Cardiovascular diseases
Most often, riders, having felt pain in the chest, begin to worry about whether they have heart problems. Scary words come to mind: aorta, aneurysm, angina, stroke, heart attack. The pressure rises, the pulse quickens and a panicked state comes over the person, further aggravating his condition.
A feeling of tightness in the chest can be a sign of a heart attack, but only if there are a number of additional symptoms:
- paleness of the skin;
- profuse sweating;
- heart rhythm disturbance;
- pain in the middle of the sternum;
- weakness that prevents you from sitting or standing up;
- nausea.
Signs of angina pectoris make it possible to distinguish this pathology from manifestations of vegetative-vascular dystonia:
- the pain has an enveloping character, it seems to burn all the insides, gradually moving from the center to the left side of the sternum;
- unpleasant sensations often appear after experiences or physical activity;
- there are breathing difficulties;
- there is a lump in the throat;
- the pain subsides after the person takes a Nitroglycerin tablet;
- Manifestations of angina occur with regularity.
In addition to an attack of angina, the cause of chest pain may be a pulmonary embolism. This condition is quite dangerous, it has the following characteristic signs:
- constant lack of air;
- feeling of tightness in the sternum;
- cough that produces blood-stained sputum;
- deterioration of general condition.
Pulmonary embolism is an extremely serious pathology that requires immediate emergency medical care.
Pain in the middle of the chest is often provoked by various forms of coronary heart disease. These pathologies share a number of symptoms:
- pain: dull, sharp, pressing, burning;
- recoil to the arms, neck, shoulder blades;
- shortness of breath with increased heart rate;
- acceleration of heartbeat;
- increase in blood pressure;
- headaches;
- swelling of the limbs;
- paleness of the skin.
Pain in the chest in the middle: causes
Experts identify a number of pathological conditions when you can often feel pain in the middle behind the sternum:
- Chest injuries;
- Heart diseases: myocardial infarction and angina;
- Lung diseases: thromboembolism;
- Diseases of the digestive system: acute pancreatitis, disruption of the esophagus, duodenal and stomach ulcers.
A characteristic symptom of myocardial infarction and angina is the appearance of acute pain in the chest of a stabbing nature. If for the first time you have pain in the middle of your chest, then you need to see a doctor right away.
If you feel a burning sensation and, in addition to everything, you have a feeling of compression in the middle of the sternum, then the cause may be an incipient myocardial infarction , so you need to immediately call an ambulance. You should not neglect such signs, since there are many cases where this led to the death of a person.
Quite often, pain of a paroxysmal nature occurs in diseases of the psychogenic type. In such conditions, the pain becomes stabbing or pressing in nature, and can also be sharp or dull. They are often felt in the middle or upper part of the chest.
Constant aching pain in the sternum poses much less risk than a sudden attack of pain. This symptom often indicates the presence of neurological diseases, spinal injuries, or problems with the digestive tract.
Why does it hurt in the middle of the sternum?
The most common causes of pain in the middle of the sternum include:
- osteochondrosis;
- coronary heart disease;
- aortic aneurysm;
- gastroesophageal reflux disease.
The disease is a destructive process that affects the intervertebral discs, which are located in the thoracic spine. Its progression triggers dystrophic reactions in the tissues of the discs, leading to disruptions in their shock-absorbing functions, and also causes changes in the bone structures of the vertebrae themselves and leads to their pathological approach to each other.
The result of such destructive reactions is impaired mobility of the spine and compression of the nerve roots located in the immediate vicinity of the spinal column. As a result, pain in the middle of the sternum radiates to the back and intensifies with physical activity, sudden movements, heavy lifting, and even when sneezing or coughing.
Factors predisposing to the development of osteochondrosis are:
- Heredity.
- Age-related changes.
- Traumatic injuries.
- Increased physical activity.
- Circulatory disorders.
- Hormonal imbalance.
- Harmful working conditions.
- Congenital morphological anomalies of the spine.
- Infectious processes.
- Chronic stress.
The lack of adequate treatment leads to the destruction of the fibrous ring and the release of fragments of the intervertebral disc into the spinal canal (hernia), which leads to increased compression myelopathy and a repeated increase in pain.
Another common cause is coronary artery disease (CAD). The pathology is an organic damage to the myocardium caused by a lack of coronary circulation in the heart muscle. It may have acute forms of manifestation (myocardial infarction, cardiac arrest) or take a chronic, protracted course (angina pectoris, cardiosclerosis). Factors contributing to the occurrence of ischemic heart disease are:
- Hyperlipedemia.
- Arterial hypertension.
- Drinking alcohol, smoking.
- Overweight.
- Metabolic disease.
The disease has a wave-like course with a slow development of pathological manifestations and a gradual increase in negative symptoms. Its main features include:
- Dizziness.
- Pressing pain in the middle of the sternum (often in the left chest).
- Increased sweating.
- Blurred consciousness.
- Nausea.
- Edema of the lower extremities.
- Dyspnea.
- Increased heart rate.
IHD is irreversible. Adequate therapeutic measures can greatly slow down its progression and prevent the most negative development scenarios. Without treatment, there is a high risk of premature death (sudden coronary death).
Aortic aneurysm
Pathology implies local expansion of a certain area of the aorta, caused by a violation of the tissue structure of its walls. Common causes of an aneurysm include:
- Arterial hypertension.
- Atherosclerosis.
- Morphan's syndrome.
- Syphilitic infection.
- Traumatic lesions of the chest.
- Fibrous dysplasia.
- Erdheim syndrome.
- Age-related changes.
- Alcohol abuse.
When the disease appears, a person not only experiences pain in the middle of the sternum, but also experiences additional symptoms:
- Tachycardia.
- Pain in the heart area.
- Dizziness.
- Bradycardia.
- Dysphonia.
- Dry cough.
- Dysphagia.
- Increased salivation.
The lack of therapeutic measures can lead to the development of various complications. The most serious of them are stroke, acute renal failure, and pulmonary hemorrhage. In critical cases, urgent surgical intervention is indicated. Prevention of the disease is primarily aimed at reducing cholesterol levels in the blood.
This pathology is characterized by the systematic reflux of stomach contents back into the esophagus. This causes an inflammatory reaction in the tissues lining the walls of the esophagus, which entails the occurrence of various negative symptoms and causes regular pain throughout the esophageal muscular tube. The main factors that provoke the development of GERD are:
- Gross power supply errors.
- Overweight.
- Pregnancy.
- Diaphragmatic hernia.
- Uncontrolled use of certain medications.
- Smoking.
- Alcohol consumption.
- Flatulence.
Main symptoms of GERD:
- Heartburn.
- Belching sour.
- A burning sensation behind the sternum.
- Odynophagy.
- Dysphagia.
- Coronary-like pain in the chest.
Most often, pain in the middle of the sternum when inhaling is associated with pulmonary diseases. When the lungs are damaged, discomfort is usually associated with a violation of their pleural membrane, which contains many nerve endings and, when ruptured, inflamed or irritated, causes discomfort in the chest, as well as pain in the spine and middle of the back. As a rule, such manifestations occur with pneumonia, tuberculosis, bronchitis, and pleurisy.
In second place are chest injuries. When falling from a height or in an accident, a rib fracture occurs, which causes pain when breathing, and especially when taking a deep breath. The third most common are intercostal neuralgia, vascular and cardiac pathologies.
In addition to all the ailments listed, pain in the sternum in the middle can also cause discomfort:
- stomach ulcer;
- vegetative-vascular dystonia;
- pathologies of the thyroid gland;
- pregnancy;
- foreign body in the esophagus.
In all cases, the reasons for such sensations require medical clarification.
Compressive (pressing, burning) pain in the middle of the chest is a common symptom of coronary heart disease (angina). Sometimes it spreads to the left half of the chest, left arm (scapula, hypochondrium, back). It usually occurs during physical activity, stress, and less often at rest. The attack lasts up to 10-15 minutes and is relieved with nitroglycerin.
Acute, sharp, intense pain in the center of the chest or on the left, accompanied by cold sweat, suffocation, nausea, and severe fear of death is a clinical sign of myocardial infarction. It occurs spontaneously, without reference to stress, even at night during sleep, lasts more than 15 minutes, and is not relieved by anti-angina medications. A heart attack requires urgent hospitalization.
Pain in the sternum is localized in the middle in diseases of the lungs (pneumonia, bronchitis, tracheitis), gastrointestinal tract (gastric and duodenal ulcers, gastritis, diseases of the esophagus), thoracic spine (osteochondrosis), peripheral nervous system (vegetative-vascular dystonia, intercostal neuralgia), with diaphragmatic abscess or cancer of the thoracic organs.
Gastroesophageal reflux disease causes a persistent burning sensation in the middle of the chest and throat (heartburn). If the pain intensifies when a person lies down, this indicates a possible diaphragmatic hernia. Painful symptoms in the upper chest are probable diseases of the upper respiratory tract.
With the above diseases, pain, usually localized in the middle of the chest, sometimes spreads to the left side of the body (less often the right or back). Only a doctor can make a diagnosis, therefore, except in cases of emergency hospitalization, it is unreasonable to postpone a visit to a specialist. It is important to track and inform the therapist about the accompanying symptoms: shortness of breath, sweating, swelling, high temperature, cough, the nature of pain during exercise/rest, eating, and different body positions.
Pericarditis (inflammation of the lining of the heart), as a rule, is accompanied by constant moderate (sometimes intensifying) aching pain that worries in the area of the heart and above it, sometimes spreading to the right half of the chest, as well as the epigastric region and left scapula. If a person lies on his back, the pain intensifies.
Other diseases with a characteristic pain symptom on both the right and left side of the sternum may be neurological problems. Inflammation, abscess, swelling of the right lung are accompanied by various types of constant pain (aching, pressing, dull, burning), sometimes radiating to the healthy side, abdomen, neck, shoulder, and aggravated by coughing.
If chest pain occurs or gets worse when you cough, it may be a sign of:
- diseases of the pleura (the lining of the internal surfaces of the chest cavity);
- impaired mobility of the thoracic spine and ribs;
- intercostal neuralgia;
- colds of the respiratory tract (tracheitis, bronchitis);
- renal colic;
- pneumothorax;
- lung oncology;
- chest injuries.
For osteochondrosis
Exacerbation of osteochondrosis of the thoracic spine is sometimes mistaken for a pathology of the cardiovascular system, because the accompanying pain in the sternum is localized, as a rule, in the region of the heart, sometimes radiating to the right half, to the back or side. The pain symptom occurs suddenly, paroxysmally, or is characterized by a mild, long-term course. Increased discomfort occurs when inhaling, exhaling (during an attack it can be difficult to breathe), coughing, moving the arms and neck.
The similarity of symptoms with heart attack and angina leads to the fact that patients unsuccessfully try to alleviate their condition with medications for these diseases. If treatment is incorrect or absent, internal organs (pancreas, liver, intestines) are affected, and malfunctions of the cardiovascular system are possible, so a visit to the doctor should not be postponed.
When driving
In many diseases (angina pectoris, heart attack, myocarditis, pleurisy, osteochondrosis, sternum injuries, rib fractures), pain in the sternum increases with movement. Sometimes discomfort occurs only during certain movements, for example, when bending over, making sharp turns, lifting heavy objects, or pressing on the chest bone. Do not neglect the examination if the pain has passed, or rely on traditional methods of treatment, because these symptoms may be the first sign of a serious problem.
If severe pain occurs suddenly and is accompanied by shortness of breath, shortness of breath, clouding of consciousness, nausea, you should immediately seek medical help.
Emergency hospitalization is indicated for diseases that have a high mortality rate without timely assistance, such as:
- myocardial infarction;
- pulmonary embolism;
- spontaneous rupture of the esophagus;
- dissecting aortic aneurysm;
- ischemic disease (angina pectoris);
- spontaneous pneumothorax.
Myocarditis
Causes of pressing heaviness behind the sternum
When visiting a doctor, the patient may describe his sensations as a pressing heaviness in the middle of the sternum. Such phenomena may indicate the development of a pathological process on the part of various internal organs and systems:
- cardiovascular (congenital and acquired defects, myocardial infarction, angina pectoris, myocarditis, aortic aneurysm, etc.);
- respiratory (bronchial asthma, tuberculosis, COPD, emphysema, pleurisy, pneumonia, pneumothorax);
- digestive (diaphragmatic hernia, reflux esophagitis, cholelithiasis, ulcerative colitis);
- musculoskeletal (spinal injuries, osteochondrosis, protrusion and herniated intervertebral discs);
- nervous (depressive states, severe neuroses, neuralgia).
A feeling of heaviness behind the sternum may appear during tumor processes in the mediastinum, during the formation of a hernia in the esophagus, or due to severe psychogenic abnormalities. In any case, only a specialist can correctly assess the condition and make the correct diagnosis.
During a visit to the doctor, the patient needs to describe in detail his feelings during the attack. For example, note that a feeling of heaviness in the chest is accompanied by shortness of breath, pain, breathing problems, or heart rhythm disturbances. These are important symptoms that will help the doctor understand the essence of the problem. An important diagnostic sign is the nature of the pain (squeezing, sharp, dull, aching or burning) and the area of its localization.
Pain and heaviness in the chest are common phenomena that accompany many pathologies. Therefore, when an unpleasant symptom appears, a comprehensive differential diagnosis is necessary to establish the cause of this condition. Let's look at the main diseases that cause heaviness in the middle of the sternum and difficulty breathing.
Pathologies of the heart and blood vessels
Diseases of the cardiovascular system pose the greatest danger to the patient, as they can be fatal.
Coronary heart disease (CHD)
It develops against the background of insufficient blood supply to the tissues of the heart, causing hypoxia (oxygen starvation) and myocardial damage. Among the main symptoms of IHD are heaviness and pain behind the sternum, radiating to the left arm, heart rhythm disturbances, dizziness, fainting, and cold sweats. When symptoms of heart failure occur, the patient suffers from shortness of breath that occurs with the slightest physical effort and swelling of the lower extremities.
Angina pectoris
The pathology is manifested by burning, pressing pain, heaviness in the left sternum. Painful sensations spread to the left half of the body and radiate to the shoulder, arm and under the shoulder blade. Angina pectoris develops against the background of coronary heart disease and is regarded as a pre-infarction condition. The cause of the attack may be severe stress or excessive exercise. It can be relieved with nitroglycerin tablets.
Myocardial infarction
A heart attack is manifested by pressing, sharp pain behind the sternum, which spreads to the left side. In this case, the patient experiences suffocation, fear of death, and attacks of nausea. There is pallor of the skin, clouding of consciousness, and pouring cold sweat. The attack cannot be relieved with conventional means (for example, nitroglycerin). The patient requires urgent hospitalization in the cardiology department.
Tachycardia
These are attacks of rapid heartbeat, during which there is a feeling of lack of air, a coma in the throat, a feeling of constriction in the chest, and inexplicable anxiety. An attack can begin against the background of physical activity, stressful situations, exacerbation of pathologies of the respiratory, nervous system or heart disease.
Heart defects (congenital or acquired)
Congenital anomalies are usually diagnosed immediately after the birth of a child, acquired ones are identified on the basis of characteristic complaints. In such conditions, the patient should be under the supervision of a cardiologist. From time to time he may be disturbed by pain in the heart, shortness of breath, a feeling of heaviness in the chest, which intensifies with physical activity and under the influence of other provoking factors (nervous tension, anxiety, stress).
Atherosclerosis
The pathological process is accompanied by blockage of blood vessels with sclerotic plaques. In fact, this disease can be considered as a pre-infarction or pre-stroke condition. It manifests itself as a persistent increase in blood pressure, a feeling of tightness and heaviness in the chest, shortness of breath, irregular heart rhythm, and tinnitus.
Respiratory diseases
Difficulty breathing and heaviness behind the sternum often cause diseases of the lungs and bronchi. In such cases, additional symptoms such as cough, shortness of breath, chest pain, general malaise, and fever occur.
Bronchial asthma and COPD
The pathologies have much in common in terms of symptoms. They are manifested by shortness of breath, general deterioration of the condition, a prolonged, dry cough, and a feeling of tightness in the sternum. Bronchial asthma is exacerbated by the influence of allergens - manifested by attacks of suffocation, rapid heartbeat, heaviness in the chest, and the appearance of cold sweat. The attack ends with the release of viscous, glassy sputum.
Chronic obstructive pulmonary disease (COPD) is most often diagnosed in long-term smokers and is accompanied by a debilitating dry cough, pressing sensations in the middle of the sternum, and a gradual increase in shortness of breath. Attacks of coughing and suffocation intensify when inhaling dusty air, tobacco smoke and other irritants.
Pulmonary embolism
In this disease, blood clots clog the branches of the pulmonary artery, causing a lack of oxygen (hypoxia), which affects all tissues and internal organs. In this case, attacks of suffocation occur, in an attempt to compensate for the lack of air, the heart works more intensely, tachycardia occurs, and a feeling of heaviness and tightness in the sternum appears. Pulmonary embolism is a dangerous disease that can be fatal if not treated promptly.
In addition, characteristic symptoms associated with a feeling of heaviness in the chest accompany bilateral pneumonia, tuberculosis, pneumothorax and other diseases of the respiratory system.
Digestive system diseases
There are several gastrointestinal pathologies that manifest themselves as symptoms of compression in the chest area.
Diaphragmatic hernia
With this pathology, a hole forms in the diaphragm of the esophagus through which the cardia of the stomach can exit. As a result, additional pressure occurs on the lungs and heart, causing heaviness in the chest, stabbing pain and shortness of breath in combination with dyspeptic disorders.
Reflux esophagitis
The disease is characterized by the backflow of stomach contents into the esophagus, which is accompanied by heartburn, belching, discomfort, a feeling of heaviness, distension behind the sternum and in the epigastric region.
Gastritis
Exacerbation of gastritis is caused by an inflammatory process in the walls of the stomach and causes pressure on the sternum, with a concomitant deterioration in respiratory functions. At the same time, digestive disorders, a general deterioration in health, abdominal cramps, a feeling of fullness, belching and heartburn are noted.
Mediastinal tumors
The formation of a tumor in this anatomical area provokes compression of nearby organs - the esophagus, lungs, pericardium and causes a persistent feeling of heaviness and pain in the sternum. When the bronchi are compressed, the patient suffers from shortness of breath and coughing attacks. When nerve endings and the superior vena cava are pinched, symptoms such as swelling and cyanosis of the facial skin, headaches, bulging neck veins, drooping eyelids or constricted pupils appear.
If the process is malignant, then the tumor quickly grows into neighboring tissues, causing pain in the heart, signs of pleurisy, inflammation and enlargement of the lymph nodes. The patient complains of general weakness, malaise, lack of appetite, and rapid weight loss.
Pathologies of the musculoskeletal system
This group of diseases includes osteochondrosis of the cervical or thoracic spine, scoliosis, protrusion and herniated discs.
Osteochondrosis
With this disease, the cartilage tissue of the intervertebral discs is destroyed, as a result, the discs “sag”, pinching the nerve roots, which causes various disorders - from a feeling of lack of air, heaviness behind the sternum, to the appearance of constant, debilitating pain in the affected part of the spine, a sensation of crawling and numbness of the skin. Sometimes the symptoms of osteochondrosis resemble a heart attack, as the pain spreads to the sternum, extends into the arm and under the shoulder blade. But such manifestations cannot be stopped with heart medications.
Scoliosis
Spinal curvature provokes complications from various body systems and over time can lead to the development of osteochondrosis, diseases of the digestive and respiratory systems, and manifestations of vegetative-vascular dystonia. Scoliosis of the thoracic region is accompanied by pain and heaviness in the chest and back, impaired respiratory function, fatigue, a feeling of numbness and tingling in the upper extremities when the neurovascular bundles are pinched.
Chest injuries
Pressing heaviness in the sternum, making breathing difficult, may be a consequence of a previous injury. Any situations associated with a strong blow to the chest can lead to damage to the periosteum, resulting in long-term pain in this area, which intensifies with physical activity and weakens at rest. An x-ray will help identify the consequences of the injury. The treatment is carried out by a traumatologist.
Nervous system diseases
Regular stress, nervous breakdowns, psycho-emotional overstrain are accompanied by a deterioration in physical condition - a feeling of lack of air, a lump in the throat, a pressing heaviness in the chest, headache, rapid heartbeat. Sometimes a stressful situation causes panic attacks, with loss of orientation, suffocation, heart rhythm disturbances, attacks of fear and severe anxiety. In such cases, taking sedatives helps relieve the acute condition.
Intercostal neuralgia
This pathological condition is accompanied by pain due to compression of the intercostal nerves. Pain of varying severity (from aching to sharp and shooting) spreads from the spine to the sternum. They are accompanied by a feeling of heaviness and constriction, difficulty moving, and limited mobility of the upper limbs. The cause of the pathology can be hypothermia, infections, pinched nerves due to osteochondrosis, or the development of radicular syndrome due to intervertebral hernia in the thoracic region. Sometimes the symptoms of neuralgia signal the development of serious diseases such as tumors of the spinal cord, mediastinum or pleurisy.
Thus, there are many reasons that can cause heaviness in the middle of the sternum. If such a symptom appears, you should not delay contacting a doctor, as it may indicate the development of dangerous pathologies.
Diagnostic principles
Heaviness in the sternum is a sign of many diseases, so the patient will undergo a wide range of laboratory and instrumental studies. In addition to taking a history and physical examination, the therapist will give directions for:
- general clinical analysis of blood and urine;
- biochemical blood test;
- analysis of sputum and pleural fluid;
- X-ray of the chest, spine;
- Ultrasound of internal organs;
- ECG and echocardiography of the heart;
- FGDS of the stomach.
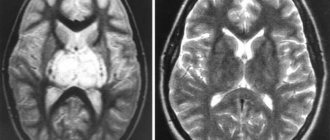
If necessary, a number of additional studies may be prescribed - spirometry, 24-hour heart rate monitoring, computed tomography or magnetic resonance imaging.
Having received the results of the examination, the specialist will make a diagnosis, on the basis of which specialized specialists - a cardiologist, gastroenterologist, neurologist, pulmonologist, phthisiatrician, oncologist or nephrologist - are involved in the treatment of the patient.
Treatment methods
Treatment tactics depend on the type of pathology, the cause causing the characteristic symptom, the presence of concomitant diseases, the severity of the condition, the age of the patient and other nuances.
In the treatment of heart and vascular diseases, drugs to lower blood pressure, cardiac glycosides, ACE inhibitors, and drugs to stabilize heart rhythm are used. For manifestations of atherosclerosis, medications are prescribed to normalize blood circulation, statins, fibrates, which prevent the formation of cholesterol plaques.
For diseases of the spine, drugs from the NSAID group are used in injections and tablets (Diclofenac, Ibuprofen), injections of vitamins (Actovegin, Combilipen), which relieve pain, stop the inflammatory process, and improve blood circulation in the affected area. To relieve muscle spasms, relaxants Mydocalm or Baclofen are used.
When relieving the symptoms of intercostal neuralgia, the treatment regimen includes muscle relaxants (relief from spasms and pain), anti-inflammatory drugs, and in severe cases, injections of hormones - Prednisolone, Dexamethasone.
For neurological disorders, the doctor will prescribe sedatives (Persen, motherwort, valerian), and if necessary, treatment will be supplemented with tranquilizers or antidepressants.
The approach to eliminating the problem that causes heaviness in the sternum is individual. Correct and effective treatment can only be selected by a specialist, taking into account the underlying disease. Self-medication is unacceptable; it can have unpredictable consequences or lead to serious complications. If you experience attacks of suffocation, heaviness and compression in the sternum area, you should visit a doctor as soon as possible or call emergency medical care.
source
Pulmonary diseases
Pulmonary pathologies are a common cause of pain in the middle of the sternum and panic provoked by their occurrence. Severe chest pain can be caused by:
- tracheitis;
- pleurisy;
- bronchitis;
- lung abscess;
- pneumonia.
Pain can be classified as pulmonary if the following additional signs are present:
- inability to fully inhale and exhale air;
- feverish condition;
- confusion;
- difficulty breathing, redness of the skin;
- change (including acceleration) of heart rhythm;
- decrease in blood pressure indicators;
- acquisition of shades of blue by the skin.
A characteristic feature of pleurisy is increased pain when inhaling air, especially if a person lies on his back.
Diagnostics
A general practitioner or family doctor will determine the cause of chest pain. To verify the diagnosis, the musculoskeletal system and internal organs are examined. The main ones are instrumental methods for visualizing anatomical structures; laboratory diagnostics are performed to clarify the cause of thoracalgia. The most informative methods:
- Electrocardiography.
To exclude or confirm the cardiac etiology of pain in the left side of the chest, an ECG is recorded in standard leads. Expansion and deformation of the complexes, elevation of the ST interval indicate myocardial ischemia. To diagnose arrhythmias, Holter monitoring is performed. - Ultrasound research
. Echocardiography (EchoCG) is necessary if the chest hurts on the left side. The contractile function of the heart muscle, ejection fraction, and signs of destructive lesions of the valve apparatus are assessed. Abdominal ultrasound is used to detect diseases of the spleen, pancreas, or gallbladder causing thoracalgia. - Radiography
. On radiographs of the chest, one can detect focal processes in the lung tissue, space-occupying formations of the lungs and mediastinum, which are usually the etiological factor of chest pain. Women are prescribed mammography. Plain radiography of the gastrointestinal tract is recommended for detecting diaphragmatic hernia and ulcerative defects. - Endoscopic methods
. To diagnose injuries to the esophagus that cause chest pain, an endoscopy is performed. During the study, the condition of the mucous membrane and the contractility of the cardiac sphincter are studied. In case of severe damage to the respiratory system, bronchoscopy is indicated to examine the mucous membrane and take material for bacterial culture.
General and biochemical blood tests reveal signs of inflammatory processes, pathologies of the liver and biliary system. Bacteriological culture of sputum and bronchial washings is necessary to establish the type of pathogen. In women, the concentration of sex hormones is determined. If you feel unbearable pain in the chest and suspect cancer, a biopsy of the suspicious formation is performed for cytological analysis.
Diseases of the gastrointestinal tract
The lungs, esophagus, stomach - all these organs are located in the thoracic region, and accordingly, a change in their normal state can cause discomfort in this area. The nature of the manifestation of pain in the gastrointestinal tract is different from those that accompany heart and vascular diseases. And the use of sedatives or cardiac drugs does not have any effect.
If a person has a hernia, it manifests itself with the following symptoms:
- heartburn;
- belching;
- chest pain;
- vomiting;
- rumbling in the stomach;
- satiation too quickly during meals.
Peptic ulcer and gastritis are diagnosed through special studies, as well as the presence of the following signs:
- excruciating pain in the middle of the sternum;
- dyspeptic disorders;
- belching;
- feeling that the stomach is bursting from fullness;
- heartburn;
- irritability;
- pulse disturbances (tachycardia).
Causes
Pathological processes in the chest wall, respiratory organs located inside the chest, diseases of the heart or aorta, irradiation (conduction) of pain behind the sternum from the spine, abdominal organs - these are all the reasons that cause pain behind the sternum.
Heart diseases
This group includes cardiac pathologies, in particular angina pectoris, myocardial infarction. They are characterized by sharp pain, of high intensity, usually localized on the left side, radiating to the left arm, the left half of the neck, and to the back on the left side.
In diseases of the aorta, they are felt in the center, behind the manubrium of the sternum. When the pulmonary vein is blocked (pulmonary thromboembolism), it also most often occurs on the left side, in the region of the heart, but what distinguishes it from pain during myocardial infarction is the intensification when performing respiratory movements.
Lung diseases
The most common causes of pain are associated with lung diseases, when the pleura is involved in the process. These are pneumonia, lung cancer, tuberculosis, their peculiarity is the intensification of pain when coughing, sneezing, and inhaling. With lower, diaphragmatic pleurisy, the pain is pressing and radiates to the abdomen on the right side, which sometimes leads to an erroneous diagnosis of liver disease.
Diseases and injuries of the chest wall
Diseases of the chest wall include osteomyelitis, in which the sternum hurts in a certain area of the bone, most often in the center; there is no dependence on the respiratory movements of the chest. When the sternum is fractured, pain is felt, which sharply intensifies with movements of the chest.
Diseases of the musculoskeletal system
Pain in the chest area, located exactly in the center or slightly to the left, may be a symptom of intercostal neuralgia, in which inflammation of the nerve fibers of the muscle tissue occurs.
Additionally, the following manifestations of pathology can be noted:
- pain increases with movement;
- it is difficult for a person to cough or sneeze; all these processes are accompanied by unpleasant sensations.
The causes of this disease can be hypothermia of the body, previous injuries to the chest, spine and limbs.
Osteochondrosis of the thoracic spine is another disease that causes pain in the middle of the chest. It occurs with the following additional symptoms:
- constant strong tension in the back muscles;
- numbness of the back muscle corset;
- increased pain during deep breaths, bending, turning or raising arms, at night and in the cold;
- tingling and “goosebumps” running in different parts of the body;
- feeling of pressure in the chest;
- intercostal pain;
- cold or heat in the lower extremities.
In order to relieve pain, a course of massage, exercise therapy and taking painkillers and anti-inflammatory drugs are used.
Pain from chest injuries
A person may experience pain in the sternum as a result of injuries sustained in a car accident, friendly wrestling, or drunken brawl. And most patients complain of pain in the chest and back.
Trauma provokes rupture of muscles and blood vessels , and this explains the appearance of pain, which begins to intensify when inhaling, turning and bending the body.
Damage to the periosteum from a blow to the chest is very dangerous. In this case, a person may feel continuous pain for a long time, which will begin to subside only after many weeks.
Getting cracks and fractures of the sternum is fraught not only with pain, but also with a disturbance in general well-being, and attempts to feel the source of pain with your hands leads to increased discomfort.
The cause of the pain may be damage to the sternum, although in each case it may be accompanied by various symptoms. At rest, the pain is felt much less, and any movement and deep breathing leads to its aggravation.
Psychological diseases due to stress
Pain in the middle of the chest, which is accompanied by a deterioration in mood, the appearance of depressive thoughts and an increase in anxiety, can be the consequences of stressful situations.
People who are suspicious and acutely sensitive to any conflict situations are susceptible to the occurrence of such pain. If the pain is accompanied by a panic attack, causing a person to become very nervous, out of breath and suffer from pressure changes and an increase in heart rate, then we are talking about autonomic disorders of the nervous system.
To get rid of such manifestations, it makes sense to seek support from a psychologist or psychotherapist, who will help cope with the experiences that worry a person, teach self-soothing and the principles of meditation.
Symptoms of diseases
When chest pain occurs, the symptoms can be quite different. This is explained by a wide range of diseases that provoke unpleasant pain.
Dangerous symptoms, if they appear, you should immediately consult a doctor:
- A sharp jump in body temperature.
- Nausea and urge to vomit.
- Increased sweating.
- The appearance of shortness of breath and impaired breathing.
- Loss of consciousness. It can become one of the main symptoms of myocardial infarction.
- Increased or decreased heart rate.
- When changing body position, coughing or active movement, the pain may increase.
- Muscle weakness.
- Body aches.
Symptoms are rarely isolated; they are often combined and interfere with proper first aid.
If the following symptoms appear, you should immediately call an ambulance:
- When the nature of pain changes.
- Painful sensations either in the left side of the chest or in the right.
- Increased pain when lying down.
- First aid medications do not show effectiveness.
What is the symptom: compression in the chest in the center, difficulty breathing? — read the answer to the question here.
DOCTORS RECOMMEND! Read more "
What does pain mean when inhaling and exhaling?
Pain in the sternum when exhaling or inhaling is not directly related to the myocardium, but is a sign of the following diseases:
- intercostal neuralgia (pain is localized more often on the left, discomfort intensifies when trying to take a deep breath or when coughing);
- pneumothorax (when air accumulates between the chest wall and the lung, characterized by pain on the left side, which intensifies when the person breathes deeply);
- precordial syndrome (severe pain unexpectedly occurs during inspiration, repeats several times a day, is not associated with stress, does not require specific treatment).
Cardialgia of cardiac origin
One common cause of chest pain is pericarditis.
Chest pain due to heart pathology does not always manifest itself in the same way and can have different origins. Each heart disease has its own characteristics, which the doctor takes into account at the stage of diagnosis.
Cardiac ischemia
Ischemia of the heart muscle occurs when there is a discrepancy between the need of muscle cells for oxygen and its delivery through the coronary arteries. Pathological changes in these vessels in this pathology vary from partial narrowing in the presence of an atherosclerotic plaque to complete occlusion by a thrombus, which determines the clinical picture of the disease from episodes of silent ischemia to transmural myocardial infarction.
Pain in this pathology is felt by a person as pressing or squeezing; it is usually localized behind the sternum or in the region of the heart and radiates to the neck, under the shoulder blade, lower jaw, and arm (usually the left). When talking about their sensations, patients show the location of the pain by clenching their hand into a fist and applying it to their chest, which once again emphasizes the nature of the pain. With angina pectoris she:
- short-term;
- occurs after physical activity;
- relieved by taking nitroglycerin.
Pain during myocardial infarction:
- intense;
- accompanied by vegetative symptoms;
- does not go away after consuming nitrates.
The diagnosis is confirmed by changes in the electrocardiogram.
Pericarditis
The outer connective tissue layer of the heart contains pain receptors. Nerve fibers from these receptors are part of the intercostal, phrenic and sympathetic nerves, which determines the possible irradiation of pain. With pathology of the pericardium, its receptor apparatus is irritated and a person experiences acute pain in the heart area, often radiating to the upper outer edge of the trapezius muscle. If inflammation spreads to the adjacent pleura, pain during pericarditis may be pleural in nature.
With dry pericarditis, the pain is very intense. At the same time, its character may differ - it can be blunt, sharp, cutting. It intensifies when trying to lie on the left side and decreases in a sitting position or bending forward. The examination reveals:
- pericardial friction rub;
- increased body temperature and symptoms of intoxication;
- changes in the blood (leukocytosis), etc.
Myocarditis
Pain due to myocarditis (inflammation of the heart muscle) appears in the chest after an infection, allergy, or parasitic infestation. It has its own characteristics:
- long-term, not paroxysmal;
- aching or stitching;
- not associated with physical activity;
- does not decrease after taking nitrates.
When examining such patients, signs of myocarditis are revealed:
- increase in heart size;
- arrhythmias;
- heart failure, etc.
Cardiomyopathies
This term unites a group of pathological conditions, the common feature of which is structural and functional changes in the heart muscle in the absence of pathology of the heart valves, damage to the coronary arteries and arterial hypertension. Cardiomyopathies can be primary or secondary. The primary cause cannot be determined. This disease is also characterized by pain syndrome, which is combined with:
- with rhythm disturbances;
- increase in heart size;
- fainting;
- congestive heart failure.
The pain can last for hours and decreases only after taking analgesics. In later stages, it may resemble that of angina pectoris and can even be treated with nitroglycerin, but other manifestations of the disease allow a correct diagnosis to be made.
Secondary cardiomyopathy is often observed against the background of hormonal changes, for example, with pathological menopause. Patients experience unpleasant sensations in the heart area of varying nature and intensity; they last for a very long time (weeks, months), sometimes weakening, sometimes intensifying. Such pains:
- not provoked by physical activity;
- combined with shortness of breath, palpitations;
- weaken after taking sedatives, using mustard plasters.
People who abuse alcohol may experience stabbing, aching pain in the chest. Often such attacks occur at night, especially on the 2-3rd day after drinking alcohol. Such patients have a characteristic appearance. They reveal:
- liver enlargement;
- symptoms of heart failure;
- various heart rhythm disturbances;
- mental changes.
Aortic pathology
Pain resembling ischemic pain occurs in individuals suffering from severe stenosis of the aortic mouth. With this pathology they occur more often than with other heart defects. Such sensations are caused by relative coronary insufficiency, but their connection with physical activity cannot be identified.
With aortic valve insufficiency, pain is also present. However, its mechanism is completely different - low diastolic pressure in the aorta in combination with atherosclerotic changes.
Particular attention should be paid to dissecting aortic aneurysm, which is more often detected in elderly people with a long history of arterial hypertension. With this disease, severe chest pain suddenly occurs, radiating to the back, followed by migration down the abdomen and lower limbs. A typical sign of this pathology is asymmetry of blood pressure and pulse in the arms and legs.
TELA
With pulmonary embolism, the pain is intense and is not relieved by taking analgesics.
Pulmonary embolism is a life-threatening condition, which can be recognized taking into account some clinical features of its course:
- pain in the chest of varying intensity, often behind the sternum, which can only be relieved with narcotic analgesics;
- its combination with shortness of breath, cough, hemoptysis, fear of death;
- heart rhythm disturbances such as extrasystole, atrial fibrillation;
- history of thrombophlebitis, fractures, surgical interventions, prolonged bed rest.
The diagnosis can be confirmed by objective examination data and additional diagnostic methods (ECG, radiography).
Autonomic dysfunction
Pain may occur due to autonomic dysfunction of the central nervous system. Moreover, disorders of this kind are more common in children and adolescents.
The reasons for the development of such pathologies are:
- psycho-emotional factors;
- lesions of the central nervous system that occurred in the perinatal period;
- heredity.
Signs of autonomic dysfunction are:
- paroxysmal pain in the chest, squeezing or pressing in nature;
- accelerated heartbeat;
- feeling of lack of air;
- panic state;
- changes in pressure, with differences from low to high numbers, and vice versa;
- decrease in body temperature;
- gastrointestinal disorders;
- dizziness;
- insomnia;
- lethargy;
- depressive moods.
As a rule, the examination does not reveal serious physical abnormalities in the patient. Attacks of pain occur periodically, decreasing and increasing, lasting from 5-10 minutes to several days. And they arise after a person is very worried or has suffered severe physical stress.
To stop an attack, you need to take a sedative (tincture of motherwort, valerian or Validol).
When does it occur?
For differential diagnosis, not only the nature of the pain syndrome is important, but also the conditions that provoke exacerbation. These factors can be inhalation and exhalation, pressing on the chest or ribs, active movement.
When driving
With ischemic heart disease, angina pectoris, atherosclerosis of the coronary vessels, with damage to the spine by scoliosis, osteochondrosis or radiculitis, with neoplasms in the thoracic region, severe pain in the sternum in the middle often appears when moving the limbs or walking.
If chest pain is associated with movement, this is a serious reason to consult a doctor.
At rest
With critical narrowing of the coronary vessels, pain under the sternum in the middle (more precisely, behind it) can occur even in a calm state, which is not very typical for angina, but occurs precisely with serious atherosclerotic lesions.
A distinctive feature of pain with angina at rest is a pressing, squeezing or burning pain syndrome, almost always accompanied by shortness of breath or lack of air.
Non-cardiac causes of pain signals in the chest in a calm state can be associated with pathologies of the spine, neuralgic and tumor diseases, as well as pathologies of the respiratory system. Diagnostic procedures suggested by your attending physician will help determine the exact cause.
When you press
The cause of painful signals that occur when pressing on the ribs or chest may be inflammation in the periosteum, which leads to disruption of the articulation of the ribs with the central bone - Tietze syndrome. This disease is typical for adolescent and young patients.
But pain in the sternum in the middle when pressed occurs not only for this reason, but as a result of injury or surgery, age-related changes in osteochondral tissues, infections, hypovitaminosis and electrolyte imbalances.
When inhaling
When there is pain in the middle of the sternum and it hurts to breathe, this can be a symptom of many pathological conditions:
- pleurisy;
- pulmonary tuberculosis;
- pneumonia;
- bronchitis;
- tracheitis;
- tumors of the respiratory organs;
- TELA;
- heart pathologies;
- injuries;
- neuralgic diseases.
Each group of probable causes is characterized by specific additional symptoms (cough, shortness of breath, bluish skin, etc.), on the basis of which a diagnostic hypothesis is built.
When breathing
Sometimes the pain makes breathing difficult and intensifies with inhalation and exhalation. Causes of these symptoms:
- neuralgic pathologies;
- disorders in the gastrointestinal tract;
- cardiovascular disorders;
- diseases of the respiratory system.
But you should not engage in self-diagnosis; it is better to tell your doctor about such symptoms.
General recommendations
Diseases of the heart, respiratory system, gastrointestinal tract, musculoskeletal system and nervous system - all of this can act as factors that provoke pain in the middle of the chest.
In order not to trigger your own condition by allowing the development of a dangerous disease or a significant deterioration in well-being, you should take the following steps in time:
- Seek advice from a therapist who will prescribe the necessary set of studies and tests to exclude a number of pathological conditions.
- Change your eating habits by eliminating fatty, salty, and spicy foods from your diet. At the same time, you should eat fresh fruits and vegetables, dairy products, cereals more often, and drink more fluids.
- Introduce moderate physical activity into your lifestyle. It can be expressed in physical therapy classes, visits to the pool or yoga courses, leisurely walks in the park or jogging in the morning.
- Give up bad habits (frequently drinking coffee-containing drinks, smoking, drinking alcohol or using drugs). The organs of the respiratory and nervous systems, heart and blood vessels will definitely appreciate such care and respond with full-fledged work throughout many years of life.
- Eliminate stressful situations from your own life: to do this, you should change your overly nervous place of work or your own attitude towards such situations. To calm yourself, it won’t hurt to master breathing techniques, meditation and relaxation techniques.
Causes
The cause of nagging or burning pain in the middle of the chest can be diseases of the heart, blood vessels, respiratory system, trauma and many other factors.
Ask your question to a neurologist for free Irina Martynova. Graduated from Voronezh State Medical University named after. N.N. Burdenko. Clinical resident and neurologist BUZ VO \"Moscow Polyclinic\".Ask a question>>
Heart pathologies
Angina and myocardial infarction
Description of the disease Angina pectoris is characterized by severe, short-term chest pain. The cause of the pathology is obstruction of the arteries, in which the heart muscle receives less blood.
It is caused by atherosclerosis, functional disorders in the body, constant high blood pressure, smoking, and high cholesterol levels in the blood.
Myocardial infarction is a pathology of the heart muscle in which its blood supply is disrupted due to damage by atherosclerosis. The heart does not receive the required amount of oxygen, resulting in the death of a section of the heart. This phenomenon can be caused by complete blockage of the artery or blood clots. The probability of death in the first 2 hours after the attack is very high. Nature of pain Angina pectoris is a pathology characterized by short, dull pain that is repeated in short episodes. It most often manifests itself when the patient moves and exerts loads. The discomfort goes away after the person has rested.
, sharp, paroxysmal pain sensations occur, similar to angina pectoris, but the sensations are more intense and lasting. The patient has an attack even when he is lying down and at rest. The patient is bothered by a strong, inexplicable feeling of fear. The patient's breathing becomes faster, his limbs pulsate, and loss of consciousness is possible.
The skin turns pale, nausea occurs, the person sweats, and feels nauseous. Speech is impaired.
Localization
With angina and heart attack, the pain seems to compress the chest, irrigating into the left region of the sternum. It often radiates to the shoulder blade and arm.
Doctor's intervention
For consultation, diagnosis and treatment, the help of a cardiologist is required
Diagnostics
The disease is diagnosed using the following methods:
- ECG. When the arteries are narrowed, such a cardiogram will show deviations from the norm.
- Ultrasound of the heart.
- Echocardiogram with exercise
- Radioisotope scanning.
Treatment
To cure angina, you should reduce the number of attacks. To do this, the doctor lowers cholesterol in the blood, the patient needs to lose weight, give up bad habits, and reduce blood sugar levels. The patient needs to monitor his blood pressure and not be nervous.
All these measures will help reduce the number of relapses.
- Treatment with medications. The patient is prescribed beta blockers and calcium channel blockers as medications. They will prevent the arteries from narrowing, and products containing nitroglycerin will increase local blood circulation, dilating the blood vessels.
- Surgical intervention. In complex and advanced cases, doctors suggest coronary bypass surgery. The operation allows the blood entering the heart to continue its path past the affected vessel. Doctors offer another surgical option - angioplasty. The surgeon places a special catheter, which inflates mechanically, expanding the narrow vessel, facilitating the passage of blood through it.
Acute pericarditis
Description of the disease Inflammation of the pericardial sac, which is characterized by pain in the chest, aggravated by breathing.
It can be caused by bacteria, and often occurs with rheumatism, kidney disease, pneumonia, heart attack and tuberculosis. Nature of pain
Painful sensations can be dull or sharp, they can be intense, and intensify with inhalation, movement, or a sudden change of posture. They can last for several days, and heart murmurs appear. The patient's pulse and blood pressure do not change, but shortness of breath appears.
Localization
Pain on the left side in the chest, irrigating to the area of the shoulder blades.
Doctor's intervention
The disease is treated by a therapist and a cardiologist.
Diagnostics
The disease can be diagnosed based on an ECG and blood tests for the level of aspartic aminotransferase. Using an x-ray, the doctor will see changes in the pericardium.
In some cases, the doctor takes a puncture to identify the disease.
Treatment
Treatment methods depend on the type of pathology and their nature. In the acute form of pericarditis, hospitalization should be carried out, and the chronic course of the disease can be treated on an outpatient basis.
- Diet. A balanced diet with limited animal fats. The patient should not drink alcohol; the amount of salt and water consumed should be reduced.
- Treatment with anti-inflammatory drugs to eliminate symptoms of the disease. Therapy is also used to relieve pain.
- The use of diuretics to remove fluid, antibiotics, and antifungals.
- Stimulation of immunity.
- The operation is used when the patient has severe consequences and the inflammatory process threatens the patient’s heart, for example, purulent phenomena, “shell heart”.
Atrial fibrillation
Description of the disease
Atrial fibrillation is characterized by a disturbed heart attack , periods of excitation and contraction of the patient's atria and individual muscle fibers. Heartbeats increase to 600 per minute. If the attack continues for more than 2 days, the patient develops ischemic disease. Blood clots may form. In chronic cases, there is a disturbance in the blood supply to the heart.
Nature of pain
In some cases, the pathology occurs without any symptoms , but most often a person begins to experience chest pain and heart rate increases. Interruptions in the functioning of the heart and cardiac arrest are possible.
The patient becomes weaker, dizzy, sweating increases, shortness of breath occurs, and the patient begins to choke. With constant heart disease, the muscle becomes exhausted, congestion occurs in the internal organs, and shortness of breath occurs when climbing stairs. At night, the patient may experience pulmonary edema, attacks of suffocation with wheezing.
The patient may lose consciousness, there may be paralysis of the limbs, a sharp drop in blood pressure, and respiratory and cardiac arrest.
Localization
The pain is localized in the heart area, radiates to the arms, less often to the jaw or peritoneum.
Doctor's intervention
Treatment requires treatment prescribed by a cardiologist.
Diagnostics
The doctor recognizes atrial fibrillation visually by examining the patient, counting the pulse, and hearing wheezing in the patient’s lungs. During an attack, the patient's blood pressure drops sharply.
If the doctor finds it difficult to make a diagnosis, he prescribes:
- ECG
- Holter monitoring
- Ultrasound of the heart with Dopplerography.
- X-ray of the sternum
- CT scan
- MRI
Treatment
- Treatment with drugs occurs through the administration of thrombolytic enzymes, diuretics, beta-blockers, anticoagulants and other medications. The course of treatment lasts several years.
- Surgical intervention. Patients are recommended to do breathing exercises to even out their heart rate.
- Specially developed exercise therapy complex
- Operation. This method is used in cases where all other methods are ineffective. Catheter ablation is aimed at cauterizing the damaged area. Ablation with a pacemaker is characterized by transferring the heart's work to an artificial pacemaker. Sewing in a defibrillator is used to eliminate an attack of arrhythmia. Labyrinth-type surgery redirects current pulses to normalize heart function.
- Folk recipes. These are compositions made from natural ingredients: viburnum, yarrow, dill seeds, walnuts, honey, etc.
Mitral valve prolapse syndrome
Description of the disease
The pathology
is characterized by disruption of the left ventricular valve of the heart (proliferation of valve tissue, myxomatous degeneration). There are no violations in other organs. The process involves the posterior or anterior leaflet of the left valve. Sometimes accompanied by deformation of the bone tissue of the sternum.
May be caused by coronary heart disease or rheumatism of the heart in the chronic stage.
Nature of pain
Characterized by periodic pain in the middle of the chest. In the early stages it is often asymptomatic and is detected during a medical examination. The patient is unwell and his temperature rises to 37.5 degrees for a long period of time. Sweating increases, and migraine attacks begin in the morning and evening. At night, the patient may choke, taking deep, convulsive breaths. Pain that begins in the heart area is not relieved by medications, and arrhythmia begins. Doctors detect the presence of a heart murmur.
Localization
The pain manifests itself in the heart area, radiating to the middle of the chest.
Doctor's intervention
To prescribe treatment, consultation with a cardiologist and therapist is necessary.
Diagnostics
Ultrasound, echocardiography, and electrocardiography are used for diagnosis.
Treatment
- It is necessary to normalize the daily routine, sleep at least 8 hours, and do not overload the body with physical activity.
- A course of psychotherapy, auto-training, acupuncture, and electrophoresis help well.
- Spine massage
- Doctors prescribe beta blockers, cardiotrophics, sedatives
- A course of antibiotics may be prescribed
Pathologies of large vessels
Aortic dissection
Description of the disease
Aortic dissection is a dangerous pathology that can result in death for the patient. It is characterized by damage to the walls of the aorta, creating an extra channel.
A complication may be bulging of the walls of blood vessels in places where they become less durable.
Nature of pain
The pain is sharp, intense, occurs suddenly, the patient may have numb legs (usually the left). The pain is described by patients as tearing. If during angina pectoris the pain tends to subside, then these unpleasant sensations continue both at rest and when changing positions.
The patient's blood pressure increases sharply and then decreases, and sweating becomes stronger. The pulse is asymmetrical, the person feels tired and weak. The skin acquires a bluish tint and turns pale. Shortness of breath appears, the person wheezes and breathes noisily. Sometimes the dissection leads to loss of consciousness and coma.
Localization
The pain begins in front of the sternum (proximal dissection), pain behind the chest or behind the scapula most often manifests itself with the distal nature of the pathology.
As the aorta dissects, pain begins in the neck, jaw, between the shoulder blades, and radiates into the back and groin.
Doctor's intervention
Urgent treatment by a vascular surgeon is needed; the pathology can mainly be corrected only by surgery.
Diagnostics
To diagnose the disease, doctors use the following methods:
- X-ray of the sternum
- Transesophageal echocardiography
- CT angiography
- magnetic resonance angiography
- ECG
- Blood tests
Treatment
The main treatment for aortic dissection will be urgent hospitalization in intensive care and surgery . Doctors relieve pain and bring a person out of shock with analgesics or narcotic substances.
The patient's condition is stabilized. In rare uncomplicated cases, drug treatment is possible. If other types of treatment are ineffective, then the patient undergoes surgery, plastic surgery of the aortic valve, prosthetic valve replacement, and coronary artery transplantation.
Pulmonary embolism
Description of the disease
This is a blockage of the arteries of the lungs with a blood clot, often a consequence of labor, and begins after operations, lung injuries, etc. The pathology is in second place in terms of deaths after cardiovascular diseases and oncology. The disease is difficult to diagnose and is associated with such a high mortality rate. When autopsying the bodies of patients, statistics show that in half of them the disease was not diagnosed.
With timely treatment of the disease, the number of deaths is reduced to 10%.
Nature of pain
The symptoms of this pathology are very diverse, which complicates diagnosis. It all depends on the speed of development of negative processes in the lungs, the stage of the disease and the prerequisites that caused pulmonary embolism.
Painful sensations depend on the location of the thrombus, for example, if it is in a large artery, then the patient may experience only shortness of breath and nothing more, and when small vessels are blocked, the pain is sharp, burning, intense.
The person suddenly develops shortness of breath. A strong heartbeat begins, the patient’s skin turns pale and gray, intestinal function is disrupted, and tension occurs in the abdominal region. The aorta pulsates, heart murmurs begin, and pressure drops.
The veins of the neck and abdominal region fill with blood and begin to bulge.
Localization
Pain sensations are localized in the middle of the chest, similar to signs of pleurisy.
Doctor's intervention
Treatment requires the intervention of a vascular surgeon.
Diagnostics
The following methods are used for diagnosis:
- ECG
- X-ray
- CT scan
- MRI
- Echocardiography
- Ultrasound examination of veins
- Scintigraphy
Treatment
- Drug treatment: intravenous fraxiparin, sodium heparin; oral warfarin;
- Using medications to dissolve blood clots, such as streptokinase, urokinase, alteplase.
- Doctors can use the following measures: chest compressions, oxygen therapy, artificial ventilation, administration of saline solutions through droppers.
- Operation. This may be the elimination of an embolus or an arterial wall with a plaque. Plastic surgery of the heart is often necessary due to stretching of the right ventricle.
- Installation of a vena cava filter, which allows for disease prevention.
Respiratory diseases
Laryngotracheitis, bronchitis
Description of the disease
These are inflammatory diseases that develop as a result of infection, accompanied by cough, chills, and difficulty breathing.
Nature of pain
The pain can be sharp or dull, but it certainly intensifies when coughing. The patient complains of a sore throat, a sore throat, a painful cough that causes pain.
The cough is dry due to swelling of the vocal cords, the temperature rises, and the sputum is thick. The larynx dries up, and there is hoarseness in the voice.
Possible enlargement of the lymph nodes in the neck.
Localization
Pain begins behind the chest when coughing.
Doctor's intervention
This disease is treated by a pediatrician, pulpologist, and otolaryngologist.
Diagnostics
The doctor identifies the disease based on a visual examination of the patient, when the patient complains, or by listening. If necessary, X-rays, computed tomography, and MRI are performed.
Blood and sputum smears are analyzed. Sometimes a biopsy of the laryngeal mucosa is done.
Treatment
- Gentle mode for the vocal cords
- A diet with no pickles, hot or cold foods, or spicy seasonings. Supplemented with plenty of alkaline drinking.
- Drug treatment with antiviral drugs (cyclofen, Ingavirin); antibiotics (Flemoclav, Azithromycin); antihistamines (Zyrtec, Suprastin); drugs that relieve inflammation (Paracetamol).
- Be sure to use cough medicines (Sinekod, Codelac) and expectorants, mulocilitics (Mukaltin, Doctor Mom).
- Use of homeopathic remedies.
Pleurisy
Description of the disease Inflammation of the pleura (the membrane that protects the lungs) due to bacteria (streptococci, fungi, pneumococci, etc.), injuries, tuberculosis, allergic reactions.
Nature of pain
Painful sensations can often be confused with heart pain ; doctors rule out the possibility of a heart attack using an ECG. When a person lies on the affected area, the discomfort decreases. The nature of the pain is intense, the patient’s temperature rises, it is difficult for him to breathe, and the cough also occurs with pain.
The patient's pulse becomes rapid.
Localization
Usually the pain is localized behind the sternum and becomes stronger when inhaling and exhaling. In atypical forms, irrigation into the abdomen is possible, so sometimes pleurisy can be confused with an attack of appendicitis.
Doctor's intervention
The disease is treated by a pulpologist.
Diagnostics
- To diagnose the disease, an x-ray is necessary to identify dark spots and fluid accumulations.
- Puncture of fluid in the pleura
- Blood biochemistry
- Pleural biopsy
- Patient examination
- Listening to the lungs
- Palpation of the chest
Treatment
- The patient must be kept in bed and wiped with a damp cloth soaked in warm water.
- Relieving inflammation with hormonal, antibacterial, decongestant medications.
- Symptomatic treatment: reducing temperature with antipyretics, pain relief with analgesics, increasing the body's defenses with immunostimulants.
- Physiotherapy with warming of the sternum
- Pumping out the contents of the pleura, which does not eliminate compression of the internal organs
- Local treatment: rubbing rubs, applying compresses and bandages.
- Recovery with the help of exercise therapy, yoga, taking vitamins and minerals, good nutrition.
Cancer (lung, bronchi, pleura, metastatic lesions of lymph nodes)
Description of the disease
A malignant neoplasm of the lungs, which is caused by inhalation of carcinogens, smoking, and hazardous production .
Nature of pain
In the early stages, the disease is asymptomatic; it simply looks like bronchitis in the chronic stage or an acute respiratory viral infection. Therefore, cancer is often diagnosed at an advanced stage of the disease. In the central form of oncology, the pathology manifests itself more quickly due to breathing problems.
First, a dull pain in the chest begins, which occurs periodically; then the pain becomes so strong that the person cannot sleep; only narcotic substances alleviate the condition. The cough is often accompanied by bloody sputum, visually similar to pink or red jelly. Shortness of breath begins.
The patient feels dizzy, has a fever, and loses weight.
Localization
The pain is localized in the chest at the site of the disease, but when the tumor grows, it can begin in the region of the ribs, in the area of nearby internal organs.
Doctor's intervention
An oncologist treats the disease.
Diagnostics
Cancer is diagnosed using the following methods:
- X-ray in two projections
- Fluorography
- Bronchoscopy
- CT
- MRI
- Mediascopy
- Biopsy of lymph nodes, internal organs
Treatment
- Surgical intervention
- Chemotherapy aimed at suppressing the growth of tumor cells. It is done with the help of Vincristine, Carboplatin, Irinotecan, Etoposide.
- A course of radiation therapy. Basic techniques: technology (IGRT) (irradiates affected cells, corrects, transfers loads to another area of tissue); brachytherapy (moving agents to cells that enhance their effect); “smart knife” (precise effect of the cyber knife on the affected cells).
- Hormonal correction
- Immunotherapy
Diseases of the gastrointestinal tract
Gastroesophageal reflux disease (GERD)
Description of the disease
Chronic pathology of the gastrointestinal tract, resulting from periodic reflux of food into the esophagus with subsequent damage to the mucous membranes and nearby organs (bronchi, pharynx, trachea).
Nature of pain
The patient complains of heartburn and sour belching. Painful burning sensations often begin when swallowing and after eating; in rare cases, vomiting occurs, followed by hiccups. The patient may complain of chest pain, similar to a heart attack or angina.
At night, due to being thrown into the esophagus, the patient begins to cough, his throat becomes sore, hoarseness occurs, and bronchitis or asthma may develop.
Symptoms intensify with physical activity and after eating.
Localization
Burning pain, accompanied by heartburn, is localized in the epigastric region and irrigates to the cervical region and shoulders. Starts 1-2 hours after eating. May become stronger after drinking soda or when moving.
Doctor's intervention
For diagnosis and treatment, consultation with a therapist and gastroenterologist is necessary.
Diagnostics
- Proton pump inhibitor test.
- Intrafood pH monitoring
- Fibroesophagogastroduodenoscopy
- Chromoendoscopy of the esophagus.
- ECG
- Ultrasound of internal organs
- X-ray.
- Blood and stool tests
Treatment
- Surgery is necessary only in extreme cases.
- Compliance with diet and special recommendations. Hot dishes are excluded from the diet, you should not eat a lot of food for dinner, eat citrus fruits, chocolate and fatty foods. You should not bend forward sharply after eating; wearing tight clothes and corsets is not recommended, so as not to increase intra-abdominal pressure.
- Weight loss is recommended if you are obese.
- You can’t take antispasmodics or prostaglandins.
- Course of medications: antacids (Almagel), prokinetics (Motilium).
Esophagitis
Description of the disease
This is a pathology characterized by inflammatory processes of the mucous membranes. If the disease is not treated, complications will include peptic ulcers and perforation of the esophagus. There are different types of pathology: the disease can be both acute and chronic. It affects the superficial or deep layers of the mucosa.
Damage to the esophagus can be complete; in some cases, inflammation extends only to the upper or lower section.
Nature of pain
The manifestations of pain depend on the inflammatory process. For example, with catarrhal form, the esophagus is sensitive only to cold and hot foods. In severe forms, intense burning pain appears. When swallowing, pain also begins. The patient complains of increased salivation, heartburn, and possible bouts of vomiting blood. Then the symptoms disappear, but within 3 months scars appear on the walls of the esophagus.
Localization
Pain is felt behind the sternum and can radiate to the cervical spine and back.
Doctor's intervention
To treat the disease, consultation with a surgeon and gastroeterologist is necessary.
Diagnostics
- X-ray
- esophagoscopy,
- endoscopic mucosal biopsy
- Histological examination
- Esophagomanometry
Treatment
- Taking medications: antacids and drugs from the famotidine group.
- Diet excluding alcoholic beverages and foods that increase the secretion of gastric juice
- Course of antibiotics
- Avoidance of tranquilizers and sedatives
- Physiotherapy (electrophoresis, mud therapy).
- Operation. It is done in extremely severe cases of scarring of the esophageal tissue.
Foreign bodies of the esophagus
Description of the disease
Foreign bodies in the esophagus are not so common , but coins, bones, dentures, food, and small parts of toys that get into it require quick help. Objects can get stuck in it due to the large volume of the object compared to the lumen of the esophagus, tumor, etc.
Nature of pain
If toys do not have sharp edges, then parents often have no idea that the lost object is stuck in the esophagus. When a body with sharp edges enters the esophagus, severe salivation is observed. Such children refuse food and do not want to turn their heads again. When exposed to bodies with a smooth surface, the patient may cough, drink, but not eat thick food.
Breathing disturbances are observed.
The patient feels thirsty and loses weight from lack of water. When an object is in the upper part of the esophagus, the larynx moves forward and becomes wider. If you palpate in front of the larynx, aching pain occurs, which goes away as soon as the doctor removes his fingers. The patient is shivering and may have a fever
Localization
Pain develops below the place where the foreign body has entered
Doctor's intervention
For consultation and diagnosis, you may need the help of a surgeon and therapist.
Diagnostics
- Visual examination of the patient
- Esophagoscopy
- X-ray
- CT
- Fistulography
Treatment
The main measures that a doctor can take are to remove the object. This can be done in a gentle way with the help of coating substances, a special diet, and rinsing with furacillin.
If the foreign body is not removed, then endoscopy must be performed with removal under general or local anesthesia.
Stomach ulcer
Description of the disease
This is a chronic disease with frequent relapses . With it, defects are formed in the stomach with penetration under the mucous membranes. The disease alternates between periods of remission and exacerbation.
Nature of pain
The clinical picture of the pathology can be different; it depends on the patient’s pain threshold, the stage of the disease, the location of the lesion, and the individual characteristics of the person. The nature of the pain can be constant or periodic (at night, after eating). The pain observed in the patient can be nagging, dull, sharp, etc. Its intensity also varies: from severe to barely noticeable pain.
The patient complains of heaviness in the abdomen after eating, belching, heartburn, decreased appetite and delayed bowel movements.
Localization
Pain is observed in the left side of the chest, radiating to the arm or back, ribs, lower back, and pelvic area.
Doctor's intervention
Treatment requires consultation with a surgeon and gastroenterologist.
Diagnostics
The disease is detected using a blood test, fibroesophagogastroduodenoscopy, x-ray, pH-metry and 24-hour monitoring of the pH of gastric juice.
Treatment
- A course of antibiotics (Amoxicillin, Tetracycline).
- Treatment with antisecretory drugs that neutralize hydrochloric acid (Maalox).
- Taking Ranitidine, Omeprazole, Sucralfate, De-nol, etc.
- It is recommended to take antidepressants and tranquilizers.
- To relieve pain, antispasmodics, for example, no-spa, are used.
- Treatment with probiotics is prescribed, for example, Linex.
Be sure to watch the next video
Causes of chest pain: diagnostic steps
You can follow this simple algorithm of actions:
- take a Nitroglycerin or Aspirin tablet (which it is advisable to always have with you);
- take a lying position;
- unbutton clothes that interfere with breathing;
- organize access of fresh air into the room;
- use breathing techniques (for example, take a deep breath - cough, inhale again and forcefully cough again).
Regardless of the causes of pain in the middle of the sternum, which causes panic, you should control yourself without falling into captivity of phobias and worries. A timely examination by a doctor and following his recommendations will save your own health and life.
In case of acute excruciating pain, you must immediately call an ambulance. It is necessary to exclude such causes as myocardial infarction, dissecting aneurysm, pneumothorax, pulmonary embolism, dry pleurisy and spontaneous mediastinal emphysema.
History taking
When clarifying the history of the disease, pay attention to the following features:
- thrombophlebitis can cause pulmonary infarction or pulmonary embolism;
- tuberculosis, emphysema, connective tissue diseases can be complicated by spontaneous pneumothorax;
- pneumonia or lung abscess accompanied by fever and chills;
- The cause of sudden pain is often herpes zoster and intercostal neuralgia.
Chest pain: types of pain, what to do
Pain in the chest indicates a problem in the body; such a signal cannot be ignored. To prevent possible future problems, it is important to identify and eliminate the cause of the failure in a timely manner.
What does chest pain mean?
This condition is called thoracalgia in medical practice. The term is created on the basis of the Latin word “thorax”, which translated into Russian means chest, as the upper part of the skeleton of the body, or the thoracic spine.
Doctors hear complaints about pain in this area not only from the elderly, but also from people in the prime of life. This is the second reason for seeking medical help after abdominal pain.
The first thing that comes to a person’s mind when obvious chest pain appears is dysfunction of the cardiovascular system.
But in reality, there are many reasons why the chest may hurt. There can be several of them, intertwined at the same time. Any type of chest pain, regardless of the cause of its occurrence, negatively affects the quality of life.
Some of them are short-term pain, they do not pose a danger, and are not a cause for concern. Some species can signal the development of conditions that threaten the health and life of the patient.
Thus, severe and sharp pain in the chest, reminiscent of an attack, requires emergency medical attention.
To differentiate dangerous pain that cannot be postponed from the physiological norm, you should answer a number of questions:
- in what exact place (or area) is pain or discomfort felt in the chest area;
- what type of pain, its distribution;
- how long does the chest hurt;
- what serves as a provoking factor;
- what symptoms accompany the painful condition.
What can hurt your chest?
The variety of reasons why the chest hurts and the complexity of the solution is explained by anatomy coupled with physiology. This osteochondral formation, an important element of the body’s defense, has the structure of a closed hollow space.
Her skeleton is formed:
- ribs connected to the spinal column (12 thoracic vertebrae);
- the sternum, which protects vulnerable lungs, heart, liver, esophagus, and important arteries from injury and damage;
- muscular frame;
- the diaphragm, which plays a major role in the respiratory process;
- ligamentous apparatus.
Potentially, all of these organs and areas can be a source of pain. When analyzing what else can cause chest pain, you should remember the anatomical features of the female body and her reproductive system.
In women, the cause of pain in the sternum may additionally be:
- physiological pain that occurs as a reaction of the nervous system in response to various stimuli that damage or destroy the glandular and connective tissue of the female breast. The mammary glands of a woman are abundantly penetrated with nerve fibers;
- breast diseases - oncology, infectious inflammation, fibrocystic diseases;
- cyclical changes in hormonal levels - during menopause or associated with the menstrual cycle (changes in the neurohumoral regulatory system, in the ovaries, uterus, and other internal genital organs);
- the onset of pregnancy;
- chest injuries, surgical interventions.
The term “mastalgia” is used to refer to a feeling of discomfort or pain localized in any part of the mammary gland. This collective concept is not a diagnosis, but a clinically significant symptom complex.
Another reason why chest pain in men is gynecomastia, a benign enlargement of the mammary gland. It is often observed in former athletes who abruptly stopped training, men with tumor diseases, and disorders of the endocrine glands.
The risk group also includes men who use hormonal, antipsychotic drugs, and tranquilizers for a long time.
Etiology of chest pain
Chest pain is accompanied by many diseases and disorders.
Depending on the causes of discomfort, it is customary to distinguish 2 types of pain syndrome:
- Vertebrogenic – caused by pathology of the spine or surrounding tissues. Occurs as a result of compression, irritation of the nerve roots of the branches of the thoracic spinal nerves or due to excessive muscle tone. Most often it is provoked by osteochondrosis or herniated intervertebral disc. The reason that the chest hurts can also be instability or fracture of the vertebrae, thoracic or cervical spondylosis, radiculitis, tumors, ankylosing spondylitis, spinal stenosis, trauma, spondyloarthropathy, types of degenerative-dystrophic and infectious lesions.
- Nonvertebrogenic – associated with diseases of internal organs, blood vessels, or is psychogenic in nature. The main cause of pain in the sternum or heart area is deterioration of coronary circulation, angina pectoris, myocarditis. Thoracalgia is accompanied by cardiac ischemia, rheumatism, pericarditis, and myocardial necrosis. Non-vertebral syndrome is caused by aortic aneurysm, pulmonary artery blockage, neuroses, panic manifestations, respiratory diseases, inflammation of the gastrointestinal mucosa, pancreatitis, tumor diseases, hernia or spasm of the esophagus, and stomach ulcers.
How to recognize the cause of pain
To decide what to do if your chest hurts, whether to call an ambulance, you need to diagnose the condition of your body and try to independently determine the cause of the pain based on the symptoms. The origin of pain can be judged by its nature, intensity, localization and by what other symptoms predominate in the clinical picture.
First of all, you should pay attention to the time factor.
What signs allow you to exclude cardiology and suspect neuralgia:
- constant pain that persists day and night, may subside in the morning and intensify when walking;
- the place where discomfort is felt usually exactly corresponds to the localization of the pathological process. The phenomenon of irradiation may be observed, when the process of excitation spreads to other nerve centers and responds in the lower back and shoulder girdle. In such cases, there is a characteristic increase in pain during physical activity, laughing, sneezing, deep breaths, coughing;
- when pressing on points located along the spine, pain begins to be felt or its intensity increases;
- local increase in temperature, hyperemia;
- muscle pain that increases when bending the body forward, lifting or stretching the arms, turning the shoulders;
- pinched nerve is accompanied by numbness of the area in which the compression occurred;
- the painful condition is a one-time one, associated with a certain action or situation - excessive overload, hypothermia, a cold, as well as with an unsuccessful movement or a sharp bend, or injury.
With heart ailments, clear local pain is rarely observed; there is predominantly reflected periodic pain, which does not last constantly and often manifests itself in attacks. What symptoms should you pay attention to?
So, if:
- the chest is burning, aching, there is a connection with food intake - gastritis, ulcers, colitis or pancreatitis are diagnosed. The violation is accompanied by heartburn, belching, and stool upset;
- pain in the center of the chest or in the upper part - a cold, most likely bronchitis, or heart problems;
- it hurts above the chest - it can be assumed that it is a consequence of drafts and heavy lifting;
- aching chest, monotonous pain in the chest, breathing hard, perhaps increased sweating, dizziness, but no other obvious symptoms are detected - this is how stress, anxiety, negative emotions, neuroses usually manifest themselves;
- constant pressing, sometimes piercing pain not associated with breathing (especially in the area of the mammary gland) - the situation should be alarming, because this may be a sign of the formation of a malignant tumor;
- paroxysmal pain that occurs behind the chest, lasting 3-5 minutes, a feeling of pressure, burning, compression in the cardiac region or more widely on the left - probably angina pectoris, often against the background of emotional stress or physical overload.
How to treat and what to do for chest pain
Only a qualified physician can accurately determine the root cause of the pain syndrome by conducting a survey, an initial examination, and laboratory and diagnostic tests.
Each specific situation requires the use of its own specially selected treatment regimen.
Which doctor to contact: patients with complaints of chest pain are helped by a therapist, a neurologist, a cardiologist, and, if necessary, a specialized doctor - a pulmonologist, gastroenterologist, oncologist.
As first aid, the patient should stop, calm down, provide fresh air, take validol, nitroglycerin, or other medicine prescribed by the doctor. You should know that for neuralgia, vasodilators do not work; analgesics (usually in the form of ointments, suppositories, patches) are used to alleviate the condition.
What to do with chest pain: if this is not a manifestation of scoliosis, but the result of the influence of psychological factors, sedatives and psychotropic drugs can help.
Conditions requiring emergency response:
- dull, prolonged pain lasting from half an hour to a day or more, when the entire front part of the chest hurts, while taking nitroglycerin preparations does not lead to regression - myocardial infarction;
- irradiation to the left hypochondrium, shoulder, armpit, neck, jaw;
- unbearable cutting pain in any area;
- severe bursting pain (often swelling of the upper limbs, neck), wandering along the spine, indicates a thoracic aortic aneurysm. If a slow pulse, cyanosis, or fainting are observed, this indicates aortic dissection, a process that is fatal;
- sudden acute pain when breathing, coupled with cough, fever, coughing up sputum with blood - pulmonary embolism, life-threatening. May lead to pulmonary infarction, persistent hypotension, shock;
- additional manifestations - lack of air, lump in the throat, impaired consciousness, palpitations, persistent increase or decrease in blood pressure, vomiting.
In any case, you should not postpone visiting a doctor; treatment should be timely and comprehensive.
Source: https://proartrit.ru/bol-v-grudnoy-kletke/
Other development factors
Discomfort, especially nagging pain in the sternum, is not always the result of cardiac pathologies. In 40-50% of situations, the cause is not related to the muscle organ at all.
- Gastritis and stomach ulcers. In the first case, we are talking about inflammation, in the second - about the formation of erosions on the mucous membrane. Both conditions can cause referred discomfort. The chest appears to be the main target.
- Reflux esophagitis. Rejection of acid back into the esophagus. With a long course of the pathological process, persistent aching pain occurs in the epigastric region; acute discomfort is not typical.
- Sternum injuries. Fractures give the most sharp, pronounced sensations.
- Pneumonia or pneumonia. Infectious origin. From the left side. Characterized by severe, pressing pain. Nitroglycerin has no effect.
- Osteochondrosis. Degenerative-destructive disease of the spinal column.
- Disc herniation (extrusion).
- Myositis or inflammation of skeletal muscles.
- Intercostal neuralgia. A common cause of discomfort.