From the first day of pregnancy until childbirth, it is extremely important for the expectant mother to monitor her health, listen to her body, monitor discharge from the genital tract, monitor her heartbeat and blood pressure. With insufficient interest in oneself, intrauterine hypoxia can begin - insufficient oxygen supply to the developing organism in the womb, leading to disastrous consequences: deviations associated with the development of the fetus, damage to the central nervous system, difficulties in the timely development of the body. Fetal hypoxia during childbirth occurs in 12-15% of cases, and this is quite common.
Degrees of hypoxia: acute and chronic
Our body cannot live without oxygen, so even a short oxygen deprivation leads to serious consequences. There are two types of hypoxia – acute and chronic.
What is the difference between them? A simple example: if a piece of food is blocked in the respiratory tract, this causes acute hypoxia. And if you live for months in a stuffy, poorly ventilated room, this causes chronic oxygen starvation.
Chronic hypoxia as a result of constant stuffiness is often the cause of malaise in adults - it leads to decreased immunity, deterioration in the quality of sleep, frequent headaches, constant fatigue and weakness.
Important! During pregnancy, prolonged stay in a stuffy room is dangerous precisely because of the risk of developing intrauterine fetal hypoxia. Therefore, doctors recommend being in the fresh air as often as possible, since they assume that all the windows in the apartment are closed and there is not enough fresh air.
The fruit is 100% dependent on the environment in which it is located. Therefore, expectant mothers need to avoid stuffiness, large crowds of people and regularly ventilate the apartment where they spend a lot of time. There is a myth that the room only needs to be ventilated for 15 minutes in the morning and evening. Ventilation should be constant, but this is not always possible due to the environment - dirt, noise, drafts, allergies.
Acute fetal hypoxia during pregnancy is the nightmare of any obstetrician. It can develop due to pathologies of intrauterine development (for example, placental abruption), or during childbirth - due to abnormalities in the birth act.
Signs
An intrauterine problem - that is, fetal hypoxia - manifests itself as follows. As soon as oxygen starvation begins, the fetus begins to move and generally behave restlessly. At the same time, the intensity of such activity will be noticeable, but you will not see that this is due to any physical activity.
It’s rare that mothers turn to doctors with such manifestations; they probably don’t think that these signs are so significant. On the contrary, they think that the child is growing up active and “will be a football player.”
However, without proper assistance from specialists, intrauterine fetal hypoxia that has just appeared begins to progress and enters the second stage. Characteristic features:
- the fetus, on the contrary, moves less actively;
- the strength and frequency of the “future football player’s” pushes are reduced.
If you notice that the fetus moves less often - on average, motor activity has decreased to 3 times per hour, this is a reason to urgently go to a specialist.
If there is a suspicion of oxygen starvation of the child, the baby’s heartbeat decreases to 160 beats per minute. There is also a noticeable muffling of heart sounds, a decrease in heart rate - up to 100 or 120 beats per minute.
Consequences: why is this intrauterine syndrome dangerous?
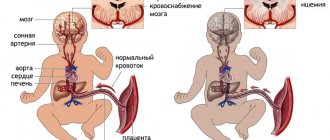
Until the moment the child is born, he does not have independent breathing. He breathes liquid with oxygen dissolved in it, which entered it through the placenta from the mother’s blood. Simply put, the child breathes the air that his mother breathes, and if there are problems with O2 delivery at any stage, a threat of fetal hypoxia is created.
When oxygen deficiency occurs, the child’s body begins to redistribute it so that first O2 enters vital organs (brain, heart and adrenal glands), and only then goes to the skin, kidneys, gastrointestinal tract and lungs. Because of this, the first violations affect the development of those organs and systems that, during hypoxia, received oxygen according to the “residual principle.”
Problems with chronic hypoxia:
- difficulty in adapting to stimuli in a newborn (convulsions, problems with appetite and breathing);
- risk of developing epilepsy;
- cardiovascular disorders;
- risk of kidney failure;
- enterocolitis, frequent regurgitation;
- secondary immunodeficiency;
What could be the consequences for a child in the future due to acute hypoxia? In this case, the central nervous system is primarily affected. Acute oxygen deficiency in the fetus can cause the following disorders:
- mental retardation;
- DIC syndrome;
- neurological disorders;
- cerebral edema;
- pulmonary hypertension;
- necrosis and ischemia of various organs.
Why does oxygen starvation of the fetus develop during pregnancy?
Intrauterine hypoxia is not identified as a separate condition, but indicates a state of lack of oxygen in the baby. It can be caused by pathological changes in the placenta, the body of the child or the mother.
Disturbance of uteroplacental blood flow
The reasons listed below lead to the development of disorders that disrupt the normal functioning of the mother-placenta-fetus system.
- Arterial hypertension, preeclampsia or eclampsia (late toxicosis or gestosis). These serious conditions complicate pregnancy in the second and third trimester. The expectant mother's blood pressure increases, all blood vessels narrow, and small blood clots form in their lumen. As a result, the functioning of all systems and organs suffers. Similar processes occur in the vessels of the placenta, as a result of which it cannot cope with its functions.
- Placenta previa (violation of its attachment). Normally, it is located in the area of the body or fundus of the uterus, along its posterior wall, with a transition to the lateral surfaces - the place of best blood supply. In case of presentation or low position, the placenta is attached to the lower parts of the uterus, partially or completely blocking the entrance to it. At the same time, it is less well supplied with blood, and the fetus accordingly receives less oxygen and nutrients.
- Anomalies of umbilical cord development : torsion or malposition of blood vessels, disruption of their attachment to the placenta, true umbilical cord knot, long or short umbilical cord, entanglement around the body or limbs, cyst or tumor. During the entire pregnancy, the anomaly may not manifest itself in any way, but during childbirth, with additional stress, the umbilical cord is often compressed, tightened or falls out.
- Abnormality of the placenta (irregular shape, underdevelopment, additional lobules, etc.). In this case, its vessels are located incorrectly and/or there is their underdevelopment.
- Placental infarction is the death of its area with cessation of blood circulation in it.
- Premature aging of the placenta or post-term pregnancy - the placenta gradually dies and loses its functions.
Maternal diseases
- Anemia. Normally, iron is part of red blood cells (erythrocytes) and is involved in the delivery of oxygen to tissues. With anemia, there is a deficiency of it in the blood of the expectant mother and in the placenta, thereby leading to a disruption in the supply of oxygen to the fetus.
- Hormonal changes. With diabetes and malfunctions of the thyroid gland, metabolic disorders occur, which lead to a decrease in elasticity and thickening of the walls of the blood vessels of the placenta. As a result, the amount of oxygen-rich arterial blood reaching the fetus is reduced.
- Pathologies of the cardiovascular system : congenital or acquired malformations of the heart and large vessels, endocarditis (inflammation of the inner lining of the heart) and myocarditis (inflammation of the heart muscle), thrombophlebitis (inflammation of the veins) and varicose veins, increased blood pressure and others. With all these diseases, hemodynamics are often disrupted, the strength of heart contractions decreases, as a result of which blood flow to the uterus decreases.
- Respiratory diseases : chronic obstructive pulmonary disease, bronchial asthma, etc. They lead to the development of respiratory failure, which causes hypoxia of the tissues and organs of the expectant mother and the fetus.
- Intrauterine infection. Various infectious diseases caused by viruses, bacteria or fungi (mycoplasmosis, chlamydia, ureaplasmosis, toxoplasmosis, cytomegalovirus, influenza, rubella, etc.). The placenta becomes infected with the development of local edema and inflammation, and the elasticity of its blood vessels is impaired. In addition, intoxication in a pregnant woman can lead to a decrease in blood volume and thickening, resulting in a decrease in blood flow to the fetus. Some viruses and microorganisms are able to penetrate the placental barrier and damage the baby's tissues. Because of this, the formation or development of its organs is often disrupted, which leads to the formation of congenital malformations or even intrauterine death of the fetus.
- Pathology of the uterus: endometriosis (with this disease, the cells of the inner layer of the uterine wall (endometrium) grow beyond its boundaries), structural anomalies (bicornuate or saddle-shaped uterus, the presence of a septum, its complete doubling). In these cases, the placenta may attach to an area that is less well supplied with blood. In addition, the walls of the uterus become overstretched as the fetus grows, which leads to poor blood flow to the placenta and uterus.
- Poisoning or intoxication with alcohol, food, drugs, salts of heavy metals and other substances. Due to vomiting and diarrhea due to fluid loss, the blood thickens, the risk of blood clots increases, the blood vessels narrow, the temperature often rises, and the functioning of all organs and systems of the expectant mother is disrupted. Together, all these processes reduce blood flow to the uterus.
- Lack of sleep and psycho-emotional stress. In these conditions, the production of cortisol, a stress hormone, increases, which constricts blood vessels in the body of the expectant mother and in the placenta.
- Smoking promotes the formation of small blood clots in the vessels of the placenta, leading to disruption of blood flow in them.
Diseases and conditions of the fetus
- Anomalies of fetal development. The main part of them are congenital defects of the cardiovascular system: defect of the interventricular or interatrial septum, etc. With such pathologies, oxygen-enriched blood is poorly delivered to the tissues and organs of the fetus.
- Hemolytic disease of the fetus or newborn, in which there is incompatibility of the blood of the mother and fetus by group or Rh factor. The maternal immune system produces antibodies that cross the placenta and destroy the fetal red blood cells (erythrocytes), which are the main carriers of oxygen. Hemolytic disease is becoming a fairly common cause of intrauterine death.
- Features or complications of pregnancy.
- The threat of premature birth is often caused by impaired uteroplacental blood flow, maternal illness, stressful situations and other factors.
- Polyhydramnios or oligohydramnios mainly develop due to the same damaging factors.
- Increased uterine tone. Frequent and prolonged contraction of the muscles of this organ disrupts the flow of arterial blood to the fetus and causes stagnation of venous blood. As a result, metabolic processes between mother and fetus are disrupted.
- Multiple pregnancy. It is much more difficult for the mother's body and placenta to provide oxygen and essential nutrients to more than one fetus.
Main causes of hypoxia
There are four main causes of oxygen deficiency in the fetus: pathologies during pregnancy (for example, a conflict of Rh factors), illnesses of the mother, her bad habits and harmful environmental influences.
Pathologies during pregnancy . Hypoxia can be caused by postmaturity, entanglement with the umbilical cord, Rh conflict between the blood of mother and child, disturbances in the development of the umbilical cord and placenta, as well as pathologies of the fetus itself:
- intrauterine trauma;
- genetic abnormalities;
- developmental defects;
- hemolytic disease.
Mom's illnesses. The range of pathologies is very wide. One of the most common causes of hypoxia in this case is iron deficiency anemia.
Oxygen deficiency in the fetus can also result from:
- pyelonephritis;
- diabetes;
- diseases of the urinary and respiratory system;
- arterial hypertension;
- endocrine diseases;
- kidney diseases;
- diseases of the immune system.
Separately, it is worth mentioning the consequences of STIs (herpes, chlamydia, gonorrhea, mycoplasmosis, bacterial vaginosis, candidiasis and trichomoniasis), malnutrition, exhaustion and severe toxicosis in the mother.
Drinking alcohol and smoking. Why does the mother’s bad habits often result in fetal hypoxia? It’s all about the effect that the listed substances have on the inner surface of the alveoli of the lungs.
The alveoli have a special lubricant that ensures rapid delivery of oxygen to the blood. Alcohol vapor dilutes this lubricant, causing it to perform its function worse. This is just one of many other harmful effects of drinking alcohol during pregnancy.
Smoking also provokes the development of fetal hypoxia: the tars in tobacco smoke “clog” the alveoli, due to which lubrication is not produced in the required quantity. Smoking contributes to chronic hypoxia - both for the mother and the unborn child.
Environmental factors . Living in an ecologically unfavorable area, working in a hazardous industry, or in the presence of toxic substances in the air can also cause fetal hypoxia. A similar effect is caused by constant stay in rooms with poor ventilation, when the air contains too much carbon dioxide and too little oxygen.
Hypoxia in adults
Symptoms of hypoxia can occur not only in children, but also in adults, due to several reasons. Brain hypoxia develops due to the following factors:
- alcohol abuse;
- diseases of the cardiovascular system;
- severe pathologies of the respiratory system;
- carbon monoxide poisoning;
- as a consequence of serious surgical operations, etc.
Symptoms of oxygen deficiency are usually very pronounced. The patient has excessively increased excitability, which manifests itself in excessive energy, as well as signs such as:
- pallor or blueness of the epidermis;
- dizziness;
- nausea with vomiting;
- disappearance of reflexes;
- fainting;
- lack of functioning of internal systems and organs.
If the disease is chronic, the person may often feel sick in the morning, there is a decrease in performance, problems with speech and coordination, insomnia, etc.
Treatment of pathology should be carried out taking into account the reasons for which it arose. Doctors usually prescribe drugs that help restore normal functioning of the body, as well as promote intensive blood supply to the brain.
Often, adult patients develop myocardial hypoxia, or oxygen starvation of the heart muscle. The pathology occurs in an acute form, in which a person’s death can occur within a short period of time, and in a chronic form, when the disease develops over years.
Symptoms of oxygen starvation of the heart muscle:
- dyspnea;
- cardiopalmus;
- bluish tint of the skin;
- increased blood pressure;
- soreness in the heart area.
For effective treatment, it is necessary to eliminate the reasons why this pathology arose. To do this, you need to undergo a thorough comprehensive examination by a doctor (you can make an appointment at the very top of the page).
Artificial ventilation is usually used if the patient’s condition is serious, as well as blood transfusions, surgery, removal of toxins from the body, nutritional correction, etc.
How to identify hypoxia: symptoms and diagnosis
The modern level of medicine makes it possible to detect the presence of hypoxia “without delay”, at its earliest stage. There are a number of diagnostic methods for this:
- analysis of the biochemical composition of blood and hormones;
- listening to heart sounds with a stethoscope (detection of bradycardia and tachycardia);
- amnioscopy - analysis of amniotic fluid (a sign of hypoxia - the presence of meconium in its composition);
- ultrasonography;
- cardiotocography;
- ECG;
- Dopplerometry (study of the circulatory system, analysis of blood circulation in all its areas).
What should you pay attention to? Very strong, sharp kicks of the child that cause pain in the mother are an alarming sign. They may be a consequence of the development of hypoxia: these are reflex movements when the child experiences a lack of oxygen and wants to increase the incoming blood flow. The next symptom is the weakening and complete disappearance of tremors.
Important! The child’s activity norm is at least ten movements in 12 hours.
At what point should fetal activity be monitored? Doctors recommend monitoring your sensations, frequency and strength of kicks, starting from the 28th week of pregnancy. However, the risk of developing hypoxia exists from the first weeks, when it is impossible to monitor fetal activity.
If there are risk factors, then obstetrician-gynecologists recommend a set of measures to prevent oxygen deficiency. In addition, the mother needs to eat in a timely and nutritious manner, avoid lack of sleep and overwork, spend more time outdoors, and ensure regular ventilation in the room.
Assessment of the baby's condition using the Apgar scale . At birth, obstetricians evaluate the baby's condition using Apgar scores (named after the author of this technique, Virginia Apgar). This method analyzes five criteria - breathing, skin color, muscle tone, and heart rate. The child's condition is assessed twice - immediately after passing through the birth canal, and five minutes after that.
- Norm (from 8 to 10 points);
- The condition requires control (from 4 to 7 points). Moderate hypoxia is possible, compensation may be required, prognosis is favorable;
- Asphyxia ( from 0 to 3 points). Severe hypoxia, in which the child requires immediate resuscitation measures.
Low scores on this scale are not always given due to hypoxia, but in most cases it is oxygen deficiency that causes the difficult condition of the newborn.
Diagnostics
Long-term hypoxia is characterized by an increase in fetal motor activity, followed by weakening and maintaining it at a low level (about 3 noticeable movements per hour).[1]
Electrocardiography of the fetus makes it possible to identify disturbances in its cardiac activity that appear during hypoxia. Doppler sonography is used to study blood circulation. Amniotic fluid testing is also used.
| This section is not completed. You will help the project by correcting and expanding it. |
Treatment and prevention
Treatment in this case involves normalizing blood flow and a stable supply of oxygen to the blood. Doctors draw up a treatment plan based on the results of the examination and studies performed. In some cases, due to a threat to the life of the fetus, labor is induced using medications.
Hypoxia is a serious pathology, therefore only a doctor has the right to prescribe treatment. There are no ready-made, universal treatment regimens. There are only general recommendations for pregnant women - rest, bed rest, sleeping on your side.
Prevention. A woman is required, first of all, to be responsible in preparing for pregnancy - preliminary treatment of the reproductive organs, adherence to the rules of a healthy diet, complete abandonment of bad habits, and physical activity.
Frequent walks in the fresh air are an important part of prevention. It is also necessary to ensure that the ventilation in the house works properly and that effective air exchange is ensured. A practical solution would be to install compact supply ventilation with a set of filters - this way you can be sure that there will always be fresh, clean air in the house.
Condition monitoring. After conception, regular medical monitoring of the fetus's condition is necessary. Special attention should be paid to the prevention of anemia, as it is one of the common causes of hypoxia. If hypoxia has been diagnosed, the correct choice of birth method is necessary, as well as measures to prevent birth injuries.
Ventilator OXY as a means of preventing fetal hypoxia
Constant stuffiness is one of the causes of chronic hypoxia. Ventilation problems usually occur due to poorly functioning hoods and the installation of plastic windows that “seal” the room. In this case, supply ventilation will help “start” normal air exchange.
An example of such ventilation is the OXY ventilator - a compact device equipped with a fan and a set of filters. To install it, a channel is drilled in the outer wall onto which the ventilator is mounted.
The OXY ventilator is an effective means of preventing fetal hypoxia. Immediately after installation, it provides a round-the-clock supply of fresh air with the windows closed. With it, the expectant mother will not be disturbed by street noise, dirt and drafts. Thanks to the optimal oxygen content in the atmosphere of the room, you will be provided with complete, healthy sleep and rest, good health and mood.