Brain contusion is a severe traumatic brain injury, which always results in a disruption of the structure of brain tissue with the formation of a focus of necrosis (local tissue death). A lot depends on the depth and extent of the lesion, as well as on how quickly first aid was provided: the volume of treatment, its timing, the duration of the rehabilitation period and the restoration of body functions.
The main and, in fact, the only cause of this pathology is head trauma, which can be either open or closed:
- household injuries (most often falling from a height onto a hard surface or objects, including from one’s own height);
- hitting your head during a traffic accident;
- criminal injury (blow to the head with a blunt object);
- injury at work, especially related to high-altitude work;
- sports injury;
- injury received during an attack of epilepsy and other diseases accompanied by convulsive syndrome.
General
Brain contusion also has another name – contusion. This term refers to an injury that damages structures related to the brain. Any part can be affected, but most often the poles and lower parts of the frontal and temporal lobes are affected. With brain contusions, the overall picture is formed from a combination of general cerebral, focal and autonomic symptoms. The extent of damage depends on the severity of the brain injury.
Treatment of a brain contusion must be carried out in a hospital and be comprehensive. Contusion is a pathology that may not leave complications behind, but can make a person disabled for life.
Hard-to-distinguish options
Concussion and brain contusion are classified as closed craniocerebral injuries (TBI), since soft tissues in these cases are not damaged, and abrasions, if any, do not extend beyond the aponeurosis. Concussion is considered to be the most favorable variant of TBI with a fairly encouraging prognosis. During a concussion, as a result of extreme inhibition of nervous tissue, functional changes occur, which, as a rule, are reversible.
As for brain contusions, there are both functional impairments and morphological metamorphoses, which are areas of dead tissue (“graveyard” of nerve cells), and these transformations for the worse can be so profound that they leave consequences for life.
It should be noted that it is not always possible to immediately draw the line between a severe concussion and a mild brain contusion. Differentiation of these conditions is initially hampered by the discrepancy between neurological disorders and the severity of damage to brain structures. In case of a concussion, minor morphological changes may also be present at first, which usually do not give a clear clinical picture characteristic of focal neurological disorders and therefore go unnoticed. Meanwhile, a concussion of the brain does not give cause for reassurance; in the future (with inadequate therapy), this type of TBI can result in very unpleasant complications. A brain injury is already initially ready for such “surprises.”
A brain contusion is characterized by a combination of general cerebral symptoms, which are also present with a concussion of the brain, and local (local, limited to foci) clinical manifestations, which, in turn, depend on the location of the blow.
https://youtu.be/1DSD47VVEAs
Causes of injury
Any mechanical injury entails bruises. A brain contusion can occur as a result of an accident, professional, domestic, criminal or sports injury. In preschool age, UGM in a child is caused by various types of falls, as is brain damage in infants. A factor in brain injury in a newborn is the narrow pelvis of the woman in labor.
This bruise can also occur when a person suddenly falls during a paroxysm of epilepsy or an ischemic attack. Often bruises are accompanied by a skull fracture and intracranial bleeding.
Damage classification
ICD-10 does not have clear criteria for designating a brain contusion. It is considered most appropriate to divide brain contusion into three degrees:
- Mild brain contusion.
- Moderate brain contusion.
- Severe brain contusion.
Each of the listed forms has its own clinical characteristics and consequences.
- A mild injury is accompanied by broken bones, hemorrhage, and the victim may lose consciousness for a short time.
- Moderate brain contusion is caused by being in an unconscious state for up to seven hours and problems with vision. Severe headache and hemorrhage may occur. The bones of the skull often break. With a moderate injury, body temperature may increase.
- If a person has been seriously injured or the brain stem has been damaged, the victim may be in a comatose state for a long time, his heart rhythm is disturbed, his breathing becomes rapid, and his blood pressure rises.
Depending on the location of the injury, disruption occurs in different areas:
- When the trunk is injured, functions important for life are disrupted.
- Contusion of the soft tissues of the brain is a serious pathology that may be accompanied by hemorrhage.
- Damage to the frontal lobe. Minor damage, as a rule, does not cause significant deviations, while severe damage to the posterior parts of this lobe leads to serious consequences.
Brain contusion can occur with both closed and open TBI.
In a child, this bruise is also divided into 3 degrees of severity, but only a specialist in this field can correctly differentiate all this. For example, meningeal signs are not as common in children as in adults. In addition, the symptoms of brain damage are especially different in newborns and young children, when the fontanelles are still open, the cranial bones are pliable, and the sutures are not ossified. Here there may be no obvious signs of pathology or an asymptomatic course of the disease, which does not exclude the development of severe complications in the future.
Symptoms, treatment and prevention for VSD
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Even healthy people have periods in their lives when, without changing their lifestyle, they become more tired, suffer from insomnia, and become lethargic or irritable. If the causes of unpleasant symptoms are vitamin deficiency, stress, overwork, after rest and vitamin therapy you feel better. But this is also how the first signs of vegetative-vascular dystonia (VSD) make themselves felt.
Strictly speaking, vegetative-vascular or neurocirculatory dystonia is not an independent disease (it is not in ICD-10), but a symptom complex, a signal from the body that something is wrong with it, its request for help. Modern medicine considers this condition intermediate between health and disease and calls it “VSD syndrome.”
Most often, vegetative-vascular dystonia is observed in schoolchildren aged 7-8 years and in adolescents, and in girls more often than in boys. But to one degree or another, it is also recorded in adults. What is this disease that is “not really a disease”? How dangerous is VSD and how to treat it? How, in general, can you treat something that doesn’t exist?
How the nervous system works
To understand what VSD is, you need to understand how the autonomic nervous system works. This section of the central nervous system is a control center that regulates unconscious physiological processes in the body: heartbeat, breathing, digestion, the functioning of endocrine and other glands.
- Its sympathetic department is responsible for daytime activity, response to physical and mental stress (increased heart rate, vasoconstriction, increased blood pressure). "Simpatika" works mainly during the day.
- The parasympathetic department regulates the restoration of strength during sleep and rest (decrease in heart rate, dilation of blood vessels, decrease in blood pressure). “Parasympathetic” is activated mainly at night.
In a healthy person, the sympathetic and parasympathetic autonomic systems are activated alternately and in concert, which allows the body to respond to external influences in a timely manner and control the functions of organs. If their relationship is disrupted, vegetative-vascular dystonia, or autonomic dysfunction of the vascular system, occurs.
Causes and risk factors
One of the causes of autonomic vascular dystonia is heredity. We are talking not only about the increased risk of primary VSD, but also about those diseases that provoke it as secondary. These are congenital dysplasia (underdevelopment) of connective tissue, heart and vascular defects and other pathologies. Hereditary dystonia manifests itself in early childhood.
Risk factors for secondary vegetative-vascular dystonia are:
- Diseases of the central nervous system and peripheral nervous system; traumatic brain injuries (bruise, concussion), which provoke a violation of autonomic functions.
- Osteochondrosis, especially of the cervical spine. People with vegetative vascular dystonia often complain of pain and “crunching” in the neck, dizziness when turning the head.
- Neurasthenia, neuropsychiatric diseases.
- Pathologies of the endocrine system (diabetes mellitus, hypo- and hyperthyroidism, thyrotoxicosis, hormonally active adrenal tumor - pheochromocytoma).
- Diseases of blood vessels and internal organs (pancreatitis, stomach and intestinal ulcers, atherosclerosis, lung diseases); acute radiation sickness.
- Occupational illnesses. Autonomic vascular dystonia sometimes develops in people who work with chemicals.
- VSD occurs during periods of hormonal changes (pregnancy, after childbirth, adolescence). At this time, the autonomic system does not cope with its function due to excess load on the body.
Vascular dystonia is complained of by people who work at a desk, move little and do not know how to actively rest, and are overweight or too underweight. The peculiarity of autonomic vascular dystonia is that it can occur suddenly. The impetus for VSD can be events that made you worry: troubles at work or in the family, a nervous breakdown. VSD makes itself felt during climate change, against the background of colds and flu, alcohol abuse or an “overdose” of tea and coffee. In summer, it is easy to “earn” vascular dystonia by overheating in the sun, and in winter, vascular spasms begin due to hypothermia.
Types of VSD
As a result of vegetative vascular dystonia, the brain and heart, kidneys, and limbs suffer. Therefore, autonomic dystonia syndrome is like a chameleon: in different people it manifests itself with such different symptoms that it is difficult to suspect their common cause. There are three types of pathology: hypertensive, hypotonic and mixed.
- If, regardless of the “internal need,” the sympathetic nervous system predominates during the day, they speak of a hypertensive type of vegetative-vascular dystonia. The person complains of attacks of palpitations and/or panic, anxiety, gets tired quickly, but has difficulty falling asleep in the evening. Blood pressure is elevated or unstable.
- When the parasympathetic nervous system predominates throughout the day, a person feels weakness, drowsiness, fatigue, and occasionally dizziness and fainting; we are talking about the hypotonic type of VSD. The pressure is reduced.
- When the sympathetic and parasympathetic systems “fight” for leadership, alternately winning and losing, hyper- and hypotonic symptoms replace each other, they speak of a mixed type of autonomic vascular dystonia.
Upon examination, it turns out that the organs and systems are in order, there are no pathologies in them, and such VSD is called primary. If the symptom complex of vegetative-vascular dystonia occurs against the background of another disease, it is considered secondary.
Symptoms
In people suffering from autonomic vascular dystonia, about one and a half hundred symptoms and about 30 disorder syndromes have been described, which are conventionally divided into several large groups. The most common:
- Cardiovascular (cardioneurosis). It can be cardiac, with heart rhythm disturbances, hyper- and hypotonic, mixed. The main complaints of patients with cardioneurosis:
- unstable blood pressure;
- cardialgia (heart aches, tingles, pulsates painfully).
vascular reactions (pallor of the skin, chilliness or numbness of the hands, feet, hot flashes);
Unlike angina, cardiac pain with VSD does not depend on the load and does not go away with Nitroglycerin. The patient’s story that they occur when he becomes nervous and is combined with other signs of dystonia will also help to make a diagnosis.
- appetite disorders;
nausea, vomiting “from excitement”, without connection with food;
At the same time, the person does not have diseases of the gastrointestinal tract that could provoke the described symptoms. Often, along with vascular symptoms, dyskinesia (decreased tone) of the biliary tract is observed.
All types of vegetative-vascular dystonia are characterized by sudden attacks - vegetative crises. Their manifestations depend on the type of VSD:
- During a crisis of dystonia of the hypertensive type, sudden excitement occurs, the heart rate increases, blood pressure rises, the legs become cold, and chills occur.
- The hypotonic type of VSD causes weakness, shortness of breath, nausea, and sweating.
- The cardiac type is manifested by sharp, stabbing pain in the heart, tachycardia, and shortness of breath. Nitroglycerin does not relieve pain.
In most cases, these symptoms are not enough to make a diagnosis of VSD. However, she will tell the doctor what other examinations are needed to confirm or refute the assumption of autonomic vascular dystonia.
Features in children
Congenital autonomic vascular dysfunction is diagnosed in babies who suffered hypoxia in the womb, in children with congenital malformations of the central nervous system and pathologies of internal organs. One of the risk factors for VSD in children is birth trauma, especially head trauma. Even if for many years they have no effect on the child’s health and development, they have a hidden effect on his cardiovascular system, and the schoolchild may develop vegetative dystonia.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Vascular dystonia often affects children who lack self-confidence and those boys and girls on whom their parents have placed a burden that is too heavy for them: additional classes in languages, sports, and music. When mental stress is combined with fatigue and lack of sleep, autonomic dystonia syndrome develops.
In addition to the same signs that are observed in adults, impaired thermoregulation is more common in children with VSD. During the day, the baby’s temperature is elevated, but never rises above 37–37.5 °C. At night she becomes normal. It differs from the temperature during a cold in that it can differ in the right and left armpits. Children with vegetative-vascular dystonia syndrome feel cold in a warm room or do not feel the cold.
Weight loss or weight gain in children, as in adults, indicates endocrine dysfunction; Boys and girls with VSD often develop acne. In adolescents, the timing of puberty is disrupted: it accelerates in girls and slows down in boys.
Diagnostics
The complaints of patients with vegetative vascular dystonia coincide with the symptoms of many diseases. Therefore, in addition to the initial examination (blood and urine tests, cardiogram, breathing tests), doctors conduct targeted examinations based on the “leading” syndrome in a particular patient with VSD, for example, cardiac. This helps to rule out serious diseases with similar symptoms. Thus, tests and a cardiogram within normal limits and cervical osteochondrosis may be the first indicators of the vegetative origin of symptoms.
It is easier for a doctor to establish a diagnosis for a patient who describes his ailments in detail. Find out where your head hurts (in the temples, in the back of the head, on one side or both), what kind of pain it is (pressing, pulsating, “shooting”). Are there any other unpleasant sensations: dizziness, nausea, double vision, fog in the eyes? When you feel bad, is the deterioration in your health associated with overwork at work, responsible situations, anxiety, fear?
- If you complain of chest pain, in addition to heart disease, it is recommended to check the patient for rheumatism, the cardiac symptoms of which resemble the cardiac type of vegetative-vascular dystonia.
- If you have high blood pressure and symptoms of VSD, you are examined for primary hypertension (it is inherent in diabetes and adrenal dysfunction).
- In case of fever, find out whether there are colds, flu, inflammation, tumors (the tumor process is often accompanied by an increase in temperature).
- Episodes of suffocation may indicate bronchial asthma or a tendency to allergies. The patient is given breathing tests and allergy tests.
If examination and tests do not show organic disorders and diseases, a diagnosis of “vegetative dystonia syndrome” is made. The patient is referred to a psychoneurologist and doctors of other specialties who find out the cause of autonomic dysfunction.
Treatment and prevention
VSD itself rarely causes complications and does not cause any particular harm to health. But due to autonomic vascular dysfunction, organs and tissues lack oxygen, and any chronic diseases are more severe. Against the background of VSD, myocardial ischemia, bronchial asthma or hypertension can develop over time.
But even if it manifests itself in a mild form, vegetative-vascular dystonia prevents a person from working and studying, makes him feel “inferior”, and causes self-doubt. A person may have intestinal failure at the wrong moment, he is embarrassed by his wet hands, or a “disease that does not exist” prevents him from getting enough sleep before an important event.
It is very difficult to reduce the symptoms of VSD if the cause of autonomic vascular dysfunction is not eliminated. However, even severe types of autonomic vascular dystonia are treated when doctors know what causes it and the patient follows all the recommendations of doctors. In most cases, non-drug methods are sufficient; in severe cases, drug therapy is used.
Non-drug treatment
Since VSD strongly depends on a person’s mental state, for successful treatment, doctors first of all advise changing the environment. It is impossible to treat a painful condition if the person continues to be affected by its causes: stress at work, overwork, and so on. Recommendations for the treatment of VSD may vary, but they always include:
- Establishing a daily routine and physical activity. Of course, you shouldn’t start playing sports, but exercise, jogging before work, swimming or cycling will make you feel better. Walking in the fresh air will also be beneficial. People diagnosed with vegetative-vascular dystonia should not be overtired; they need to learn to alternate work with rest, and sleep at least eight hours at night. Children are limited in their time watching TV or using the computer.
- Psychotherapy. Modern people, especially city dwellers, do not know how to relax, so they more often suffer from VSD. Music and positive emotions help calm your nerves (after all, it’s not without reason that they say that laughter lengthens life!). In some clinics, patients are offered to learn breathing exercises, meditation, or master a relaxation technique that they like (qigong, yoga, etc.). Treatment of VSD will be more successful if you quit smoking and do not get involved in alcohol. In severe cases of vegetative-vascular dystonia, hypnosis sessions are prescribed.
Physiotherapy. This includes electrophoresis, massage of the collar area, and if there are no contraindications, acupuncture, radon baths and therapeutic showers, for example, Charcot's shower.
An important part of treating autonomic disorder is diet. The diet should be complete and include foods high in potassium and magnesium - microelements for the health of the heart and blood vessels. They are found in buckwheat, oatmeal, soybeans and beans, peas, apricots and dried apricots, rose hips, nuts, and eggplants.
Hypertensive patients should reduce salt intake, exclude fried, smoked, fatty and floury foods; limit marinades and pickles, drink less coffee and tea. This diet will also help them lose weight, which is important for VSD. Hypotonic patients benefit from seafood rich in iodine; dairy products high in calcium (cheese and cottage cheese) and products for vascular tone: tea and (in moderation!) coffee.
Sometimes non-drug methods are enough to improve the functioning of the autonomic system and reduce or eliminate the symptoms of autonomic vascular dystonia. But if they don't help, you will be prescribed medications.
Medicinal and herbal medicine
The goal of treating VSD is to at least reduce its manifestations and, at maximum, to restore the function of the autonomic system. Several groups of drugs are used for this:
- Nootropics (improves cerebral circulation and metabolism in nerve cells): Piracetam, Pantogam®, Cavinton®, Cerebrolysin®.
- Vitamin and mineral complexes. For the treatment of vegetative vascular dystonia, B vitamins, potassium and magnesium are important.
- Antispasmodics. For headaches due to VSD, adults are prescribed Analgin, Tempalgin or Spazmalgon; for abdominal cramps and for children with any spasmodic pain - Papaverine and No-shpu.
- Antipsychotics. With increased anxiety, a tendency to panic, neurasthenia and other similar conditions, people with autonomic vascular dysfunction are recommended to take antidepressants, tranquilizers, psychostimulants, and antipsychotics. Depending on the severity and cause, Bellataminal®, Amitriptyline, Rexetine® and other drugs are prescribed.
Even a doctor without examination will not always distinguish autonomic dysfunction syndrome from a serious disease, so do not diagnose yourself with “autonomic vascular dystonia.” And even more so, do not buy drugs for treatment “from a commercial” or on the advice of friends and acquaintances. First of all, this applies to antipsychotics: with long-term use, addiction develops to them, and in addition to VSD, you will develop drug dependence.
Herbal remedies for mild forms of vegetative-vascular dystonia are used separately, and for severe ones - together with medications. As with other medications, you should not take tinctures and herbal preparations without consulting your doctor: herbs and tinctures can be just as potent as pills or injections and have contraindications in the same way.
In case of loss of strength, lethargy, fatigue, people with symptoms of vegetative-vascular dystonia will come to the aid of natural psychostimulants: ginseng, eleutherococcus, zamanikha, leuzea, aralia. They should not be taken in the afternoon, otherwise you will pay for the morning vigor with insomnia. For neurasthenia and anxiety, teas based on valerian root, motherwort, mint, hops, sage and lemon balm are recommended; tinctures of valerian, peony root, motherwort. Alcohol tinctures are prescribed from the age of 16; soothing tea can be given even to small children with VSD.
Symptoms
Symptoms of a brain contusion depend entirely on the severity of the injury.
Main signs of injury:
- Chronic headaches.
- Partial or complete loss of consciousness.
- Attacks of nausea and vomiting that do not bring relief.
- Impaired coordination of movements.
- Memory problems in the form of retrograde amnesia.
- Impaired speech, vision, hearing, and swallowing reflex.
- Blood pressure is increased, pulse rate is slow.
- Involuntary bowel and bladder emptying.
- Breathing is weak.
- The pupils change in size.
- Strabismus and nystagmus appear.
- Blood is leaking from the ears and nose.
- Paralysis.
- Coma.
Important! With moderate to severe brain contusion, body temperature rises significantly and meningeal symptoms appear. Brain contusion with compression causes bradycardia, paresis, and edema. Compression is one of the least common but more dangerous brain injuries.
First aid
First aid for a brain injury is to:
- Carefully lay the victim down and ensure free access of air. This is necessary because with TBI, respiratory functions are primarily impaired.
- Call a medical team, explaining to the dispatcher the reason for the call.
- First aid also includes stopping bleeding and clearing the airways of blood or vomit.
- Before the ambulance arrives, it is necessary to ensure that the patient is not given water, food or medicine.
- When the “emergency” arrives, tell the doctors about the cause of the injury and the measures taken.
Important! For brain injury, treatment should only occur after a diagnosis has been made.
Diagnostics
After being admitted to a medical clinic with brain injuries, the victim is sent for a detailed examination. This is necessary in order to make an accurate diagnosis, which will help draw up a treatment plan and avoid negative consequences. Diagnostic methods include the following:
- Study of the state of the cardiovascular system.
- Respiratory system check
- Examination of the victim.
- Neurological examination using the Glasgow Coma Scale.
- CT scan. This examination allows you to determine a skull fracture and identify the presence of hemorrhage or hematoma in the brain.
- MRI. This method of examination for TBI is rarely used, since in this case lengthy preparation is required.
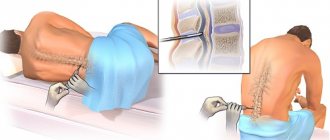
In case of complex injuries, additional research methods may be needed - lumbar puncture, electroencephalography.
Treatment
Treatment of a brain contusion with mild stages should be carried out only in a hospital, and a severe brain contusion should be treated in intensive care with subsequent transfer to a hospital.
Basically, treatment for contusion is carried out conservatively, but there have been cases when patients with such a diagnosis required surgical treatment. The main criterion determining the treatment method is the severity of the injury.
The first thing that needs to be done is to restore and maintain important functions of the body - breathing and blood circulation. To do this, the patient is given oxygen inhalation and, if necessary, artificial ventilation of the lungs.
Since almost any brain injury entails a decrease in circulating blood volume, it is necessary to replenish it with the help of intravenous administration of colloids and crystalloids.
To lower intracranial pressure, you should raise the head end of the bed, reduce high body temperature, and maintain the level of oxygen in the blood. Among medications, decongestants are used, followed by the administration of diuretins.
Neuroprotective therapy is carried out to maintain brain tissue with nutrients that protect brain cells from subsequent disorders resulting from circulatory disorders and cerebral edema.
In case of epileptic seizures, the doctor prescribes anticonvulsants.
Surgery may be needed in the following cases:
- If during conservative therapy the symptoms of cerebral edema increase, and dislocation of brain structures occurs with displacement. Such a violation is dangerous to the patient's life.
- If the bruise area has increased several times and represents crushed brain tissue.
- If intracranial pressure cannot be corrected with medications, and neurological symptoms increase.
Surgical treatment consists of craniotomy and resection of the area of destroyed brain tissue, if there is a prerequisite for this
An important role in the treatment and recovery after a concussion is played by full patient care and prevention of bedsores. In case of threat of bacterial complications, antibacterial therapy is carried out.
Application of therapeutic actions
In view of the seriousness of this injury and its consequences for human health, modern medicine is constantly searching for new advanced treatment methods and improving existing technologies for eliminating the consequences and normalizing the condition of patients with this diagnosis.
As for modern diagnostic methods, due to the inability to collect any data about the injury from the patients themselves, the most reliable method in this situation is computed tomography. After a general examination of the patient and excluding the need to treat other associated injuries, such as a bruised nose, the doctor can finally make a diagnosis and prescribe treatment appropriate to the situation.
The very first step is hospitalization of the victim. Bed rest for the first degree of severity is indicated for 1 week and this is the minimum period for this injury. With the second, this period increases to 2 weeks, and with the third – at least 2 weeks. The maximum period in severe cases can be set by the attending physician individually, depending on the dynamics of the patient’s condition and the recovery of vital signs.
In case of this injury, especially its severe stage, even before admission to the hospital, the victims are given resuscitation measures by means and by emergency teams. These activities provide the following assistance:
- removal of mucus, vomit and blood accumulated in the upper respiratory tract;
- tracheal intubation or tracheostomy placement;
- sometimes artificial ventilation is performed;
- elimination of the hematoma by suctioning blood from the subarachnoid space through a specially made puncture.
Rehabilitation
Any rehabilitation largely depends on the severity of the injury, but there are general recommendations for people who have suffered a brain contusion. Compliance with them will help avoid negative complications. These include the following actions:
- Care and attention of loved ones of the injured person.
- Eliminate toxic effects on the human body. To do this, it is necessary to carry out wet cleaning using humidifiers and air purification devices.
- Avoid foods that stimulate the nervous system - coffee, alcohol, strong tea.
- Ensure proper rest and eliminate stressful situations. Reduce time in front of the TV and computer to a minimum.
TBI is often accompanied by adverse complications, including death. Therefore, in case of this damage, you should not neglect contacting a specialist, as this will help save life or prevent the development of dangerous consequences. The recovery period lasts several months, a year.
How is a concussion treated?
In modern conditions - weaning from the smartphone, since the most important aspect of therapy is rest. The brain needs to come to its senses, deal with the damaged neurons and pave new paths for nerve impulses. Scrolling through social networks, watching movies, reading books and playing “three candies in a row” do not contribute to this. Even listening to music and podcasts can overwhelm a traumatized brain.
It is vital for athletes to avoid strenuous play and play until recovery is complete to avoid serious long-term consequences.
Some days a person with a concussion will feel worse, some days better, and the temptation to immediately take care of the backlog must be overcome. Otherwise, recovery will take longer.
The return to study or work should be gradual, with a slow increase in load. This applies not only to working at a computer, but also to accompanying sensory stimuli - the flickering of fluorescent lamps, background noise, conversations, etc. It is necessary to eat well, give up alcohol and cigarettes, and, of course, sleep a lot.