Bronchoscopy is one of the most informative instrumental methods for examining the tracheobronchial tree, which allows not only to establish a diagnosis, but also, if necessary, to carry out a number of therapeutic measures (sanitation, removal of a foreign body, taking swabs, etc.). Before performing bronchoscopy it is mandatory
An X-ray or CT scan of the chest organs is performed.
Bronchofibroscopy allows with an accuracy above 97%
diagnose lung cancer, pneumonia of any type, chronic bronchitis and other diseases of the respiratory system.
In the diagnostic department of the Central Clinical Hospital of the Russian Academy of Sciences in Moscow, you can perform a bronchoscopy at any time convenient for the patient at an affordable price. Important: endoscopy of the lungs, bronchi or trachea must be performed by an experienced specialist in conditions equipped with advanced anesthesia and diagnostic equipment. This way, the patient can count on the absence of discomfort and guaranteed informative results.
Carrying out
Endoscopic examination of the lungs
and other organs of the respiratory system is carried out as follows:
- The patient is given drugs that have a bronchodilator effect to facilitate passage of the bronchoscope.
- The patient is seated in a special chair equipped with advanced anesthesia equipment.
- Anesthesia of the larynx and vocal cords is performed.
- The bronchoscope is inserted during a deep breath. Further, its passage through the respiratory tract is performed with careful rotational movements.
- During the examination, necessary manipulations can be performed - treating organs with medicinal solutions, collecting material for a biopsy, etc.
- After the examination, the bronchoscope is carefully removed, after which the patient is not recommended to eat or shop for 2 hours.
Bronchoscopy
Tracheobronchoscopy (full name of the procedure) is a modern diagnostic and treatment method for visualizing the internal surfaces of the trachea and bronchi.
The examination is performed with a special optical device – a fiberoptic bronchoscope. Essentially, this is a multifunctional endoscope, which consists of a flexible cable with a light source and a video/photo camera at the end and a control handle with an additional manipulator.
Indications for bronchoscopy
The decision to perform bronchoscopy is made by a pulmonologist. He also determines the scope and frequency of the examination, taking into account the preliminary diagnosis and age of the patient.
Bronchoscopy is prescribed in the following cases:
- Darkening (disseminated lesions) on x-rays;
- Suspicion of cancer;
- Suspicion of the presence of a foreign body;
- Chronic shortness of breath not associated with diseases of the cardiovascular system or bronchial asthma;
- Hemoptysis;
- Abscesses or cysts in the lungs;
- Long-term recurrent pneumonia;
- Protracted inflammatory processes in the bronchi;
- Bronchial asthma (to determine the cause);
- Abnormal expansion or narrowing of the lumen of the bronchi;
- Monitoring the condition of the upper and lower respiratory tract before and after surgical treatment.
Manipulations that can be additionally performed during the procedure:
- selection of pathological contents to determine sensitivity to antibiotics;
- biopsy – collection of biomaterial for histological analysis;
- administration of a contrast agent necessary for other diagnostic procedures;
- removal of foreign bodies;
- washing the bronchi from pathological contents (sputum, blood);
- targeted administration of drugs (directly to the area of inflammation);
- elimination of abscesses (foci with purulent contents) by drainage (suction of fluid) and subsequent introduction of antibacterial drugs into the inflamed cavity;
- endoprosthetics - installation of special medical devices to expand the lumen of abnormally narrowed airways;
- determining the source of bleeding and stopping it.
Bronchoscopy is performed even on newborn children, but in this case it is performed to examine only the upper respiratory tract and only under general anesthesia.
Contraindications
There are also a number of contraindications to this procedure, the absolute ones of which are:
- stenosis of the larynx and trachea 2 and 3 degrees;
- respiratory failure 3rd degree;
- exacerbation of bronchial asthma.
These three conditions carry a risk of bronchial injury when the endoscope is inserted.
- Aortic aneurysm - nervous overstrain of the patient and manipulation with the endoscope can provoke rupture of the aneurysm.
- Heart attack and stroke less than 6 months old;
- Bleeding disorders;
- Mental illnesses (schizophrenia, psychosis, etc.). Stress and acute lack of oxygen during the procedure can significantly worsen the patient’s condition, causing another attack of the disease.
- Individual intolerance to painkillers. A reaction to them can provoke an allergy in any degree of its manifestation, up to the most severe – anaphylactic shock and suffocation.
Among the relative contraindications - conditions in which it is desirable to postpone the procedure to a later date, are:
- acute course of infectious diseases;
- menstrual bleeding (due to decreased blood clotting during this period);
- asthmatic attack;
- 2-3 trimester of pregnancy.
However, in cases of resuscitation (emergency), bronchoscopy is performed regardless of the presence of contraindications.
Preparation for bronchoscopy
Before bronchoscopy, it is necessary to undergo a number of diagnostic tests:
- radiography of the lungs,
- ECG (electrocardiogram),
- blood tests (general, for HIV, hepatitis, syphilis),
- coagulogram (blood for clotting)
- and others according to indications.
You can take mild sedatives the night before;
Dinner should be no less than 8 hours before the procedure;
On the day of the study, smoking is prohibited (a factor that increases the risk of complications);
Bronchoscopy is performed strictly on an empty stomach;
In the morning, do a cleansing enema (prevention of involuntary bowel movements due to increased intra-abdominal pressure);
It is recommended to empty your bladder immediately before the procedure.
If necessary, the doctor will prescribe mild sedatives on the day of the procedure. Patients with bronchial asthma must have an inhaler with them.
For people suffering from cardiovascular pathology, preparation for bronchoscopy is carried out according to an individually developed program.
Methodology
The duration of bronchoscopy is 30-40 minutes.
Bronchodilators and painkillers are administered to the patient subcutaneously or by spraying, facilitating the advancement of the tube and eliminating discomfort.
The patient's body position is sitting or lying on his back.
It is not recommended to move your head or move. To suppress the urge to vomit, you need to breathe often and not deeply.
The bronchoscope is inserted through the oral cavity or nasal passage.
In the process of moving to the lower sections, the doctor examines the internal surfaces of the trachea, the slit and the bronchi.
After the examination and the necessary manipulations, the bronchoscope is carefully removed, and the patient is sent to the hospital for some time under the supervision of medical staff (to avoid complications after the procedure).
Feelings after bronchoscopy
Feelings of numbness, a lump in the throat and nasal congestion will persist for up to 30 minutes. During this time and after another hour, it is not recommended to smoke or eat solid food. Also, doctors do not recommend driving a car on this day, since the administered sedatives can impair concentration.
Decoding the research results takes only 10-15 minutes, since the image from the video/photo camera on modern devices is of very high quality.
The specialist has the opportunity to view the image on a computer monitor in real time and print it on paper.
The result of bronchoscopy is assessed by a pulmonologist, and then, if necessary, he prescribes a course of treatment for the patient.
Possible complications
The risk of negative consequences, although minimal, is possible. Therefore, you should immediately consult a doctor if you notice the following symptoms:
- hemoptysis for a long time;
- pain in the chest;
- audible wheezing;
- feeling of suffocation;
- nausea and vomiting;
- rise in body temperature.
These symptoms may be signs of pneumothorax, bronchial injury, bronchospasm, pneumonia, allergies, bleeding, etc.
Bronchoscopy is considered relatively safe, the most modern and most informative diagnostic procedure.
Timely and high-quality implementation of the procedure, competent interpretation of the study results allow us to establish the correct diagnosis with 100% accuracy and prescribe adequate treatment.
Or refute assumptions about the presence of a disease, thereby avoiding a medical error and saving the patient’s health, and sometimes even life.
Source: https://www.diagnos.ru/procedures/manipulation/bronhoskopia
What is this procedure?
Bronchoscopy is a procedure that allows the doctor to examine the inside of the bronchi, which are the main passages for air into the lungs. During the procedure, the doctor inserts a thin bronchoscope through the nose or mouth, which transmits an image to an eyepiece or monitor. The images are used to diagnose infections, tumors, bleeding and other lung diseases. A bronchoscope can also be used to remove foreign objects, administer medications, place stents in the airways, or perform biopsies.
Possible side effects
After bronchoscopy, the throat feels numb for half an hour, and the voice becomes hoarse or nasal. You may expect to cough up dark brown mucus for a couple of days after the procedure. This should not be a cause for concern, but if you cough up bright blood, you should contact your doctor immediately. Damage to the bronchial wall is possible as a result of inaccurate insertion (removal) of the bronchoscope or improper behavior of the patient during the procedure. It is extremely rare that a perforation of the lung is observed during bronchoscopy; in such cases, surgery is performed. In rare cases, inflammatory diseases of the respiratory tract are possible due to infection during bronchoscopy; this is manifested by fever, cough, and chest pain a few days after the procedure. Such complications are treated with antibacterial agents.
What is the purpose of the procedure?
- Diagnosis of infection, tumor or collapsed lung
- Finding the source of bleeding
- Determining the causes of chronic cough, shortness of breath
- Finding blocked airways
- Assessing damage after inhaling toxic or hot gases
- Carrying out a biopsy
Doctors also use bronchoscopy to treat certain conditions, for example by:
- removing fluid, mucus (debridement), or foreign objects in the airways
- widening blocked or narrowed airways
- cancer treatment
- drainage of abscesses
How is the procedure done?
In a flexible endoscope procedure, the doctor sprays a local anesthetic into the nose and throat. The procedure with a rigid bronchoscope is performed under general anesthesia. The endoscopist inserts the bronchoscope through the nose and throat into the bronchi. As the tube enters the lungs, the patient may experience a sensation of pressure or pulling. The doctor may administer oxygen throughout the procedure to make breathing easier. Next, the doctor examines the bronchial tree and performs the necessary manipulations. During a bronchoscopy, your doctor may do an ultrasound to look at the tissue around the bronchi. After examination, the bronchoscope is removed. The procedure usually lasts 20–30 minutes.
Virtual bronchoscopy
Technologies do not stand still, so today, along with the usual form of examination, virtual bronchoscopy can be used. It is a special method of computed tomography of the bronchi.
Thanks to new equipment, doctors do not need to go inside a person to see what is happening. Now a special device together with a program simulates a three-dimensional image on the monitor. Today, this technique helps monitor the development of bronchial cancer. But, taking into account all the advantages, at this stage of technological development, virtual bronchoscopy is inferior to the classical method.
Tavaluk Natalya, medical columnist
12, total, today
( 41 votes, average: 4.80 out of 5)
Blood test for microreaction: what is it, explanation, how to take it
Blood test for thyroid hormones: interpretation and rules for taking it
Related Posts
For what purposes are diagnostics carried out?
Bronchoscopy for pneumonia is a diagnostic study, which is advisable to carry out to determine the disease and its therapy. In most cases, the examination is carried out to accurately determine the presence or absence of a tumor.
When an X-ray reveals negative processes in the lung tissues, and the patient complains of hemoptysis, then these are important indications for bronchoscopy. In addition, such manipulation will help remove foreign bodies. Bronchoscopy and biopsy are two interrelated concepts in cases where it is necessary to determine the nature of the neoplasm. So, bronchoscopy is performed in the following cases:
- thermal injury – assess the degree of damage to the respiratory system;
- cough - find out the reasons contributing to the formation of a chronic symptom;
- hemoptysis - determine the reasons why blood and mucus are released;
- the presence of foreign bodies in the respiratory system;
- detection of agents of respiratory infections;
- taking tissue for examination;
- assessment of developmental stage;
- correction of therapy.
Now it has become clear what bronchoscopy is and what opportunities it opens up. It allows you to learn as much information as possible about the disease, adjust the treatment, or even carry it out.
For medicinal purposes, the study is carried out for:
- removal of a foreign object;
- removal of blood and pus;
- administering medications directly to the site of injury;
- eliminating mild collapse;
- regeneration of tracheal patency.
Today, a procedure such as sanitary bronchoscopy plays a very important role. Its essence is that the bronchi are washed with a certain disinfectant solution. The procedure is actively used for purulent lung diseases.
Bronchoscopy: what is it, types, preparation, technique - MEDSI
Bronchoscopy is an endoscopic method for examining the respiratory tract: larynx, trachea and bronchi in order to identify diseases of the mucous membranes of these organs. The procedure is carried out using a bronchoscope - a flexible or rigid tube with a diameter of 3-6 mm, equipped with a lighting lamp and a photo-video camera.
Modern devices are based on fiber optic technology, which ensures high diagnostic efficiency. The image is displayed on a computer monitor, so it can be enlarged tens of times and the recording can be saved for subsequent dynamic observation.
The optical system of the device allows you to examine the respiratory tract up to the second branch of the bronchi and in 97 percent of cases make an accurate diagnosis. Bronchoscopy is used in the diagnosis of chronic bronchitis, recurrent pneumonia, and lung cancer.
If necessary, tissue samples can be taken for biopsy during bronchoscopy.
The technique of bronchoscopy provides the possibility of using the procedure for medicinal purposes - for:
- removal of foreign bodies from the bronchi;
- cleansing the trachea and bronchi from pus and mucus;
- washing and administration of medicinal solutions (antibiotics, glucocorticoids, mucolytics, nitrofurans);
- expansion of the narrowed lumen of the bronchi;
- removal of small tumors.
To treat respiratory diseases and take material for histological examination, the bronchoscope is equipped with the necessary surgical instruments.
If necessary, two studies are carried out together - bronchoscopy and bronchography.
Bronchography is an x-ray method in which a contrast agent is injected into the airways through a catheter or fiberoptic bronchoscope.
The study allows us to study in detail the structure of the bronchial tree (especially those parts of it that are inaccessible for endoscopic examination) and evaluate its motor function during breathing.
Indications for bronchoscopy
Bronchoscopy is used for diagnostic purposes in the presence of:
- unmotivated painful cough;
- shortness of breath of unknown origin;
- hemoptysis;
- frequent bronchitis and pneumonia;
- suspicion of a foreign body in the bronchi or tumor;
- cystic fibrosis and tuberculosis;
- bleeding from the respiratory tract.
For therapeutic purposes, bronchoscopy is performed in the following cases:
- entry of a foreign body into the trachea or bronchi;
- coma and other states of respiratory failure;
- bleeding - to stop it;
- the presence of viscous sputum, pus or blood;
- a tumor that has blocked one of the bronchi;
- the need to administer antibiotics and other drugs directly into the respiratory tract.
Bronchoscopy for pneumonia can be prescribed for both diagnostic and therapeutic purposes.
How is bronchoscopy performed?
The technique of performing bronchoscopy requires it to be carried out in a hospital setting - in a specially equipped room and in full compliance with the rules of sterility. The procedure involves a pulmonologist (or endoscopist), a physician assistant, and an anesthesiologist.
The patient is pre-prepared for bronchoscopy in order to avoid possible complications (for more information on preparing for the procedure, see the article:
Expert opinion
The bronchoscopy technique allows you to carefully examine the mucous membrane of the respiratory tract and detect signs of various pathologies:
- inflammatory diseases (endobronchitis, pneumonia);
- tuberculosis;
- violation of the tone of the bronchial tree (hypotonic dyskinesia);
- narrowing of the lumen of the bronchi due to inflammatory changes or due to tumor growth;
- cystic fibrosis;
- tumors – benign and malignant;
- bronchial asthma.
The result of bronchoscopy may be the implementation of medical procedures - as a result of diagnosing certain pathologies.
Contraindications for bronchoscopy
Due to the fact that the bronchoscopy technique is a surgical intervention, this procedure has a number of contraindications.
The following are absolute contraindications:
- Allergic reactions to anesthesia;
- Hypertension;
- Recent heart attack or stroke (less than 6 months);
- Chronic pulmonary or heart failure;
- Severe arrhythmia;
- Mental disorders (epilepsy, schizophrenia, etc.);
- Aortic aneurysm;
- Narrowing of the larynx (stenosis).
In some situations, bronchoscopy should be postponed:
- During pregnancy (after the 20th week);
- During menstruation;
- With exacerbation of bronchial asthma;
- When blood sugar increases in patients with diabetes.
The need for bronchoscopy and the possibility of performing it can only be determined by a pulmonologist or therapist.
Advantages of bronchoscopy at MEDSI
- MEDSI clinics are equipped with expert-class equipment for performing bronchoscopy;
- The study is carried out by a team of highly qualified experienced specialists: a pulmonologist, a physician assistant and an anesthesiologist;
- The high accuracy of bronchoscopy makes it possible to diagnose respiratory diseases in 97 percent of cases;
- The procedure is painless, as it is carried out using effective anesthetics, and, if necessary, in a state of medicated sleep;
- The patient's condition during bronchoscopy is under the control of doctors using special equipment for this.
Source: https://medsi.ru/articles/bronkhoskopiya-tekhnika-provedeniya/
What type of anesthesia is used?
The presented diagnostic method for pneumonia is done under anesthesia. Local anesthesia is used when a flexible device is used in the process. When using rigid models, the procedure is performed under general anesthesia.
If bronchoscopy of the lungs is performed under local anesthesia, then a 2–5% lipocaine solution is used. As a result, the patient feels numbness in the palate, the presence of a lump in the throat, difficulty swallowing and slight congestion in the nasal passages. This type of pain relief may cause severe coughing or vomiting. Before inserting the bronchoscope, the doctor treats the mucous membrane of the larynx, ligaments, trachea and bronchi with an anesthetic spray.
When the procedure is performed under general anesthesia, the diagnosis is most likely carried out in young patients and people with an unstable mental state. While under general anesthesia, the patient sleeps and does not feel any painful or unpleasant sensations.
Do you need preparation for the study?
Bronchoscopy is an invasive procedure that requires careful preparation for its implementation (this will help increase the information content of the study and reduce the risk of complications).
First of all, the patient must be carefully examined. The required minimum is:
- general blood analysis;
- blood test for coagulation (coagulogram);
- determination of blood gas composition;
- X-ray of the chest organs.
So, based on the data obtained, the doctor will determine whether there are contraindications to the study and, if there are none, he will tell the patient about how the bronchoscopy will proceed and how the patient should behave during the procedure.
The patient, in turn, is obliged to notify the doctor about his existing chronic diseases of the heart, endocrine and other organs, about his history of allergic reactions (it is very advisable to know what exactly he was allergic to and how it manifested itself), about the medications he is taking permanently (you will probably have to stop taking some of them temporarily).
- It is important to perform the procedure on an empty stomach, so the patient should not eat for at least 8 hours before the bronchoscopy. This will minimize the risk of food getting into the trachea and bronchi.
- On the day of the study you should stop smoking.
- During bronchoscopy, the patient's intestines must be emptied. To achieve this, on the day of the study, in the morning, he will have to do a cleansing enema or use suppositories (suppositories) with a laxative effect.
- To prevent the patient from having to go to the toilet during the diagnostic process, it is necessary to empty the bladder before starting the diagnostic process.
- If the subject shows excessive anxiety, he may be administered. For the same purpose, the doctor can prescribe tranquilizers and sleeping pills the day before - the patient should be calm and well rested during the procedure.
- After bronchoscopy, the patient may experience short-term hemoptysis, so he should have a towel or napkins with him.
Types of bronchoscopy
As noted above, modern bronchoscopes come in rigid and flexible types. Each model has its own advantages and scope of use.
If bronchoscopy of the lungs for pneumonia is performed using a flexible bronchoscope (fiber bronchoscope), then the following advantages can be highlighted:
- penetration into the lower sections of the bronchi, which cannot be examined by rigid equipment;
- less trauma to the bronchi;
- the small diameter of the fiber-optic bronchoscope allows it to be used in pediatrics;
- no general anesthesia required.
This type of diagnosis is used in the following cases:
- examination of the lower parts of the trachea and bronchi;
- assessment of the mucous membrane of the respiratory tract;
- removal of small foreign bodies.
The advantages of a rigid bronchoscope include the following:
- It is widely used for therapeutic activities that cannot be performed using a flexible bronchoscope. It is possible to detect the expansion of the lumen of the bronchi and remove foreign objects obstructing the airways.
- Thanks to a rigid bronchoscope, it is possible to insert a flexible one for the assessment and examination of thin bronchial walls.
- Reduce the consequences and pathological processes identified during diagnosis.
- Resuscitation of patients who have been drowned and... In this case, they remove fluid and mucus from the lungs.
- The manipulation is carried out under general anesthesia, so the person does not feel any unpleasant symptoms. This is very important for a patient who experiences severe anxiety and fear.
Diagnostics using a hard device is used for the following purposes:
- regeneration of the patency of the bronchi and trachea, which arose due to the presence of scars or tumors, installation of a wall to enlarge and reduce the bronchi;
- elimination of scars, neoplasms, clots of viscous sputum;
- detection of lesions of the respiratory system;
- elimination of bleeding;
- removal of foreign bodies;
- bronchial lavage and administration of medicinal solutions.
Indications for bronchoscopy
This diagnostic method is used to clarify the diagnosis in the following clinical situations:
- if the patient has an unmotivated persistent cough;
- if the patient has shortness of breath of unknown etiology (when the most common causes - COPD - are excluded);
- with hemoptysis (blood with sputum);
- if there is a suspicion of the presence of a foreign body in the bronchi;
- if it is suspected in the lumen of the tracheobronchial tree or on, as well as to determine the boundaries of the spread of lung cancer along the bronchi;
- if the fact of a long-term inflammatory process has been established, the nature of which could not be previously clarified;
- in case of recurrent events in the patient’s history (in order to find their cause and eliminate it);
- if dissemination syndrome is detected on a chest x-ray (multiple foci (suspicion of), cavities or cysts in the lungs);
- for the purpose of taking the contents of the bronchi to determine the sensitivity of its microflora to antibiotics;
- when preparing a patient for lung surgery.
Preparatory activities
Before performing bronchoscopy for pneumonia, the following series of recommendations must be followed:
- Perform chest x-ray and electrocardiography. A test for the presence of urea and gases in the plasma is required for preparatory purposes.
- Inform your doctor about illnesses such as heart attack and coronary heart disease. If the patient is taking antidepressants and hormonal medications, then the doctor should also be informed about this.
- The procedure should be carried out on an empty stomach. You can eat your last meal the night before, but no later than 21:00.
- Drinking water before diagnosis is prohibited. Bronchoscopy to determine pneumonia is performed in a specially equipped room and in complete sterility. If this is not observed, then there is a high probability of the body becoming infected. Therefore, before diagnosis, the patient must make sure that all sanitary standards are met in the medical institution.
- The procedure cannot be performed on a patient who is in an excited state. For these purposes, he is given a sedative injection.
- You must take a towel with you to the office, as consequences such as hemoptysis may occur. If you have dentures, piercings, or bite plates, they must be removed.
Bronchoscopy in children
The general algorithm for performing the procedure in a child of any age is the same as in adults. The most common reason for receiving a referral for bronchoscopy in children is the need to remove a foreign body: coins, food particles, toy parts. Of the pathological conditions, such a check of the tracheobronchial tree is required:
- tuberculosis;
- malformations of the bronchopulmonary system;
- lung abscess;
- bronchopulmonary cystic fibrosis (systemic disease of the respiratory system);
- the appearance of tumors in the lungs;
- pulmonary hemorrhage, hemoptysis;
- bronchial asthma
- other diseases of unknown etiology.
Preliminary medical examinations (ECG, blood tests, x-rays) are agreed upon with the doctor, as is the prescription of sedatives. 8 hours before the bronchoscopic examination, the child is stopped feeding, and 4 hours before the child is given fluids. Breastfed infants receive milk for the last time 4 hours before the examination. Features of its implementation:
- Children under 3 years old are given inhalation anesthesia (through a mask), others are often given an intravenous injection.
- The procedure is carried out using a flexible device (fibre-optic bronchoscopy), the diameter of which is less than 3 mm for infants and less than 6 mm for children under 3 years of age. The child is in a horizontal position.
- Due to the high risk of edema and bronchospasm, the doctor should prepare for artificial ventilation.
- After the procedure, the child is prescribed antibiotics.
Article on the topic: How vascular senile dementia manifests itself - the first signs and symptoms of senile dementia that should alert you
Procedure implementation process
How is bronchoscopy done for pneumonia? Before proceeding to the procedure, the patient must enter the office without outer clothing and with an unbuttoned collar. 45 minutes before the start, the person is administered diphenhydramine, seduxen and atropine, and 25 minutes later - a solution of aminophylline. When bronchoscopy is performed under anesthesia, the patient must inhale a salbutamol aerosol to dilate the bronchi. For local anesthesia, nebulizers are used. With their help, the nasopharynx and oropharynx are treated. Such activities can eliminate the gag reflex.
During the diagnosis, the person must lie or sit. A specialist will indicate the correct position. The examination device is inserted through the nose or mouth, and then the doctor examines all areas of interest.
Together with the doctor, there is a nurse in the office who constantly monitors the patient. If there are signs of difficulty breathing due to swelling of the larynx or laryngospasm, bleeding, bronchospasm, you must immediately notify your doctor.
Consuming food and water is allowed only after the gag reflex is restored. As a rule, a few hours are enough. You must first drink water in small sips or suck on pieces of ice.
The nurse should reassure the patient and explain to him that loss or hoarseness of the voice and painful sensations in the nose will soon disappear. When the gag reflex is restored, the person is given emollient solutions for rinsing and tablets to eliminate a sore throat.
Preparation for bronchoscopy and how it is performed
Bronchoscopy is an examination of the mucous organs of the respiratory system (nose, larynx, cleft, trachea, bronchi) using a special endoscope (bronchofiberscope).
Although today it is more correct to say not a fiber-optic bronchoscope, but a video bronchoscope (“fibro” should be replaced with “video”). Bronchoscopy is considered one of the most informative methods for diagnosing tumors of the respiratory tract.
Thanks to it, you can take a tissue sample from a questionable place. This biopsy is performed for cytological and histological analysis.
Is bronchoscopy painful?
The evening before the test, the patient takes a sedative prescribed by the doctor. Immediately before the procedure, the doctor uses a special spray to irrigate the throat, which suppresses the gag reflex.
There are no pain receptors in the bronchial mucosa, so the movement of the bronchoscope does not cause pain in the patient. Doctors suggest breathing frequently and shallowly while advancing the device and remembering that the tube of the device is so thin that it does not interfere with breathing.
During the examination, the bronchoscope tube will move and discomfort may be felt, but even taking a biopsy will not cause pain. At the request of the patient and the doctor's indications, bronchoscopy can be done while sleeping. Typically, medicated sleep is prescribed for children and people with emotional lability.
But in German clinics, bronchoscopy, as a rule, has long been performed under anesthesia. Therefore, the procedure is painless for the patient and well tolerated.
Preparing the patient for bronchoscopy
Preparation of the patient for bronchoscopy is divided into general and immediate.
Algorithm for general preparation of the patient for bronchoscopy.
1. Psychological preparation of the patient for bronchoscopy.
The patient must understand the essence of the upcoming manipulation and give consent to it.
To do this, the doctor talks in an accessible way about the sequence of actions during bronchoscopy, and the patient asks all the questions that concern him, in particular, is it painful to do bronchoscopy, what type of anesthesia will be used, how to properly prepare, how long does bronchoscopy last, what cannot be done after the examination? If a patient suffers from allergies, has concomitant diseases, or takes anticoagulants or insulin, he must tell the doctor about this.
2. It is necessary to undergo some examinations (take an X-ray of the lungs, identify coagulogram indicators, donate blood for tests, ECG)
3. The day before the test, you should not drink alcohol.
4. There is no special diet before bronchoscopy, but the procedure is performed on an empty stomach.
5. The night before, as prescribed by your doctor, you must take sedatives.
6. Clothes during the procedure should be comfortable and loose.
Algorithm for direct preparation of the patient for bronchoscopy.
- You should not smoke before bronchoscopy.
- Premedication with tranquilizers is carried out 1-1.5 hours before the start of bronchoscopy.
- Before the examination, it is necessary to remove piercing jewelry, dentures, orthodontic plates for correcting the bite and for correcting teeth, and contact lenses.
- Immediately before the study, the patient must empty the bladder.
Where is bronchoscopy performed?
Bronchoscopy is performed in an endoscopy room, where all the standards of a sterile operating room are observed. The study can be performed on an outpatient basis.
How is bronchoscopy performed?
- The patient is asked to sit on a chair, place his hands between his legs and tilt his head back slightly.
- Before the examination, use a spray for local anesthesia of the pharynx (if you are not allergic to it); thanks to this anesthesia, the gag reflex is suppressed when passing through a video bronchoscope.
- After pharyngeal irrigation, the patient can be placed horizontally on his back on the endoscopic transforming table. The head should be tilted back slightly. You cannot bend over or make sudden movements. You need to relax and breathe calmly.
- The patient may then be given a short-acting narcotic intravenously, so that during the test he does not feel anything at all, but is awake.
- The doctor inserts the bronchoscope through the lower nasal passage into the nasopharynx and then into the trachea. If the nasal passages are narrowed, swollen, or the patient has frequent nosebleeds, the bronchoscope tube is inserted through the mouth. A rigid bronchoscope is inserted only through the mouth, but rigid bronchoscopes are now used very rarely.
- The doctor examines the mucous membrane of the respiratory tract, which can be imagined as a “bronchial tree” with branches. The endoscopist examines all bronchi as much as possible. The level of examination depends on the thickness of the bronchoscope and the condition of the bronchial tree. Under favorable conditions, the doctor can examine not only the large bronchi, but also their branches. The airways themselves are not sensitive to pain, so the biopsy procedure is painless.
- If bronchial lavage is necessary, the doctor injects approximately 20 to 100 milliliters of sterile fluid into the lower airways and then suctions it out. This way he obtains bacteria and cells from the surface of the respiratory tract for subsequent research in the laboratory. In addition, during bronchoscopy in case of viscous sputum, the bronchi can be washed and medications administered.
What pathologies can be detected?
During diagnosis, it is possible to identify the following pathological conditions regarding the bronchial wall:
- inflammatory process;
- swelling;
- expansion of submucosal lymph nodes and mouths of mucous glands;
- neoplasms;
- the presence of cartilage in the lumen.
Complications of the trachea include detection of stenosis, compression, and disruption of bronchial branching.
If tissues and cells obtained during bronchoscopy were diagnosed, then it is possible to diagnose:
- interstitial form of pneumonia;
- lung cancer of a bronchogenic nature;
When making a final diagnosis, it is necessary to combine all the data obtained from x-rays, bronchoscopy and cytological examination.
Bronchoscopy is an effective method for diagnosing various diseases of the respiratory system. The manipulation itself is not pleasant, but the use of anesthesia allows you to eliminate all painful manifestations during diagnosis. Using bronchoscopy, it is possible not only to assess the condition of the disease, but also to carry out certain therapeutic measures that cannot be carried out in the usual way.
Joseph Addison
With the help of exercise and abstinence, most people can do without medicine.
An important argument when choosing pain relief
serve the technical capabilities of the medical institution. Bronchoscopy under anesthesia requires a team of four people, including a qualified anesthesiologist (it is often more difficult to administer anesthesia during bronchoscopy than during surgery). Bronchoscopy under local anesthesia is performed by a doctor and a bronchology nurse.
For bronchoscopy
under anesthesia in an outpatient setting there are no fundamental contraindications, but appropriate conditions are necessary: a team, equipment, the ability to observe the patient for several hours after the end of bronchoscopy, and, if necessary, to hospitalize.
The bronchoscopy procedure itself
under anesthesia, of course, is more humane, but a painful cough after the patient awakens and muscle pain, which sometimes does not allow the patient to get out of bed, reduce the benefits of general anesthesia.
If using telescopic optics
eliminates the possibility of examining the bronchial tree with both methods of anesthesia, then for performing a biopsy in some cases, for example from the left upper lobe bronchus, anesthesia provides better conditions due to the greater possibility of straightening the angles of the bronchi. Thus, I.A. Stadnitskaya (1966) considers anesthesia especially indicated when examining the bronchi of the left lung.
Spontaneous breathing
allows you to better differentiate the limitation of bronchial mobility.
This argument in favor of local anesthesia can be countered by the possibility of restoring breathing during subanesthesia bronchoscopy. But with therapeutic bronchoscopy, maintaining contact with the patient and the possibility of coughing allows for better removal of the contents of purulent cavities into which the aspirator tip does not penetrate. The listed arguments in favor of both methods of pain relief
do not exhaust all the advantages and disadvantages of local anesthesia and anesthesia.
In general terms, we consider it advisable
be guided by the following principles when choosing anesthesia in bronchological practice: 1. In a modern thoracic surgical department, it is necessary to be fluent in the methods of local anesthesia and anesthesia during bronchoscopy, strictly individually choosing the method of anesthesia for each study; 2. Scientific pulmonology centers should test and improve methods of pain relief during bronchological studies;
3. In medical institutions that do not have anesthesia departments (therapeutic hospitals, anti-tuberculosis dispensaries), as well as in outpatient settings, the method of choice for bronchoscopy should be local anesthesia;
4. If there are indications for bronchoscopy in a surgical department that does not have experience in bronchological work, it is advisable to perform bronchoscopy by an anesthesiologist under anesthesia (intubation experience will help the anesthesiologist to insert a bronchoscope);
5. Bronchoscopy under anesthesia should be performed only with a special respiratory bronchoscope, since when using conventional bronchoscope models, examination under anesthesia loses all its advantages and becomes unsafe;
6. Pulmonary specialization and training of bronchologists create optimal conditions for ensuring the effectiveness and safety of diagnostic studies.
ATTENTION!
GASTROCENTER (CLINIC OF PROFESSIONAL ENDOSCOPY AND CLINICAL GASTROENTROLOGY) HAS ONE ADDRESS: MOSCOW, BERZARINA STREET, 12 AND ONE WEBSITE ADDRESS WWW.site. NO BRANCHES!
THE STUDIES ARE CARRIED OUT USING A HIGH-RESOLUTION ENDOSCOPIC DIGITAL VIDEO SYSTEM OLYMPUS EVIS EZERA, NBI SYSTEM, Japan
MOLAKA EKATERINA YURIEVNA endoscopist, gastroenterologist-hepatologist, candidate of medical sciences, head. Department of Endoscopy and Gastroenterology (work experience since 1994),
KUZNETSOV KONSTANTIN VALERIEVICH Endoscopist-surgeon, gastroenterologist, head. Department of Endosurgery, member of the European Association of Gastrointestinal Endoscopy (work experience since 1995),
KHARNAS SERGEY SAULOVICH Laparoscopic surgeon, professor, doctor of medical sciences, head of the advisory department of surgery and oncology,
We examine and treat patients with:
- diseases of the tracheobronchial tree, larynx, hypopharynx
- diseases of the esophagus
GERD, reflux disease, esophagitis, Barrett's esophagus, diaphragmatic hernia, achalasia cardia and cardiospasm, etc... - diseases of the stomach and duodenum:
peptic ulcer, erosive lesions of the stomach and duodenum, all types of gastritis, etc. - intestinal diseases:
IBS - irritable bowel syndrome, intestinal polyps, diarrhea and constipation, ulcerative colitis and Crohn's disease, celiac disease, SIBO - bacterial overgrowth syndrome in the colon, dysbiosis, etc. - liver diseases,
fatty liver disease (steatosis, fatty hepatosis), we verify hepatitis of viral, toxic and autoimmune origin - diseases of the pancreas -
pancreatitis, - benign and malignant tumors
- diseases of the gallbladder -
biliary dyskinesia, polyposis of the gallbladder, cholelithiasis (GSD)
We conduct full CHEK UP screening examinations to identify early tumors of the larynx and tracheobronchial tree, gastrointestinal tract and other localizations (in our center in one day you can laryngoscopy, bronchoscopy, gastroscopy and colonoscopy were performed in one dream by expert doctors with European practice, followed by consultation with a gastroenterologist, PhD)
Advantages of GASTROCENTER
(specialized center for professional endoscopy)
o :
At the GASTROCENTER you can undergo a complete examination (Chek-up) of the bronchial tree, larynx and gastrointestinal tract in one day, painlessly and inexpensively, to exclude the development of tumors, which rank first in prevalence in the world and in Russia.
o
: do an examination - gastroscopy, colonoscopy, bronchoscopy - in your sleep, which improves the quality of the examination and makes it comfortable and safe.
o ALL TESTS AT ONCE
: during the study we perform all tests - Helicobacter Pylori (ready in 3 minutes), histology, etc.
o do a study on EVIS EXERA II (Japan) - ultra-precise modern equipment: with the possibility of optical and electronic zoom., NBI, HDTV. o :
, Ph.D., have 20 years of experience in the largest Russian medical institutions, experience in Europe and training in Japan to identify and remove through a flexible endoscope the smallest tumors invisible in a conventional endoscope.
In addition, our specialists treat patients, being at the same time gastroenterologists, hepatologists and nutritionists (European standard of gastroenterologist). o IN THE GASTROCENTER you will be advised immediately after the examination by a doctor, candidate of medical sciences. o DO A GASTROSCOPY, COLONOSCOPY, VIDEO CAPSULE ENDOSCOPY, BRONCHOSCOPY IN YOUR SLEEP IMMEDIATELY IN ONE DAY
: AT THE GASTROCENTER you can do all types of endoscopic examinations and/or several in one day research immediately: and immediately get advice from the same specialist on drug treatment and the necessary additional examination of your diseases.
o simultaneously during gastroscopy or colonoscopy, bronchoscopy: in the Gastrocenter all types (see price list, list of operations) of endoscopic operations are performed through a flexible endoscope (“surgery without an incision”) by expert class specialists. o TAKE ALL TESTS IMMEDIATELY:
All types of laboratory tests and ultrasound are performed at the GASTROCENTER. You can undergo a complete examination of the gastrointestinal tract in one day, and for smokers, check the condition of the tracheobronchial tree and lungs.
- The GASTROCENTER
cooperates with major medical institutions in Russia in the field of studying Helicobacter pylori; the GASTROCENTER widely practices programs
.
MORE ABOUT BRONCHOSCOPY
- What is bronchoscopy and in what case is it the most accurate?
- Is the patient experiencing pain?
- Indications for bronchoscopy. When should bronchoscopy be performed?
What is bronchoscopy and when is it most accurate?
Bronchoscopy (tracheobronchoscopy,
laryngotracheobronchoscopy, fibrobronchoscopy (FBS)
is the most accurate method of examining the tracheobronchial tree, i.e. examination from the inside of the trachea, larynx, large and small bronchi using a flexible device (fiber bronchoscope). To assess the condition of the lung tissue (not the bronchi) use radiological methods (CT-computed tomography, radiography).Bronchoscopy and computed tomography are two methods that are mandatory and complement each other for an accurate diagnosis of the condition of the chest organs.
How is bronchoscopy performed?
In the endoscopic department of the GASTROCENTER, brochoscopy is performed by expert level specialists with twenty years of experience ( see SPECIALISTS)
,
using digital endoscopic equipment from OLYMPUS with the possibility of digital photography. Before starting the procedure, the patient consults with specialists, the endoscopist and anesthesiologist study the CT (computed tomography of the chest) findings and other medical data that the patient has. For elderly patients and patients with concomitant diseases, it is better to take with them the medical documents that are available (extracts, ECG, tests, etc., the anesthesiologist will definitely read them), the patient is explained what additional manipulations may be performed during bronchoscopy.
The examination is carried out with anesthesia
and in a state of superficial short-term sleep (sedation, not related to anesthesia), which lasts no more than 15 minutes, the patient immediately wakes up after the end of the procedure, awakening and sleep itself are tolerated very comfortably.
During the examination, the doctor-endoscopist examines the laryngopharynx, trachea, bronchi using an endoscope, and, if necessary, performs additional important diagnostic procedures (bronchial lavage for microbiological culture for sensitivity to antibiotic drugs and phages, biopsy, sanitation of the tracheobronchial tree with antibacterial drugs, instillation of drugs and others). Also, under sedation, operative bronchoscopy is performed - removal of benign tumors (neoplasms) of the larynx and tracheobronchial tree, for example, polyps, papillomas of the tracheobronchial tree, singer's nodules, foci of hyperplastic laryngitis, electrocoagulation and electrocautery and other operations. Neither before the start of the procedure, nor during, nor after it, the patient does not experience any discomfort. The patient's condition during sedation is monitored by an anesthesiologist (see SPECIALISTS).
After the examination is completed, the patient is given a study protocol with photographs, specialists advise the patient on the results of the study, and within 30 minutes the patient can leave the clinic; patient accompaniment is not required (optional, optional).
What are the contraindications for bronchoscopy?
An immediate contraindication is intolerance to the drug LIDOCAINE, which is detected earlier most often during local anesthesia at the dentist. Why is lidocaine needed if the patient is sleeping anyway? The fact is that this drug is used separately for local anesthesia of the larynx and other important areas of the tracheobronchial tree, so that the examination is quick and comfortable. There are no other absolute contraindications; elderly patients and patients with severe concomitant diseases are consulted in detail by an anesthesiologist before the procedure to determine contraindications.
When should bronchoscopy be performed?
Indications for bronchoscopy
, main symptoms: 1. Cough, long-lasting 2. Smoking experience for more than 5 years, screening - preventive diagnostic bronchoscopy 3. Diagnosis of neoplasms (tumors) of the lungs. Prevention of lung cancer. Bronchoscopy is the most important, basic examination in the diagnosis of lung cancer; it allows us to identify tumors of very small diameter and thus prevent their development. Modern digital fiberoptic bronchoscopes allow you to examine large and small bronchi up to their second-order branches - subsegmental bronchi, and take a piece of the mucous membrane (biopsy) for subsequent morphohistological examination. 4. Lung tumors in first-level relatives, preventive examination 5. Chronic bronchitis: a pulmonologist may prescribe bronchoscopy to assess the condition of the mucous membrane of the tracheobronchial tree and to perform bronchial washout (lavage) followed by microbiological culture, when it is necessary to accurately identify the spectrum of microorganisms for prescribing antibiotics. Patients with chronic bronchitis and bronchiectasis often need sanitation bronchoscopy, during which the tracheobronchial tree is washed from pathological secretions, sanitation using medicinal and antiseptic solutions.. 5. Release of blood when coughing (Hemoptysis). The release of streaks of blood when coughing is an alarming symptom, observed with lung tumors, most often with lung cancer, with some forms of tuberculosis and lung abscesses, often accompanies COPD, bronchiectasis, echinococcosis, pulmonary tissue infarctions, pneumonia, etc., as well as congestion blood in lung tissue in cardiac patients. When hemoptysis with cough, either sputum streaked with blood, or rusty-colored sputum, or pure scarlet blood is released. 6. Chronic obstructive pulmonary diseases (COPD) - the entire spectrum of long-term recurrent chronic obstructive pulmonary diseases, which are accompanied by frequent episodes of infection of the secretion of the bronchial tree (sputum). Here, too, bronchoscopy can help in assessing the condition of the bronchial mucosa, identifying the pathogen (microorganisms) in the infectious nature of bronchitis (bronchial lavage - BAL with culture for sensitivity to antibiotics).
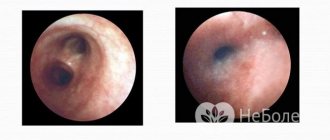
Bronchoscopic picture
Normally, the mucous membrane of the trachea and bronchi is pink, shiny, contains a small amount of transparent secretion on the surface, the carina and spurs of the bronchi are narrow, easily displaced during instrumental palpation. The bronchoscopic picture consists of an assessment and description of seven main bronchoscopic signs: 1) the type of mucous membrane of the trachea and bronchi, 2) the type and quality of secretion in the lumens of the trachea and bronchi, 3) the elasticity (compliance) of the walls of the trachea and bronchi, 4) bleeding of the mucous membrane of the trachea and bronchi, 5) the type and mobility of the spurs and the mouths of the segmental and subsegmental bronchi. 6) the type of vascular pattern of the mucous membrane, 7) the type and nature of folding of the mucous membrane. The tone of the bronchi, the nature and degree of infiltration of its wall are also taken into account. In diseases of inflammatory origin, one or another degree of endo-bronchitis is always detected. Detailed endoscopic characterization of the prevalence and severity of inflammatory changes in the bronchi is of great importance in assessing the extent of the lesion, treatment results and preoperative preparation. According to the bronchoscopic picture, the following types of bronchitis are distinguished: diffuse, diffuse partial and limited.
Diffuse bronchitis - widespread to all bronchi visible during B. The distal border of inflammation is not visible; it seems to be lost in the divisions of small bronchi. Diffuse partial bronchitis differs from the previous one in the intactness of the upper lobe bronchi and their divisions. Limited (local) bronchitis of large bronchi is characterized by clearly defined boundaries of inflammation. Each of these forms of bronchitis can be unilateral or bilateral, combined with varying degrees of inflammation. 1st degree - swelling of the mucous membrane almost erases the normal relief of cartilage, spurs and mouths of the lobar bronchi. The folding is preserved, the vascular pattern is smoothed out, but is distinguishable in typical places. Secretion is moderate. 2nd degree - the mucous membrane and spurs of the bronchi are swollen and somewhat thickened, the relief of the cartilage is erased, the lobar and segmental orifices are narrowed, but distal examination is possible. The folding is smoothed out, the vascular pattern is indistinguishable. 3rd degree - hypersecretion is so abundant that it often interferes with research; the lumen of large bronchi is narrowed so much that the bronchoscope tube is retained in the right intermediate or left lower lobe bronchi. It is almost impossible to examine the segmental bronchi.
In the diagnosis of lung tumors, B. has two goals: visual diagnosis and biopsy. In practice, both studies are inseparable, because a presumptive diagnosis must always be confirmed histo- or cytologically. Equally important is identifying the extent of the tumor along the length of the bronchial tube. Based on these signs, bronchoscopic diagnosis of operability is based and the extent of surgical intervention is planned. Examination and biopsy are a single time-consuming action that forms the essence of bronchological treatment for suspected lung cancer. Numerous bronchoscopic symptoms and syndromes of lung cancer can be combined into thirteen characteristic signs: 1 - combination of an obligatory symptom - thickening of the bronchial wall, detected by instrumental palpation, with one or more of the following symptoms: the presence of bronchial secretions of normal quantity and quality, atrophic mucous membrane, normal mucous membrane, stationary wall of the trachea or bronchus, absence of respiratory movements of the carina or transmitting pulsation of the heart and large vessels; 2—a combination of two mandatory symptoms; local hyperemia of the mucous membrane in a limited area with a normal amount of unchanged bronchial secretion; 3 — “dead mouth” syndrome (lack of respiratory mobility and movement of secretion droplets); 4 — absence of passive replacement of the bronchial tube; 5 - combination of abrasion of the pattern of cartilaginous rings with bronchial secretion that is normal in quality and quantity, or with a normal mucous membrane, or with the absence of transmission pulsation, or with local hyperemia of the mucous membrane: 6 - increased bleeding of the mucous membrane in the presence of bronchial secretion that is normal in quality and quantity , with atrophic mucous membrane, normal (circumferentially) mucous membrane of the bronchi, absence of transmission pulsation; 7 - combination of local hyperemia of the mucous membrane with the absence of transmission pulsation of large vessels of the heart: 8 - infiltration of the wall of the bronchus or trachea; 9 - a combination of loose mucous membrane with one of the following symptoms: bronchial secretion of normal quantity and quality, normal mucous membrane in circumference, atrophic mucous membrane, age over 40 years, absence of transmission pulsation, worn out pattern of cartilaginous rings; 10 - immobility of the walls of the bronchi in combination with one of the symptoms of sign 9, except age; 11 - combination of concentric narrowing of the bronchial lumen with one of the symptoms of sign 9, except age; 12 - a combination of the absence of respiratory movements of carina with one of the symptoms of sign 9, except for age; 13 - tumor or shapeless growths in the lumen of the bronchus.
Rice. 3. Biopsy by biting the tumor of the segmental bronchus through a bronchoscope.
Endobronchial biopsy through a bronchoscope is performed following the initial examination. Biting biopsy (Fig. 3) is the simplest. It is performed under visual control from exophytic tumors located in the trachea, main, intermediate, middle and lower lobe bronchi. Curettage biopsy, often “blind”, is most effective for creeping infiltrates and retrostenotic formations. Aspiration biopsy is performed after catheterization through a bronchoscope of segmental or subsegmental bronchi with radiopaque catheters using optical telescopes and X-ray television control.
Bronchial catheterization can be used to debride lung abscesses or cavities by targeted rinsing with antiseptics and aspiration. A similar method is used as a bronchological aid at the time of status asthmaticus; in this case, endobronchial lavage is combined with bronchoscopic aspiration. The latter serves as the basis for the treatment of postoperative atelectasis, and in combination with the instillation of medicinal substances - the basis for bronchoscopic therapy.