| Hallucinosis | |
| ICD-10 | 10.5210.52 |
| ICD-9 | 291.3291.3 |
Hallucinosis
or
hallucinatory syndrome
is a psychotic disorder, the main manifestation of which is an abundant influx of hallucinations (usually simple, that is, within the same analyzer), in the absence of disorders of consciousness [1]. The term “hallucinosis” was first used by Carl Wernicke in 1900 to refer to the condition of multiple auditory hallucinations accompanied by lucidity that occurs in alcoholics[2].
The development of hallucinosis is usually preceded by a state of anxiety, fear, and restlessness. Hallucinosis may be accompanied by delusional ideas that are identical in plot to the content of hallucinosis (hallucinatory delusions). This is especially typical for verbal hallucinosis (words, phrases).
Variants of the syndrome according to the type of deception of feelings
Verbal hallucinosis occurs suddenly in the form of a monologue or dialogue. There are commentary, imperative (imperative) hallucinosis. Under the influence of hallucinations, patients may perform certain incorrect, often aggressive, actions towards themselves or others. Verbal hallucinosis is often worse in the evening and at night.
Visual hallucinosis. True visual hallucinosis is not accompanied by disorders of consciousness and is quite rare.
Peduncular visual hallucinosis develops when the pathological process is localized in the cerebral peduncles. A peculiarity of such hallucinosis is the appearance in the twilight of numerous moving visual visions in the form of figures of people, animals, and scene-like paintings. A critical attitude towards this type of disorder remains.
Van Bogart visual hallucinosis is characterized by vivid visual hallucinations in the form of butterflies, birds, and fish. Hallucinations develop after 1 to 2 weeks of increased sleepiness, which can result in narcolepsy. Described in encephalitis.
Gobek's olfactory hallucinosis manifests itself in the fact that the patient perceives bad odors supposedly emanating from his body, sometimes combined with tactile hallucinations and ideas of relation.
Tactile hallucinosis. Sensation of worms, insects, microbes crawling on or under the skin. Usually the sensations are accompanied by an extremely unpleasant, painful feeling, itching, and anxiety.
What is alcoholic hallucinosis
Hallucinations are one of the most common symptoms of intoxication in the human body. They develop in approximately fifteen percent of all alcoholics who drink alcohol on a regular basis. Most often, hallucinosis affects men over forty years of age, who have a weakened psyche and some physical indicators due to drinking alcohol for several years. Women can suffer from these symptoms, but unlike men, their rehabilitation process is much more difficult.
Alcoholic hallucinosis manifests itself in the form of auditory and visual hallucinations. At the same time, the patient continues to navigate space and is fully aware of himself and his behavior. Voices and other signs of mental damage are real for the patient himself. Most often they are hostile and threaten to harm the alcoholic. For example, maim, wound or even kill. For women, imaginary voices may threaten rape or death of loved ones. The voice that appears during intoxication may belong to a man and even children. As a rule, women's voices behave inappropriately - they scream, swear, or, on the contrary, call for help and ask to come somewhere.
Alcoholic hallucinosis manifests itself in the form of auditory and visual hallucinations
Due to the full sensation of these signs, the alcoholic becomes restless. He develops a mania of persecution, and fear or anxiety is clearly expressed. An alcoholic may also take a defensive position and try to protect himself from the emerging threat. Because of this, a dangerous situation often arises in families when the drunk tries to harm both himself and others. In this state, suicide attempts are possible.
Alcoholic hallucinosis is a compelling reason for hospitalization in a hospital and further compulsory treatment under the supervision of specialists from narcology and psychiatry.
Clinical picture
Hallucinations manifest themselves in one or more modalities. Cocaine addiction is characterized by tactile or haptic hallucinosis. If the disorder is caused by other psychoactive substances, visual visions may appear. If a person has epilepsy with damage to the frontal lobe, then such patients are more often diagnosed with olfactory hallucinations.
Dumb people often experience auditory hallucinations, while those with cataracts and blindness often experience visual hallucinations. But most often organic hallucinosis occurs in the form of auditory hallucinations. They appear during wakefulness. At the same time, there are no significant deviations in the cognitive functions of patients.
Most often, visual hallucinations look like little people or animals. Sometimes musical hallucinosis is diagnosed, which is characterized by visions in the form of religious songs.
Alcoholic hallucinosis is much worse. In this case, the patient hears threats from imaginary people or accusations. Very often, alcoholic hallucinations are imperative; they require the alcoholic to do something bad to himself or to people who are nearby.
Diagnosis, course and prognosis
The disease is diagnosed based on medical history and the presence of hallucinations. As soon as organic hallucinosis is suspected, it is necessary to find the organic factor that is its cause based on the data described above. Depending on the form of hallucinations, it is necessary to ask the patient about his lifestyle and illnesses.
It is impossible to say exactly how long hallucinosis will last, because the duration depends on the cause of the disease. Medical statistics show that organic hallucinosis lasts from several hours to weeks. If a person takes hallucinogens, the syndrome goes away quickly. But sometimes the disease becomes chronic (for example, with cataracts or deafness).
In medicine, there are many diseases that at first glance are similar. That’s why it’s so important to differentiate—to separate them from each other. Organic hallucinosis is similar in nature to delirium or some forms of dementia. In addition, similar symptoms are observed during delusional syndromes, but in these syndromes the delirium is systemic in nature. With hallucinosis, if there is delusion, it is associated with unreal visions. In addition, delusion during hallucinosis is unstable, that is, after a while there will be no hint that it happened.
In this case, a person can have organic delusional syndrome and organic hallucinosis at the same time. Therefore, we must take into account the possibility of such a scenario. It is necessary to distinguish hallucinosis from confabulosis, but in the first case there are no cognitive impairments, while in the second there are significant problems with memory.
There are also hypnagogic or hypnopompic hallucinations, which are characteristic of a person falling asleep or waking up. Organic hallucinosis manifests itself only in an awake patient.
Visual or auditory hallucinations can also occur with epilepsy and manifest themselves as part of a seizure.
A very common question is: what is the difference between alcoholic hallucinosis and delirium tremens? In the latter case, hallucinations are often visual, and intensify closer to night. It is also worth separating hallucinations in organic hallucinosis from schizophrenia.
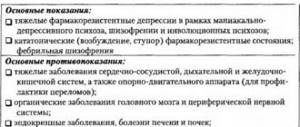
Antipsychotic therapy is used to relieve hallucinations. Although the entire course of treatment is selected strictly individually each time. No one universal scheme can be applied here. It all depends on the cause that led to the onset of hallucinosis. If the reason is temporary, then the patient can be convinced that he has an illness.
Related materials:
Dysthymia is a mental disorder manifested by a depressed emotional state. Unlike depression, dysthymia is characterized by the absence of pronounced behavioral disturbances.
VERBAL HALLUCINOSIS
Read:- Alcoholic psychoses (delirium, hallucinosis, paranoid, Korsakov psychosis). Clinic and treatment.
- Alcoholic hallucinosis, clinical picture, differential diagnosis.
- ALCOHOLIC HALLUCINOSIS.
- In general, there can be a lot of reasons, but it is customary to distinguish alcoholic and atherosclerotic hallucinosis as a separate unit.
- Hallucinatory-delusional syndromes. Paranoid syndrome. Hallucinosis. Paranoid syndrome. Kandinsky-Clerambault mental automatism syndrome. Paraphrenic syndrome.
- Differential diagnosis of alcoholic hallucinosis and paranoids
- METAL ACOHOLIC HALLUCINOSISES AND PARANOIDS
- Peduncular visual hallucinosis (Lhermitte hallucinosis)
- Psychoses: delirium, alcoholic hallucinosis, alcoholic paranoid, alcoholic paranoia, Gaiet-Wernicke encephalopathy (fever, dehydration, stalemate reflexes), Korsakoff psychosis
Hallucinosis is a condition, the clinical picture of which is almost completely exhausted by abundant hallucinations and is not accompanied by clouding of consciousness. There are acute and chronic hallucinosis, depending on the type of hallucinations - verbal, visual and tactile.
Verbal hallucinosis -
an influx of auditory hallucinations in the form of a monologue, dialogue, or multiple “voices”; accompanied by fear, anxiety, motor restlessness, and often figurative delirium. Motor restlessness may fade as hallucinosis develops; patients outwardly remain calm or only sometimes, interrupting work or conversation, listen to something. The examination reveals true hallucinations and pseudohallucinations, which predominate in cases of chronic verbal hallucinosis.
Acute symptomatic psychoses can occur in the form of acute verbal hallucinosis (without stupefaction). Such psychosis develops suddenly with the appearance of verbal hallucinations of a commentary nature (usually in the form of dialogue), accompanied by confusion, anxiety and fear. In the future, hallucinations may acquire imperative content. In this state, patients, under the influence of hallucinatory experiences, commit dangerous actions towards others and themselves. Verbal hallucinosis worsens at night. A rapid influx of verbal hallucinations can lead to the development of so-called hallucinatory confusion.
With vascular psychoses, chronic verbal hallucinosis may appear, often developing after acute hallucinatory psychosis. Chronic vascular hallucinosis is defined by polyvocal true verbal hallucinosis. It flows in waves, often at the height of development it becomes scenic (scenes of public condemnation of a patient, etc.), usually intensifies in the evening and at night, and has a predominantly threatening content. The intensity of hallucinosis is subject to temporary fluctuations with the temporary appearance of criticism of hallucinatory experiences (when they weaken).
Verbal hallucinosis occurs in intoxication (alcohol, hashish, barbiturate, etc.) psychoses, organic diseases of the brain (traumatic, vascular, syphilitic lesions), epilepsy, symptomatic psychoses, schizophrenia.
Date added: 2015-02-05 | Views: 1128 | Copyright infringement
| | | | | | | | 9 | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Symptoms of hallucinosis
Despite some common features, depending on the underlying cause, the symptoms of hallucinosis may vary. For example, with the organic version of hallucinosis, the patient does not lose clarity of consciousness, despite the hallucinations that occur. In the case of epilepsy, visual phenomena are characteristic - simple geometric figures before the eyes, as well as simple sound hallucinations in the form of beeps, whistles, rustling.
More complex verbal hallucinations arise over time and are usually neutral in nature. The patient does not have critical thinking regarding them and tries, for example, to discover the source of sounds or voices. Increasing feelings of anxiety, fear, and worry provoke an “intensification” of verbal hallucinations. The voices become threatening and unpleasant.
The semantic load takes on an offensive character for the patient, spurring his anxiety: the voices discuss the person among themselves, as if behind his back, threaten him with violence, mock him, critically discuss his past and present actions. The very content of hallucinations may vary and depend on the patient’s life experience.
In addition, voices can not only communicate with each other, but also address the subject himself, making him an accomplice of unfolding events and scenes, which makes them seem as vivid as possible and as if they are being experienced in reality. The intensity can also vary, from whispers to screams.
Knowing what hallucinosis is, you can promptly identify its external signs. The moment of manifestation of hallucinatory disorders is expressed by short-term retardation of the patient, detachment. The initial period is marked by the emergence of delusional ideas: the patient begins to say that he is being persecuted, that he is constantly being watched, that they want to kill him or “donate his organs.”
As a rule, they talk about persecution not by one person, but by a group of people. These can be very real individuals, for example, neighbors, former colleagues, work colleagues and even family. Such psychotic disorders are generally characterized by a paranoid attitude to feel danger in almost everything. In this state, affect may develop, which is characterized by despair, anxiety, outbursts of fear and panic, and uncontrolled sudden movements.
Most often, attempts at self-defense and even calls to the police and prosecutor's office are observed. Less often – irritability for no reason, aggression, attempts at suicide. Over a period of time, the patient’s behavior may become orderly, creating a false impression of recovery and normalization.