According to standard medical calculations, pneumonia is an inflammatory-degenerative and, at the same time, the most common infectious disease of the lower respiratory tract. The second name of the pathology is pneumonia, which eloquently testifies to the essence of the pathogenic process.
However, it is not correct to say that only lung tissue is involved in the pathogenic process. The disease affects the structures of the bronchi and, in some cases, other anatomical structures of the lower respiratory tract. We are talking about a complex and multifaceted disease that is potentially fatal.
According to statistics, this disease occurs in every hundredth person. At least every third person knows first-hand what the disease described is. Treatment should begin immediately in all cases of pneumonia, so the prognosis will be the most favorable. What do you need to know about such a disease?
Causes of the disease
Causes of the disease
The reason for the development of the disease is always the same - the penetration and reproduction of an infectious agent, only the factors under which this occurs differ:
- untreated viral, bacterial or fungal diseases;
- complications after illnesses;
- damage to the respiratory system by various chemical reagents or vapors when inhaled;
- increased level of radiation with the addition of infection;
- allergies that affect the respiratory system;
- colds due to hypothermia;
- thermal burns of the lungs in a fire;
- penetration of a foreign body into the respiratory tract.
Any condition that creates a favorable environment for the proliferation of microbes and the development of pneumonia can be considered the cause of the disease. Therefore, doctors divide pneumonia into hospital-acquired and community-acquired forms.
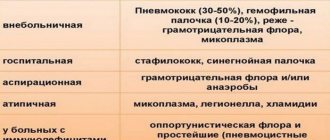
In addition, pneumonia is divided into types depending on the pathogen; the severity of the disease and the clinical picture also depend on this:
- streptococci are the most common pathogens; the disease is always severe and often causes death;
- mycobacteria – children and young people are often infected;
- chlamydia infection often occurs among the younger generation and middle-aged people, mainly in facilities equipped with artificial ventilation;
- Haemophilus influenzae usually affects the respiratory system of smokers and patients with chronic diseases of the lungs and bronchi;
- infection with enterobacteriaceae occurs rarely; as a rule, this occurs in patients with diabetes mellitus and those suffering from heart, kidney and liver diseases;
- staphylococcal pneumonia develops more often in older people who have had the flu;
- There are pneumonias caused by unknown or rare fungi and bacteria.
Causes of the disease
When making a diagnosis and prescribing treatment, it is necessary to take into account the etiology of pneumonia, the causative agent, medical history and the presence of third-party diseases. Pneumonia is often treated on an outpatient basis; in severe cases, the patient is hospitalized.
Who gets pneumonia more often and what is its danger?
Acute pneumonia of an infectious nature is called pneumonia. Of the people who apply with suspicions, I diagnose the disease in 5–10%; in the elderly and children, the frequency increases by 5%. The causative agents of the disease are:
- fungal and viral infections;
- mycoplasma;
- staphylococci and pneumococci;
- gram-negative microorganisms.
Among other things, the causes of inflammation without fever can be mechanical damage to the chest area, toxin poisoning and allergies. Special control should include:
- elderly people (over 65 years old);
- people with weakened immune systems;
- those who have been using immunosuppressants for a long time;
- people with respiratory diseases such as chronic obstructive pulmonary disease (COPD);
- those who use inhaled corticosteroids for long periods of time;
- smokers and alcohol abusers;
- registered at a tuberculosis dispensary with pulmonary tuberculosis;
- cancer patients;
- HIV-infected;
- those who underwent long-term, artificial ventilation;
- having swallowing disorders;
- people with kidney and heart diseases.
The release of toxins by certain microorganisms causes necrosis of lung tissue. Complications due to late treatment of the disease are life-threatening in nature, developing:
- pulmonary edema;
- purulent pleurisy;
- infectious-toxic shock;
- senile psychosis;
- sepsis;
- myocarditis.
Infection by airborne droplets occurs more often than through blood from foci of infection inside the body.
The first signs of pneumonia in adults
The first signs of pneumonia in adults
Previously, there was a fairly high mortality rate among patients with pneumonia. Today's medicine in the treatment of the disease gives a positive prognosis, subject to timely treatment. Therefore, it is necessary to know how the first signs of pneumonia :
- sudden increase in body temperature, chills;
- cough, the first days may be dry, then wet;
- runny nose;
- general malaise;
- hard breath.
It must be remembered that the incubation period for pneumonia is very short, only 2-3 days, then the disease begins to progress rapidly, and if treatment is not carried out on time, the patient may die. Therefore, it is important to contact a medical facility at the first signs of pneumonia.
The onset of the disease is always acute, but symptoms depend on age, immune system and individual characteristics of the body. The first signs of pneumonia can vary significantly from person to person. Some people may not have a fever or cough, especially if the person was previously treated with antibiotics for another illness.
Additional symptoms appear later in adult patients:
- purulent sputum begins to separate;
- chest pain;
- respiratory failure;
- cyanosis of the skin, especially on the face, this is due to oxygen starvation;
- tachycardia, low blood pressure.
One of the first signs of pneumonia is a cough of varying intensity. At first it may be infrequent and dry, then, if treatment has not been started, it becomes wet. Purulent greenish sputum appears.
Chest pain
If a person falls ill with ARVI, then his condition should improve in a week; if this does not happen, and the condition worsens, pneumonia can be suspected. In this case, the temperature is usually very high, only atypical pneumonia is accompanied by low-grade fever. It often happens that the patient begins to experience relief, but there is a sharp increase in temperature and the condition worsens. As a rule, antipyretic drugs have no effect. This is a signal for an urgent visit to the doctor.
Often the sick person feels pain in the chest when coughing or breathing; this alarming symptom indicates that the pleura is involved in the inflammatory process. The person becomes pale, has difficulty breathing, sweating increases, fever, delirium and other symptoms of intoxication of the body appear.
All these manifestations can be considered the first signs of pneumonia, which requires immediate examination. It should be noted that the first signs of pneumonia in women are no different from men, the only difference is that due to smoking, men are more likely to expose themselves to this disease than women.
How to identify asymptomatic pneumonia
Latent or asymptomatic pneumonia is characterized by a latent course without the manifestation of characteristic signs of inflammation. High body temperature, cough, or a sharp deterioration in general condition are absent in this case, but an experienced doctor differentiates latent pneumonia from other respiratory diseases.
In children at an early age with this course of the disease, the following is observed:
Loss of appetite is one of the signs of asymptomatic pneumonia in children
- a sharp decrease in appetite, up to complete refusal to eat;
- sleep disturbance;
- difficulty breathing;
- frequent coughing during the day and at night;
- general weakness, lethargy, moodiness;
- increased sweating;
- signs of asphyxia are a bluish tint to the lips and fingertips.
Based on these signs, the pediatrician recognizes the pathology of the lung tissue and refers the baby for additional examination and consultation with a pulmonologist.
Adult patients suffering from asymptomatic pneumonia report fatigue, tachycardia, and shortness of breath. Sleep and appetite are disturbed, nervousness occurs, and depression is possible. Sometimes an obsessive cough appears.
Sputum analysis
To make an accurate diagnosis, the doctor refers the patient to a blood and sputum test. In the biological fluids of a patient with pneumonia, an increased content of leukocytes is determined, which indicates a hidden inflammatory process. Based on the test results, the patient is referred for an X-ray examination. In the case of pneumonia, the image shows focal changes in the pattern of the lung in the form of a darkened area.
An x-ray is the basis for the final diagnosis, however, early age and pregnancy are contraindications for this research method.
First signs in children
First signs in children
With pneumonia, the first signs in children differ significantly from adults. Parents are advised to pay attention to the slightest changes in the child’s well-being. The first symptoms of pulmonary inflammatory processes can be considered:
- high, persistent temperature, usually above 390C, which is not reduced even by antipyretics;
- the child becomes lethargic, refuses to eat, and cries constantly;
- sweating increases;
- it is necessary to take into account that in infants the thermoregulation function is not yet fully regulated and the temperature may not be high;
- In babies, the rhythm of breathing is disturbed, it becomes frequent; if you pay attention to the child’s chest, one side will be delayed when breathing. In newborns, foam may be released from the nose or mouth; the child may puff out his cheeks due to shortness of breath;
- if atypical pneumonia develops, the symptoms may be similar to ARVI, but shortness of breath and fever are alarming factors;
- The cough usually develops, first coughing occurs, then a dry cough, turning into a wet one;
- infants may suffer from diarrhea and vomiting;
- The baby is capricious, refuses to breastfeed, cries often, and sleeps poorly.
If such symptoms occur, you should immediately call a doctor; with timely treatment, pneumonia usually has a positive prognosis and resolves without complications.
Possible consequences
When taking the medicine, strictly adhere to the instructions or follow the doctor's instructions! Inadequate and incorrect treatment of pneumonia in adults can lead to the development of serious complications, which include:
- acute respiratory failure;
- pleurisy;
- bronchial obstruction;
- septic shock;
- sepsis;
- lung collapse;
- cardiovascular failure.
More about the consequences
Forms of pneumonia
Forms of pneumonia
Pneumonia, based on the localization of the process and the severity of the disease, is divided into four forms, which have different first signs:
- An acute form of inflammation does not pose a danger if treated in a timely manner. Complications may occur if left untreated. It develops due to the penetration of an infectious agent, and may be a consequence of previous diseases. The first sign is high fever and cough.
- A chronic form of pneumonia, the causative agent of which is constantly present in the tissues and mucous membranes of the respiratory tract. This form of the disease has phases of exacerbation and remission, develops in rare cases, but is dangerous due to its protracted course and vague symptoms. The very first sign of this form of the disease is a weakened immune system, and if the patient is not treated in time, the inflammation may develop into pleurisy and result in death.
- Lobar pneumonia is characterized by damage to a larger lobe of the lung and is considered the most dangerous form. Treatment is carried out in a hospital setting under the supervision of doctors. This form of the disease is usually a continuation of acute or chronic forms of pneumonia and the first sign is difficulty breathing and high temperature.
- Focal pneumonia develops in a certain segment of the lungs and is not dangerous, but timely treatment is necessary, otherwise an acute or chronic form may develop with all the ensuing consequences.
In order to determine the form of pneumonia, it is necessary to conduct a series of blood tests and take a chest x-ray. To understand the seriousness of the disease, it is enough to pay attention to the first signs and additional symptoms; the brighter the clinical picture, the more dangerous pneumonia is for a person’s life.
Factors that provoke a decrease in the body's defenses
- Long-term and chronic stress, frequent psycho-emotional overload.
They cause active production of three hormones of the adrenal cortex: adrenaline, norepinephrine, cortisol. These substances provoke inhibition of the production of interferon and leukocytes, and change the composition of the blood. All this is fraught with a decrease in the activity of the immune system.
- Nutritional factors.
They are also nutritional factors. An incorrectly formulated diet leads to the fact that the body’s defense system is unable to give a worthy rebuff to bacteria and viruses. A lack of vitamin C is the most dangerous, since it is this substance that is responsible for the normal synthesis of interferon in the body.
- Weakened immunity due to frequent acute respiratory viral infections and other bacterial pathologies. They undermine the body's strength from the inside, causing a chronic decrease in the activity of the body's defense system.
- The presence of foci of chronic infection. Dangerous, including carious cavities, sore throat, affected joints.
- Tobacco smoking. Negatively affects the functioning of all systems and organs of the human body. Hot smoke, nicotine, harmful tars, all of this has an extremely negative effect on the body. In particular, the lungs suffer: the alveoli expand, fill with exudate, etc. The suppression of local and general immunity is determined.
- A history of complex chronic diseases. Simply put, they draw the immune system’s attention to themselves. To give a worthy response to viruses and bacteria, the defense system simply does not have the strength left.
- Abuse of ethyl alcohol. Drinking alcoholic beverages causes a decrease in immunity. The maximum permissible dose of alcohol per day is no more than 50 milliliters. In this case, the effect will be the opposite. Anything more is an excess, leading to all sorts of problems.
- Heart failure, arterial hypertension. These ailments can provoke a congestive form of pneumonia.
Despite all that has been said, there are other forms of pneumonia, provoked by traumatic damage to the chest, ionizing radiation (radiation), and allergic agents (the so-called secondary allergic pneumonia). To determine the nature of the process, you need to undergo a thorough diagnosis.
What to do at the first signs of pneumonia?
It is important to observe bed rest.
Knowing how the first signs of pneumonia appear, you can consult a doctor in time and begin treatment. Some forms of the disease are almost asymptomatic, which makes their diagnosis difficult. If we are talking about children or the elderly, therapy is required immediately when characteristic signs of pneumonia appear.
First of all, it is necessary to provide the patient with bed rest and rest. If your body temperature is very high, you need to take an antipyretic. You can give tea with lemon.
Antibacterial therapy should be prescribed by a doctor after examining sputum and identifying the pathogen. Antiviral therapy may be required in parallel.
At home, you can drink herbal tea, badger fat and honey. Under no circumstances should warming procedures be performed on the chest. At the first signs of pneumonia, you should immediately consult a doctor; the measures that will be aimed at treating the disease in the first 7-9 hours determine the duration and prognosis of treatment.
Causes and risk factors for developing the disease
The development of pneumonia is caused by the entry of pathogens into the human body with a weakened immune system. Thus, in addition to exposure to pathogenic bacteria, viruses or fungi, the main factor predisposing to the development of pneumonia is weakened immunity.
Learn more about the various causes of pneumonia
The most common causes of weakened defenses and risk factors for developing pneumonia:
- Old age - over the years, our body wears out, metabolic and regenerative processes slow down, and various diseases arise throughout life. All this leads to a decrease in the tension of the immune system, which is why old people are more likely to get pneumonia.
- Chronic diseases – we are talking about any diseases of a chronic nature, especially those that affect the respiratory system. The constant course of pathological processes in the body weakens it, reducing immunity.
- Bad habits - smoking, alcoholism, drug addiction - cause harm in a complex way, but in relation to pneumonia, smoking is considered the most serious threat.
- Constant stress and sleep disturbances – these two factors are inextricably linked. If a person sleeps little or restlessly, then becomes nervous during the day at work or under other circumstances, this also affects the state of immunity and health in general.
- Hypothermia - if pathogenic microbes have already entered the body, hypothermia, acting as stress, can trigger the onset of pneumonia.
There can be many similar factors, these include poor and unhealthy nutrition, systematic overwork, frequent sore throats and acute respiratory viral infections, unfavorable environmental conditions and much more. In addition, the development of pneumonia occurs more often during the cold season, but this does not mean that it is impossible to get sick in the summer.
Expert opinion
Anna Sandalova
Pulmonologist, doctor of the highest category
Ask a Question
The routes of infection by pneumonia pathogens are different. The main risks are the airborne route of infection, microaspiration and hematogenous route.
More about etiology and pathogenesis
Complications caused by pneumonia
Complications from pneumonia are very dangerous.
Inflammatory processes in the respiratory system can lead to serious complications. This is due to the fact that blood washes the lungs and can spread the infection throughout the body, thereby provoking:
- blood poisoning, sepsis;
- inflammation of the brain, meningitis;
- inflammation of the heart muscle, endocarditis, pericarditis.
If pneumonia develops in an elderly person after surgical treatment, this poses a double threat. Inflammation of the lungs during pregnancy can provoke infection of the fetus with staphylococcus or pneumococcus, which will lead to miscarriage or premature birth. If a pregnant woman has breathing problems, she should immediately contact the clinic.
You cannot self-medicate; pneumonia cannot be cured using traditional methods. Treatment at home can muffle the symptoms and give a misleading picture of improvement, while the inflammatory process will gradually increase.
Classification
There is an extensive and diverse classification of pneumonia. Pneumonia can be either a primary or secondary disease.
Separate types, types and forms of this pathology are also distinguished depending on the causative agent, the nature of the course, the extent of damage to the lung tissue, the localization of the process, and the degree of severity. However, first of all, it is worth highlighting two main classes of pneumonia:
- Community-acquired - this formulation refers to the most common type of pneumonia; it includes all cases of infection outside the walls of a hospital department. An adult can “catch” community-acquired pneumonia at home, on the street, in transport, or when communicating with a patient with pneumonia.
- Hospital (nosocomial) – such a disease is considered when the body is damaged by microbes in hospital conditions, taking into account a hospital stay of more than 72 hours. Pathogenic microorganisms are resistant to antibiotics used in the treatment of pathology.
Pneumonia in adults is classified according to the type of pathogen. As mentioned earlier, the following types of pneumonia are distinguished:
- bacterial;
- viral;
- fungal;
- mixed;
- non-infectious.
If we classify the pathological process depending on the location of the lung lesion, pneumonia is divided into the following subtypes:
- Unilateral or bilateral - as the name implies, the inflammatory process is localized in one or both lungs.
- Lobar - inflammation can be found in both one and two lungs, and an entire lobe of the organ is affected.
- Segmental – we are talking about damage to one or more segments of the lung.
- Total - in most cases, the pathology covers one lung completely; much less often, both halves of the respiratory organ are affected.
Depending on how the disease progresses, pneumonia is divided into acute, protracted and chronic.
In addition, there are three degrees of severity of pneumonia:
- light form;
- medium-heavy;
- heavy.
In the presence or absence of complications, pneumonia is characterized as complicated or uncomplicated.
More details about these and other types in another article.
Treatment
Treatment is usually carried out with medications and antiviral drugs.
Treatment should be comprehensive, including various measures. First of all, this is drug therapy:
- antibiotics to combat the causative agent of the disease, if they are used for more than a week, it is advisable to replace them with another drug in order to avoid the development of bacterial resistance to the drug;
- if necessary, antiviral or antifungal agents are prescribed;
- anti-inflammatory drugs, antipyretics (used at temperatures above 380C);
- mucolytic and bronchodilator agents for thinning sputum and removing it from the respiratory tract, the use of these agents is mandatory, accumulated sputum can cause inflammation in a new circle;
- Doctors often prescribe inhalations using essential oils of eucalyptus, pine and cedar;
- to eliminate toxins, take antihistamines and blood cleansers;
- At the same time, it is necessary to strengthen the immune system;
- in cases where complications concern the heart and blood vessels, cardiac medications are prescribed.
Treatment cannot be stopped on your own; in the absence of symptoms, the inflammatory process can continue and worsen over time, only in a severe form. During the recovery period, it is recommended to perform breathing exercises, monitor your diet and take walks in the fresh air.
How does the disease arise and develop?
The main ways microbes enter the lungs are:
- aspiration of the contents of the oral cavity and pharynx;
- inhalation of air containing germs.
Less commonly, the infection spreads through the blood vessels from other foci of infection (for example, with endocarditis) or enters directly into the lung tissue when the chest is injured or abscesses of neighboring organs.
The most common route of entry of pathogens is from the mouth and pharynx during sleep. In healthy people, microorganisms are immediately eliminated by the cilia lining the bronchi, coughing, and are also killed by immune cells. If these protective mechanisms are disrupted, conditions are created for pathogens to “fix” themselves in the lungs. There they multiply and cause an inflammatory reaction, manifested by general and local symptoms. Thus, in order to get pneumonia, you do not have to come into contact with a sick person. The pathogens live on the skin and in the nasopharynx of the sick person and are activated when the body’s defenses are reduced.
Inhalation of microbial aerosol is observed less frequently. It has been described, for example, in Legionella pneumonia, the classic outbreak of which was caused by the microorganism entering a hotel air conditioning system.
The most common causative agent of community-acquired pneumonia is pneumococcus; a little less often it is caused by chlamydia, mycoplasma and legionella, as well as Haemophilus influenzae. A mixed infection is often determined.
Viruses, as a rule, are only a “conductor” for the bacterial flora, inhibiting those protective mechanisms that we discussed above. Therefore, the term “viral-bacterial pneumonia” is considered incorrect. Viruses, including the influenza virus, do not infect the alveoli, but the interstitial (intermediate) tissue of the lungs, and it is not recommended to call this process pneumonia.
Prevention
Prevention of pneumonia includes nonspecific and specific methods.
Specific methods of preventing the disease are vaccination with pneumococcal vaccine and influenza vaccination. It is suggested that these vaccinations be given to the following categories of the population who are at high risk of pneumonia and its complications:
- all people over 50 years of age;
- persons living in nursing homes;
- patients with chronic heart or lung diseases, diabetes mellitus, kidney disease, immunodeficiency conditions, including HIV-infected people;
- women in the 2nd and 3rd trimesters of pregnancy;
- family members of the listed persons;
- medical workers.
Vaccination is carried out in October-November annually.
Nonspecific prevention of pneumonia:
- labor protection and compliance with hygiene standards at work;
- public health education;
- healthy lifestyle and giving up bad habits;
- treatment of caries, chronic tonsillitis, pustular skin diseases;
- timely treatment of acute viral infections and influenza.
What it is?
Pneumonia is an infectious lung disease that affects not only adults, but also children. In rare cases, such diagnoses are made even to newborn babies, but this happens extremely rarely and, as a rule, through the banal negligence of medical personnel during childbirth. If the fluid could not be completely pumped out of the lungs, then as a result the baby will begin an inflammatory process.
Even if the patient has already encountered pneumonia before, the disease may well appear again. When a patient’s lungs become infected again, an ideal environment for various pathogenic processes and their development may be formed in his body. Often the disease affects young people or children whose immune systems are not yet or are no longer sufficiently strengthened.
Of course, recurrent pneumonia can be avoided. But this can only be done in cases where the patient completely and completely follows the doctor’s recommendations. To do this you need to trust him completely. An important factor on the path to recovery is the mandatory follow-up treatment of the inflammatory process.
After restoring the immune system, the patient will be able to create a protective barrier that will act as a high fence for the sources of the disease. If you stop treatment halfway through, the likelihood of complications increases several times, in principle, the same as the cost of the treatment itself.
Symptoms of the disease
They are characterized not only by specific signs of damage, but also by general manifestations of intoxication. The main signs (symptoms) of the disease are:
- Cough – often wet, with copious sputum;
- shortness of breath with difficulty in both inhalation and exhalation;
- a significant increase in temperature (usually within 39-40C);
- pain in the chest area that occurs or gets worse when coughing;
- general symptoms (lethargy, irritability, sleep and appetite disturbances, sweating).
It is important to remember that the above symptoms are characteristic not only of pneumonia, but also of many other respiratory diseases. Therefore, only a specialist can make a final diagnosis.
How dangerous is this disease?
What is pneumonia and why is it dangerous? Pneumonia refers to inflammatory diseases of an infectious nature. It was officially recognized as a pathology leading to dangerous conditions with a fatal outcome.
More often, it occurs acutely, with severe clinical manifestations:
- Fever;
- Coughing;
- Sudden increase in body temperature;
- Dyspnea;
- Retrosternal pain;
- Weakness, drowsiness.
Pneumonia, according to medical statistics, affects the human body more often than other pathologies. It is also important that pneumonia is a complication of other diseases. People of any age and gender can face this problem.
The risk group includes young children and the elderly. Doctors use the term “pneumonia” to include a combination of several pathological conditions; what unites them is that each of them provokes inflammation of the tissues located in the lungs.
There are several types of pneumonia. Each type has its own symptoms and developmental characteristics. According to WHO, about 10% of pneumonia patients in the world die from the disease.
Doctors attribute this to age and the time it takes for the patient to seek help. Neglected treatment is the main cause of such complications.
Diagnostic methods
For the correct diagnosis of pneumonia, both the identification of signs and an objective examination, as well as instrumental and laboratory tests, are important.
Objective examination includes the following methods:
- Percussion - a dull percussion sound appears over the pathological focus, however, in the case of a small focus or its deep location, the sound may remain clear pulmonary;
- Auscultation - moist fine bubbling rales are most often heard.
When the first signs of the disease occur, it is necessary to conduct certain instrumental studies:
- X-ray of the chest organs in direct and lateral projections - the method allows you to visualize areas of compaction caused by inflammatory infiltration;
- computed tomography of the lungs - a diagnostic method is considered additional and is used when radiography results are questionable;
- Pulse oximetry - allows you to determine the level of oxygen in the blood in small tissue capillaries, which allows you to indirectly judge the functional state of the lungs.
Laboratory test results can provide important information, such as:
- Clinical blood test - the most characteristic sign is an increase in the level of leukocytes above 10*109. Also in favor of the presence of a focus of bacterial infection is an increase in ESR and an increase in the number of neutrophils with a possible shift in the leukocyte formula;
- biochemical blood test - although the results of this analysis do not reflect the presence of an infectious process as such, it allows you to diagnose general disorders in the functioning of organs, which is a risk factor for the development of pneumonia;
- blood test for antibodies - the test allows you to determine the presence in the blood of antibodies specific to the causative agents of atypical forms of pneumonia;
- microscopic and bacteriological analysis of sputum - the study is aimed at detecting the pathogen in sputum, determining its sensitivity to antibiotics, as well as analyzing the qualitative and quantitative composition of sputum.
Video on the topic
Pneumonia: signs, symptoms and treatment of pneumonia
Health TV. Pneumonia (pneumonia) is an inflammation of the lung tissue, usually of infectious origin, with predominant damage to the alveoli (the development of inflammatory exudation in them) and the interstitial tissue of the lung.
Pneumonia symptoms
Video channel “Catch the answer!”
The first symptom of pneumonia is an increase in temperature. In other words, the immune system tries to independently revive those body cells that are destroyed during the development of this disease. Accordingly, the body spends too much energy, which often leads to body temperature rising sharply and not falling for several days.
The second symptom of the inflammatory process is soreness. As a rule, it is also due to the fact that healthy lung cells are gradually destroyed, obeying the inflammatory process. Accordingly, a person begins to feel a regular tickle, which over time develops into a dry cough. It, in turn, can be characterized by regularity and severity. In other words, a person’s cough is more reminiscent of attacks, rather than the body’s usual reaction to, say, a cold.
The third symptom of pneumonia is the gradual appearance of sputum. This is due to the fact that the body gives up and the immune system completely loses its strength. In other words, the cough becomes wet, and the discharge becomes as abundant as possible. It is worth noting that getting rid of this disease is not easy and it is better to immediately consult a doctor rather than try to treat the lungs yourself.
When you need to urgently call an ambulance
Sometimes infected lung tissue can no longer supply the body with the amount of oxygen it needs. Because of this, the cardiovascular system and other vital organs, including the brain, are seriously affected and even fail. This type of pneumonia is called severe.
Urgently dial 103 or 112 if the following symptoms are added to a common cold:
- Breathing increased to 30 breaths per minute (one breath every 2 seconds or more).
- Systolic (top) pressure dropped below 90 mmHg. Art.
- Diastolic (bottom) pressure dropped below 60 mm Hg. Art.
- Confusion of consciousness appeared: the patient reacts sluggishly to the environment, answers questions slowly, and is poorly oriented in space.
If there are no threatening symptoms, but thoughts about pneumonia remain, check our checklist.
Pathogenetic and symptomatic therapy
If pneumonia is severe or has caused complications, the following drugs are used in addition to antibiotics:
- fresh frozen plasma and human immunoglobulin to restore immunity;
- heparin in combination with dextran to correct microcirculation disorders;
- albumin in case of a violation of the protein composition of the blood;
- saline sodium chloride solution, if necessary, potassium and magnesium salts for detoxification;
- oxygen using a nasal catheter, a mask, or even transfer to artificial ventilation;
- glucocorticoids in shock;
- vitamin C as an antioxidant that reduces cell damage;
- bronchodilators for proven bronchial obstruction: ipratropium bromide, salbutamol via nebulizer;
- mucolytics (ambroxol, acetylcysteine) orally or through a nebulizer.
The patient needs bed rest and then gentle rest, a sufficiently high-calorie diet that is easy to digest, and plenty of fluids. Breathing exercises should be started 2-3 days after body temperature normalizes. It can include both special exercises and basic ones, for example, inflating balloons 1-2 times a day.
During the period of resorption of the inflammatory focus, physiotherapy is prescribed:
- inductothermy;
- microwave therapy;
- electrophoresis of lidase, heparin, calcium chloride;
- thermal procedures (paraffin compresses).
After recovery, the patient is recommended to undergo sanatorium-resort treatment in local forest sanatoriums or places with a warm and humid climate, by the sea. It will be useful to undergo a course of reflexology, massage, and air ionization sessions.