Mastoiditis, what is it? Symptoms and treatment
Mastoiditis is an infectious inflammation of the mastoid process located on the temporal bone. Most often, this disease is complicated by the acute form of otitis media. As it develops, the temperature rises, intoxication of the body occurs, throbbing pain and swelling in the area of the mastoid process appear, the ear hurts, and hearing deteriorates.
The causative agents of the disease are usually: staphylococci; pneumococci; influenza stick; streptococci. Sometimes mastoiditis occurs, which develops due to infection due to tuberculosis, secondary syphilis, and sepsis.
What it is?
Mastoiditis is an inflammation of the mucous lining of the cave (antrum) and the cellular structures of the mastoid process of the temporal bone, located behind the ear and containing air-filled bone cavities. Mastoiditis develops due to the spread of infection to the cells of the mastoid process.
Most often, secondary mastoiditis develops, which occurs as a complication of untreated acute or chronic otitis media caused by an infection of the middle ear. Occasionally, primary mastoiditis is observed, when the pathological process initially develops in the structures of the mastoid process (for example, due to injury).
Diagnosis of the disease Mastoiditis
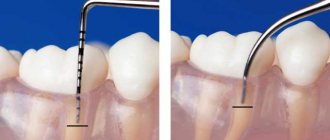
Diagnosis of mastoiditis in typical cases is not difficult, but with an atypical course of the disease the diagnosis becomes more complicated. The totality of objective signs of mastoiditis should be taken into account. Radiography is important; if necessary, CT or MRI of the temporal bones is performed, which are the most informative diagnostic method, and a decrease in pneumatization and veiling of the mastoid cells are determined at various intensities. Differential diagnosis of mastoiditis is carried out with a boil of the external auditory canal when it is localized in the posterior wall. In this case, as with mastoiditis, swelling occurs behind the auricle. Pressure on the planum mastoideum and the tip of the mastoid process is painful with mastoiditis, and with a boil, pressing on the tragus, chewing, and pulling on the auricle causes pain. With mastoiditis, these symptoms are absent, but there is a pronounced decrease in hearing, which is not typical for a boil. In addition, with a boil, a narrowing is observed in the membranous-cartilaginous section, and with mastoiditis - in the bone section.
Classification
The occurrence of infection varies:
- primary mastoiditis, with initial entry of the inflammatory agent into the mastoid cavity,
- secondary mastoiditis, which occurs as a complication of inflammatory processes in the body.
Secondary mastoiditis can occur:
- as a result of otitis media, it is called otogenic,
- as a result of head injuries,
- as a focus during sepsis (septicopyemic focus).
Along the way, mastoiditis can be:
- typical, with all the classic symptoms present,
- atypical or latent, sluggish inflammatory process without pronounced symptoms.
Treatment
Treatment should begin immediately after diagnosis. For this purpose, drugs from the following pharmaceutical groups are selected:
- Broad-spectrum antibiotics, including cephalosporins and macrolides. If the infection is caused by a specific flora (Koch bacillus, spirochete pallidum), drugs are used to treat primary infections;
- Anti-inflammatory drugs based on steroid hormones;
- Immunomodulatory drugs. Since steroidal anti-inflammatory drugs significantly reduce immune function, it is necessary to use drugs to increase immune activity;
- Antihistamines to eliminate local swelling;
- Detoxification drugs to eliminate symptoms.
Surgical interventions may also include:
- Paracentesis (puncture);
- Mastoidotomy (opening of the appendix);
- Mastoidectomy (removal of the mastoid process).
Only a doctor should choose the treatment for such a serious disease!
Causes
In the vast majority of cases, mastoiditis is a complication of acute otitis media - inflammation of the middle ear. In this case, the infection spreads from the tympanic cavity to the mastoid area. Consequently, the same bacteria that cause otitis media cause mestoiditis, namely:
- Streptococcus pneumoniae,
- Haemophilus influenzae,
- Moraxella catarrhalis.
The spread of infection from the middle ear area is facilitated by:
- reduced immune status of the body;
- lack of adequate treatment of otitis (untimely drainage of the tympanic cavity, late paracentesis, a small-diameter hole in the eardrum or its early closure, preventing the outflow of purulent masses).
Infection can enter the mastoid process hematogenously (through the bloodstream) in tuberculosis, secondary syphilis, and sepsis.
All cases of mastoiditis described above are secondary (i.e., arising against the background of another disease). Primary mastoiditis is also possible. It appears when the cells of the mastoid process are damaged due to:
- blow;
- gunshot wound;
- traumatic brain injury.
In these cases, blood enters the mastoid cavity, which is an excellent breeding ground for many types of bacteria.
Against the background of chronic somatic diseases (tuberculosis, diabetes mellitus, rheumatic diseases, hepatitis, etc.) and pathological processes in the nasopharynx (chronic rhinitis, sinusitis, pharyngitis, laryngitis, tracheitis), as well as with existing changes in the structure of the ear (due to injury , previous otitis), acute mastoiditis occurs more often and is more severe.
Course of the disease Mastoiditis
This is the most common complication of acute otitis media. Changes in the mastoid process with mastoiditis vary depending on the stage of the disease. At the 1st exudative stage, the mucous membrane and periosteum of the mastoid cells are involved in the process, the cells are filled with exudate, the mucous membrane is inflamed and sharply thickened. Stage 2 is characterized by a predominance of proliferative-alterative changes, extending to the bone structures of the mastoid process - this is the alterative, or destructive, stage. In this case, bone is destroyed by osteoclasts and granulations form. The bone bridges between the cells become necrotic. The cells merge, forming one common cavity filled with pus - an empyema of the mastoid process is formed. The process of bone destruction can reach the dura mater of the middle or posterior cranial fossa and cause various intracranial complications. When one of the walls of the mastoid process is destroyed, pus can break through to its surface with the formation of a subperiosteal abscess, into the zygomatic process or into the scales of the temporal bone, into the petrous part of the pyramid of the temporal bone, through the apex of the process into the interfascial spaces of the neck. Sometimes several paths for the outflow of pus are formed at once.
Mastoiditis is more often observed in patients with a pneumatic type of mastoid structure; its development is facilitated by a number of factors: high virulence of the infectious agent, decreased body resistance (in particular, in diabetes, nephritis, and other chronic diseases), difficulty in outflow from the antrum and tympanic cavity. One of the reasons for the development of mastoiditis is irrational treatment of acute otitis media.
Symptoms of mastoiditis
The symptoms of mastoiditis vary, and it usually appears together with purulent otitis media (at 2 or 3 weeks). Mastoiditis in children can develop even in the absence of a formed bone process (up to 3 years the process does not yet have time to form).
The usual symptoms of the disease are:
- decreased perception of sounds;
- increased body temperature;
- headache;
- sharp pain behind the ear;
- suppuration that is observed from the external ear canal.
If the volume of suppuration significantly exceeds the size of the eardrum or it is damaged, then this indicates the spread of the disease beyond the middle ear. If the amount of pus is insignificant, the infection does not spread further and the integrity of the eardrum is preserved.
The patient can observe a protruding ear, the formation of smoothness behind the ear instead of the skin fold usually located there. Pus can spread to all parts of the skull, causing blood clots, necrosis of the periosteum and the formation of an external fistula.
Features of the disease in children
Since the mastoid process is underdeveloped in infants, pus in otitis media penetrates only into the cave of the temporal bone - the antrum and leads to the development of purulent anthritis. Otitis and anthritis are diagnosed in children with reduced body resistance, premature and rickety children.
A distinctive feature of the pathology in children is the rapid development of a subperiosteal abscess, often without bone destruction.
Clinical symptoms of mastoiditis in children:
- Fever,
- Cry,
- Moodiness,
- Restless sleep
- Poor appetite
- Symptoms of meningism,
- Copious purulent discharge.
Otoscopic manifestations: bulging of the eardrum, change in its color, swelling, the appearance of a pulsating reflex at the site of perforation.
How are cholesteatoma and mastoiditis related?
Cholesteatoma is a formation that consists of dead skin cells that accumulate in the middle ear chamber or mastoid process. The accumulation and expansion of cholesteatoma occurs due to the bone tissue into which it penetrates. At the same time, it creates pressure that changes the structure of the bone. Bone erosion is accelerated by the presence of enzymes that stimulate the activity of osteoclasts, which remove old bone tissue. In this case, the growth of cholesteatoma leads to brain dysfunction.
The location of congenital cholesteatoma is the anterior mesotympanic region or the perieustachian region of the middle ear cavity. As congenital cholesteatoma grows, it blocks the eustachian tubes and allows fluid to form in the ear chamber, leading to conductive hearing loss. Cholesteatoma can also block the auditory ossicles, leading to hearing loss.
Primary acquired cholesteatoma is a consequence of serous chronic otitis, in which negative pressure is created in the middle ear chamber, and the membrane ruptures and is pulled inward. This causes erosion of the walls of the epitympanic recess of the temporal bone.
Retraction of the eardrum can cause destruction of the auditory ossicles. It is also possible to destroy mastoid cavities or structures of the inner ear, depending on the direction of expansion of the cholesteatoma. Another complication is pressure and dysfunction of the facial nerve, which results in paralysis of the facial muscles.
Thus, you need to know that any rupture of the eardrum can lead to the formation of cholesteatoma if the process of accumulation of squamous epithelium occurs. This also applies to surgery to insert a drainage tube into the eardrum. The appearance of cholesteatoma is possible if squamous epithelium enters the middle ear chamber.
Diagnostics
Diagnosing overt mastoiditis is not difficult. Diagnosis of an atypical type of disease is considered more severe, when obvious symptoms (swelling, suppuration, pain) are not observed.
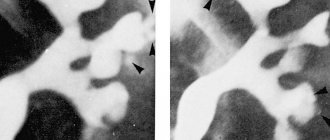
An important method for studying the disease is radiography. But CT and MRI of bone tissue in the temporal region are considered the most effective.
The doctor examines the eardrum and the area behind the ear. Blood tests may also be ordered. In this case, the parameter of interest to the doctor is ESR. This characteristic may indicate the inflammatory process in the body and its intensity.
Consequences
The most serious complications of mastoiditis are lesions of the facial nerve:
- facial asymmetry occurs
- the corner of the mouth or eye moves downwards,
- the face becomes like a mask,
- the eyelid does not close well.
The second dangerous complication of mastoiditis is the breakthrough of pus into the cranial cavity with the formation of inflammation of the meninges or brain matter. This causes general symptoms of infection:
- fever with inflammatory changes in the blood,
- sleep and appetite disturbances,
- nausea and even vomiting,
- refusal to eat due to ear pain.
How to treat mastoiditis?
Treatment of symptoms of mastoiditis is prescribed only after a complete examination of the patient. It can be conservative or surgical, which is carried out in a hospital setting (in the ENT department).
Conservative treatment of mastoiditis can be successful only at the exudative stage of the disease, until bone destruction develops and the outflow of exudate is not impaired. In this case, antibiotics for mastoiditis are mandatory, most often intravenously. You should also ensure free outflow of pus from the middle ear cavity and be sure to use local antibacterial drugs. The selection of these drugs is carried out taking into account the sensitivity of the ear flora. The prognosis for mastoiditis of this form is positive only if therapy is started in a timely manner and all doctor’s prescriptions are followed.
Partial but clear improvement in the patient’s condition is a good sign and allows for prolongation and optimization of conservative treatment. If, within 24 hours after the start of treatment, the main symptoms of the disease, such as fever, pain in the area behind the ear during palpation and reactive phenomena in the ear area, do not decrease, the patient is referred for surgical treatment.
Symptoms of the disease
Symptoms of mastoiditis depend on the form of the disease and its severity. Very often, at an early stage, the clinical picture of inflammation is blurred, masquerading as otitis media . Both inflammations occur simultaneously, so even a qualified specialist is not always able to detect infection of the mastoid process at an early stage. As mastoiditis progresses, it manifests itself in adults with the following symptoms:
- hyperthermia (increased temperature);
- ear pain, the appearance of extraneous noise;
- swelling of the tissues behind the ear, their redness;
- the skin fold behind the ear is smoothed out, the skin in this area is stretched;
- the ear on the side of the mastoid process protrudes;
- headaches radiating to the temple and upper jaw;
- purulent discharge from the auricle with a strong unpleasant odor;
- decreased hearing acuity;
- poor appetite and, as a result, weight loss.
When purulent contents penetrate the subcutaneous tissue, a subperiosteal abscess is formed with severe pain in the area behind the auricle. Further melting of the soft tissues of the head leads to the breakthrough of pus and the formation of an external fistula opening.
Prescribing treatment at the initial stage of the disease allows you to quickly relieve its symptoms . In this case, the patient’s general condition can completely normalize within the first two to three days after starting to take the medications.
If the doctor's recommendations are not followed, there are errors in the drug dosage regimen, deviations from the prescribed dosages, or premature cessation of treatment, the symptoms of mastoiditis may intensify. In this case, pain in the area behind the ear will be constantly present, sharply intensifying when pressure is applied to the affected area.
Forecast
Cure of mastoiditis is possible with immediate medical intervention. Therefore, early seeking of medical help is important. But since antibiotics have difficulty penetrating the mastoid structures, the infection is difficult to cure; Relapses cannot be ruled out. Various complications associated with the spread of infection to adjacent anatomical structures are possible. It is possible to develop hearing impairment, inflammation of the labyrinth of the inner ear (labyrinthitis), causing dizziness; Tinnitus can progress along with hearing loss, making communication difficult.
The infection can affect the facial nerve (cranial nerve VII), resulting in weakness or paralysis of the facial muscles on the affected side. Other complications include Bezold's abscess (an accumulation of pus under the sternocleidomastoid muscle of the neck), Citelli's abscess, subperiosteal (subperiosteal) abscess of the mastoid process of the temporal bone, which typically leads to displacement and protrusion of the auricle.
Severe complications occur when the infection spreads to brain tissue. Such complications include meningitis (inflammation of the meninges), epidural abscess (between the bones of the skull and the dura mater), thrombosis of the dura mater sinuses, and brain abscess.
What is otitis media
With a cold, flu, or other diseases of the upper respiratory tract, the patient's nasopharyngeal mucosa first swells. If the disease is delayed, inflammatory processes spread to the Eustachian tubes. They become swollen, which blocks the normal flow of air into the ear chamber.
Long-term dysfunction of the Eustachian tube leads to exudative otitis media. If the Eustachian tube cannot equalize the pressure in the ear cavity due to blockage, inflammation or malformation, negative pressure develops in the ear chamber. This leads to the fact that the eardrum bends inward, and fluid is visible behind it, which normally should not be there.
Fluid appears due to negative pressure, under the influence of which transudate is pumped from the mucous membrane of the middle ear into the ear chamber, creating conditions for the proliferation of microorganisms. It is worth noting that transudate and exudate are different concepts. Exudate is rich in proteins and nutrients, while transudate is poor in these substances. In this case, exudate is a consequence of inflammatory processes, while transudate appears without them.
Otitis media, due to the anatomical structure of the ear chamber, can spread to the mastoid protrusion. Due to their porous structure, the cavities of mastoid cells provide an excellent environment for the development and reproduction of pathogenic microorganisms. In this case, the infection affects the entire mastoid growth. If not treated in time, infection from this part of the temporal bone can spread to the membranes of the brain and cause meningitis.
Prevention
Preventive measures for mastoiditis include:
- Moderate physical activity
- Elimination of foci of chronic infection in the body,
- Immune stimulation,
- Proper, healthy eating,
- Full sleep
- Maintaining a healthy lifestyle,
- Prevention of diseases complicated by mastoiditis - otitis media, tuberculosis, diabetes mellitus, rhinitis, sinusitis.
- Timely diagnosis and treatment of inflammatory diseases of the middle ear.