.
Life prognosis for pulmonary hamartoma
The prognosis for life with this diagnosis is favorable. Such tumors are usually characterized by slow growth. However, it is worth considering that hamartomas can reach enormous sizes.
Malignancy of neoplasms of this type is quite rare. Malignancy does not exceed 6-8%. If malignancy occurs, then degeneration can affect both tissues of mesenchymal and epithelial origin. Metastases during malignancy of hamartoma can be localized in the regional lymph nodes of the chest, pleura, liver and thoracic spine.
Be healthy!
Advantages of Israeli hospitals
- Doctors with enormous clinical experience are among the world's best experts in the diagnosis and treatment of tumors of the respiratory system.
- Examination within a few days using the most modern diagnostic techniques.
- The widest range of treatment options includes various types of open and minimally invasive lung surgeries, contact and non-contact radiotherapy, systemic and targeted chemotherapy.
- In almost any Israeli clinic, the patient is assigned a personal curator-translator, who is responsible for coordinating doctors, solving everyday issues and translating documents.
Classification
Based on tissue predominance
- Chondromatous (chondrogamartoma, chondroma).
- Lipomatous.
- Leiomyomatous.
- Fibromatous.
- Angiomatous.
- Organoid hamartoma (there is a combination of different tissues)[7][13][22][23].
By number of tumors
- Single hamartoma.
- Multiple hamartomas[11][19].
By localization
- Peripheral (parenchymal).
- Endobronchial[13][24].
3. Symptoms and diagnosis
The vast majority of cases of pulmonary hamartoma are asymptomatic, and the carrier may not even be aware of the presence of a tumor for a long time. In isolated cases, with a significant size and specific localization of the hamartoma, painful discomfort, wet cough, as well as changes in respiratory acoustics that can be detected by auscultation are encountered.
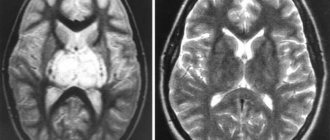
As a rule, a hamartoma is discovered accidentally, for example, during a preventive or planned (for another reason) X-ray examination, and necessarily becomes the object of differential diagnosis - primarily with malignant neoplasia. Depending on the situation, computed tomography, fiber-optic bronchoscopy, and puncture are prescribed to take a biopsy sample; histological analysis allows us to definitively establish the nature of the tumor.
| hamartoma | Speciality | |
Pathological anatomy
Macroscopically, a hamartoma usually has a round shape with a smooth or finely lumpy surface, and a dense elastic or dense consistency; it does not have a capsule, but is clearly demarcated from the surrounding lung tissue [13]. On a section, the tumor is grayish or grayish-yellow, lobular in appearance, includes foci of cartilage and is divided by fibrous layers, lime inclusions are often detected[18]. In some cases, a hamartoma removed from its bed breaks up into separate lobules. The tumor bed is formed by compressed alveoli; there is no anatomical connection between it and the tumor, which explains the possibility of enucleating the hamartoma during surgery[19][20]. Most pulmonary hamartomas do not exceed 4 cm in diameter, but sometimes they can reach 10 cm[1]. In the medical literature there are isolated descriptions of cases of giant hamartomas[21], when the tumor occupied 2 lobes of the lung and even 3/4 of the corresponding half of the chest (Prozorov A.E., 1939)[15][19].
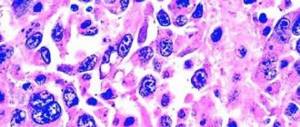
Microscopically, hyaline or, less commonly, elastic cartilage of an atypical structure is determined, around which there are layers of fatty and fibrous or myxoid connective tissue, sometimes hyalinized, with small round or oval nuclei. Areas of ossification or calcification are also identified. Sometimes smooth muscle fibers and lymphoid accumulations are found [13][19][20]. Between the cartilaginous plates there are often slit-like passages that can transform into cysts. The lining of these passages and cysts is formed by glandular epithelium. The epithelial component of a hamartoma is usually represented by a small number of malformed glandular and papillary structures[14].
Spreading
This disease is diagnosed in more than half of the cases of all identified pulmonary tumors that arise on the surface or on the inside of the lungs. In men, hamartoma is detected during preventive X-ray examinations on average three times more often than in women of the same age, and the right lobe is mainly affected. The approximate age of patients is about 40 – 45 years.
There are several types of hamartoma:
- Endobronchial (a very rare form, in only 10% of cases);
- a peripheral tumor localized in the anterior pulmonary segments is isolated;
- There is a peripheral tumor arising on the posterior segments.
You shouldn’t treat a runny nose as a minor ailment. You may miss the first symptoms of sinusitis, which will lead to long-term illness. A signal of the development of laryngitis is your frequent loss of voice. Find out from the article the main reasons for the development of vocal cord disease.
The disease consists of lung tissue, but, nevertheless, its structure is not similar to the structure of the organ itself due to the arrangement of cells different from the normal position of cells, as well as varying degrees of specific differentiation. The disease has the shape of an oval or circle with slightly uneven edges. The structure of the neoplasm is often with a smooth surface or slightly lumpy, high density. Quite clearly differentiated from the lung tissue itself.