Inflammation of the conjunctiva, the mucous membrane of the eyes lining the eyelids from the inside, occurs in childhood much more oftenthan in an adult.
Acute conjunctivitis in children can be caused by various pathogens, or may occur as a result of an allergic reaction.
In newborns, infection occurs from an infected mother during childbirth , passing through the birth canal or in utero.
In older children, the pathogen enters the conjunctival sac through contact, through dirty hands or care items. Airborne and dust transmission methods are also possible.
Odnoklassniki
Causes
Inflammation of the eye mucosa can be caused by various reasons. In accordance with them, the following types of conjunctivitis are distinguished:
- Viral - occurs as a result of damage to the mucous membrane by viruses that cause colds. Conjunctivitis caused by the herpes virus can cause especially a lot of trouble.
- Bacterial - caused by the activity of microorganisms that have entered the eye. Bacteria such as cutaneous and Staphylococcus aureus, gonococci, pneumococci, as well as microorganisms that provoke chlamydial infection behave especially aggressively.
- Allergic – manifests itself as a reaction to irritation as a result of exposure to various allergens (pollen, odors, dust, and so on).
Most often, conjunctivitis in children develops due to bacterial and viral infections.
Preventive measures
Due to the fact that conjunctivitis can become inflamed again, it is necessary to unquestioningly follow the doctor’s instructions and carry out preventive procedures that will help consolidate the result. Preventive measures against conjunctivitis include:
- Constant personal hygiene.
- Careful processing of personal care items, since they contain a large concentration of bacteria.
- Disinfection of the room where the patient lives, and after recovery, constant wet cleaning with a disinfectant is recommended. In order to reduce the accumulation of dust in the apartment, it is best to turn on the air conditioner instead of ventilating, which will circulate clean air.
- The doctor may also prescribe additional preventive care measures for the child after completion of the course of treatment.
Conjunctivitis in newborns
Often takes on severe forms, with secondary bacterial infection. This disease is especially difficult for premature, low birth weight babies who have weak immunity. The most common type of conjunctivitis in newborns is blenorrhea. Infection occurs as it passes through the birth canal. The causative agents of blenorrhea are chlamydia and gonococci.
Often newborns' eyes water and stick together, which is explained by blockage of the tear ducts. As a rule, these symptoms disappear during the first month of life and do not require drug treatment. If there is prolonged inflammation of the conjunctiva of the newborn, it is necessary to show it to the pediatrician.
First signs
All types of inflammation of the conjunctiva have similar symptoms. Parents should suspect the onset of the disease if the following symptoms occur:
- itchy eyes;
- discharge of pus;
- redness of the eyes;
- swelling;
- sour eyes;
- swelling of the eyelid;
- increased lacrimation;
- sticking of eyelashes after waking up.
At the beginning of the disease, the baby vigorously rubs his eyelids. He is irritated by bright lighting: the baby develops a fear of light and the eyelids begin to involuntarily shrink (blepharospasm).
Symptoms of the disease
Symptoms appear suddenly and develop rapidly. After waking up, the baby cannot “unstick” his swollen, swollen eyes. Closer examination reveals:
- Swelling of one or both eyelids;
- Redness of the eyes, aggravated by the child’s constant desire to scratch and rub them;
- Children are afraid of bright light, pain when looking out the window or at a lamp;
- tearing of one or more eyes;
- Protein hyperemia on the affected side;
- Burning and stinging, feeling like something is in the eyes.
This is how any conjunctivitis manifests itself; it can be bacterial (in 70% of cases), allergic or viral in nature. Various reasons cause an increase in certain signs of the disease. But almost all of them provoke children to rub their sore eyes with their hands, which aggravates the situation and creates the possibility of complications due to infection entering and developing in them.
Symptoms of conjunctivitis in children
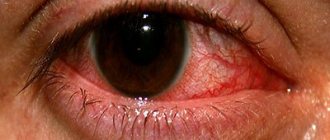
Each type of conjunctivitis has characteristic symptoms (see photo). Let's take a closer look at them.
Bacterial conjunctivitis
Usually lasts from 3 to 5 weeks. The duration of the course depends on the type of pathogen:
- pinpoint hemorrhages in the eyeball;
- burning and itching sensations in the eyes;
- hyperemia of the mucous membrane of the eye;
- copious purulent or foamy discharge from the eyes;
- swelling of the eyelids;
- sticking of eyelids in the morning;
- increased eye fatigue.
Viral conjunctivitis
The disease accompanies ARVI or influenza. First, inflammation occurs in one eye, and then moves to the second. Characteristic features are:
- profuse lacrimation;
- hyperthermia;
- hyperemia of the mucous membrane of the eyes;
- a burning sensation or a foreign body in the eyes (often children associate this with the feeling of sand in the eyes).
Allergic conjunctivitis
The allergic form of the disease has age-related characteristics and is more likely to occur in a 3-year-old child than in a teenager. Symptoms of the disease develop within 24 hours after contact with the allergen. The inflammation spreads to both eyes.
Signs:
- copious watery discharge, lacrimation;
- severe burning and itching, especially when moving the eyes;
- swelling of the eyelids;
- redness of the eye;
- small papillae appear on the mucous membrane;
- feeling of dry eyes;
- increased photosensitivity.
The disease is often accompanied by allergic skin reactions, urticaria, atopic dermatitis and allergic rhinitis.
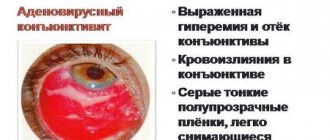
Adenoviral conjunctivitis
In addition to inflammation of the eyes, pharyngitis, hyperthermia, headache, runny nose, weakness, cough, chills appear. They are followed by inflammation of the conjunctiva, first in one eye, and then in the second eye. There is swelling of the eyelids and redness of the mucous membrane. The discharge is scanty, mucous, transparent.
Adenoviral conjunctivitis can occur in three forms:
- Catarrhal, characterized by slight redness and scanty discharge. The duration of the disease is up to 7 days.
- Membranous. With this form, grayish films are formed on the eye, which can be easily removed with a cotton swab. After removing the film, the erosive surface is exposed. Infiltrates and pinpoint hemorrhages may appear, which disappear after treatment.
- Folicular, in which bubbles appear on the mucous membrane of the eye.
Diphtheria conjunctivitis
It occurs against the background of diphtheria of the pharynx and is characterized by gray films on the mucous membrane of the eye. After their removal, the bleeding surface is exposed. The eyelids are swollen and thickened with a bluish tint. The discharge is cloudy with flakes. The general condition is unsatisfactory, there is a headache, fatigue, weakness, and increased body temperature.
Chlamydial conjunctivitis
May occur in newborns 5 to 10 days after birth. In a one-year-old child, infection can occur while swimming in an enclosed body of water, and in a teenager - during early onset of sexual activity.
In most cases, one eye is inflamed. The disease begins acutely and is accompanied by swelling and infiltration of the eyelid mucosa, the formation of large follicles in the lower fornix, and mucopurulent discharge.
Conjunctivitis in childhood
The eyeballs of children are lined with several membranes. One of them is the conjunctiva. It covers the outside of the eye and also lines the back of the eyelids. The main functions of the conjunctiva are to produce fluid and provide moisture to the eyeball. Conjunctivitis is an infectious-allergic disease.
The basis is the inflammatory process. The disease can occur in acute and chronic forms. Over the years, the prevalence of this pathology has decreased. The peak incidence occurs in preschool age. The following types of conjunctivitis are known depending on the etiological factor:
- viral;
- bacterial;
- chlamydial;
- contact;
- allergic;
- fungal.
Depending on the nature of the disease, inflammation can be acute or chronic. In 1 case, symptoms persist for 1-2 weeks. The chronic form of the disease rarely develops. Based on the nature of the exudate, conjunctivitis is divided into purulent, catarrhal, follicular and membranous.
Types of conjunctivitis
Main etiological factors
This ophthalmological disease develops for various reasons. The following risk factors for conjunctivitis in a child are known:
- penetration of bacteria, viruses and fungi into the eye;
- allergy;
- swimming in open reservoirs and pools;
- getting dust and other foreign objects into the eyes;
- eye infection through dirty hands;
- herpetic infection;
- the presence of chronic sinusitis or tonsillitis.
Sometimes damage to the organ of vision is observed with chickenpox. Infectious conjunctivitis of the eyes is most often detected. The causative agents are staphylococci, streptococci, diphtheria bacilli, Koch-Wicks bacteria, viruses, chlamydia and gonococci. Acute conjunctivitis in children is possible during the neonatal period.
The reason is infection of the baby during childbirth from a mother with gonorrhea or chlamydia. In this case, gonoblennorrhea or paratrachoma develops. Microbes can enter the baby’s conjunctiva from other sources of infection. Sources include the paranasal sinuses, oral cavity, tonsils and pharynx.
A risk factor is the presence of pyoderma (pustular skin lesions). Signs of conjunctivitis in children often appear during a period of decreased immunity. Predisposing factors are blockage of the nasolacrimal duct and eye injuries.
The viral form of childhood conjunctivitis develops during influenza, adenovirus infection, chickenpox and herpes. In this situation, combined damage to the eyes, nasal mucosa and pharynx is often observed.
The allergic form of the disease is caused by contact with pollen, dust, wool, fluff and other irritants. Such children often develop diseases: asthma, hay fever and rhinitis.
The risk of developing conjunctivitis at 2 years of age and older increases with low air humidity, poor living conditions, poor nutrition and insufficient care from parents.
Reasons for autology
Development of infectious conjunctivitis
Children aged 1 year often develop a bacterial form of the disease. In most cases, both eyes are affected. Often inflammation initially occurs on one side, then microbes infect the second apple. Very often this pathology is complicated by keratitis and blepharitis. Features of bacterial conjunctivitis in a child are:
- contagiousness;
- bilateral lesion;
- presence of purulent discharge;
- sticking of eyelids;
- the appearance of crusts;
- involvement of the eyelids and cornea in the process;
- acute course.
The causative agents are cocci, Pseudomonas aeruginosa and Haemophilus influenzae. The disease is most severe in weakened children.
For bacterial conjunctivitis in children, symptoms include the presence of:
- mucopurulent discharge;
- secretion deposits on the eyelashes and the edge of the eyelids;
- difficulty opening eyes;
- sticking of eyelashes;
- redness;
- edema;
- lacrimation and fear of bright light.
Bacterial conjunctivitis
In severe cases, pain and a feeling of the presence of a foreign body occur. Purulent discharge has a yellowish or greenish color. With chlamydial infection, the following symptoms are possible:
- drooping eyelids;
- redness of the conjunctiva;
- papillary hypertrophy;
- presence of liquid discharge.
Children aged 3-4 years sometimes develop the diphtheria form of the disease. It is characterized by combined damage to the eyes and pharynx. Upon examination, a film is detected on the conjunctiva. Without treatment, there is a risk of developing complications such as the formation of ulcers in the cornea, its clouding and loss of vision.
A feature of viral conjunctivitis is the presence of common symptoms such as fever, runny nose and cough. The discharge is liquid and abundant. If the cause is herpes, a rash may appear. The disease is well treated with antiviral drugs in the form of drops.
Acute purulent conjunctivitis
Damage to the conjunctiva in newborns
Conjunctivitis develops not only in children 3 years of age and older, but also during the neonatal period. An example is gonoblennorrhea. The causative agents are gonococci. In the absence of proper assistance, there is a risk of developing gonitis and generalization of infection. Symptoms of the disease appear two or three days after birth. Microbes are transmitted to the child from a sick mother.
This does not happen in utero, but during the baby’s passage through the infected birth canal. Most often, both eyes are affected. The following symptoms are observed:
- thickening of the eyelids;
- swelling;
- redness;
- inability to turn eyelids;
- incomplete opening of the palpebral fissures;
- softening of the eyelids;
- the presence of serous-hemorrhagic or purulent secretion.
In severe cases, infiltrates and corneal ulcers form. This is fraught with the formation of a cataract, decreased vision, blindness and endophthalmitis.
Conjunctivitis in newborns
Allergic form of the disease
The second most common is allergic conjunctivitis. It is caused by immune reactions in response to exposure to an allergen. The latter can be:
- contact lenses;
- pollen;
- dust;
- fluff;
- medicines;
- food products;
- animal hair;
- cleaners;
- cosmetics.
Allergic conjunctivitis
The following types of allergic conjunctivitis in children are known:
- hay fever;
- spring;
- medicinal;
- atopic keratoconjunctivitis.
This disease can be year-round, periodic and contact. Chronic pollinous conjunctivitis occurs in the spring, when plants begin to actively bloom. Otherwise, this pathology is called hay fever. Exacerbations occur in May, June and July. Less commonly, symptoms appear in September.
Children aged 3 years and after 14 years often develop vernal keratoconjunctivitis. Its peculiarity is that the cornea is involved in the process. Unlike the hay fever form, the discharge is more viscous, and lacrimation may be absent. This conjunctivitis often goes away without treatment during puberty.
Symptoms of pathology
At 3 years of age, the drug-induced form of the disease may develop. It is characterized by the absence of seasonality and age restrictions, inflammation of the skin of the eyelids, cornea, dysfunction of the retina and optic nerve. Large papillary conjunctivitis is separately identified. It develops in children who wear contact lenses and prosthetic eyes.
The cause of inflammation is prolonged contact with a foreign body. It is possible to develop conjunctivitis after surgery, when sutures remain in the eye. The atopic form is very rare in children.
It affects adults more often. Common symptoms of allergic conjunctivitis in a child are itching, mild swelling, pain, mild redness and watery eyes.
How to treat different types of conjunctivitis?
It is known that, depending on the cause of eye inflammation, the following types of conjunctivitis are distinguished, the treatment of which is different:
- Viral conjunctivitis. Treatment is prescribed by a doctor after examination. Typical pathogens are herpes, adenoviruses, enteroviruses, and coxsackieviruses. If the virus is of herpetic etiology, then Zovirax ointment and Acyclovir are prescribed. Drops with antiviral action Actipol (aminobenzoic acid), Trifluridine (effective against herpes), Poludan (polyriboadenylic acid).
- Bacterial conjunctivitis. The most effective remedy is “Albucid” together with the local use of antibiotic drops and ointments, such as “Levomycetin” or “Tetracycline”. This type of conjunctivitis occurs due to the penetration of microbes and bacteria into the mucous membrane of the eye. The most common pathogens are staphylococci, streptococci, pneumococci, gonococci and chlamydia. In cases where conjunctivitis appears as a side effect of a more serious disease or is protracted, it is necessary to use oral antibiotics for treatment.
- Allergic conjunctivitis. Allergic conjunctivitis is caused by various irritants - house dust, pollen, household chemicals, food, medicines, strong odors and others. Like bacterial conjunctivitis, it is accompanied by redness, swelling of the eyelids, lacrimation, itching (the child constantly scratches his eyes). It is necessary to find out which allergen irritates the child’s eye mucosa and, if possible, limit contact with it. Antihistamines and antiallergic drops reduce the manifestation of the disease. It is imperative to undergo a comprehensive examination by an allergist, since the tendency to allergic reactions in children with other provoking factors can contribute to the development of more serious manifestations of allergies, including bronchial asthma. Treatment: Cromohexal, Allergodil, Olopatodine, Lecrolin, Dexamethasone.
Until a diagnosis has been established, you should not decide on your own how to treat conjunctivitis if the child is 2 years old or younger. But if for a certain reason it is not possible to immediately visit a specialist, if you suspect an allergic or viral form of the disease in a 2-year-old child, you can drop Albucid into the eyes. If there is a suspicion of an allergic nature of the disease, the child should be given an antihistamine.
Treatment
Most conjunctivitis in childhood responds well to treatment. Thanks to proper therapy, complete recovery is achieved without consequences. The prescribed treatment is always comprehensive and includes:
- impact on the cause of the disease;
- therapy for the underlying disease or concomitant pathologies.
In severe cases, accompanied by general symptoms, as well as in the allergic nature of the disease, complex treatment of the whole organism is required.
Washing
Before using any medications, it is necessary to remove the remains of dried exudate, accumulations of pus, and dust particles from the eyelashes and mucous membranes of the eyelids.
Wash the child's eyes with caution using cotton swabs in newborns or special cups in older children.
An individual cotton swab is used for each eye. Begin rinsing with the healthier eye.
Use a weak solution of potassium permanganate, furatsilin, herbal decoctions : calendula, yarrow, chamomile. The solution should be prepared immediately before washing; it should be warm, but not hot. Repeat the procedure at least four times a day , be sure to before introducing drops or ointments into the conjunctival cavity.
Attention! For allergic conjunctivitis, the use of herbs is prohibited to avoid worsening the reaction.
Compresses
One of the methods of treating the disease is the use of compresses in the form of gauze bandages with medicinal substances. solution of boric acid, furacilin, and syntomycin emulsion is used as an impregnating liquid . Compresses are recommended by traditional medicine: it is believed that applying a paste of fresh dill or grated potatoes soothes irritation and relieves itching.
Eye drops
For children, eye drops are the simplest and most convenient form of treatment. Depending on the cause of the disease, there are:
- antiviral drops - Oftalmoferon, Interferon, etc.;
- antibacterial - Levomycetin, Ciprofloxacin, Gentamicin, etc.;
Photo 2. Packaging and bottle of Gentamicin in the form of eye drops with a volume of 5 ml. Manufacturer: USApharm.
- antiallergic - Cromoglin, Cromohexal, Sofradex;
- antifungal - Candide, Fluconazole.
Important! sodium sulfacyl is not recommended due to its irritating effect on the mucous membrane!
Drops are instilled at least three times a day at equal intervals, one drop in each eye.
Ointments
In ophthalmological practice, placing ointment behind the eyelid is a common and effective method of treatment, especially proven as a means of combating bacterial conjunctivitis.
An ointment containing antibiotics (Tetracycline, Gentamicin ) covers the eyeball and eyelid from the inside with a thin film, creating a supply of the drug directly at the site of inflammation.
A small amount of medication is enough, no more than 0.5 cm per eye . The drug must be administered at least twice during the day and always in the evening before bedtime.
How to wash your eyes?
Washing the eyes and removing purulent crusts and mucus is an important procedure in the treatment of conjunctivitis. If there is mucopurulent discharge and crusts, the eyes should be washed with solutions and infusions that you can prepare at home yourself.
- Sage infusion: a tablespoon of sage leaves is steamed with a glass of boiling water;
- Tea infusion: pour a tea bag with a glass of boiling water and leave for 10 minutes;
- Saline solution: dissolve a teaspoon of table salt in a liter of warm boiled water;
- Boiled warm water is good for removing purulent discharge from the eyes;
- Chamomile infusion: two tablespoons of chamomile flowers are steamed with a glass of boiling water, left for 40 minutes;
- Furacilin solution 0.02%: one tablet of furatsilin 0.02 g is dissolved in 100 ml of boiling water;
Before using eye drops or placing ointment behind your eyelid, you should thoroughly clean and rinse your eyes.
Treatment with folk remedies
With the doctor's permission, you can cope with conjunctivitis in a child using alternative medicine. The following recipes are considered the most effective for inflammation of the mucous membrane of the eye in children:
- Pour a glass of boiling water over 2 tablespoons of dried chamomile flowers and leave the solution for 5 minutes. Soak a cotton pad in the cooled, strained solution and gently wipe your eyes with it, moving from the outer corner to the inner.
- Squeeze the juice out of several aloe leaves and mix it with warm boiled water in a ratio of 1 to 10. Moisten a small piece of gauze in the resulting infusion and apply it to your eyes for 10 minutes. Diluted aloe juice can also be used as eye drops.
- Grate 1 raw potato on a small grater and apply the resulting pulp to the inflamed organ of vision for 15 minutes. For the best effect, it is recommended to combine potatoes with egg whites and apply a compress to the sore eye.
- Combine 3 teaspoons of carrot juice with 1 teaspoon of parsley juice and take the resulting mixture orally before each meal for a week.
Folk remedies for conjunctivitis help to quickly relieve symptoms and alleviate the baby’s condition, but they cannot be used for permanent treatment.
Before using any prescription, you should consult your doctor and determine the exact cause of the pathology.
How to instill drops correctly?
Here are some rules:
- For conjunctivitis in a child less than a year old, instillation is carried out using a pipette that has a rounded end, this avoids accidental damage to the inflamed eye.
- Place the baby on the surface without a pillow, let someone help you and hold your head. Initially, you need to pull the eyelid a little and add 1-2 drops. The drug will spread evenly over the surface of the eye on its own. Excess can be blotted off with a gauze napkin. Separate wipes should be used for each eye.
- If an older child closes his eyes. This is not a problem, no need to worry, shout at him or force him to open his eyes. This is not necessary; in this case, it is enough to drop the medicine between the upper and lower eyelids. The solution will get into the eye when the child opens it. But even a closed eye can be opened by simply stretching the eyelids in different directions with two fingers.
- If the drops are stored in the refrigerator, they must be warmed before instillation. Cold drops can act as an additional irritant.
- Do not use eye drops for conjunctivitis that are expired, unlabeled, or if they have been stored open for a long time.
- To treat conjunctivitis in older children, it is better to teach them to independently perform the instillation procedure under the strict supervision of their parents.
Drops for conjunctivitis for children
For effective and prompt recovery, eye drops for conjunctivitis
. There are basic tools that you cannot do without in therapy, and many new drugs have appeared on the market today. Let's look at the most effective medications, including:
Let's look at what drops for conjunctivitis in children
are the most effective, based on reviews from parents (from the
BABYBLOG
and other well-known resources).
These drops have an antiviral effect and provide protection against allergies, helping to quickly and effectively relieve itching. For children, this effect is extremely important due to their habit of constantly scratching their eyes, and this can provoke the introduction of infectious diseases and bacteria. At the beginning of treatment, instillation is carried out frequently, then less frequently.
The drug has a large number of good and beneficial effects on the child’s body. It helps relieve irritation and eliminate itching, effectively and quickly relieves the inflammatory process and creates the necessary conditions for a speedy recovery.
This drug is one of the most frequently used due to its wide spectrum of action, but there is one caveat: it cannot be used for children under 2 years of age. Treatment with these drops in many cases is more convenient than using other means. The course lasts only a week, during which time the main signs of the disease are eliminated. And a nice price
the drug makes it a sales leader.
This remedy also has a wide range of effects, but is recommended for use by children over 1 year of age. Treatment is also carried out over the course of a week, but at first it is carried out intensively, and then the number of drops is reduced. Reviewing the best eye drops for conjunctivitis for children
, it can be noted that this product is the most optimal in terms of price and quality ratio.
This medicine is another effective drug to eliminate the disease. The course of treatment ranges from a week to an unlimited period, depending on the doctor’s instructions. It has an affordable price and a wide range of effects, making it popular among many mothers.
Features of eye drops
If conjunctivitis of the eyes is detected, treatment in children is drops
. However, it is important to know the subtleties of how to instill eye drops so that they feel comfortable and infections die.
- up to a year, instillation is carried out only using a pipette;
- it is necessary to pull back the child’s lower eyelid and drop 1-2 drops;
- wait until the medicine is completely distributed over the eye;
- remove excess drops with gauze or bandage;
- It is important to use a different napkin for each eye.
Using these rules will allow you to achieve optimal treatment results in a short period of time.
How many days does it take to treat conjunctivitis in children?
With adequate and timely treatment, the acute process can be cured in 4-5 days. It may take 4 to 5 weeks for the symptoms of the chronic form of the disease to resolve.
You should not let the disease take its course, even if it is mild. Advanced conjunctivitis can cause serious complications that can lead to vision impairment.
Possible complications
If you do not treat conjunctivitis in a child aged 3 years or self-medicate, the inflammatory process can become chronic, causing the following complications:
- clouding, ulceration of the cornea;
- blepharitis;
- thorn;
- spread of infection;
- constant tearfulness;
- decreased quality of vision.
Conjunctivitis in children rarely leads to complications, but sometimes inflammation can lead to negative consequences such as vision impairment, death of the optic nerve, and even blindness. Such serious complications can be avoided if you consult a doctor in a timely manner and begin proper treatment.
Prevention
Is conjunctivitis contagious in children? More often, inflammation of the mucous membrane of the eyes is infectious in nature, is considered contagious and is transmitted from a sick person to a healthy one. Therefore, it is necessary to observe preventive measures:
- Do not rub or scratch your eyelids, as the other eye will become infected;
- The child must have an individual face towel;
- keep your hands clean;
- carry out regular eye hygiene;
- during epidemic outbreaks of viral conjunctivitis in schools and kindergartens, do not contact the children's team.
If a child has had an eye injury (a speck, a midge, an eyelash has gotten into it), this can lead to bacterial infection of the conjunctiva and acute conjunctivitis. It is imperative to show the baby to an ophthalmologist. The doctor will examine the condition of the mucous membrane and, if necessary, prescribe preventive treatment.
Viral conjunctivitis
As medical practice shows, viral conjunctivitis is accompanied by an acute respiratory viral infection. That is why conjunctivitis is characterized by characteristic symptoms (fever, general weakness and lethargy). In this case, the infection of the eye does not go away immediately, but gradually. At first, a liquid, water-like discharge appears from the child’s eyes (initially, many parents believe that these are tears and do not pay due attention to such an obvious symptom of a serious pathology).
Well, the further path of development of conjunctivitis depends on the infection from which it formed. So, with herpetic conjunctivitis, the baby develops blistering inflammations on the eyelids and a rash, and with measles, a corresponding rash occurs.