Inflammatory processes that appear in the organs of the digestive tract bring many difficulties to the patient. They manifest themselves in a change in regimen and the appearance of a diet menu that includes healthy foods. If the first symptoms of the disease appear, a person should contact a specialist who will provide medical assistance. Self-medication is inappropriate, because a person can further harm the body by choosing the wrong medications.
One of the dangerous diseases is acute cholecystitis, which is often diagnosed in patients. The disease affects the walls of the gallbladder due to improper movement of bile. If the patient comes in at an advanced stage, the disease becomes chronic, which is not so easy to cure.
Description
Symptoms of acute cholecystitis are similar to pancreatitis, appendicitis or cystitis. The disease is more common in women aged 30-50 years, rarely manifests itself in men and in childhood.
If treatment of the disease began on time, then the acute stage gradually subsides, and the symptom no longer appears. But when symptoms appear again and again, the patient may develop a chronic type. In any case, acute cholecystitis appears due to the spread of infection, which appears when the outflow of bile is impaired or the organ is damaged.
This disease attracts the attention of many researchers because more and more patients are becoming ill, and there are no clear opinions about the causes and treatment. Much controversy arises about when a patient should undergo surgery: immediately when the acute phase appears, or after it subsides? But medicine is developing, and a great achievement is the reduction in deaths.
Diagnosis of cholecystitis.
After listening to the patient’s complaints described above, any doctor must examine him, paying attention to the color of the skin, sclera, and frenulum of the tongue (they may be jaundiced).
On palpation of the abdomen, possible cholecystitis is indicated by pain detected in the right hypochondrium and at special gall bladder points and local muscle tension over this area. Such patients often experience pain when gently tapping the right costal arch and the area of the right hypochondrium. To accurately determine the diagnosis, the patient is usually sent for examination.
The following diagnostic methods help to identify cholecystitis:
- hemogram (with disease activity, signs of inflammation are revealed: leukocytosis, thrombocytosis, accelerated ESR);
- biochemical blood tests (during an exacerbation, markers of cholestasis can be detected - an increase in alkaline phosphatase, bilirubin, gamma-glutamyl transpeptidase, an increase in acute-phase inflammatory proteins - CRP, haptoglobin, etc.);
- urine analysis (after an attack, bile pigments may be present in it);
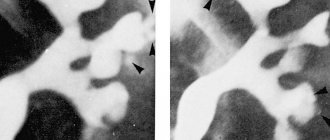
- ultrasonography (the study evaluates the size of the gallbladder, the presence of deformations, stones, tumors in it, the homogeneity of bile, the condition of its walls and tissues around it; in acute cholecystitis, the walls are stratified, their “double contour” appears, and in chronic cholecystitis they thicken, sometimes to clarify the functional disorders, this study is complemented by a test with a choleretic breakfast);
- MRI/CT (the diagnostic capabilities of non-contrast survey studies are similar to ultrasonography; MRI cholangiography, which analyzes the condition and patency of the ducts, excluding some complications of cholecystitis, is more informative);
- endoscopic ultrasonography (the method combines fibrogastroduodenoscopy and ultrasonography, since the diagnostic sensor is placed on the endoscope, it better visualizes the condition of the bile ducts);
- duodenal intubation (the results of the method indirectly indicate cholecystitis, if the collected bile in the cystic portion is cloudy with flakes, parasites are present);
- bile culture (detects pathogens, clarifies their type and sensitivity to various antibacterial drugs);
- plain radiography of the abdomen (a simple study can confirm perforation of the inflamed gallbladder, its calcification, and detect some stones);
- cholecystography is an X-ray contrast method, during which contrast is injected directly into a vein or through the mouth (it detects stones, a “disabled” bladder, functional disorders, but after the widespread introduction of ultrasonography into routine practice, it is used extremely rarely);
- retrograde cholangiopancreatography (allows you to identify a complication - blockage of the ductal system and even remove some stones);
- cholescintigraphy with technetium (radioisotope technique is indicated for verification of acute cholecystitis and exclusion of a “disabled” bladder);
- hepatocholecystography (radioisotope diagnostic procedure to clarify the type of functional disorders);
- stool microscopy to detect eggs or fragments of worms, Giardia cysts;
- immunological (ELISA) and molecular genetic tests (PCR) to detect parasites.
Classification
The disease is more common in women aged 30-50 years.
The classification of acute cholecystitis plays an important role in the study of the disease, because it helps doctors make the correct diagnosis of the patient and select the appropriate treatment complex. Depending on the manifestations of inflammation according to the ICD, the following are distinguished:
- calculous form, which is characterized by the appearance of stones in the gall bladder;
- stoneless, in which there are no stones.
The stoneless form is divided into several subspecies:
- Acute catarrhal form, which is the mildest. This type is characterized by enlargement of the gallbladder, swelling of its walls, and the presence of serous impurities in the bile.
- Also, according to the ICD, a destructive form is distinguished, which, in turn, is divided into several types: purulent, gangrenous and fibrinous. The purulent type is characterized by erosions and ulcers, inflammation of the walls of the gallbladder and its mucous membrane, and purulent discharge. As a result, the bubble shell may collapse. The gangrenous type is characterized by the covering of the walls of the organ with dead tissue, which may result in the appearance of biliary peritonitis. The fibrinous type, which is also called diphtheric, is characterized by the appearance of coatings inside the organ that are tightly adjacent to the inner wall.
- Perforated type, which appears as a result of inflammatory processes or under the influence of pancreatic proteases.
- The last type that is distinguished according to the ICD is a complicated type, in which the signs of hepatitis and cholangitis are often mixed.
Pathogenesis
Since the trigger point is considered to be a violation of the outflow of secretions, it is necessary to find out its cause. These include various stenoses of the cystic duct, the terminal part of the common bile duct or the greater duodenal papilla, blockage with mucus, stones, parasites, etc. Intravesical hypertension reduces the barrier function of the epithelium of the gallbladder, which facilitates the penetration of microorganisms into it that cause an inflammatory process. Such bacteria include Klebsiella, Escherichia coli, and pseudomonas.
In elderly patients, the cause of inflammation may be tissue ischemia, allergic reactions, and bile stagnation. This variant of the disease is called acalculous cholecystitis.
Gallstones
Causes of acute cholecystitis
One of the reasons is an insufficient amount of vegetables and fruits.
When acute cholecystitis occurs, infectious infection plays an important role and is the main factor. Bacteria can enter the organ through blood flow, which provokes the development of severe irritation. These microorganisms can come from other organs, for example those related to the digestive system or from the nasopharyngeal area. pin up
Another reason may be bile stagnation or impaired drainage function of the bladder. If the functioning of an organ is disrupted, its membranes become inflamed due to the acids contained in bile. Other factors include:
- impaired diet (insufficient amount of vegetables and fruits, the presence of fatty, spicy and salty foods in large quantities);
- constant consumption of alcoholic beverages;
- lack of physical activity;
- changes in hormonal levels;
- diseases of the endocrine system (for example, diabetes);
- the patient is overweight;
- vascular atherosclerosis.
Often the disease begins due to stones formed in the bile ducts. In most patients, cholecystitis is combined with the appearance of stones, as a result of which an acute calculous form of cholecystitis is diagnosed.
As a result of such factors, the patient’s body weakens, and the ability of the immune system to combat environmental factors decreases.
Symptoms of cholecystitis.
In a small proportion of patients, cholecystitis may be asymptomatic (its chronic version), they do not have clear complaints, so the diagnosis is often verified randomly during the examination.
But still, in most cases the disease has clear clinical manifestations. They often manifest themselves after some kind of dietary error (feast, consumption of fried foods, alcohol), psycho-emotional stress, bumpy driving or excessive physical activity.
All signs of cholecystitis can be combined into the following syndromes:
- painful (dull or sharp pain, localized, as a rule, in the right hypochondrium, but sometimes it occurs in the epigastric region and in the left hypochondrium, and can radiate to the right shoulder, neck, under the shoulder blades);
- dyspeptic (bloating, bitter taste in the mouth, nausea with vomiting, various stool disorders, a feeling of heaviness in the upper right part of the abdomen, intolerance to fat);
- intoxication (weakness, fever, loss of appetite, muscle aches, etc.);
- syndrome of autonomic disorders (headaches, sweating, premenstrual tension, etc.). Patients may not experience all of the listed symptoms. Their severity varies from barely noticeable (with a sluggish chronic course) to almost unbearable (for example, in the case of biliary colic - a sudden attack of intense pain).
Symptoms
Acute cholecystitis is characterized by a clinical picture, which is explained by a number of factors:
- gallbladder changes;
- timing of the disease;
- the appearance of complications;
- characteristics of the patient.
The first symptom is the presence of pain in the area of the right hypochondrium.
The first symptom is the presence of pain, localized in the area of the right hypochondrium. In addition, the pain can spread to the shoulder and back areas. The pain occurs unexpectedly and resembles attacks. Over time, the appearance of pain becomes more intense, accompanied by an increase in body temperature. During the period of exacerbation, upon palpation, you can notice severe abdominal pain, which is a protective reaction of the body.
The syndrome is accompanied by nausea and frequently recurring vomiting, which does not bring relief to the patient and is contaminated with bile. Patients with acute cholecystitis may experience a feeling of bitterness in the mouth. In addition, if you examine the patient, you may notice dry mouth and the presence of a white coating on the tongue. Acute cholecystitis is characterized by increased blood pressure, which affects the general condition of the patient. A person loses his appetite, his heart rate increases, and general weakness is observed.
Types of disease
Acute cholecystitis most often affects the female half of the population, and the risk of occurrence increases with age. There is a possibility that its appearance is influenced by hormonal imbalance. The classification of acute cholecystitis depends on the causes of the development of the disease.
The disease is divided into 4 types, which differ in the degree of inflammation:
- Acute obstructive cholecystitis. In this form, the inflammation is superficial without pus.
- Acute phlegmonous cholecystitis. This type affects all layers of the gallbladder and causes pus.
- Gangrenous uncomplicated form. With this form of the disease, part or all of the organ wall dies.
- Gangrenous complicated cholecystitis. With it, the walls of the bladder become thinner and rupture. Bile enters the abdominal area and causes more serious problems.
Acute cholecystitis is also divided into 3 types of severity:
- Light form. This type is distinguished by the fact that the disease lasts less than 3 days, there are no symptoms of complications, and other organs are not damaged.
- The average type is characterized by the course of the disease for more than 3 days, the number of leukocytes in the blood already increases significantly, the affected organ is felt upon palpation, there are symptoms of peritonitis, cell death and an increase in the size of the diseased organ. If a patient has any of these signs, this indicates that he has moderate acute cholecystitis.
- In severe cases, there are symptoms of changes in one of the organs in the body:
- blood pressure drops below 80/50;
- depression of consciousness;
- breathing problems;
- changes in kidney function are usually accompanied by a sharp decrease in the amount of urine excreted and an increase in creatinine in the circulatory system (more than 176.8 µmol/l), which indicates the presence of renal failure;
- decrease in platelet count (less than 100*109/l);
- changes in liver parameters in tests (increased prothrombin index, decreased protein content and other components that are metabolized in the gallbladder).
Tests and diagnostics
To examine the patient, they find out whether the diet was violated and whether the patient was in a stressful state. The diagnosis is influenced by syndromes detected by palpation. Further diagnosis consists of performing an ultrasound, which determines the degree of organ enlargement and the presence of gallstone manifestations.
Next, a computed tomography scan is performed, which shows a detailed clinical picture. A mandatory item is blood and urine tests, which show even the slightest signs of inflammatory processes. An important point is to carry out differential diagnosis. It is needed to rule out the occurrence of other diseases and begin proper treatment.
Acute cholecystitis. Symptoms, diagnosis, treatment of acute cholecystitis.
Acute cholecystitis develops in 13-18% of patients with acute surgical diseases of the abdominal organs. Women get sick 3 times more often than men.
The reasons for the development of acute cholecystitis are varied. These include hypertension in the biliary tract, cholelithiasis, infection in the biliary tract, poor diet, stomach diseases accompanied by dyscholia, decreased nonspecific resistance of the body, changes in the vessels of the biliary tract due to atherosclerosis.
Violation of the closing function of the sphincters located in the terminal section of the common bile duct and the large duodenal nipple leads to the development of spasm. This delays the release of bile into the duodenum and causes hypertension in the biliary tract. The causes of hypertension can also be morphological changes - stricture of the terminal part of the common bile duct, which occurs in the presence of long-term choledocholithiasis. This stricture causes permanent cholestasis. In patients, the liver becomes enlarged and hyperbilirubinemia syndrome develops. Hypertension can also be caused by the presence of single gallstones larger than 0.3-0.5 cm, which are displaced into the distal part of the common bile duct, which leads to the development of progressive obstructive jaundice and cholecystocholangitis.
It has been established that in 80 - 90% of cases, acute cholecystitis is a complication of cholelithiasis. In this disease, stones that remain in the lumen of the gallbladder for a long time disrupt the integrity of the mucous membrane and the contractile function of the gallbladder. Often they obstruct the mouth of the cystic duct, which contributes to the development of the inflammatory process.
The nutritional factor, as a rule, is the trigger in almost 100% of patients. Spicy and fatty foods, taken in excessive quantities, stimulate intense bile formation, which leads to hypertension in the ductal system due to spasm of the sphincter of Oddi. In addition, it is possible that food allergens act on the sensitized membrane of the gallbladder, which is also manifested by the development of spasms.
Among the diseases of the stomach that can lead to the development of acute cholecystitis , chronic hypoacid and anacid gastritis, accompanied by a significant decrease in the secretion of gastric juice, especially hydrochloric acid, should be noted. With achylia, pathogenic microflora from the upper parts of the digestive canal can enter the biliary tract from the lumen of the duodenum into the gallbladder.
The development of acute cholecystitis is facilitated by local ischemia of the mucous membrane of the gallbladder and a violation of the rheological properties of the blood. Local ischemia is the background against which, in the presence of pathogenic microflora, acute destructive cholecystitis easily occurs.
The clinical picture of acute cholecystitis depends on the pathomorphological changes in the gallbladder, the duration of the disease, the presence of complications and the reactivity of the body. The disease usually begins with an attack of pain in the right hypochondrium. The pain radiates upward to the right shoulder and scapula, the right supraclavicular region. It is accompanied by nausea and repeated vomiting. Characteristic signs are the appearance of a bitter sensation in the mouth and the presence of bile in the vomit. In the initial stage of the disease, the pain is dull; as the process progresses, it becomes more intense. In this case, there is an increase in body temperature to 38 ° C, and sometimes there is chills. The pulse quickens in accordance with the increase in body temperature. With destructive and especially perforative cholecystitis, complicated by peritonitis, tachycardia up to 100-120 per minute is observed. Sometimes there is icterus in the sclera. Severe jaundice occurs when the patency of the common bile duct is impaired due to obstruction of the lumen by a stone or inflammatory changes.
The tongue is dry and coated. On palpation, the abdomen is painful in the right hypochondrium; protective tension of the abdominal muscles and symptoms of peritoneal irritation are observed here, which are most pronounced in destructive cholecystitis.
Specific symptoms of acute cholecystitis are pain when tapping the edge of the palm along the right costal arch (Grekov-Ortner symptom), pain on deep palpation in the right hypochondrium (Ker's symptom), increased pain on palpation during inspiration (Obraztsov's symptom), pain on palpation between the legs of the right sternocleidomastoid muscle (Mussy-Georgievsky symptom). The patient cannot inhale during deep palpation in the right hypochondrium (Murphy's symptom).
Leukocytosis, neutrophilia, and lymphopenia are detected in peripheral blood. The following classification of acute cholecystitis :
- acute calyx cholecystitis;
- acute acalculous cholecystitis - simple (catarrhal), phlegmonous, gangrenous, perforative, complicated (peritonitis, cholangitis, obstruction of the common bile duct, perivesicular abscess, liver abscess, etc.).
The most characteristic symptom of acute simple cholecystitis is pain in the right hypochondrium. Half of the patients experience nausea and vomiting. Body temperature is normal or subfebrile. The abdomen is soft, the liver is not enlarged, and the gallbladder is not palpable. Positive symptoms of Ortner, Kehr, Obraztsov, etc. are noted.
The clinical picture of destructive cholecystitis (phlegmonous, gangrenous) is characterized by the presence of constant pain in the right hypochondrium (in 100% of patients), vomiting (in 70%), high body temperature - up to 38-40 ° C (in 65%), jaundice (in 39 %). An objective examination reveals sharp pain in the right hypochondrium, muscle tension, enlargement of the gallbladder and liver (in the presence of jaundice). The positive symptoms of Ortner, Obraztsov, Kera, Mussi, Shchetkin - Blumberg, etc. are determined. It should be remembered that with gangrene of the gallbladder, pain may decrease due to the death of nerve endings in its wall. At the same time, the patient’s condition worsens, and intoxication symptoms increase.
The clinical picture of perforated cholecystitis is characterized by the appearance of pain, first in the right hypochondrium, and then throughout the abdomen. Perforation of the gallbladder most often occurs 48 - 72 hours from the onset of the disease, and, as a rule, in elderly and senile patients.
Changes in the wall of the gallbladder can develop not only as a result of an inflammatory process of microbial origin, but also as a result of the action of proteolytic enzymes of the pancreas that enter the lumen of the gallbladder through the biliary tract. These enzymes make the gallbladder wall permeable to bile within 4-6 hours. Bile peritonitis develops.
Acute cholecystitis, complicated by cholangitis and hepatitis, from the very beginning occurs with intermittent fever with chills, heavy sweats and jaundice.
Due to intoxication of the body, lethargy, depression or euphoria develop. Sometimes loss of consciousness occurs. Jaundice is usually intense. It is accompanied by acute liver failure, and then acute renal failure.
Differential diagnosis.
Acute cholecystitis most often has to be differentiated from renal colic, acute pancreatitis, perforated gastric and duodenal ulcers and acute appendicitis.
Renal colic, in contrast to an attack of acute cholecystitis, is characterized by the occurrence of acute pain in the lumbar region, radiating to the genital area and thigh, as well as the development of dysuric phenomena. Body temperature remains normal, leukocytosis is absent. Formed elements of blood and salts are found in the urine. There are no symptoms of peritoneal irritation. Pasternatsky's symptom is positive.
Acute appendicitis with high localization of the appendix can simulate acute cholecystitis. Unlike acute appendicitis, acute cholecystitis occurs with repeated vomiting of bile, characteristic irradiation of pain to the right shoulder blade and shoulder. There is no Mussi sign in acute appendicitis.
Making a diagnosis is facilitated by a history of evidence that the patient has gallstone disease. Acute appendicitis is usually more severe and is characterized by rapid development of peritonitis.
Perforated ulcers of the stomach and duodenum, mostly covered, sometimes simulate acute cholecystitis. Acute cholecystitis, in contrast to perforated ulcers, is characterized by the absence of a history of ulcers and the presence of indications of cholelithiasis.
Acute cholecystitis occurs with repeated vomiting of bile and characteristic irradiation of pain. The pain is localized in the right hypochondrium and increases gradually, body temperature is elevated.
Covered perforations of ulcers have an acute onset. In the first hours from the onset of the disease, pronounced tension in the muscles of the anterior abdominal wall appears. Often there is local pain in the right iliac region due to leakage of gastric contents, which is not typical for acute cholecystitis. In acute cholecystitis, liver dullness is preserved.
Acute pancreatitis, in contrast to acute cholecystitis, occurs with rapidly increasing symptoms of intoxication, tachycardia, and intestinal paresis. The pain is localized mainly in the left hypochondrium or epigastric region, and is of a girdling nature. It is accompanied by frequent and sometimes uncontrollable vomiting.
Differential diagnosis of acute cholecystitis and acute pancreatitis is very difficult and is carried out in a surgical hospital.
Treatment
patients
with acute cholecystitis should be started at the prehospital stage. An antispasmodic mixture is administered intravenously: 2 ml of a 2% solution of no-shpa, 2 ml of a 2% solution of papaverine hydrochloride, 2 ml of a 0.2% solution of platyphylline hydrotartrate and 1 ml of a 0.1 %
solution of atropine sulfate. This relieves spasm of the sphincter of Oddi and reduces intraductal pressure due to improved outflow of bile into the duodenum.
All patients with acute cholecystitis are subject to urgent hospitalization in a surgical hospital for further treatment (conservative and surgical).
Complications
When a form of acute cholecystitis is detected, complications may arise that are associated with the spread of infection. As the disease progresses, acute pancreatitis may appear, which changes the nature of the disease. In addition, diabetes mellitus may develop, which, when combined with cholecystitis, can lead to angina pectoris or myocardial infarction.
The most serious complication may be biliary peritonitis, which occurs due to abdominal trauma or severe infection. Because of this, unpleasant complications of acute cholecystitis can develop, including the fusion of ruptured areas of the bladder with neighboring organs.
Causes and pathogenesis
By its structure, bile does not have a sterile environment, since microbes and bacteria from the duodenum regularly enter it, however, for inflammation to occur, favorable conditions must be present.
These include stagnation in the bubble. In 90% of cases, the cause of bile stagnation is the presence of stones that close the lumen and form a barrier to outflow. In this situation, acute calculous cholecystitis develops.
The calculous form of this pathology in the literal sense of the word is “stone”. The presence of stones is detected in 10-20% of cases in the age group over 40 years. In Western countries, stones formed by cholesterol are more common due to the characteristics of the national cuisine. In African and Asian countries, pigmented stones are found due to a large number of infectious diseases of the biliary tract (malaria).
Much less common are symptoms of acute cholecystitis caused by stagnation of bile due to other development factors. In this situation, this pathology will be called acute acalculous cholecystitis. Reasons for appearance:
- Concentration of bile and the formation of a plug that prevents outflow.
- Biliary dyskinesia (BD) - this disease develops as a result of impaired contractions of the gallbladder and its ducts, which create favorable conditions for stagnation of bile.
- Anatomically incorrect formation of the bladder and duct, in which the outflow of secretions is disrupted.
- Narrowing of the duct due to the presence of tumors or injuries.
- Change in the shape of the gallbladder.
- A change in the shape and location of the duct, which is caused by inflammation of nearby organs.
- External physical activity.
Treatment
If a person is diagnosed with “Acute cholecystitis,” he requires emergency medical care. Treatment of acute cholecystitis can be conservative or surgical, depending on the degree of development of exacerbations of the disease.
Conservative treatment is aimed at cleansing the body of infection with the help of special antibacterial drugs, including antibiotics. An important role in therapy is played by a properly selected diet, which should not contain chemically grown products. The doctor prescribes medications that relieve pain. These are antispasmodics that begin to act within a few minutes.
If such therapy does not help, the doctor prescribes surgery. But before it is carried out, the patient must be fully examined so as not to injure any area.
Treatment of cholecystitis.
Medical tactics are determined by the form of cholecystitis, its stage and severity. Acute forms of the disease are treated exclusively in a hospital. With chronic variants, patients with mild and uncomplicated forms without intense pain syndrome can do without hospitalization. Therapeutic measures can be conservative and radical (surgical).
Conservative treatment.
It is mainly used in cases of chronic variants of the disease. Possible non-surgical methods include:
- diet;
- drug therapy;
- extracorporeal lithotripsy (shock wave).
Medical nutrition.
The nutrition of patients in the acute phase of the process must certainly be gentle and fractional. In particularly serious cases, sometimes they even resort to a couple of “hungry” days, during which only liquids are allowed (weak warm tea, rosehip decoction, diluted berry or fruit juices, etc.). Next, all products are boiled or cooked using a double boiler, and then pureed.
Stewing and baking before remission occurs are prohibited. All fatty dishes and products are removed from the diet (dairy, pork, goose, lamb, duck, red fish, lard, pastry creams, etc.), smoked foods, canned food, spicy seasonings, sweets, cocoa- and caffeine-containing drinks, chocolate, egg yolks , baked goods. Slimy soups, pureed porridges, vegetable, fish, meat or cereal soufflés, puddings, dumplings, steamed cutlets, jelly, mousses, and protein omelettes are welcome.
Butter (as a source of mucous membrane protector - vitamin A) and vegetable oils (soybean, corn, vegetable, cottonseed, olive, etc.) are allowed.
All drinks and meals should be served warm to the patient, as cold can cause a painful attack of pain. After the long-awaited remission occurs, baking and stewing are allowed, food is no longer pureed, and fresh berries, herbs, vegetables, and fruits are included in the diet.
To improve the composition of bile and reduce its ability to form stones, dietary fiber is indicated. It is rich in grains (buckwheat, oats, barley, etc.), kelp, bran, vegetables, algae, and fruits.
Read more:
Diet “Table No. 5”.
Drug treatment of cholecystitis.
During an exacerbation of any cholecystitis, patients may be prescribed:
- antibiotics that penetrate the bile in concentrations sufficient to destroy the infection (doxycycline, ciprofloxacin, erythromycin, oxacillin, rifampicin, zinnate, lincomycin, etc.);
- antibacterial agents (biseptol, nevigramon, furazolidone, nitroxoline, etc.);
- antiparasitic drugs (depending on the nature of the parasite, they are prescribed - Macmiror, Metronidazole, Tiberal, Nemozol, Biltricid, Vermox, etc.);
- detoxification agents (Ringer's solutions, glucose, reamberin, etc.;
- non-narcotic analgesics (baralgin, spazgan, trigan D, took, etc.);
- antispasmodics (papaverine, halidor, mebeverine, no-shpa, buscopan, etc.).
- perinephric novocaine blockade (for unbearable pain, if it is not relieved by other medications);
- means for stabilizing the autonomic nervous system (elenium, motherwort, eglonil, melipramine, benzohexonium, etc.);
- antiemetic drugs (domperidone, metoclopramide, etc.);
- immunomodulators (imunofan, polyoxidonium, sodium nucleinate, lykopid, timoptin, etc.).
After stopping the inflammation in the case of calculous cholecystitis, some patients try to dissolve the stones with the help of medications. For this purpose, doctors prescribe medications with ursodeoxycholic or chenodeoxycholic acid (ursofalk, henofalk, urdoxa, ursosan, etc.). It is best not to take these drugs on your own, as they may only be effective in 20% of patients. There are certain clear indications for their use, which can only be determined by a qualified specialist.
For each patient, the optimal doses of medications are determined individually. They must be taken for a long time (about a year) and regularly. Treatment is carried out under medical and laboratory supervision (periodically it is necessary to determine biochemical blood parameters and perform ultrasound).
Self-medication is fraught with the development of pancreatitis (inflammation of the pancreas), blockage of the bile ducts, intense pain, and severe diarrhea.
During the remission phase of acalculous cholecystitis, patients can begin a course of choleretic drugs. But for this it is advisable to have information about the type of functional disorders. The arsenal of modern choleretic drugs is extremely rich. Patients are recommended hofitol, odeston, oxafenamide, pumpkinol, cholenzym, nicodin, hepatofalk, milk thistle, tansy, fume, barberry, immortelle, galstena, cholagogum, magnesium salts, xylitol, etc. In the presence of confirmed stones in any fragment of the biliary system (bile ducts or gall bladder) choleretic drugs are dangerous .
Extracorporeal lithotripsy (shock wave).
The stones are destroyed by shock waves generated from special installations. The technique is possible only if the cholesterol composition of the stones and the contractility of the bladder are preserved. It is often combined with medicinal litholytic therapy (drugs of cheno- and ursodeoxycholic acid) therapy, which is needed to eliminate fragments of stones formed as a result of extracorporeal lithotripsy. In the Russian Federation, this technique is used quite rarely.
Prevention
It is necessary to give the body physical activity.
To avoid the onset of the disease, you need to remember the following preventive measures:
- Remove spicy, fatty and salty foods from your diet, because such foods have a detrimental effect on the digestive system.
- You need to give your body physical activity, play sports, walk more.
- It is necessary to follow a diet.
- Prevent the appearance of roundworms.
- Avoid stressful situations whenever possible.
- Drink plenty of fluids.
Conclusion
Acute cholecystitis is a serious disease that requires urgent medical advice. According to the ICD, several types of disease are distinguished, which are characterized by certain symptomatic series. Depending on the degree of development of exacerbations of the disease, the doctor can select the most appropriate medicine or prescribe surgery. It depends on how early the patient went to the doctor.
The best option would be examinations by a doctor at least once a year, tests for research and an ultrasound scan. In addition, you need to lead an active lifestyle and remember to eat properly. This will help maintain overall health and prevent the development of diseases. Otherwise, complications of acute cholecystitis occur, which cannot always be cured.