Pneumonia is a dangerous disease of the lower respiratory tract, which is associated with inflammation of the lung parenchyma. As a rule, the course is quite severe, especially in children under five years of age. However, there are also atypical, asymptomatic forms - more dangerous pneumonia; symptoms in children are already more difficult to determine than in adults. Considering that diagnosing this kind of disease is much more difficult, and the consequences from it can be very, very serious.
This disease occurs, in most cases, as a continuation of an acute respiratory viral infection. There is another type - aspiration pneumonia. It occurs when food or vomit enters the respiratory tract. It happens quite often in children, usually under the age of one year (especially in children with pyloric spasm or pyloric stenosis - they often spit up). Quite rarely, pneumonia is primary in nature (that is, it develops as an independent pathology). Such a dangerous disease as pneumonia in children under one year of age, the symptoms are characteristic enough for the disease to be diagnosed in time.
Reasons for the development of the problem
Pneumonia develops in children for various reasons. There are two main groups of reasons for the problem.
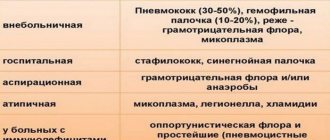
The first group of factors concerns the penetration of pathogenic flora into the lower respiratory tract. What microorganisms cause pneumonia in a baby? Typical and atypical infectious viral structures can be distinguished.
We have to talk about the following agents:
- Pneumococci. Real record holders among the culprits in the development of pneumonia. They are round bacteria capable of forming spores in unfavorable conditions. They cause the development of pneumonia in 60-80% of clinical situations. They provoke complex pneumonia with a protracted and prolonged course.
- Staphylococci. Staphylococci provoke the development of pneumonia that is dangerous to life and health. Staphylococcus aureus and Staphylococcus hemolytic (to a slightly lesser extent) pose a particularly great threat to the patient’s health. The danger lies in the likelihood of inappropriate treatment and resistance to therapy in the future.
- Streptococci. They cause weak, but long-lasting and difficult to treat, sluggish inflammation of the lungs. Streptococcus manifests itself most actively in children's bodies.
Here are the three most prominent causes of pneumonia. There are, as already mentioned, atypical pathogens.
Atypical pathogens
- Klebsiella. It only affects children. Adults suffer from pneumonia induced by Klebsiella spp. much less frequently.
- Chlamydia.
- Mycoplasmas. Mycoplasma is a general name for microorganisms of a single type. This includes mycoplasma hominis, various types of ureaplasma, etc. These are extremely harmful agents that provoke pneumonia that is difficult to cure.
- Coronaviruses. Responsible for the formation of atypical pneumonia. The most famous cases of the pandemic of atypical pneumonia in 2002-2003.
- Legionella. They act as the most dangerous agents and often provoke fatal pneumonia in representatives of the younger age group.
Herpes spectrum viruses
There are many of them. There are at least 6 strains that can cause pneumonia.
- Strain of the first type. It's also the herpes simplex virus. It most often provokes pneumonia in young patients. However, pneumonia itself is not typical for HSV.
- Strain of the second type. Genital herpes. Causes life-threatening lesions.
- Strain of the third type. Varicella-Zoster virus. Detects chickenpox and herpes zoster. It extremely rarely provokes pneumonia in children, which cannot be said about adult patients.
- Strain of the fourth type. Epstein-Barr virus. Causes life-threatening diseases, including mononucleosis.
- Strain of the fifth species. Cytomegalovirus. Provokes cytomegaly with the formation of generalized damage to the body. The pathogenic process involves the lower respiratory tract, organs of the digestive tract, cardiovascular system, and dermal layer.
- Herpes of the sixth type, subtype “B”. Provokes pneumonia.
The list of pathogens is incomplete. However, they are the ones that most often provoke pneumonia.
Causes of the disease
The occurrence of pneumonia in a child is facilitated by factors such as weakened immunity, chronic pulmonary diseases, frequent colds, and the special structure of the pulmonary system. And also some features of the child’s body create a favorable environment for the proliferation of bacteria. These include :
underdevelopment of the lungs for adequate air exchange;- low porosity;
- small lung volume;
- narrow air passages;
- too thin mucous membranes, which contribute to the appearance of edema;
- Difficulty removing mucus.
If one of the family members smokes in the apartment, this also increases the risk of developing infection. Moreover, it enters the lungs not only through the bronchi, but also through the bloodstream and lymph. Most often this occurs during chronic inflammatory processes in other organs and causes secondary pneumonia. Penetration of allergens, toxic fumes or chemicals into the respiratory system can also provoke pneumonia.
There is such a thing as congenital pneumonia. The child becomes infected during childbirth (when amniotic fluid enters his body) if the mother is infected with chlamydia or herpes.
Routes of infection
The ways of transmitting pathogenic flora to children are multiple.
This:
- Contact and household path. As a rule, the child “picks up” pathogenic microorganisms in the maternity hospital. Infections are transmitted from infected personnel to a small patient through dirty hands, undisinfected nipples, etc. If a child suffers a similar fate in the maternity hospital, there is a high probability of infection through interaction with other children.
- Descending path. When passing through the infected birth canal of the mother.
- Placental or perinatal route. Through the placenta, bypassing all anatomical barriers to the child.
Causes of a weak immune response
The second significant factor in the development of the problem is a decrease in the activity of the body’s defense system.
Some of the reasons for this problem include:
- Frequent acute respiratory viral infections. They suppress the immune system, exhaust it so much that there is simply no strength left to counteract distant foci.
- Single or, especially, multiple hypothermia.
- Prolonged stress, psycho-emotional stress and similar factors. The fact is that as a result of stress, stress hormones are actively synthesized: adrenaline, cortisol, norepinephrine. They actively suppress the synthesis of specific immune cells. This reduces the activity of the immune system.
- Tobacco smoking (in adolescents) does not have the best effect on the immune system due to stenosis of large main vessels.
- Poor nutrition. Children rarely eat properly and fully. Much more often we are talking about an excess of fast carbohydrates, fats, etc.
In a combination of two groups of reasons, the first signs of pneumonia in a child appear.
The difference between bronchitis and pneumonia
It is simply impossible to differentiate bronchitis from pneumonia in children, as they say, “by eye.”
There are differences in symptoms, there are differences in objective diagnostic data. It is based on the research results that conclusions need to be drawn.
In general, we can name the following differences between one disease and another:
- Body temperature during pneumonia is usually a few tenths of a degree or several degrees higher. Thus, with bronchitis, low-grade fever predominates with an increase in temperature to a maximum of 38.1 degrees. Inflammation of the lungs is often accompanied by febrility and even pyretic thermometer readings (over 38.1 degrees). But you need to remember that bronchitis, bronchitis and pneumonia are different.
- The duration of hyperthermia in pneumonia is more than three days. With bronchitis - less.
- With pneumonia, the cough is almost always wet, with the discharge of a large amount of viscous, thick sputum. The same cannot be said about bronchitis.
- Pneumonia is accompanied by blue discoloration of the nasolabial triangle (cyanosis).
- Also, pneumonia is accompanied by shortness of breath and suffocation. The work of additional muscles is observed.
However, it is possible to limit diseases only through objective research.
Treatment of pneumonia
Pneumonia is a serious disease that can threaten the life of a child, especially at an early age. The successful use of antibiotics has significantly reduced mortality from pneumonia, however, untimely consultation with a doctor, delayed diagnosis and late initiation of treatment for pneumonia can lead to the development of severe complications, even leading to disability. Therefore, in the case of a cold, you should not try to diagnose your child yourself, much less treat him. A timely visit to the doctor and strict implementation of all his prescriptions will protect the child from the unpleasant consequences of the disease.
Signs and symptoms
The symptoms of pneumonia in children are quite specific. Intense inflammation of the pulmonary structures affects.
With interstitial pneumonia or small-focal lesions, there may be no temperature.
- In a child, the first signs of pneumonia are expressed by hyperthermia. That is, an increase in body temperature above normal values. As a rule, pneumonia is characterized by the development of febrility (over 38.1 degrees Celsius). Indicators even higher are possible, such as pyretic temperature (39-40 degrees Celsius).
- Next, an intense cough develops with the discharge of a large amount of sputum. However, this is not an axiom either. There may be an absence of cough, which is typical for small focal forms of pneumonia, or a dry cough.
- Pain when inhaling and exhaling. Seen frequently. The pain is dull and intensifies with inhalation or exhalation.
- Symptoms of general intoxication of the body with characteristic manifestations such as headache, weakness, heaviness throughout the body, a feeling of body weakness, etc.
- Shortness of breath, suffocation. Development of respiratory failure.
- A child may have no symptoms of pneumonia at all. Or appear sluggishly. In this case we are talking about a typical, classic type of pneumonia.
Symptoms of atypical pneumonia
Signs of atypical pneumonia are quite nonspecific. The same symptoms of pneumonia appear, but to a less active degree.
With legionellosis, on the contrary, their more intense manifestation is observed. In any case, the specific symptoms in children depend on the causative agent of the disease.
Signs of pneumonia in children
In most cases, pneumonia develops as a complication of a viral infection, and initially the child’s temperature rises, a runny nose appears, appetite decreases, and the baby becomes tearful. The temperature during pneumonia is maintained for three days, then it is possible, but not necessarily, for an imaginary improvement in the condition, when the temperature can return to normal for one or two days. And again it suddenly increases again, increased breathing rate, cough, pale skin, sweating, shortness of breath, and general poor health appear.
Cough, contrary to popular belief, is not the main symptom of pneumonia; it may not be present at all. If such a symptom is present, it can be different: superficial or deep, paroxysmal, dry or wet. Symptoms of intoxication increase. The child may complain of a headache, dizziness, vomiting, lethargy, pain and bloating, and diarrhea.
There is no single symptom specific to pneumonia. Only a doctor can determine the disease based on complaints, the timing of the disease, and the dynamics of its development. When examining a baby, the doctor can obtain a lot of information: signs of intoxication, respiratory failure, the presence or absence of wheezing in the lungs.
In young children, especially in the first year of life, there may be few clinical manifestations, but intoxication and respiratory failure will help the doctor suspect pneumonia. At an early age, pneumonia is “seen better than heard”: shortness of breath, retraction of auxiliary muscles, blue discoloration of the nasolabial triangle, refusal to eat may indicate this disease.
Diagnostics
Diagnosis of a pathology such as pneumonia in a child, the symptoms of which were described above, does not present great difficulties in the vast majority of cases.
Pulmonologists are responsible for identifying the root cause of the described illness and its treatment.
At the initial appointment, the patient is interviewed about complaints and their nature, duration and possible origin.
Subsequently, an anamnesis is collected (that is, the doctor identifies what diseases the patient has suffered or is currently suffering from). It is important to determine the characteristic prerequisites for the disease: contact with patients, etc.
Finally, it’s time for objective research:
- X-rays of the chest organs. Required in all cases. Allows you to identify characteristic signs of inflammation of the pulmonary structures and bronchial tree. Gives typical highlights or blackouts.
- Bronchoscopy. It is prescribed extremely rarely. Only in controversial cases.
- MRI/CT diagnostics. It is also prescribed only in controversial cases. Required to clarify the nature of the process with a small focus or sluggish flow.
- General blood test. Gives a classic picture of the inflammatory process with the formation of leukocytosis and an increase in the erythrocyte sedimentation rate.
- Analysis of sputum and its culture on nutrient media. This way you can detect a specific pathogen and its sensitivity to antibiotics.
This is more than enough to verify the diagnosis.
Treatment
Therapy is specific and in most cases is carried out in a hospital setting.
The following medications are required:
- Anti-inflammatory drugs of non-steroidal origin. They help relieve generalized inflammation, as the name of the pharmaceutical group suggests.
- Antibacterial pharmaceuticals. Required to destroy the original source of the problem.
- Corticosteroids to relieve inflammation.
- Analgesics for pain relief.
- Bronchodilators to ease breathing and relieve bronchospasm.
If the inflammation is caused by Koch's bacillus, only fluoroquinolones can fight it. The development of resistance to this group of antibiotics will mean a death sentence for the patient.
Treatment should be systematic and comprehensive. Only doctors should perform therapy.
Self-administration of medications leads to the fact that the virus, bacteria or other agent only becomes stronger. Their resistance to the antibiotic increases, which poses a danger to the patient’s life.
Treatment and prevention measures
Antibacterial therapy is carried out only after confirmation of the causative agent of the disease within 10 days. In cases where pneumonia was caused by a virus, mucolytic and antipyretic drugs, bronchodilators and antispasmodics are prescribed for treatment.
Treatment of severe conditions is carried out in the intensive care unit with artificial ventilation of the lungs. In the absence of complications, the child’s full recovery occurs after 4 weeks.
During the recovery period after suffering any lung disease, walking in the fresh air is important. Parents should ensure that the child does not become overcooled or overtired.
You should also find out why the child may often get sick. For example, you should be wary if the occurrence of ARVI, influenza, or bronchitis occurs more than twice a year.
Reasons for hospitalization
The child's body is extremely unpredictable. Therefore, hospitalization is recommended in most cases.
The absolute grounds for hospitalization are:
- Intense shortness of breath. Dyspnea is an increase in the number of breathing movements per minute.
- Choking of any severity. It is fraught with the development of breathing problems (respiratory failure). Possible death.
- Increased body temperature above 39 degrees Celsius.
- Tension of muscles that are not usually responsible for the breathing process.
- Stiffness of the neck muscles.