Classification
High protein concentrations can also be observed in completely healthy people (physiological hyperproteinemia). This happens during pregnancy; blood is taken for analysis 30 minutes after a long stay in a horizontal position. According to etiopathogenesis, there are 2 types of hyperproteinemia:
- Hemoconcentration (false). This type develops as a result of thickening of the blood due to a decrease in its liquid part. Occurs with diarrhea, extensive burns, profuse sweating.
- Hypersynthetic (true). The increase in protein levels occurs due to increased protein production. Characteristic of infectious and non-infectious, acute and chronic inflammatory diseases, storage diseases, monoclonal gammopathies.
Hyperproteinemia can occur due to an increase in any protein fraction. Highlight:
- Hyperalbuminemia. Increase in albumin fraction. Occurs mainly with dehydration of the body.
- Hyperglobulinemia. Increased levels of alpha-beta-gammaglobulins and immunoglobulins in the blood. It is observed in infections, various autoimmune, chronic inflammatory diseases.
- Paraproteinemia. Characterized by the production of structurally abnormal proteins - macroglobulins, Bence-Jones protein. These proteins appear in Waldenstrom macroglobulinemia and multiple myeloma.
Causes of false hyperproteinemia
The development of this type of hyperproteinemia is associated with an increase in the relative protein content due to a significant decrease in the amount of fluid in the blood. In this case, there is no hyperproduction of protein. Typical for:
- acute intestinal infections (salmonellosis, dysentery), accompanied by uncontrollable vomiting and profuse diarrhea;
- extensive burns;
- prolonged hectic fever with profuse sweating.
The degree of hyperproteinemia is almost always moderate and quickly regresses after correction of water deficiency.
Hyperproteinemia
Causes of true hyperproteinemia
Infections
One of the most common causes of this condition. When an infectious agent (bacteria, viruses, parasites) enters the human body, phagocytosis occurs. In the process of phagocytosis of microorganisms, leukocytes begin to produce peptide factors and proinflammatory cytokines (interleukins, interferon, tumor necrosis factor).
These substances, together with the activation of the sympathoadrenal system, stimulate the formation of acute phase proteins in the liver (C-reactive protein, complement system proteins, seromucoids) and immunoglobulins (antibodies) in B-lymphocytes. An increase in protein concentration is observed approximately 5-6 hours after the onset of an acute or exacerbation of a chronic infectious disease and reaches a maximum after 48-72 hours.
The level of hyperproteinemia correlates with the activity of the pathological process, but rarely reaches large values (the degree is mostly moderate). Protein levels are higher in bacterial (pneumonia, pyelonephritis) and parasitic (malaria, trypanosomiasis) infections, as well as in generalized infections of any etiology (sepsis). The protein concentration normalizes quite quickly after inflammation subsides under the influence of specific therapy.
Inflammatory diseases
This group mainly includes pathologies of an autoimmune nature - rheumatoid arthritis, systemic connective tissue diseases (SLE, systemic scleroderma), inflammatory bowel diseases (Crohn's disease, ulcerative colitis). The exact pathogenetic mechanism of hyperproteinemia in chronic inflammatory autoimmune diseases is still unknown.
It is assumed that, under the influence of an unknown etiological factor, there is an increased production of inflammatory proteins (mainly CRP) and globulins (autoantibodies) as part of immune autoaggression. Hyperproteinemia appears only during the period of exacerbation of the disease, almost always minor or moderate. After a relapse, hyperproteinemia may persist for some time (from several days to several weeks).
Monoclonal gammopathies (paraproteinemias)
This group of diseases should be suspected in cases of high and long-lasting hyperproteinemia. These include multiple myeloma (Rustitsky-Culler myeloma), Waldenström macroglobulinemia, and light chain disease. The pathogenesis is based on the overproduction by tumor plasma cells of paraprotein proteins, abnormal in molecular structure and immunological properties: macroglobulins, monoclonal immunoglobulins, kappa or lambda light chains.
A distinctive feature of this type of hyperproteinemia is that it serves not only as a diagnostic marker, but also directly determines the severity of the disease. Due to the physical properties of paraproteins, they increase blood viscosity several times, which significantly impairs blood circulation in all organs and tissues, especially in the brain.
Hyperproteinemia in these diseases can lead to a coma (paraproteinemic coma). Protein concentration increases slowly over several years, paralleling tumor progression. Total protein levels increase by approximately 15-20%. Its reduction occurs only after removal of excess paarproteins from the systemic circulation using extracorporeal blood purification methods (plasmapheresis).
Rare causes
- Various forms of amyloidosis.
- Familial Mediterranean fever (periodic disease).
- Cryoglobulinemia.
Diagnostics
Hyperproteinemia itself is a rather rare phenomenon, so its detection requires special attention and differential diagnosis. If you receive a biochemical blood test with a high protein content, you must first consult a general practitioner. Anamnestic data are important: the patient’s age, previously diagnosed chronic diseases.
It is clarified what preceded the appearance of high levels of protein - profuse sweating, prolonged diarrhea, etc. Also, during a physical examination of the patient, the presence of certain symptoms is revealed, which can help in establishing the cause of deviations in tests, for example, fever during infections, joint pain with autoimmune rheumatological pathology, bone pain and repeated nosebleeds with paraproteinemia. To identify the cause of this laboratory phenomenon, the following examination is prescribed:
- Blood tests. In a general blood test, markers of inflammation are noted - an increase in CRP and erythrocyte sedimentation rate. These indicators are especially high with severe exacerbation of rheumatic diseases and paraproteinemia. Leukocytosis and anemia may be detected. In case of hyperproteinemia, the content of individual fractions – albumin, alpha and gamma globulins – must be determined.
- Urine tests. A general urine test often shows proteinuria. In multiple myeloma, Bence Jones protein is found in the urine.
- Protein electrophoresis. This study is carried out to obtain more accurate and complete information about the content of various protein fractions. Monoclonal gammopathies are characterized by a high concentration of M protein.
- Identification of the infectious agent. To identify an infectious agent, microbiological and virological studies are performed: bacterial culture of sputum, urine, blood on nutrient media; ELISA and PCR methods check for the presence of DNA of microorganisms or antibodies to them.
- Examination for autoimmune pathology. The titer of autoantibodies - rheumatic factor, antibodies to cyclic citrullinated peptide, DNA, etc. - will be determined. If inflammatory bowel disease is suspected, a fecal calprotectin test is informative.
- X-ray. In autoimmune arthropathy, a narrowing of the joint space and periarticular osteoporosis are visualized on the radiograph. Myeloma is characterized by multiple foci of osteolysis and osteodestruction, which are especially clearly visible in the skull area (“punching symptom”)
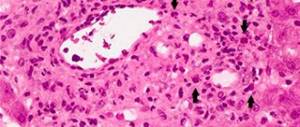
- Histological studies. Obtaining a bone marrow aspirate by trephine biopsy or sternal puncture is indicated only if the malignant nature of hyperproteinemia is suspected. The following changes can be detected: lymph or plasma cell infiltration, stromal fibrosis.
Hyperproteinemia is diagnosed based on the results of a biochemical blood test
Methods for diagnosing edema syndrome
To begin treatment for this pathological condition, it is first very important to determine the root cause of its occurrence. The patient goes to see a therapist, but in the future, consultation with specialized specialists may be required. First of all, the doctor examines the affected area. To identify the cause of the problem, studies such as:
- protein electrophoresis;
- determination of T3 and T4 content;
- radioimmunoassay;
- liver function tests;
- echocardiography;
- radioisotope angiography of the heart;
- CT scan;
- radiography;
- phlebography;
- Doppler ultrasound examination of veins;
- lymphangiography.
Consultation with an endocrinologist and cardiologist is especially important for patients who have developed chronic edema. Only after identifying the root cause of the pathology and assessing the general condition of the patient, a decision is made on the need for hospitalization and the choice of treatment.
Symptoms
Symptoms of hypoproteinemia are determined by the processes that are triggered in the body when there is a deficiency of protein in the blood:
- colloid-asthmatic blood pressure decreases, as a result of which fluid from the vascular bed passes into the surrounding tissues;
- the transfer of nutrients to the cells of internal organs slows down;
- antibody synthesis decreases.
As a result of these changes, the following pathological manifestations occur:
- Diffuse (over the entire body) or limited swelling is formed. In the second case, the legs most often swell.
- The body's resistance to infections decreases. Immune suppression is especially pronounced if hypoproteinemia is observed in children.
In severe cases, fluid may leak into various organs and tissues:
- into the pericardial sac (pericardium) – arrhythmia and pericarditis develop;
- into the pleural cavity - pleurisy or pneumonia occurs, accompanied by breathing disorders;
- into the peritoneum – ascites is observed.
Hypoproteinemia during pregnancy is one of the signs of late gestosis. As a rule, it is supplemented by:
- excessive weight gain;
- edema syndrome;
- the presence of protein in the urine;
- hypertension;
- hypertonicity of the uterus.
This condition is regarded as a severe complication of pregnancy. Without treatment, it can lead to thrombocytopenia and fetal dystrophy.
What is edema syndrome and how to treat it?
Edema syndrome is a pathological condition characterized by the accumulation of fluid in soft tissues and serous cavities. Such a violation leads to the emergence of a number of negative processes. To one degree or another, edema syndrome is familiar to many. Mild swelling may appear throughout the day and disappear after proper rest. However, often such a pathological condition indicates the development of extremely life-threatening diseases.
The severity of tissue saturation with excess fluid can vary significantly depending on the etiology of the problem. In some cases, this syndrome is so severe that the patient loses the opportunity to live a full life. For example, people suffering from severe forms of elephantiasis often cannot even get out of bed, since the increase in the volume of fluid accumulating in the lower and upper extremities makes it simply impossible to move them.
Treatment
The treatment strategy for hypoproteinemia depends on the characteristics of the patient's condition. Possible areas of therapy:
- low level of protein in the diet - dietary changes;
- liver diseases – hepatoprotectors, vitamins, glucose;
- kidney dysfunction - antibiotics, diuretics, anti-inflammatory drugs, hemodialysis;
- gastrointestinal diseases - probiotics, enzymes, etc.
In addition to treating the underlying disease, correction of hypoproteinemia is carried out with the help of anabolic steroids - drugs that enhance protein synthesis (Retabolil). To compensate for protein deficiency, solutions with albumin can be used - “Lactoprotein”, “Aminoven” and others.
If hypoproteinemia is complicated by fluid effusion into the pleura or peritoneum, aspiration is performed during laparocentesis or thoracentesis, respectively.
Hypoproteinemia
Hypoproteinemia is a pathologically caused sharp or gradual decrease in the level of total protein in the plasma component of the blood. For the formation of this pathological condition, it is enough only to disrupt the nutritional intake of protein-containing products into the body. In this case, a mild form of hypoproteinemic syndrome develops. If hypoproteinemia develops as a result of a malfunction in the body of the liver, which is the main regulator of protein metabolism, severe organic changes occur in the human body that require immediate drug correction.
We advise you to read: Hypertension with pulmonary edema
Prevention
Directions for preventing protein deficiency in the blood:
- balanced diet;
- timely treatment of liver, kidney and gastrointestinal diseases.
In order to prevent the development of hypoproteinemia, it is necessary:
- timely treatment of diseases contributing to its development;
- formation of an adequate diet with sufficient amounts of protein, minerals, and vitamins.
Education: higher education, 2004 (State Educational Institution of Higher Professional Education “Kursk State Medical University”), specialty “General Medicine”, qualification “Doctor”. 2008-2012 – postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty “pharmacology, clinical pharmacology”). 2014-2015 – professional retraining, specialty “Management in Education”, Federal State Budgetary Educational Institution of Higher Professional Education “KSU”.
The information is generalized and is provided for informational purposes. At the first signs of illness, consult a doctor. Self-medication is dangerous to health!
Treatment of hypoproteinemia
The nutritional type of hypoproteinemia is the most favorable in terms of the prognosis for the patient’s recovery, since therapeutic measures for this condition are limited to the correction of the patient’s eating behavior. Severe variants of hypoproteinemia require emergency drug correction in a hospital setting.
The only effective method of eliminating hypoproteinemia is the prescription of medications, a group of anabolic steroids, the action of which increases protein production (intramuscular administration of Retabolil in a dose of 5 mg once every three weeks). To improve the effectiveness of anabolic steroids, this therapy should be supplemented with the prescription of vitamin-containing preparations with complex action.
If there are signs of exudative pleurisy or ascites, laparocentesis and thoracentesis are used as symptomatic therapy.
Hypoproteinemia – which doctor will help? If you have or suspect the development of hypoproteinemia, you should immediately seek advice from doctors such as a hematologist, nephrologist and transfusiologist.
source
Classification
Low protein content can also be observed in healthy people (physiological hypoproteinemia), for example, in children under 3 months of age or women in the third trimester of pregnancy. Also, the concentration of total protein may be reduced during prolonged hospitalization in bedridden patients. Based on their origin, pathological hypoproteinemias are divided into:
1. Hemodilution (false). A decrease in protein levels occurs due to its “dilution” with excess liquid part of the blood (hypervolemia) due to water intoxication, oligo- or anuria, primary hyperaldosteronism, syndrome of inadequate secretion of antidiuretic hormone.
2. True. With this type, hypoproteinemia develops due to decreased protein synthesis, increased protein loss in the urine, or accelerated breakdown. In turn, they are divided into:
- Primary (hereditary, congenital). This group includes various genetic defects in the synthesis of major blood proteins - autosomal recessive analbuminemia, X-linked agammaglobulinemia (Bruton's disease), congenital immunodeficiencies.
- Secondary (acquired, symptomatic). The most common type of hypoproteinemia. They occur mainly in diseases of the liver, kidneys and starvation.
Based on the reduction in the content of a particular protein fraction, the following are distinguished:
- Hypoalbuminemia. The main type of hypoproteinemia occurs in many diseases and pathological conditions.
- Hypoglobulinemia. Low globulin levels are associated with immunodeficiencies.
Causes of hypoproteinemia
Health conditions that affect digestion or the absorption and utilization of proteins from food often cause hypoproteinemia.
Limiting food intake or following strict diets can also lead to protein deficiency in the body.
Malnutrition and starvation
Hypoproteinemia can be directly related to a person's diet, especially if the person does not eat enough high-calorie foods or avoids certain food groups.
Diet-related hypoproteinemia may occur in the following cases:
- If a person has insufficient income to buy food and does not consume enough calories from protein.
- During pregnancy, as women need much more protein than usual for fetal development. Those who are unable to take in enough calories from protein sources due to severe nausea and vomiting are at high risk of hypoproteinemia.
- The person has an eating disorder such as anorexia and bulimia nervosa. These conditions are often characterized by a diet that does not provide the person with sufficient amounts of protein.
- People who follow a strict diet, such as one that eliminates almost all sources of plant and animal protein, may be at risk for hypoproteinemia.
Liver diseases
The liver plays a key role in processing proteins in the body.
If the liver is not functioning fully, the body may not be able to get enough protein to perform its vital functions. This can occur in people with a variety of liver diseases, including liver failure, hepatitis A, hepatitis B, or cirrhosis.
Kidney problems
The kidneys help filter waste from the blood into the urine. When functioning properly, the kidneys allow protein to remain in the bloodstream.
However, when the kidneys are damaged or not functioning fully, they can leak protein into the urine.
This can occur in people who have hypertension (high blood pressure), diabetes, and certain kidney diseases (diabetic nephropathy, pyelonephritis, kidney failure, etc.). As a result, a person may experience a combination of hypoproteinemia and proteinuria (protein in the urine).
Celiac disease
Celiac disease is an autoimmune disease in which the immune system mistakenly attacks the body's cells in the small intestine.
This reaction occurs when a person eats foods that contain gluten, a protein found in wheat, rye and barley.
Autoimmune damage to the small intestine can result in decreased absorption of many nutrients, including protein.
Inflammatory bowel disease
Some forms of inflammatory bowel disease (IBD) cause inflammation in the small intestine. This is where the body breaks down many essential nutrients and absorbs them.
Damage to the small intestine can lead to various nutritional deficiencies, including hypoproteinemia.
A blood test can reveal whether a person has enough protein in their body.
Your doctor may perform a series of blood tests known as total protein, albumin, and albumin/globulin ratios. Albumin and globulin are two proteins produced by the liver.
This test can reveal whether total protein levels are low and whether albumin and globulin proteins are at optimal levels.
If these two proteins are out of balance, it could signal a medical problem, such as liver and kidney disease or autoimmune diseases.
Etiology of edematous syndrome
The appearance of this pathological condition is observed in a number of extremely dangerous diseases, which can cause the death of the patient in the shortest possible time. The characteristic manifestations of edematous syndrome depend on its etiology. By assessing the severity and localization of soft tissue saturation with fluid, in some cases doctors can determine the characteristics of existing problems in the body. Currently, there is general and local swelling. Each of them has its own characteristics. Local edema develops, as a rule, against the background of a violation of the outflow of fluid in a separate area or organ. The general variant is diagnosed if there is a violation of the outflow of fluid throughout the body. This form of edema usually indicates severe impairment. Depending on the etiological factor, edema syndrome can be:
- renal;
- cardiogenic;
- traumatic;
- hepatic;
- portal;
- lymphostatic;
- angioneurotic;
- venous;
- endocrine;
- neurogenic;
- membranogenic;
- iatrogenic;
- hypoproteinemic, etc.
Cardiogenic edema
Often edema develops precisely against the background of problems of the cardiovascular system.
Fluid accumulation in the lower extremities is often observed with chronic heart failure, as well as with persistently high blood pressure. In addition, often the accumulation of fluid in the soft tissues of the legs is the result of a malfunction of the venous valves. We advise you to read: What diseases cause swelling of the eyes
In this case, there is dilation of blood vessels due to stagnation. Damaged vein walls become permeable, so plasma begins to leak into the soft tissue, causing severe swelling. In addition, such a disorder can be caused by thrombosis in a separate section of the blood vessel.
Hepatic edema
The accumulation of fluid in the abdominal cavity, as well as swelling of the face, is often associated with impaired liver function. Ascites often indicates the development of a decompensated form of cirrhosis, as a result of which there is a disruption in the production of proteins that prevent the leakage of plasma from the blood vessels.
Lymphostatic edema
Lymphostatic edema has an extremely diverse nature. Body tissues can become saturated with fluid due to diseases such as recurrent erysipelas, lymphedema, filaria infection, elephantiasis, and limb injuries. The problem in this case lies in the obstruction of the lymphatic pathways and impaired fluid outflow.
Renal edema
Diseases such as systemic lupus erythematosus, amyloidosis, nephropathy of pregnancy, rheumatoid polyarthritis, diabetic glomerulosclerosis, lymphocytic leukemia, etc. can lead to impaired renal function, which can provoke the development of swelling of the soft tissues of the upper and lower extremities and face.
Endocrine edema
Endocrine variants include edema that appears against the background of myxedema. Dropsy of pregnancy and fatty edema syndrome may be included in this category.
Iatrogenic edema
Yandrogenic or drug-induced edema often develops during long-term treatment with large doses of hormonal drugs, including female sex hormones. Protein edema can be caused by taking certain medications. This disorder can be caused by taking anti-inflammatory antihypertensive drugs. In some cases, such a disorder can be caused by MAO inhibitors and Midantan.
Neurogenic edema
edema syndrome
Pathological conditions that often provoke neurogenic edema include Parhon's disease and Mege's trophedema. Such a disorder can be caused by a pathological condition such as reflex sympathetic dystrophy and damage to the hypothalamus of any etiology.
Membranogenic edema
Membranogenic edema develops against the background of intoxication of the body, as well as due to inflammatory and allergic reactions. Saturation of soft tissues with fluid can occur against the background of neurological diseases that are accompanied by paralysis.
Hypoproteinemic edema
Hypoproteinemic edema is associated with poor nutrition. Often, a similar problem is observed in girls who are so eager to lose weight that they refuse food containing components necessary for the body’s functioning, including protein. In this case, fluid accumulates in the areas of the knees and feet, and characteristic puffiness of the face appears.
Hunger or nutritional edema, accompanied by swelling of the eyelids and face, is often observed in adolescents trying to lose weight, since the body cannot cope with the existing loads against the background of an irrational diet.
Additional symptoms of deficiency include a red tongue, rapid weight loss, and cheiliosis. Protein-free edema can be the result of alcohol abuse, but this happens infrequently. Hypoproteinemia and fluid accumulation in soft tissues can be caused by severe vitamin deficiencies, intestinal diseases, impaired albumin synthesis and damage to the pancreas.
Recommended amount of protein
Eating a balanced diet that includes foods high in protein will allow most people to get the protein they need.
The recommended daily intake of protein is 0.8 g per kilogram of body weight per day.
To calculate how much protein a person needs each day, they can multiply their body weight in kg by 0.8.
At least 10% of your daily calories should come from protein. People who are very active, pregnant, or trying to build muscle may need more than these recommended amounts.
Treatment of edematous syndrome
The doctor’s actions are aimed at stabilizing the patient’s condition and eliminating the root cause of the problem.
For each specific disease that can cause swelling, there is its own treatment regimen.
At the same time, the doctor, as a rule, prescribes symptomatic therapy. In some cases, taking diuretics may be indicated. They can only be used on the recommendation of a specialist, since in some cases such drugs can cause a worsening of the condition.
Regardless of the cause of edema, it is recommended to reduce the daily dose of fluid intake. In severe cases, you need to drink no more than 1 liter of water per day. In the treatment of edema, changing the diet is of no small importance.
For most types of this pathological condition, it is recommended to reduce the daily dose of salt intake, and it is best to completely eliminate this component.
Salt promotes fluid retention in soft tissues. If swelling is associated with insufficient nutrition, a special diet is required, which includes not only protein, but also other substances necessary for the body. Proper comprehensive treatment of the primary disease in combination with therapy aimed at eliminating excess fluid from the body, in most cases, allows one to achieve good results.
source
Choosing the Right Proteins
Proteins are made up of amino acids, which are the building blocks of tissue. The body needs a large number of different amino acids to perform its various functions.
Animal proteins offer “complete” proteins. Examples include meat, fish, eggs and poultry. Soy, a plant protein, is also a source of complete protein.
These products contain all the essential amino acids needed by the body.
Plant proteins
Many plant proteins, including nuts, seeds and beans, contain only a few essential amino acids.
People following a vegetarian diet should make sure they get all the amino acids they need by eating a variety of healthy plant-based protein foods every day.
Animal proteins
Although animal proteins contain all essential amino acids in adequate proportions, many of them can adversely affect health. For example, red meat is often high in saturated fat and calories.
Fish may contain mercury or other contaminants, so children or pregnant women should avoid eating fish.
In general, eating moderate amounts of lean meat, poultry, and fish is the most effective way to consume a variety of proteins.
What's better?
Consuming a variety of proteins from animal and plant sources is usually the best way to avoid developing hypoproteinemia. Although most plant-based foods are not complete proteins, they do contain fiber, vitamins, minerals and antioxidants that help fight disease.
Instead of focusing on any one type of protein, eating a varied diet is the best way to be healthy.
In order to prevent the development of hypoproteinemia, it is necessary:
- timely treatment of diseases contributing to its development;
- formation of an adequate diet with sufficient amounts of protein, minerals, and vitamins.
Features of the course in pregnant women
Hypoproteinemia that develops during pregnancy may be one of the signs of late toxicosis (preeclampsia). Preeclampsia is a serious condition that increases the risk of perinatal mortality by approximately 5 times compared to the average sample of healthy pregnant women.
The main diagnostic criterion for hypoproteinemia is a decrease in protein concentration in the blood plasma to a level of less than 60 g/l, determined during a laboratory blood test.
The decrease in the concentration of total protein in the blood serum can also be relative and absolute.
Relative hypoproteinemia is usually associated with an increase in the volume of water in the bloodstream and is observed in the following conditions:
· water load (“water poisoning”);
· cessation of urine flow (anuria);
· decreased diuresis (oliguria);
· intravenous administration of large quantities of glucose solution to patients with impaired renal excretory function;
· increased secretion into the blood of the antidiuretic hormone of the hypothalamus - a hormone that promotes water retention in the body.
Absolute hypoproteinemia is usually associated with hypoalbuminemia. In this case, a decrease in the concentration of total protein in the blood serum occurs when:
· insufficient intake of protein into the body (starvation, malnutrition, narrowing of the esophagus, dysfunction of the gastrointestinal tract, for example, of an inflammatory nature - enteritis, enterocolitis, etc.);
· suppression of protein biosynthesis, which accompanies chronic inflammatory processes in the liver (hepatitis, liver cirrhosis, intoxication, liver atrophy);
· congenital disorders of the synthesis of certain blood proteins (analbuminemia, Wilson-Konovalov disease, other defectoproteinemias - much more rarely);
· increased breakdown of protein in the body (malignant neoplasms, extensive burns, hyperfunction of the thyroid gland (thyrotoxicosis), conditions after surgery, prolonged fever, injuries, long-term treatment with corticosteroids);
· increased protein loss (nephrotic syndrome, glomerulonephritis, diabetes mellitus, prolonged (chronic) diarrhea, bleeding);
· movement of protein into “third” spaces (ascites, pleurisy).
A decrease in the concentration of total protein in the blood serum is also observed under certain physiological conditions, for example, during prolonged physical activity, in women in the last months of pregnancy and during lactation.
Serum total protein levels may be affected by certain medications. For example, corticotropin, corticosteroids, miscleron, bromsulfalein and clofibrate help to increase the concentration of total protein in the serum, and pyrazinamide and estrogens help to reduce it.
The degree of total protein concentration can also be influenced by body position: when changing the horizontal position of the body to a vertical one, the concentration of total protein increases by approximately 10% within 30 minutes.
Clamping of blood vessels during blood collection and “hand work” can also lead to an increase in the concentration of total protein in the blood serum.
When interpreting the results of determining total protein in blood serum, it is necessary to take into account the value of hematocrit - in some cases this helps to distinguish a relative change in total protein from an absolute one, and, therefore, correctly make a diagnosis and determine treatment tactics.
WHEN FASTING: After 48 hours of fasting, the concentration of bilirubin in the blood may increase. Fasting for 72 hours reduces blood glucose concentrations in healthy people to 2.5 mmol/l, increases the concentration of triglycerides, free fatty acids without significant changes in cholesterol concentrations. Long-term fasting (2 - 4 weeks) can also affect a number of laboratory parameters. The concentration of total protein, cholesterol, triglycerides, urea, lipoproteins in the blood decreases; excretion of creatinine and uric acid by the kidneys in the urine increases. Prolonged fasting is closely associated with decreased energy expenditure. As a result, the concentration of thyroid hormones in the blood - total thyroxine and, to an even greater extent, triiodothyronine - decreases. Fasting also leads to increased levels of cortisol and dehydroepiandrosterone sulfate in serum samples. The increase in total protein in the blood serum can be relative and absolute.
Relative hyperproteinemia is associated with a decrease in water content in the vascular bed, which can be caused by the following conditions:
Hypoproteinemia
· A decrease in the concentration of total protein in the blood serum can also be relative and absolute.
Absolute hypoproteinemia is usually associated with hypoalbuminemia. In this case, a decrease in the concentration of total protein in the blood serum occurs when:
· insufficient intake of protein into the body (starvation, malnutrition, narrowing of the esophagus, dysfunction of the gastrointestinal tract, for example, of an inflammatory nature - enteritis, enterocolitis, etc.);
A conjugated system is a system in which there is an alternation of simple and multiple bonds, or in other words, a system in which multiple bonds are located at a distance of one single bond from each other. Such a chain of conjugated bonds is called a conjugation chain.
Conjugation is a redistribution (equalization) of electron density in a conjugated system, leading to stabilization of the molecule.
Conjugation is possible only if all the atoms taking part in this process are located in the same plane, i.e. the coplanarity condition must be satisfied.
3.2. Closed coupled systems. Aromaticity.
Conjugated systems with a closed conjugation chain are arenes, heterocyclic compounds and non-benzenoid aromatic structures. The simplest closed conjugated structures are arenes, the ancestor of which is benzene. Benzene has been known for a long time, but for a long time its structure was not proven, and only in 1865 A. Kekule proposed depicting the structure of the benzene molecule in the form of a regular hexagon with a system of alternating double and single bonds. It is customary to depict the formula of benzene in this way even now.
All carbon atoms in the benzene ring are in sp2 hybridization, all C–C bonds are equal to each other, have a length of 1.40 A° and occupy an intermediate position between single (1.54 A°) and double (1.33 A °) bonds. In this case, each carbon atom forms three s-bonds (one C–H bond and two C–C s-bonds) lying in the same plane, i.e. each carbon atom has one p-electron left, the orbitals of which, due to double overlap with each other, form a closed p-electron system that covers all carbon atoms. p-Electron density in such a system is distributed uniformly. The closed sextet of electrons is a bond that is different from other types and is often called aromatic. The electronic structure of the benzene molecule can be described using the resonance theory, according to which the benzene molecule is considered as a resonant hybrid of two limiting (boundary structures)
The concept of aromaticity arose more than a hundred years ago. Currently, aromatic systems include any flat closed cycles that meet the criteria of aromaticity.
1. The molecule has a flat cyclic structure.
2. All atoms in the cycle are in a state of sp2 hybridization (hence the s-skeleton is flat and all pz-orbitals are parallel.
3. In the molecule there is a delocalized p-electron system containing 4n + 2 p-electrons, where n = 0,1,2, is a natural series of numbers. This rule was called Hückel's rule, proposed in 1931 based on the molecular orbital method).
examples of biologically important aromatic compounds.
Didn't find what you were looking for? Use the search:
Symptomatic manifestations of edema syndrome
With the local manifestation of this pathological condition, up to 0.5 liters of water accumulates in a separate organ or area of the body. The general syndrome develops when the volume of required fluid in the body exceeds the norm by 2-4 liters. There is usually excess fluid in the extremities. This is accompanied by a number of symptoms, including:
- increase in the volume of a leg or arm;
- swelling of the skin;
- redness;
- decreased elasticity.
When palpating the swollen area, a pasty consistency of the skin is revealed. When pressed, a characteristic pit remains, which quickly disappears. With false edema, for example, formed against the background of myxedema, the limb is palpated with obvious difficulty, and the resulting hole persists for several minutes and sometimes hours. Against the background of severe edema, the skin may subsequently acquire a pale color, which is associated with squeezing of blood vessels and disruption of oxygen supply to tissues. In addition, with the unfavorable development of this syndrome, cracks may appear on the integument, through which liquid will constantly ooze.
With lymphatic edema, the skin becomes denser to the touch. When the leg is raised above the body position, the accumulated fluid decreases rather slowly. In severe cases, it does not disappear completely. Subsequently, the constant presence of protein in the tissues from the lymphatic fluid leads to the proliferation of collagen fibers and the development of elephantiasis.
With hypothyroidism, swelling is expressed in the shoulders, face and legs. With light pressure, there is no dimple in the tissue, and the skin acquires a yellowish tint, peels off and becomes dense.
Fatty edema is characterized by the appearance of severe symmetrical swelling on the legs. As a rule, this is a pathological condition in very obese women. At the same time, the accumulation of excess fluid in the soft tissues of the legs increases before menstruation. The area of edema remains soft, and upon palpation the characteristic pits remain. Signs of chronic venous stagnation may appear.
Forecast
Severe hypoproteinemia can lead to adverse consequences for the patient. A drop in albumin levels reduces the oncotic pressure of the blood plasma, which leads to sweating of fluid in the body cavity (abdominal, pleural, pericardial). Also, with a low protein concentration, the level of cholesterol in the blood increases, fatty degeneration of the liver occurs and the production of anti-infective proteins - immunoglobulins, proteins of the complement system - is disrupted. Therefore, detection of hypoproteinemia requires contacting a doctor.
Edema, definition, classification, pathogenesis, principles of edema therapy
Edema is an excessive accumulation of fluid in the intercellular space, as a result of impaired water exchange between blood and tissues.
We advise you to read: Swelling of the legs after phlebitis
The accumulation of fluid in body cavities is called dropsy .
There are dropsy of the abdominal cavity - ascites, pleural hydrothorax; pericardial – hydropericardium, etc.
The fluid that accumulates in these cavities is called transudate.
The main local factors for the development of edema:
a) an increase in hydrostatic pressure in the capillaries;
b) reduction of hydrostatic (mechanical) pressure in tissues;
c) decrease in plasma oncotic and/or osmotic pressure;
d) increase in oncotic pressure of perivascular fluid;
e) increase in capillary permeability;
Depending on which of the listed factors is leading in the pathogenesis of edema, they are divided into:
— hydrostatic (hemodynamic, mechanical, stagnant);
The clinical classification of edema is based on two principles:
In accordance with this, edema is divided into:
There are two groups of causes leading to the development of edema:
a) pathological conditions accompanied by Na delay:
- use of medications (corticosteroids, non-steroidal anti-inflammatory drugs)
b) hypoproteinemia – liver disease, nephrotic syndrome.
Causes and pathogenesis of hemodynamic edema.
The development of these edemas is associated with an increase in hydrostatic pressure in the capillaries due to impaired outflow of venous blood. A primary increase in A/D, as a rule, does not lead to edema.
Venous edema is impaired in a number of pathological conditions:
- venous hyperemia in the systemic or pulmonary circulation with circulatory failure;
- compression of the veins of the uterus during pregnancy.
The development of hemodynamic edema is also promoted by a decrease in tissue mechanical resistance due to tissue depletion of collagen (during inflammation); decreased pressure in cavities, for example, in the pleural cavity (which can lead to the development of hydrothorax.
Initially, hemodynamic edema occurs in the legs, and then “rises” to the upper body.
Causes of hypooncotic edema.
When the concentration of protein in the blood plasma decreases below 5%, the oncotic pressure in it becomes unable to retain water in the lumen of the capillary and it begins to leak into the tissue.
Hypoonkia is caused by:
b) disruption of proteins - the synthetic function of the liver;
c) significant protein losses due to enteropathies and extensive burns;
d) protein and complete fasting.
Sometimes this type of edema develops when the protein content is normal, but with severe dysproteinemia, when the albumin - globulin ratio is sharply reduced (normally 2:10).
The development of edema according to the oncotic mechanism is observed in tissue hyperonkia. The swelling in this case is local in nature.
This happens when:
— release of plasma proteins into tissues;
— release of cellular proteins during their alteration
- increasing the hydrophilicity of proteins in the intercellular space under the influence of H, Na, histamine, serotoin, thyroxine ions, and Ca deficiency.
Pathogenesis of membrogenic edema.
Membranogenic edema is associated with increased permeability of the vascular wall. Increased permeability of the vascular wall is caused by various neurogenic mechanisms, poisons, acidosis, increased temperature, as well as biologically active substances - histamine, bradykinin, serotonin.
Many of these reasons that increase capillary permeability suggest the participation of the membrane factor in the development of a wide variety of edema, but it is leading for inflammatory, allergic, toxic and angioedema. In this case, an increase in the permeability of the vascular wall leads to the release of a large amount of albumin into the intercellular fluid, and albumin effectively binds and retains fluid in the tissues.
Mechanisms of development of lymphogenous edema.
Lymphogenic edema is caused by a violation of lymph edema, which leads to the accumulation of protein-rich edematous fluid in the tissues.
The causes of obstructed lymph outflow can be congenital hypoplasia of lymphatic vessels, compression by scars, or compression by tumors and metastases.
Prolonged lymphatic edema leads to the accumulation of protein in the tissue, followed by the proliferation of collagen fibers and deformation of the organ - elephantiasis.
Pathogenesis of cardiac edema.
The mechanism of development of cardiac edema can be represented in the form of a diagram:
Decreased myocardial contractility
Decrease in blood volume and venous stagnation.
| outflow of blood through the venous system. | decreased renal blood flow | Irritation of volume receptors of the right atrium | Tissue hypoxia. |
| Activation of Renin – angiotensin-aldosterone mechanism. | Acidosis | ||
| Increased Na reabsorption | Increased permeability of local blood vessels. | ||
| Increase in P osm. | |||
| Increased ADH production | |||
| Water retention |
Nephrotic edema is associated with massive renal proteinuria, the development of hypoproteinemia, hypoonkia and the transition of a significant amount of fluid into the tissue. The resulting hypovolemia and decrease in BCC turns on renin-angiothesin, the aldosterone mechanism of Na retention, and the ADH mechanism of water retention is connected to this.
Pathogenesis of renal (nephrotic) edema.
This duality of mechanisms: hypoonkia on the one hand and H2O retention by the kidneys on the other, makes nephrotic edema very pronounced and persistent.
Pathogenesis of nephritic edema.
Nephritic edema occurs in kidney diseases with a predominant diffuse lesion of the glomerular apparatus of inflammatory and/or allergic origin in the renal cortex, causing increased secretion of renin by juxtaglomerular (JGA) cells, which, in turn, activates the renin-angiotensin-II-aldosterone-ADH system.
This leads to Na and water retention in the body. It is important that diffuse glomerulonephritis is characterized by damage to the membranes of microvessels and, above all, capillaries in many tissues and organs of the body. An increase in their permeability is an important mechanism for the development of nephritic edema. Gradual damage to the kidneys with glomerulonephritis leads to the same gradual increase in edema.
However, initially the liquid begins to come out of the vessels located in loose tissues. Therefore, nephrotic edema occurs first in the retina of the eyes, in the eyelid area, in the soft tissues of the face, neck, and then the torso.
Pathogenesis of hepatic edema.
In the occurrence of hepatic edema, the main role is played by damage to the liver parenchyma during hepatitis and cirrhosis of the liver.
In this case, the following mechanisms play an unconditional role:
a) – damaged hepotocytes do not synthesize a sufficient amount of albumin, a decrease in the concentration of which in the blood involves the hypo-oncotic pathway of fluid transfer into tissues;
b) – connective tissue developing during cirrhosis of the liver, squeezing blood vessels, causes portal stagnation, which impedes the outflow of blood from the abdominal organs, leading to the formation of ascites;
c) – a decrease in the volumetric fluid, due to its retention by the liver, leads, on the one hand, to a decrease in the activity of the volume receptors of the left atrium and an increase in the release of ADH, and on the other hand, to irritation of the volume receptors of the right atrium and an increase in the secretion of aldosterone;
d) – a liver with impaired blood flow (stagnant) poorly inactivates hormones, including aldosterone and ADH, which contribute to the retention of salts and water in the body.
Correction
To combat hyperproteinemia, it is necessary to treat the underlying disease against which it developed. Physiological hyperproteinemia does not require any intervention, since it is not a sign of disease or pathological condition. To correct hemoconcentration hyperproteinemia, it is enough to eliminate the fluid deficiency orally or by intravenous administration of crystalloid solutions. In other cases, the following activities are carried out:
- Anti-infective therapy. To eliminate the infectious pathogen, antibacterial (amoxicillin, levofloxacin), antiparasitic (hydroxychloroquine, mefloquine) are prescribed. For generalized bacterial infections (sepsis, endocarditis), a combination of at least 2 antibiotics from different groups is recommended.
- Anti-inflammatory therapy. In order to stop the inflammatory process and achieve remission of autoimmune diseases, glucocorticosteroids (prednisolone), immunosuppressants (cyclophosphamide, azathioprine), and 5-aminosalicylic acid derivatives (sulfasalazine) are used. In severe cases, they resort to genetically engineered biological drugs (monoclonal antibodies), such as rituximab.
- Chemotherapy. If monoconal gammopathy is confirmed, combinations of chemotherapeutic agents are used to slow down the proliferation of tumor cells - nucleoside analogues (fludarabine), alkylating drugs (chorambucil), tumor necrosis factor inhibitors.
- Bone marrow transplantation. For a certain group of patients with oncohematological diseases, hematopoietic cell transplantation is indicated in conjunction with chemotherapy courses.
- Plasmapheresis. Plasmapheresis is the only way to directly reduce serum protein levels. Removal of excess protein from the patient's body is prescribed only for myeloma and Waldenström's macroglobulinemia, accompanied by extremely high hyperproteinemia, causing a pronounced picture of GBS.
Hyperproteinemia in the vast majority of cases does not have any adverse consequences for the patient. The prognosis is determined by the disease that caused the development of this laboratory phenomenon. The exception is high protein levels in monoclonal gammopathies, when hyperproteinemia can cause coma, trophic ulcers and gangrene of the extremities, and chronic renal failure. Therefore, any excess of protein reference values, especially high and persistent ones, requires contacting a doctor.
| ICD-9 | MeSH | DiseasesDB | MedlinePlus |